Abstract
Heart failure with preserved ejection fraction (HFpEF) is the fastest growing form of heart failure in the United States. The cardinal feature of HFpEF is reduced exercise tolerance (peak oxygen uptake, VO2peak) secondary to impaired cardiac, vascular, and skeletal muscle function. There are currently no evidence-based drug therapies to improve clinical outcomes in patients with HFpEF. In contrast, exercise training is a proven effective intervention for improving VO2peak, aerobic endurance, and quality of life in HFpEF patients.This brief review discusses the pathophysiology of exercise intolerance and the role of exercise training to improve VO2peak in clinically stable HFpEF patients. It also discusses the mechanisms responsible for the exercise training-mediated improvements in VO2peak in HFpEF. Finally, it provides evidence-based exercise prescription guidelines for cardiac rehabilitation specialists to assist them with safely implementing exercise-based cardiac rehabilitation programs for HFpEF patients.
Keywords: cardiorespiratory fitness, cardiac function, vascular function, skeletal muscle function
Condensed Abstract
Heart failure with preserved ejection fraction (HFpEF) is characterized by severe exercise intolerance. The review provides the pathophysiology underlying exercise intolerance and role of exercise training to improve peak oxygen uptake (VO2peak) in HFpEF. It also provides exercise prescription guidelines designed to maximize improvements in VO2peak in patients with HFpEF.
Heart failure (HF) is a major healthcare problem associated with high morbidity and mortality.1 Currently, >6 million Americans ≥ 20 yr of age have HF, and its prevalence is expected to increase by 46% by 2030.1,2 Nearly half of all HF patients have preserved left ventricular ejection fraction (HFpEF) and this phenotype is more common in older individuals, women, and those with a history of hypertension, obesity and anemia.1,3 Decreased exercise tolerance is a hallmark feature in clinically stable HFpEF patients and is associated with reduced quality of life.4,5 Given the relationship between cardiorespiratory fitness (i.e. peak oxygen uptake; VO2peak) and survival,6,7 an important goal of therapy should be to improve HFpEF patients’ cardiorespiratory fitness.8–12
Currently, exercise training is the only proven effective intervention to improve VO2peak, aerobic endurance, and quality of life in HFpEF patients.4,10 Several recent meta-analyses have reported that endurance exercise training, performed alone or combined with resistance training, improves VO2peak and 6-min walk test distance by 2.2 mL/kg/min and 33 m, respectively.4,13,14 Accordingly, understanding the mechanisms responsible for reduced VO2peak and its improvement with exercise training is critical to optimally improve HFpEF patients’ functional capacity and quality of life.
In this brief review, the pathophysiology of exercise intolerance and the role of exercise training to improve VO2peak in clinically stable patients with HFpEF is discussed. Further discussion of the mechanisms responsible for the exercise training-mediated increase in VO2peak is provided, along with evidence-based exercise prescription guidelines for clinically stable HFpEF patients participating in an exercise-based cardiac rehabilitation (CR) program.
PATHOPHYSIOLOGY OF EXERCISE INTOLERANCE IN HFPEF
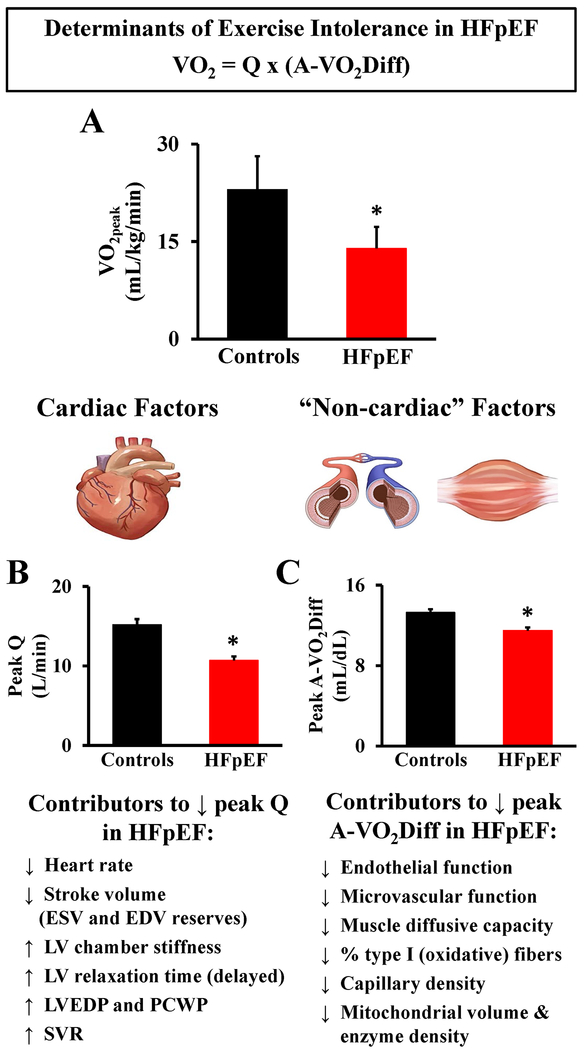
Appreciating the Fick principle for VO2 is fundamental to understanding the pathophysiology of exercise intolerance in patients with HFpEF. Specifically, the Fick principle dictates that VO2 = cardiac output (Q) × arterial-venous O2 content difference (a-vO2Diff), with Q and the a-vO2Diff each having their own modulating factors that ultimately drive the highest achievable VO2 at peak exercise (Figure 1).
Figure 1.
Magnitude and pathophysiology of exercise intolerance in patients with heart failure and preserved ejection fraction (HFpEF). A. HFpEF patients demonstrate severe exercise intolerance, measured objectively as a ~40% reduction in peak oxygen uptake (VO2peak) (mL/kg/min) during peak aerobic exercise compared to healthy age-matched controls, adapted and pooled (mean ± SD) from published data by Bhella et al. (2011)50, Dhakal et al. (2015)16, and Haykowsky et al. (2011)17. B. HFpEF patients demonstrate reduced peak exercise cardiac output (Q) (L/min), adapted from published data (mean ± SE) by Dhakal et al. (2015)16. C. HFpEF patients demonstrate reduced peak exercise arteriovenous oxygen difference (a-vO2Diff) (mL/dL), adapted from published data (mean ± SE) by Dhakal et al. (2015)16. EDV: end-diastolic volume, ESV: end-systolic volume, LV: left ventricle, LVEDP: left ventricle end-diastolic pressure, SVR: systemic vascular resistance, PCWP: pulmonary capillary wedge pressure. * indicates significant (P <.05) difference between HFpEF and healthy age-matched controls for all figures.
