Abstract
Objective:
Mental illness stigmatization has harmful effects on recovery from serious mental illness (SMI). Experiencing prejudice and discrimination can lead to internalized stigma (i.e. the cognitive and emotional internalization of negative stereotypes and application of those stereotypes to the self). Internalized stigma may lead to decrements in self-esteem and self-efficacy, negatively affecting recovery. However, to date no study has examined the effects of stigma experiences on recovery-related outcomes serially through internalized stigma, self-esteem, and self-efficacy in a single comprehensive model. The present study sought to address this gap.
Methods:
During baseline assessments for two randomized controlled trials, adults with SMI (N = 516) completed standardized measures assessing the variables of interest. In a secondary analysis of these data, separate serial mediation models were tested for recovery orientation, perceived quality of life, and social withdrawal as outcomes. Experiences of stigma was entered as the predictor variable, and internalized stigma, self-esteem, and self-efficacy as serial mediators, in that order. Competing models with alternate orders, as well as parallel mediation models, were also tested to evaluate directionality.
Results:
Our hypothesized serial mediation model was the best fit, though self-efficacy was not found to be a critical mediator. Experiences of stigma led to internalized stigma, which influenced self-esteem, and recovery-related outcomes consistent with the social-cognitive model of internalized stigma.
Conclusions and Implications for Practice:
Internalized stigma is an essential target for intervention. Treatments that omit it as an explicit target and only address downstream effects of stigma experiences (e.g., self-esteem), may not be effective.
Keywords: Stigma, Serious mental illness, Recovery, Self-esteem, Self-efficacy
Serious mental illness (SMI) is among the leading causes of disability in the United States (Office of Disease Prevention and Health Promotion, 2016), affecting over 10 million individuals in 2016 (National Institute of Mental Health, 2017). In recent decades, the goals of SMI treatment have broadened from symptom reduction and clinical stabilization to a conceptualization of recovery focused on overall wellness and self-direction (Bellack, 2006; Substance Abuse and Mental Health Services Administration [SAMHSA], 2012). Recovery is conceptualized as a process of developing self-efficacy, hope, illness management, life meaning, and empowerment skills (Bellack, 2006). This shift to the recovery paradigm has been linked to numerous improvements in health, treatment, and quality of life outcomes for individuals with SMI (Green et al., 2013; Resnick, Rosenheck, & Lehman, 2004).
However, the stigmatization of mental illness persists and has widespread harmful effects on individuals’ recovery (Link, Struening, Neese-Todd, Asmussen, & Phelan, 2001). Experiencing any societal prejudice and discrimination (e.g., due to sexism, racism, other marginalized identities) is stressful and can lead to social withdrawal, reduced goal-striving persistence, demoralization, and anger (e.g., Hartshorn, Whitbeck, & Hoyt, 2012; Newcomb & Mustanski, 2010; Sue, 2010), and can also erode one’s self-esteem and perceived well-being (e.g., American Psychological Association, 2016; Crocker & Quinn, 2000; Link et al., 2001). Further, stigma exposure can lead to internalizing the prejudicial messages, which compounds the harms of experiencing societal stigma (Corrigan, Watson, & Barr, 2006).
Internalization is the process of “absorbing” social messages into one’s thinking about one’s self. In the case of mental illness stigmatization, it means perceiving prejudiced assumptions or judgments about people with mental illness as at least sometimes accurate and as pertaining to one’s self. The social-cognitive model of internalized stigma is the prevailing model that elucidates this into a specific process (Corrigan, Rafacz, & Rusch, 2011; Corrigan et al., 2006; Watson, Corrigan, Larson, & Sells, 2007). It posits that (1) people tend to be aware of negative stereotypes about mental illness as a matter of constant exposure in society, and that (2) people tend to tacitly accept at least some of them as legitimate due to frequent exposure. Then, for many, the social category of “person with a mental illness” becomes personally relevant at some point (e.g., through personal categorization, professional diagnosis, mental health service use, hospitalization). This heightened personal relevance of the identity and the associated stigma leads to (3) applying the stigma messages or stereotypes to one’s self. The extent to which this happens can depend on how legitimate the person perceives the stereotypes to be and on how strongly a person’s self-concept counters the prejudicial messages. How and the extent to which a person applies stigma to the self then determines (4) the degree to which self-esteem is reduced or harmed by the process.