Role of Cardiac Function on Exercise Limitations in HFpEF
The reduction in VO2peak observed in patients with HFpEF is due, in part, to a reduction in cardiac function during exercise. Several independent laboratories have demonstrated that peak Q is 30-40% lower in patients with HFpEF compared with control subjects.15–18 Evidence to date suggests that chronotropic incompetence rather than SV is a fundamental concern for the blunted Q response to peak exercise in patients with HFpEF.15–17,19–21 Indeed, significant relationships between Q (independent of major reductions in SV)15 and HR19 with VO2peak have previously been reported, even when matched for important co-morbidities,20 supporting that underlying chronotropic incompetence is a major contributor to reduced Q and subsequent reductions in VO2peak in HFpEF.
Despite the major role that HR plays on the severely reduced peak exercise VO2 in patients with HFpEF, several impairments in left ventricular function have also been reported (Figure 1). Normally, left ventricular (LV) relaxation is augmented during exercise to compensate for the reduction in filling time in healthy individuals.22 However, during exercise in patients with HFpEF, increased LV chamber stiffness and impaired (delayed) LV relaxation causes an increased reliance on left atrial contribution to LV filling.8,23 Further, a functional consequence of marked increases in pulmonary capillary wedge (PCWP) and pulmonary artery pressures is profound dyspnea.8,24,25 A recent study by Obokata et al. 26 highlighted the important contribution of elevated LV filling pressures to exercise intolerance in HFpEF by showing that increased PCWP during exercise was directly correlated with greater dyspnea and lower VO2peak.26
Role of Vascular Function on Exercise Limitations in HFpEF
Impaired vascular function also contributes to reduced exercise tolerance in HFpEF. Hundley et al.27, using cardiac magnetic resonance imaging, demonstrated that distensibility of the proximal thoracic aorta (a measure of arterial stiffness and a contributor to increase afterload and impaired LV-arterial coupling) was lower in HFpEF versus healthy age-matched controls, and predicted the lower VO2peak. Kitzman et al.28 extended these findings by showing a significant reduction in distensibility of the carotid artery in patients with HFpEF compared to healthy age-matched controls, which was also associated with a lower VO2peak. Cumulatively, these findings suggest that increases in central arterial stiffness beyond normal aging contribute to the reduction in exercise tolerance in HFpEF.
Emerging evidence also suggests that skeletal muscle hyperemia is blunted in HFpEF; underscoring a fundamental impairment in O2 delivery to the active limb. Indeed, Lee et al.29 found that femoral artery blood flow during one-leg kicking exercise was 15-25% lower in HFpEF patients compared to healthy age-matched controls performing similar work rates. Likewise, femoral artery blood flow recovery has been shown to be approximately 25% slower following exercise compared to healthy normal values. 30,31
The exact mechanism driving differences in skeletal muscle blood flow during exercise in HFpEF remains incompletely understood. Endothelial dysfunction, measured by flow-mediated dilation in a conduit artery, is indeed impaired in HFpEF patients compared to age-matched reference controls.32,33 However, such group differences are ameliorated when participants are rigorously screened to exclude for the confounding effects of atherosclerosis.28,34,35 Lee et al. 36 suggest that HFpEF may be associated with microvascular dysfunction, because reactive hyperemia—the magnitude of limb reperfusion immediately following a 5-min arterial cuff occlusion—was reduced in HFpEF compared to controls. However, caution is warranted when interpreting these results, as one cannot partition the role of skeletal muscle-mediated differences in the ischemic stimulus without knowing the extent of tissue desaturation during cuff occlusion between groups.37 In support of the microvascular hypothesis; however, Balmain et al.38 demonstrated marked impairments in acetylcholine-induced cutaneous vasodilation (a measure of microvascular function) using iontophoresis coupled laser Doppler imaging in HFpEF compared to controls.38 Likewise, Boyes et al.39 recently reported that priming exercise, a stimulus that may transiently improve microvascular function,40 increased skeletal muscle tissue oxygenation and conferred a substantial increase in the rate of VO2 in the exercising muscles of HFpEF patients. Taken together, these data suggest that microvascular dysfunction may be an important therapeutic target; however, more work is clearly needed to fully elucidate the mechanism(s) contributing to impaired O2 delivery within skeletal muscle in HFpEF. Emerging technologies capable of quantifying skeletal muscle microvascular perfusion and oxygenation should help shed light on these unmet knowledge gaps.41
Role of Skeletal Muscle Dysfunction on Exercise Limitations in HFpEF
A growing body of compelling evidence demonstrates that abnormalities in skeletal muscle composition and function play a major role in limiting VO2peak in patients with HFpEF.42,43 Haykowsky et al.17 found that the strongest independent predictor of VO2peak in patients with HFpEF was the change in estimated a-vO2Diff, and this accounted for approximately 50% of the reduction in VO2peak even when major cardiac determinants of VO2peak were included in the multivariate analysis. These findings have since been confirmed by direct measurement of a-vO2Diff,16 and support the prevailing hypothesis that impaired diffusive O2 conductance (transport of O2 from red blood cell to muscle mitochondria) and/or an inability to sufficiently augment O2 extraction during maximal exercise may be important contributors to reduced VO2peak found in HFpEF (Figure 1).44
Adverse changes in leg muscle mass and volume may directly limit the increase in a-vO2Diff during exercise in patients with HFpEF. Specifically, it has been shown that both percent total and percent leg lean mass are significantly reduced in patients with HFpEF,5 and that the intermuscular adipose tissue and intermuscular adipose/skeletal muscle area ratio are markedly increased.45 Moreover, the increased intermuscular adipose tissue and ratio of intermuscular adipose to skeletal muscle area have both been found to significantly predict a lower VO2peak in HFpEF.45 This finding is important because intramuscular fat may adversely affect mitochondrial density and biogenesis.45,46
Not unlike HFrEF, adverse muscle fiber changes have also been detected in HFpEF. Consistent with a shift to relatively greater glycolytic-dependent metabolism, HFpEF patients have less type I (oxidative) fibers, a lower type I/type II fiber ratio, and a lower capillary/fiber ratio,47 and this fiber type and capillary interface profile is associated with a lower VO2peak. Moreover, patients with HFpEF have been shown to have a reduction in mitochondrial content, citrate synthase activity, and mitochondrial fusion compared with healthy age-matched controls, which is consistent with a lower maximal oxidative capacity.46 Mitochondrial fusion is an important cellular process that ensures that mitochondrial quality and function are preserved by constantly fusing two originally distinct mitochondria together.48,49 This process allows for repair and removal of mitochondria with damaged DNA and creation of new healthy mitochondria via mitochondrial fission (cell division). As such, dysfunction of mitochondrial fusion may lead to accumulation of dysfunctional organelles within the mitochondrial network, leading to reduced overall oxidative phosphorylation capacity. Indeed, impaired mitochondrial fusion is predictive of a low VO2peak and 6-min walk test distance in patients with HFpEF.46 Lastly, during dynamic planter flexion exercise with simultaneous phosphorous magnetic resonance spectroscopy, patients with HFpEF demonstrate a more rapid decrease in phosphocreatine and attenuated maximal oxidative capacity compared to healthy age-matched controls,50,51 which could also be secondary to microvascular impairment. Accordingly, therapies that target microvascular and skeletal muscle function may prove to be most beneficial for patients with HFpEF.
EXERCISE TRAINING AND IMPROVEMENT IN VO2PEAK IN HFPEF
As highlighted in Table 1, only a few studies have examined the role of exercise training to improve VO2peak in clinically stable HFpEF patients. Meta-analyses of exercise (endurance alone or combined with resistance exercise) training versus sedentary usual care have reported a mean increase in VO2peak and 6-min walk test distance of 2.2 mL/kg/min 4,13,14 and 33 m, respectively, which exceed clinically meaningful changes for HF patients.11 In accordance with the Fick Principle, the mechanisms underpinning the improvement in VO2peak may be due to central or peripheral factors. Notably, evidence to date suggests that the increased VO2peak observed with exercise training is primarily secondary to non-cardiac peripheral adaptations.52,53
Table 1.
Randomized controlled exercise intervention trials in heart failure patients with preserved ejection fraction (HFpEF).
| Study | Group (n) | EF (%), NHYA class | Male (%) | Age (yr) | Frequency, Intensity, Time, Training Mode | ET Length (wk) | Main Findings |
|---|---|---|---|---|---|---|---|
| Angadi et al. (2015)55 | HIIT (9) | 65, II-III | 89 | 69 | 3 d/wk 4 × 4 min intervals at 85-90% HRpeak with 3 min active recovery at 50% HRpeak between intervals 25 min total exercise time (16 min HIIT), Treadmill | 4 | ↑ VO2peak; ↓ E, DD grade; ↔ VO2 at VT, LAVI, A, E/A, DT, e’ (septal), E/e’, IVRT, EF, BAFMD |
| MICT (6) | 66, II-III | 67 | 72 | 3 d/wk 60-70% HRpeak 30 min, Treadmill | ↔ VO2peak, VO2 at VT, LAVI, E, A, E/A, DT, e’ (septal), E/e’, IVRT, DD grade, EF, BAFMD | ||
| Edelmann et al. (2011)56 | ET (44) | 67, II-III | 45 | 64 | 2-3 d/wk cycle + 2 d/wk RT (wk 5-12) 50-70% VO2peak cycle, 15 reps at 60-65% 1RM RT 20-40 min, Cycle + RT |
12 | ↑ VO2peak, VO2 at VT, 6MWD, QoL, NYHA class, e’; ↓ E/e’, LAVI, procollagen type I; ↔ LVEF, LVMI, NT-proBNP |
| CON (20) | 66, II-III | 40 | 65 | ||||
| Fu et al. (2016)53 | ET (30) | 58, II-III | 67 | 61 | 3 d/wk 5 × 3 min intervals at 80% VO2peak with 3 min active recovery at 40% VO2peak between intervals 30 min, Cycle | 12 | ↑ VO2peak, arteriovenous oxygen difference, leg muscle oxygenation; ↓ Ve/VCO2, E/e’; ↔ LVEF, LVIDd, LVIDs, peak SVI, CI, HR |
| CON (30) | 57, II-III | 60 | 63 | ||||
| Kitzman et al. (2010)59 | ET (24) | 61, II-III | 17 | 70 | 3 d/wk 40-70% HRR 60 min, Treadmill/Cycle |
16 | ↑ VO2peak, VO2 at VT, 6MWD, physical QoL; ↔ rest E, A, DT, IVRT, LV EDV, ESV, EF, LVM, LVM/volume, norepinephrine, BNP |
| CON (22) | 60, II-III | 9 | 69 | ||||
| Kitzman et al. (2013)58 | ET (24) | 58, II-III | 28 | 70 | 3 d/wk 40-70% HRR 60 min, Treadmill/Cycle/Arm Ergometer |
16 | ↑ VO2peak, VO2 at VT, peak HR, 6MWD, physical QoL; ↔ carotid arterial stiffness, BAFMD, rest E, A, DT, IVRT, LV EDV, ESV, EF |
| CON (30) | 56, II-III | 20 | 70 | ||||
| Kitzman et al. (2016)57 | ET (24) | 61*, II-III | 19 a | 67 a | 3 d/wk 40-70% HRR 60 min, Treadmill |
20 |
Main Effect for ET:
↑ VO2peak, 6MWD; ↓ peak DBP, NYHA class, body weight, fat mass; ↔ rest E, E/A, E/e’, LVM, EDV, EF, LAD, arterial stiffness |
| CR (24) | -400 kcal/d CR |
Main effect for CR: ↑ VO2peak, 6MWD, rest E/A, leg muscle quality, QoL; ↓ peak DBP, NYHA class, body weight, lean mass, fat mass (abdominal visceral and subcutaneous, thigh subcutaneous), rest LVM, h/R |
|||||
| CR + ET (24) | -350 kcal/d CR + ET | ||||||
| CON (22) | |||||||
| Smart et al. (2012)60 | ET (12) | 59, II-III | 58 | 67 | 3 d/wk 60-70% VO2peak 30 min, Cycle |
16 | ↑ VO2peak; ↓ Ve/VCO2 slope; ↔ peak HR, rest E, A, E/A, S, E/e’, DT, strain, strain rate, LVEF, CO |
| CON (13) | 57, II-III | 46 | 62 |
↑ = increase; ↓ = decrease; ↔ = no change; 1RM = one repetition maximum; 6MWD = six minute walk-test distance;
Abbreviations: A, atrial filling velocity; CI, cardiac index; CO, cardiac output; CR, caloric restriction, DBP, diastolic blood pressure; DD, diastolic dysfunction grade; DT, deceleration time; E, early filling velocity; e’, early diastolic velocity of the mitral annulus; E/A, early to atrial filling velocity ratio; E/e’, early mitral inflow velocity to early diastolic mitral annulus ratio; EDV, end-diastolic volume; EF, ejection fraction; ESV, end-systolic volume; ET, exercise training; HIIT, high-intensity interval training; h/R, relative wall thickness; HR, heart rate; HRpeak, peak heart rate; HRR, heart rate reserve; IVRT, isovolumic relaxation time; LAD, left atrial diameter; LAVI, left atrial volume index; LVEDVI, left ventricular end-diastolic volume index; LVESVI, left ventricular end-systolic volume index; LVIDd, left ventricular internal diameter in diastole; LVIDs, left ventricular internal diameter in systole; LVM, left ventricular mass; LVMI, left ventricular mass index; MICT, moderate-intensity continuous training; NT-proBNP, N-terminal pro b-type natriuretic peptide; NYHA, New York Heart Association; QoL, quality of life; Reps, repetitions; RT, resistance training exercise; S, systolic annular velocity; SV, stroke volume; SVI, stroke volume index; VT, ventilatory threshold; VO2peak, peak oxygen uptake.
indicates whole group mean.