Thus, internalized stigma, self-esteem, and self-efficacy are highly correlated elements through which many of the person-level harms of societal stigma occur. Internalized stigma involves decreased self-esteem and is often accompanied by self-blame (Corrigan et al., 2006; Corrigan, Watson, & Miller, 2006; Corrigan et al., 2011), as well as poorer social functioning and reduced empowerment (Livingston & Boyd, 2010; Lysaker, Roe, & Yanos, 2007). The social-cognitive model of internalized stigma (e.g., Corrigan et al., 2006; Watson et al., 2007) suggests directionality among these variables: that changes in internalized stigma may precede changes in self-esteem and self-efficacy, and recovery-related outcomes (e.g., Mashiach-Eizenberg, Hasson-Ohayon, Yanos, Lysaker, & Roe, 2013; Vauth, Kleim, Wirtz, & Corrigan, 2007; Yanos, Roe, Markus, & Lysaker, 2008). Given the linear steps posited in the social-cognitive model of internalized stigma (Corrigan et al., 2011; Corrigan et al., 2006; Watson et al., 2007), examining the factors in more complex models is critical. Hill and Startup (2013) found internalized stigma to be strongly negatively correlated with self-efficacy and social functioning among individuals hospitalized with schizophrenia. However, they found no evidence that self-efficacy mediated the relationship between internalized stigma and social functioning. In a broader sample of adults with SMI, Mashiach-Eizenberg and colleagues (2013) found that self-esteem mediated the relationship between internalized stigma and hope.
Among people with schizophrenia, Vauth and colleagues (2007) found that avoidant coping styles (a common effect of aversive stigma experiences) were a risk factor for internalized stigma, which in turn, eroded self-efficacy and empowerment, leading to increased depression and reduced quality of life. Livingston and Boyd’s (2010) meta-analysis of 45 studies of internalized stigma emphasized its consistent negative correlations with a range of recovery-oriented psychosocial variables (e.g., hope, self-esteem, self-efficacy, empowerment, quality of life, and social support). This meta-analysis and similar studies (e.g., Link et al., 2001) strongly suggest that social and structural stigma negatively affect individuals’ recovery at least in part through internalized stigma and its decrements to self-esteem and self-efficacy.
Therefore, it is likely that internalized stigma, self-esteem, and self-efficacy are important mediators of the relationship between experiences of stigma and recovery. However, these causal pathways are far from proven. For example, Munoz, Sanz, Perez-Santos, and de los Angeles Quiroga (2011) found that self-efficacy, self-esteem, and empowerment were not significantly associated with internalized stigma.
To date, no sizeable analysis has included all of these variables (i.e., social stigma, internalized stigma, self-esteem, self-efficacy, and recovery-related outcomes) to examine the sequential effects of the variables on each other, perhaps providing avenues for improving recovery outcomes. For example, if experiences of stigma lead to internalized stigma which then influences self-esteem and recovery orientation, then interventions designed to increase self-esteem without first addressing experiences of stigma and internalized stigma may not be optimally effective. Additionally, a single comprehensive model, rather than piecemeal models of a few variables, would help clarify pathways of interrelationship and determine variables’ relative importance and mutual influences. Therefore, examining all of these variables in a single analysis could beneficially inform intervention development and provide guidance for future studies testing the directionality of these effects.
Accordingly, the aim of this secondary analysis was to create and test a serial mediation model, using cross-sectional data, and to then test competing models to further evaluate directionality of the paths (see Figure 1 for illustration of hypothesis). We hypothesized that:
Figure 1.
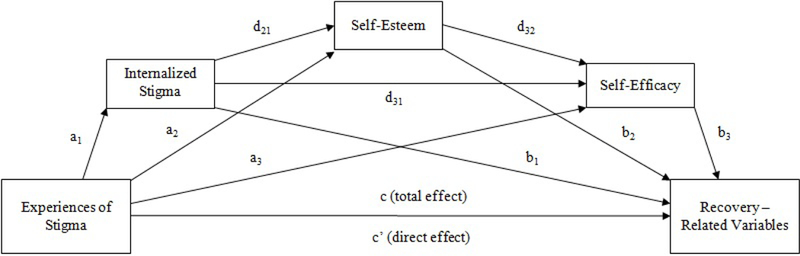
Paths of the serial multiple mediation model with internalized stigma, self-esteem, and self-efficacy as proposed mediators of the effect of experience of stigma on recovery related variables (i.e., recovery orientation, quality of life, social withdrawal).
Internalized stigma, self-esteem, and self-efficacy would serially mediate the relationship between experiences of stigma and recovery orientation (paths a1 → d21 → d32 → b3).
Internalized stigma, self-esteem, and self-efficacy would serially mediate the relationship between experiences of stigma and perceived quality of life (paths a1 → d21 → d32 → b3).
Internalized stigma, self-esteem, and self-efficacy would serially mediate the relationship between experiences of stigma and social withdrawal (paths a1 → d21 → d32 → b3).
Competing models in which the order of mediators was reversed would not be significant (e.g., paths a2 → d32 → d31 → b1, paths a3 → d32 → d21 → b1).
Models in which mediators were assessed in parallel, as opposed to serially, would not be significant.