Exercise Training and Cardiac Function in HFpEF
Several studies have investigated changes in resting54–59 and peak exercise cardiac function52,53 following exercise training (typically employed in CR programs) in HFpEF. The majority of these studies report little to no change in resting LV volumes, systolic or diastolic function after training.54,56–59 In agreement with these findings, Fujimoto et al.60 found no improvement in invasively measured LV diastolic compliance after 1 yr of progressive and vigorous endurance training in HFpEF patients. In addition, a recent meta-analysis by Fukuta et al.4 concluded that the improvements in VO2peak associated with exercise training occurred without significant changes in resting LV systolic or diastolic function in patients with HFpEF.
To date, only two studies have assessed changes in the Fick principle determinants of VO2peak following exercise training in HFpEF.52,53 Haykowsky et al.53 reported that 16-wk of moderate-intensity endurance training significantly increased estimated peak a-vO2Diff with no change in peak Q. Importantly, 84% of the endurance training-mediated increase in VO2peak was due to the change in estimated a-vO2Diff. Fu et al.52 confirmed these findings by demonstrating that increases in VO2peak with 12 wk of high-intensity interval training (HIIT) were secondary to increased estimated a-vO2Diff, with no changes in peak exercise SV or Q. Taken together, the findings suggest that the improvements in VO2peak observed following exercise training in HFpEF appear to be driven by “non-cardiac” peripheral adaptations that may facilitate improved O2 extraction and utilization by exercising muscles, with little to no change in resting or peak exercise cardiac function.
Exercise Training and Vascular Function in HFpEF
Exercise training-mediated improvements in peak exercise a-vO2Diff may be the result of improvements in peripheral vascular and/or skeletal muscle adaptations.52,53 Several studies have investigated the effects of exercise training on peripheral vascular function in patients with HFpEF.54,56,57 Kitzman et al.56,57 found that 16-20 wk of moderate-intensity endurance training did not change carotid arterial stiffness, carotid-femoral pulse wave velocity, or brachial artery flow-mediated dilation. Angadi et al.54 confirmed and extended these findings by showing that 4 wk of either moderate-intensity endurance training or HIIT did not change brachial artery flow-mediated dilation. To our knowledge, no study has evaluated the effect of exercise training on microvascular function. This is an important unaddressed knowledge gap which warrants future investigation.
Exercise Training and Skeletal Muscle Function in HFpEF
Currently, no studies have examined the role of exercise training on skeletal muscle morphology or function. However, given the plethora of skeletal muscle abnormalities that contribute to exercise intolerance in HFpEF,44,47,50,51 future studies are urgently needed to examine the improvements in skeletal muscle morphology and oxidative metabolism following exercise training in HFpEF.
NOVEL INTERVENTIONS TARGETING EXERCISE INTOLERANCE IN HFPEF
High-intensity interval training
High-intensity interval training (HIIT) consists of brief intermittent bursts of vigorous exercise (85-95% peak HR), interspersed with periods of rest or active recovery. A growing body of evidence shows that HIIT can serve as an effective alternative to traditional endurance-based training, inducing similar or even superior physiological adaptations in both healthy individuals and diseased populations.61,62 A 2014 systematic review and meta-analysis by Weston et al.62 demonstrated that HIIT elicits a 9% superior improvement in VO2peak compared to traditional moderate-intensity endurance training when carried out in clinical populations that included patients with coronary artery disease, HF, hypertension, metabolic syndrome, and obesity. To date, only two randomized controlled trials have assessed the effects of HIIT on improvement in VO2peak in HFpEF.52,54
Angadi et al.54 were the first group to compare improvements in VO2peak with HIIT versus traditional moderate-intensity endurance training in patients with HFpEF. Despite a shorter duration 4 wk), HIIT elicited a significant increase in VO2peak (+1.8 mL/kg/min), with no changes observed following moderate-intensity endurance training. Furthermore, the improvements in VO2peak occurred with only modest changes in cardiac function. Fu et al.52 compared the effects of 12 wk of HIIT on VO2peak and its determinants versus a standard of care sedentary control group in patients with HFpEF. HIIT increased VO2peak by 2.5 mL/kg/min, secondary to increases in peak exercise a-vO2Diff and improved muscle oxygenation of the vastus lateralis, with little to no changes in peak exercise cardiac function. Taken together, these short-term HIIT studies suggest that HIIT is an effective stimulus to improve VO2peak; however, the magnitude of improvement (mean change: +2.2 mL/kg/min) is no different to the mean improvement reported following longer duration moderate-intensity endurance training in patients with HFpEF.4,13,14 As such, it is still unclear if HIIT is superior to moderate-intensity endurance training for improving VO2peak in the long-term (>3 mo). However, a large multicenter randomized controlled exercise training intervention study (OptimEX-CLIN) is currently ongoing to assess the optimal dose and intensity of exercise training for improvement of VO2peak in patients with HFpEF, including a direct comparison between 12 mo of HIIT versus moderate-intensity endurance training.63
Dietary caloric restriction and exercise training
Over 80% of patients with HFpEF are either overweight or obese, and excess adiposity has been shown to adversely affect cardiac, vascular, and skeletal muscle function.45,64–67 In obese older adults without HF, weight loss via dietary caloric restriction improves LV hypertrophy and diastolic function, cardiorespiratory fitness, glycemic control, blood pressure regulation, body composition, and skeletal muscle function.68–72 However, current HFpEF management guidelines do not include dietary caloric restriction as a treatment,73 in part due to observational studies reporting that overweight or moderate obesity may improve survival in patients with HFpEF when compared to those patients who are normal or underweight.67
Despite the apparent presence of an obesity paradox in HFpEF, Kitzman and colleagues56 recently demonstrated that 20 wk of caloric restriction improved VO2peak, body composition, skeletal muscle quality, and quality of life in obese patients with HFpEF. Furthermore, combining caloric restriction with moderate-intensity endurance training created an additive effect for the improvement in VO2peak (+2.5 mL/kg/min), compared to endurance training (+1.2 mL/kg/min) or caloric restriction (+1.3 mL/kg/min) alone. Finally, improvements in VO2peak were also positively associated with improvements in percent lean mass and the change in thigh muscle to intermuscular fat ratio. Further studies are warranted to establish whether the favorable changes in cardiorespiratory fitness and body composition observed with caloric restriction alone or in combination with exercise training result in reduced clinical endpoints (mortality, hospital readmissions) in patients with HFpEF.
EXERCISE TRAINING AND IMPROVEMENT IN QUALITY OF LIFE IN HFPEF
Supervised exercise training not only improves VO2peak and aerobic endurance, but also patient-reported quality of life in clinically stable HFpEF patients.55,57,58 Indeed, a recent meta-analysis by Fukuta and colleagues4 reported that endurance exercise training, performed alone or combined with resistance training, improves Minnesota Living with Heart Failure Questionnaire (MLHFQ) total score (an index of patient-reported quality of life) by 9.1 points compared to usual care controls. A closer examination of the individual components that encompass qualify of life in HF according to the MLHFQ and 36-item Short-Form Survey (SF-36) demonstrate that overall improvements in quality of life following exercise training are driven in large part by improvements in physical, but not mental or emotional, dimensions of quality of life in HFpEF.4 Given the improvements in exercise tolerance and functional capacity that accompany exercise training, it is not surprising that the physical dimensions of quality of life consistently improve in HFpEF. However, it is currently unclear why there is no change in mental or emotional dimensions in quality of life following exercise training in this patient population.
APPLICATIONS TO PRACTICE
Criteria for Inclusion in Exercise-Based Cardiac Rehabilitation
Supervised exercise-based CR is recommended for all clinically stable patients with HF and New York Heart Association (NYHA) functional class I – III.74,75 Clinical stability is defined as no change NYHA functional class, no hospitalizations for HF, and no major cardiovascular events, or procedures during the prior 6 wk.74,75 Once clinically stability is established, the patient should undergo further screening to determine any contraindications to exercise training based on medical history, clinical examination, electrocardiography, echocardiography, and symptom-limited cardiopulmonary exercise test (CPX).74,75 A full list of contraindications to exercise testing and training for HF patients can be found in Piepoli et al.75 In particular, CR health care professionals should pay particularly close attention to: large recent weight gain (>1.8 kg over the previous 1-3 d), progressive worsening of exercise tolerance or dyspnea at rest over previous 3-5 d, NYHA functional class IV, supine resting HR >100 bpm, decrease in systolic blood pressure during exercise, significant ischemia or complex ventricular arrhythmia presenting during low-intensity exercise, or presence of pre-existing co-morbidities that may limit exercise tolerance and patient safety.
Cardiac Rehabilitation Exercise Training Guidelines
In clinically stable HFpEF patients who do not meet any of the aforementioned contraindications to exercise training, large muscle mass (cycling, walking) endurance exercise is recommended for 45 to 60 min, 3 to 5 d/wk at a moderate to high-intensity to improve VO2peak.74,75 Endurance training intensity can be prescribed based on maximal heart rate reserve (HRR), percentage of VO2peak, or rating of perceived exertion (RPE). In patients who have undergone a maximal CPX, the initial training intensity in the first few training sessions is 40-50% of VO2peak and should progressively increase to 70-80% of VO2peak after several weeks of training as training adaptations and improved exercise tolerance occur.75 Alternatively, if peak HR is measured, the recommended training intensity is 40-70% of HRR, calculated as HRR = 40% to 70% (peak HR ‒ resting HR) + (resting HR).75 While exercise prescription based on VO2peak or peak HR are preferred, in instances where VO2peak or peak HR are either not measured, are unattainable, or unreliable (e.g. ß-blockade), the training intensity can be prescribed based on the Borg RPE scale (range: 10-14 out of 20).
While the number of studies that have assessed the efficacy and safety of HIIT in HFpEF patients is limited,52,54 several recent reviews provide guidelines for implementation and monitoring of HIIT in clinical populations.74,76,77 Based on these guidelines, HIIT should consist of large muscle mass (cycling, walking) high-intensity intervals (10-20 min of high interval time) interspersed with periods of active recovery for a total of 25-35 min of exercise on 3 d/wk. The high-intensity intervals can consist of either short duration intervals (15-60 s of exercise at 80-100 peak power output followed by 15-60 sec periods of active or passive recovery) or longer-duration intervals (4 min of exercise at 90-95% peak HR followed by 3 min of active recovery at 50-70% peak HR). HFpEF patients should begin an exercise training program with shorter-duration intervals and gradually increase exercise interval duration as exercise tolerance improves. If there is difficulty obtaining a reliable or meaningful exercise-related HR during intervals, the intensity can be determined using RPE (training goal 15-18 out of 20 for high-intensity intervals) to ensure that HFpEF patients are meeting HIIT intensity goals.77 Furthermore, those implementing and monitoring exercise training should strive to keep HR and RPE within these recommended target zones and increase workload (e.g. speed/incline on treadmill or watts on bike) to account for training adaptations over time.77 Finally, a brief (3-5 min) light to moderate-intensity warm-up and cool-down is recommended prior to and following each continuous endurance or HIIT session.
As outlined earlier, HFpEF patients exhibit abnormalities in both skeletal muscle quantity and quality, with a reduced percentage of lean mass and greater intramuscular adipose to skeletal muscle area that contribute to poor exercise tolerance and physical function.43,45,78 As such, resistance training is an effective mode of training to improve muscle strength, quality (composition), and physical function in HF patients.55,79 The optimal intensity of resistance training is dependent on the patient’s training goals. If the goal is improve muscular endurance, lower intensity (30-40% 1-RM, 10-25 repetitions) upper and lower extremity resistance exercises should be performed on 2-3 d/wk.75 If the goal is to improve muscular strength, the intensity of training should be higher (40-60% 1-RM, 8-15 repetitions) on 2-3 d/wk.75 However, it should be noted that resistance training studies performed in physically frail elderly individuals80 and elderly patients with HFrEF79 suggest that an intensity of 80% of 1-RM may be required to achieve optimal strength gains in elderly populations. To ensure patient safety and appropriate muscular strength progression, a lower intensity should be incorporated initially with gradual increases in intensity over time to prevent skeletal muscle injury and maximize adaptations in skeletal muscle.
Safety of Exercise Training in HFpEF
A recent meta-analysis by Dieberg et al.13 that included 7 exercise training intervention studies (performed primarily in a CR setting) with 258 HFpEF patients reported no deaths directly attributable to exercise training in 3,744 h of exercise training. This suggests that the risk of a fatal or adverse event occurring during exercise training is very low in a supervised CR setting. Finally, by ensuring that HFpEF patients are clinically stable and free of contraindications to exercise training as outlined in this paper and others,74,75 CR specialists can greatly limit the risk of adverse events occurring during training.
Future Directions
As outlined in this review, numerous studies have shown that exercise training is a safe and effective non-pharmacological therapy to improve exercise tolerance, aerobic endurance, and quality of life in HFpEF. However, in the absence of data regarding the effect of exercise training on clinical events, Medicare and Medicaid currently do not reimburse for exercise-based CR in patients with HFpEF, despite covering those with HFrEF.81 As such, future large scale, multicenter exercise-based CR trials are needed to establish the efficacy of exercise training to improve survival outcomes and rate of hospitalizations in HFpEF. In addition, future research is warranted to establish whether exercise training performed outside of a medically monitored, non-supervised setting is safe and efficacious in patients with HFpEF.
SUMMARY
HFpEF patients exhibit severe exercise intolerance secondary to cardiac, vascular, and skeletal muscle abnormalities. Randomized controlled exercise intervention trials performed to date demonstrate that moderate to high-intensity endurance training alone or combined with resistance training is efficacious for increasing VO2peak, aerobic endurance, and quality of life in patients with HFpEF. Evidence to date suggests that the improvements in VO2peak are secondary to peripheral ‘non-cardiac’ factors that result in increased O2 extraction by the exercising muscles. Novel exercise (high-intensity interval training) interventions have also been shown to improve VO2peak in HFpEF. Large muscle mass (cycling, walking) endurance continuous exercise is recommended for 45 to 60 min on 3 to 5 d/wk at a moderate to high intensity (40-70% VO2peak). High-intensity interval training should consist of large muscle mass (cycling, walking) high-intensity (80-100% peak power output, 90-95% peak HR, 15-18 RPE on Borg 20-point Scale) intervals (10-20 min of high interval time) interspersed with periods of active recovery for a total of 25-35 min of exercise training on 3 d/wk. Resistance training can be supplemented to improve muscular strength, quality (composition), and physical function, with intensity being prescribed based on the goals of the patient.
Acknowledgments
Funding Information: Dr. Tucker was financially supported by the American Heart Association (AHA) Postdoctoral Fellowship Grant (AHA Award Number: 18POST33990210). Dr. Haykowsky is financially supported by the Moritz Chair in Geriatrics at the University of Texas at Arlington. Drs. Haykowsky, Nelson and Sarma are financially supported by National Institutes of Health (NIH) grant: P01 HL137630-01. Dr. Tomczak is financially supported by the Saskatchewan Health Research Foundation and the Heart and Stroke Foundation. All other authors have no disclosures of funding.
Footnotes
Conflict of Interest: All authors declare no conflicts of interest.
REFERENCES
- 1.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56–e528. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–944. [DOI] [PubMed] [Google Scholar]
- 3.Gottdiener JS, McClelland RL, Marshall R, et al. Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med. 2002;137(8):631–639. [DOI] [PubMed] [Google Scholar]
- 4.Fukuta H, Goto T, Wakami K, Kamiya T, Ohte N. Effects of exercise training on cardiac function, exercise capacity, and quality of life in heart failure with preserved ejection fraction: a meta-analysis of randomized controlled trials. Heart Fail Rev. 2019. [DOI] [PubMed] [Google Scholar]
- 5.Haykowsky MJ, Brubaker PH, Morgan TM, Kritchevsky S, Eggebeen J, Kitzman DW. Impaired aerobic capacity and physical functional performance in older heart failure patients with preserved ejection fraction: role of lean body mass. J Gerontol A Biol Sci Med Sci. 2013;68(8):968–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nadruz W Jr., West E, Sengelov M, et al. Prognostic Value of Cardiopulmonary Exercise Testing in Heart Failure With Reduced, Midrange, and Preserved Ejection Fraction. J Am Heart Assoc. 2017;6(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orimoloye OA, Kambhampati S, Hicks AJ 3rd, , et al. Higher cardiorespiratory fitness predicts long-term survival in patients with heart failure and preserved ejection fraction: the Henry Ford Exercise Testing (FIT) Project. Arch Med Sci. 2019;15(2):350–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borlaug BA. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2014;11(9):507–515. [DOI] [PubMed] [Google Scholar]
- 9.Del Buono MG, Arena R, Borlaug BA, et al. Exercise Intolerance in Patients With Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73(17):2209–2225. [DOI] [PubMed] [Google Scholar]
- 10.Fukuta H, Goto T, Wakami K, Ohte N. Effects of drug and exercise intervention on functional capacity and quality of life in heart failure with preserved ejection fraction: A meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2016;23(1):78–85. [DOI] [PubMed] [Google Scholar]
- 11.Kitzman DW. Exercise training in heart failure with preserved ejection fraction: beyond proof-of-concept. J Am Coll Cardiol. 2011;58(17):1792–1794. [DOI] [PubMed] [Google Scholar]
- 12.Tucker WJ, Nelson MD, Beaudry RI, et al. Impact of Exercise Training on Peak Oxygen Uptake and its Determinants in Heart Failure with Preserved Ejection Fraction. Card Fail Rev. 2016;2(2):95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dieberg G, Ismail H, Giallauria F, Smart NA. Clinical outcomes and cardiovascular responses to exercise training in heart failure patients with preserved ejection fraction: a systematic review and meta-analysis. J Appl Physiol. 2015;119(6):726–733. [DOI] [PubMed] [Google Scholar]
- 14.Pandey A, Parashar A, Kumbhani D, et al. Exercise training in patients with heart failure and preserved ejection fraction: meta-analysis of randomized control trials. Circ Heart Fail. 2015;8(1):33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abudiab MM, Redfield MM, Melenovsky V, et al. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail. 2013;15(7):776–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhakal BP, Malhotra R, Murphy RM, et al. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: the role of abnormal peripheral oxygen extraction. Circ Heart Fail. 2015;8(2):286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haykowsky MJ, Brubaker PH, John JM, Stewart KP, Morgan TM, Kitzman DW. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. J Am Coll Cardiol. 2011;58(3):265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kitzman DW, Higginbotham MB, Cobb FR, Sheikh KH, Sullivan MJ. Exercise intolerance in patients with heart failure and preserved left ventricular systolic function: failure of the Frank-Starling mechanism. J Am Coll Cardiol. 1991;17(5):1065–1072. [DOI] [PubMed] [Google Scholar]
- 19.Borlaug BA, Melenovsky V, Russell SD, et al. Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circulation. 2006;114(20):2138–2147. [DOI] [PubMed] [Google Scholar]
- 20.Borlaug BA, Olson TP, Lam CS, et al. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2010;56(11):845–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phan TT, Shivu GN, Abozguia K, et al. Impaired heart rate recovery and chronotropic incompetence in patients with heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3(1):29–34. [DOI] [PubMed] [Google Scholar]
- 22.Nonogi H, Hess OM, Ritter M, Krayenbuehl HP. Diastolic properties of the normal left ventricle during supine exercise. Br Heart J. 1988;60(1):30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borlaug BA, Jaber WA, Ommen SR, Lam CS, Redfield MM, Nishimura RA. Diastolic relaxation and compliance reserve during dynamic exercise in heart failure with preserved ejection fraction. Heart. 2011;97(12):964–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borlaug BA. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction. Circ J. 2014;78(1):20–32. [DOI] [PubMed] [Google Scholar]
- 25.Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3(5):588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Obokata M, Olson TP, Reddy YNV, Melenovsky V, Kane GC, Borlaug BA. Haemodynamics, dyspnoea, and pulmonary reserve in heart failure with preserved ejection fraction. Eur Heart J. 2018;39(30):2810–2821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hundley WG, Kitzman DW, Morgan TM, et al. Cardiac cycle-dependent changes in aortic area and distensibility are reduced in older patients with isolated diastolic heart failure and correlate with exercise intolerance. J Am Coll Cardiol. 2001;38(3):796–802. [DOI] [PubMed] [Google Scholar]
- 28.Kitzman DW, Herrington DM, Brubaker PH, Moore JB, Eggebeen J, Haykowsky MJ. Carotid arterial stiffness and its relationship to exercise intolerance in older patients with heart failure and preserved ejection fraction. Hypertension. 2013;61(1):112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee JF, Barrett-O’Keefe Z, Nelson AD, et al. Impaired skeletal muscle vasodilation during exercise in heart failure with preserved ejection fraction. Int J Cardiol. 2016;211:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thompson RB, Pagano JJ, Mathewson KW, et al. Differential Responses of Post-Exercise Recovery of Leg Blood Flow and Oxygen Uptake Kinetics in HFpEF versus HFrEF. PLoS One. 2016;11(10):e0163513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thompson RB, Tomczak CR, Haykowsky MJ. Evaluation of Cardiac, Vascular, and Skeletal Muscle Function With MRI: Novel Physiological End Points in Cardiac Rehabilitation Research. Can J Cardiol. 2016;32(10 Suppl 2):S388–s396. [DOI] [PubMed] [Google Scholar]
- 32.Kishimoto S, Kajikawa M, Maruhashi T, et al. Endothelial dysfunction and abnormal vascular structure are simultaneously present in patients with heart failure with preserved ejection fraction. Int J Cardiol. 2017;231:181–187. [DOI] [PubMed] [Google Scholar]
- 33.Marechaux S, Samson R, van Belle E, et al. Vascular and Microvascular Endothelial Function in Heart Failure With Preserved Ejection Fraction. J Card Fail. 2016;22(1):3–11. [DOI] [PubMed] [Google Scholar]
- 34.Hundley WG, Bayram E, Hamilton CA, et al. Leg flow-mediated arterial dilation in elderly patients with heart failure and normal left ventricular ejection fraction. Am J Physiol Heart Circ Physiol. 2007;292(3):H1427–1434. [DOI] [PubMed] [Google Scholar]
- 35.Kitzman DW, Haykowsky MJ. Vascular Dysfunction in Heart Failure with Preserved Ejection Fraction. J Card Fail. 2016;22(1):12–16. [DOI] [PubMed] [Google Scholar]
- 36.Lee JF, Barrett-O’Keefe Z, Garten RS, et al. Evidence of microvascular dysfunction in heart failure with preserved ejection fraction. Heart. 2016;102(4):278–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosenberry R, Munson M, Chung S, et al. Age-related microvascular dysfunction: novel insight from near-infrared spectroscopy. Exp Physiol. 2018;103(2):190–200. [DOI] [PubMed] [Google Scholar]
- 38.Balmain S, Padmanabhan N, Ferrell WR, Morton JJ, McMurray JJ. Differences in arterial compliance, microvascular function and venous capacitance between patients with heart failure and either preserved or reduced left ventricular systolic function. Eur J Heart Fail. 2007;9(9):865–871. [DOI] [PubMed] [Google Scholar]
- 39.Boyes NG, Eckstein J, Pylypchuk S, et al. Effects of heavy-intensity priming exercise on pulmonary oxygen uptake kinetics and muscle oxygenation in heart failure with preserved ejection fraction. Am J Physiol Regul Integr Comp Physiol. 2019;316(3):R199–r209. [DOI] [PubMed] [Google Scholar]
- 40.DeLorey DS, Kowalchuk JM, Paterson DH. Effects of prior heavy-intensity exercise on pulmonary O2 uptake and muscle deoxygenation kinetics in young and older adult humans. J Appl Physiol. 2004;97(3):998–1005. [DOI] [PubMed] [Google Scholar]
- 41.Tucker WJ, Rosenberry R, Trojacek D, et al. Studies into the determinants of skeletal muscle oxygen consumption: novel insight from near-infrared diffuse correlation spectroscopy. J Physiol. 2019;597(11):2887–2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Upadhya B, Haykowsky MJ, Eggebeen J, Kitzman DW. Exercise intolerance in heart failure with preserved ejection fraction: more than a heart problem. J Geriatr Cardiol. 2015;12(3):294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tucker WJ, Haykowsky MJ, Seo Y, Stehling E, Forman DE. Impaired Exercise Tolerance in Heart Failure: Role of Skeletal Muscle Morphology and Function. Curr Heart Fail Rep. 2018;15(6):323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Houstis NE, Eisman AS, Pappagianopoulos PP, et al. Exercise Intolerance in Heart Failure With Preserved Ejection Fraction: Diagnosing and Ranking Its Causes Using Personalized O2 Pathway Analysis. Circulation. 2018;137(2):148–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haykowsky MJ, Kouba EJ, Brubaker PH, Nicklas BJ, Eggebeen J, Kitzman DW. Skeletal muscle composition and its relation to exercise intolerance in older patients with heart failure and preserved ejection fraction. Am J Cardiol. 2014;113(7):1211–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Molina AJ, Bharadwaj MS, Van Horn C, et al. Skeletal Muscle Mitochondrial Content, Oxidative Capacity, and Mfn2 Expression Are Reduced in Older Patients With Heart Failure and Preserved Ejection Fraction and Are Related to Exercise Intolerance. JACC Heart Fail. 2016;4(8):636–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kitzman DW, Nicklas B, Kraus WE, et al. Skeletal muscle abnormalities and exercise intolerance in older patients with heart failure and preserved ejection fraction. Am J Physiol Heart Circ Physiol. 2014;306(9):H1364–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hales KG. The machinery of mitochondrial fusion, division, and distribution, and emerging connections to apoptosis. Mitochondrion. 2004;4(4):285–308. [DOI] [PubMed] [Google Scholar]
- 49.Benard G, Karbowski M. Mitochondrial fusion and division: Regulation and role in cell viability. Semin Cell Dev Biol. 2009;20(3):365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bhella PS, Prasad A, Heinicke K, et al. Abnormal haemodynamic response to exercise in heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13(12):1296–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weiss K, Schar M, Panjrath GS, et al. Fatigability, Exercise Intolerance, and Abnormal Skeletal Muscle Energetics in Heart Failure. Circ Heart Fail. 2017;10(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fu TC, Yang NI, Wang CH, et al. Aerobic Interval Training Elicits Different Hemodynamic Adaptations Between Heart Failure Patients with Preserved and Reduced Ejection Fraction. Am J Phys Med Rehabil. 2016;95(1):15–27. [DOI] [PubMed] [Google Scholar]
- 53.Haykowsky MJ, Brubaker PH, Stewart KP, Morgan TM, Eggebeen J, Kitzman DW. Effect of endurance training on the determinants of peak exercise oxygen consumption in elderly patients with stable compensated heart failure and preserved ejection fraction. J Am Coll Cardiol. 2012;60(2):120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Angadi SS, Mookadam F, Lee CD, Tucker WJ, Haykowsky MJ, Gaesser GA. High-intensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: a pilot study. J Appl Physiol. 2015;119(6):753–758. [DOI] [PubMed] [Google Scholar]
- 55.Edelmann F, Gelbrich G, Dungen HD, et al. Exercise training improves exercise capacity and diastolic function in patients with heart failure with preserved ejection fraction: results of the Ex-DHF (Exercise training in Diastolic Heart Failure) pilot study. J Am Coll Cardiol. 2011;58(17):1780–1791. [DOI] [PubMed] [Google Scholar]
- 56.Kitzman DW, Brubaker P, Morgan T, et al. Effect of Caloric Restriction or Aerobic Exercise Training on Peak Oxygen Consumption and Quality of Life in Obese Older Patients With Heart Failure With Preserved Ejection Fraction: A Randomized Clinical Trial. Jama. 2016;315(1):36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kitzman DW, Brubaker PH, Herrington DM, et al. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. J Am Coll Cardiol. 2013;62(7):584–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kitzman DW, Brubaker PH, Morgan TM, Stewart KP, Little WC. Exercise training in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. Circ Heart Fail. 2010;3(6):659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smart NA, Haluska B, Jeffriess L, Leung D. Exercise training in heart failure with preserved systolic function: a randomized controlled trial of the effects on cardiac function and functional capacity. Congest Heart Fail. 2012;18(6):295–301. [DOI] [PubMed] [Google Scholar]
- 60.Fujimoto N, Prasad A, Hastings JL, et al. Cardiovascular effects of 1 year of progressive endurance exercise training in patients with heart failure with preserved ejection fraction. Am Heart J. 2012;164(6):869–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. 2012;590(5):1077–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Weston KS, Wisloff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227–1234. [DOI] [PubMed] [Google Scholar]
- 63.Suchy C, Massen L, Rognmo O, et al. Optimising exercise training in prevention and treatment of diastolic heart failure (OptimEx-CLIN): rationale and design of a prospective, randomised, controlled trial. Eur J Prev Cardiol. 2014;21(2 Suppl):18–25. [DOI] [PubMed] [Google Scholar]
- 64.Obokata M, Reddy YNV, Pislaru SV, Melenovsky V, Borlaug BA. Evidence Supporting the Existence of a Distinct Obese Phenotype of Heart Failure With Preserved Ejection Fraction. Circulation. 2017;136(1):6–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shah SJ, Kitzman DW, Borlaug BA, et al. Phenotype-Specific Treatment of Heart Failure With Preserved Ejection Fraction: A Multiorgan Roadmap. Circulation. 2016;134(1):73–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Upadhya B, Kitzman DW. Heart Failure with Preserved Ejection Fraction in Older Adults. Heart Fail Clin. 2017;13(3):485–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Haass M, Kitzman DW, Anand IS, et al. Body mass index and adverse cardiovascular outcomes in heart failure patients with preserved ejection fraction: results from the Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circ Heart Fail. 2011;4(3):324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Beavers KM, Miller ME, Rejeski WJ, Nicklas BJ, Kritchevsky SB. Fat mass loss predicts gain in physical function with intentional weight loss in older adults. J Gerontol A Biol Sci Med Sci. 2013;68(1):80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.de las Fuentes L, Waggoner AD, Mohammed BS, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009;54(25):2376–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Haufe S, Utz W, Engeli S, et al. Left ventricular mass and function with reduced-fat or reduced-carbohydrate hypocaloric diets in overweight and obese subjects. Hypertension. 2012;59(1):70–75. [DOI] [PubMed] [Google Scholar]
- 71.Prior SJ, Blumenthal JB, Katzel LI, Goldberg AP, Ryan AS. Increased skeletal muscle capillarization after aerobic exercise training and weight loss improves insulin sensitivity in adults with IGT. Diabetes Care. 2014;37(5):1469–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Villareal DT, Chode S, Parimi N, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364(13):1218–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776–803. [DOI] [PubMed] [Google Scholar]
- 74.Haykowsky MJ, Daniel KM, Bhella PS, Sarma S, Kitzman DW. Heart Failure: Exercise-Based Cardiac Rehabilitation: Who, When, and How Intense? Can J Cardiol. 2016;32(10 Suppl 2):S382–s387. [DOI] [PubMed] [Google Scholar]
- 75.Piepoli MF, Conraads V, Corra U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13(4):347–357. [DOI] [PubMed] [Google Scholar]
- 76.Karlsen T, Aamot IL, Haykowsky M, Rognmo O. High Intensity Interval Training for Maximizing Health Outcomes. Prog Cardiovasc Dis. 2017;60(1):67–77. [DOI] [PubMed] [Google Scholar]
- 77.Taylor JL, Holland DJ, Spathis JG, et al. Guidelines for the delivery and monitoring of high intensity interval training in clinical populations. Prog Cardiovasc Dis. 2019;62(2):140–146. [DOI] [PubMed] [Google Scholar]
- 78.Kinugasa Y, Yamamoto K. The challenge of frailty and sarcopenia in heart failure with preserved ejection fraction. Heart. 2017;103(3):184–189. [DOI] [PubMed] [Google Scholar]
- 79.Pu CT, Johnson MT, Forman DE, et al. Randomized trial of progressive resistance training to counteract the myopathy of chronic heart failure. J Appl Physiol. 2001;90(6):2341–2350. [DOI] [PubMed] [Google Scholar]
- 80.Fiatarone MA, O’Neill EF, Ryan ND, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330(25):1769–1775. [DOI] [PubMed] [Google Scholar]
- 81.Upadhya B, Haykowsky MJ, Kitzman DW. Therapy for heart failure with preserved ejection fraction: current status, unique challenges, and future directions. Heart Fail Rev. 2018;23(5):609–629. [DOI] [PMC free article] [PubMed] [Google Scholar]