Methods
Participants
Baseline assessment data from two randomized controlled trials (RCTs) of a psychosocial intervention aimed at reducing internalized stigma and its effects among adults with SMI (Blinded for review, 2016) were used for the present study. Only baseline data were used as randomization of participants and the intervention influenced variables of interest; this secondary data analysis was designed to elucidate paths among these variables, not assess effects of the intervention. Therefore, data from time points beyond baseline could not be utilized. Participants (N = 516) were recruited from five Maryland community-based psychosocial rehabilitation programs and mental health clinics/programs in three large Veterans Affairs (VA) medical centers. Participants were mostly male (73.3%), African-American (51.9%) or Caucasian (39.3%), unmarried (89.1%), and unemployed (92.6%). The mean age of participants was 48.9 years (SD = 11.7). Most had at least a high school education (80.4%) and approximately half were residing in a supervised living facility (45.8%). Psychiatric diagnoses included: bipolar disorder (34.2%), schizophrenia (28.1%), schizoaffective disorder (23.7%), major depressive disorder with psychosis (6.5%), major depressive disorder without psychosis (4.5%), and other psychosis (2.2%). Just over half of the participants were Veterans (50.4%; 247 from VA sites,13 from community sites).
Procedures
Participants were recruited through clinician referrals, recruitment flyers posted in participating clinics, and verbal invitation at program community meetings. At the VA sites, participants were also recruited from review of clinic and program rosters; a partial HIPAA waiver was obtained to allow review of charts to confirm eligibility. These individuals were then approached in-person at appointments or sent letters regarding the study. Eligible individuals for both studies were consenting clients between 18 and 80 (for VA) or 18 and 90 (for community) years of age who were willing and able to participate in all aspects of the study. At the VA sites, eligibility criteria also included a chart diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, or major depression with psychotic features. In the community study, participants were recruited from programs that serve adults meeting Maryland’s “severely mentally ill priority population” definition, which requires a diagnosis of schizophrenia, bipolar disorder, recurrent major depressive disorder, schizotypal or borderline personality disorder, or another delusional or psychotic disorder, with documented functional impairments (Beacon Health Options, 2016). Exclusion criteria at both sites included a documented history of severe or profound intellectual developmental disorder. All participants provided written informed consent. Baseline assessments, lasting approximately 90 minutes, typically occurred immediately following consent. Study procedures for the two RCTs, as well as procedures to combine baseline data from the two RCTs, were approved by the appropriate institutional review boards.
Measures
Demographic and Clinical Characteristics:
Demographic information -- age, race/ethnicity, sex, education, living situation, marital status, and employment status -- was obtained from all participants. Mental health diagnosis was obtained from the participant’s clinical chart or medical record. Demographic information was used as a covariate.
Brief Symptom Inventory (BSI; Derogatis, 1993):
Self-reported psychiatric symptoms were measured using the BSI, a multidimensional symptom inventory derived from the Symptom Checklist-90-Revised (Derogatis, 1993). Participants rate how distressed they have been by each of 53 symptoms over the past 7 days using a 5-point scale ranging from “Not at All” to “Extremely.” The measure provides standardized t-scores on nine symptom dimensions (e.g., psychotic symptoms, anxiety, depression), and three global indices of distress. For the present analyses, we used only the depression subscale, as a covariate; it had an internal consistency reliability of 0.85 in this sample.
Consumer Experiences of Stigma Questionnaire (CESQ; Dickerson, Sommerville, Origoni, Ringel, & Parente, 2002; Wahl, 1999):
The CESQ is used to measure self-reported experiences of social stigma and discrimination associated with mental illness, and was included as the predictor variable in all models. Participants indicate the degree to which they have experienced each of the 20 concerns about or experiences of stigma-related disrespect (9 items) or outright discrimination (11 items) due to having a mental illness or using mental health services. Items are rated on a 5-point scale, from “Never” to “Very often”; and then summed for each subscale score. We used only the 9-item Experiences of Stigma-Related Disrespect subscale total score (CES-QS) for the present analyses. We chose this over the full CESQ (20 item) total because the Discrimination subscale’s very specific items (e.g., discrimination in legal proceedings, denial of passport or permits) do not pertain to many participants. Therefore, the CES-QS provides a more accurate global score of stigma experiences. Example items include, “I have been treated as less competent by others when they learned I am a consumer,” “I have seen or read things in the mass media (eg, tv, movies, books) about consumers and their illnesses that I found hurtful or offensive,” and “I have been shunned or avoided when it was revealed that I am a consumer.” Internal consistency reliability was acceptable (Cronbach’s α = 0.81).
Internalized Stigma of Mental Illness Inventory (ISMI; Ritsher, Otilingam, & Grajales, 2003):
The ISMI was used to measure internalized stigma, a hypothesized mediating variable in the model. Respondents indicate to what extent they agree with 29 statements, using a 4-point scale from “Strongly disagree” to “Strongly agree.” In addition to an overall score, the ISMI returns five subscale scores: Alienation, Stereotype Endorsement, Discrimination Experience, Social Withdrawal, and Stigma Resistance, each assessing different aspects of internalized stigma. The current analyses utilized the ISMI total score, excluding the Stigma Resistance subscale, which has previously been shown to be less psychometrically sound than the other subscales (Ritsher et al., 2003) Cronbach’s alpha for the total score (excluding Stigma Resistance subscale) was 0.90.
Self-Esteem Rating Scale–Short Form (SERS-SF; Nugent, 2004; Nugent & Thomas, 1993):
The SERS-Short Form is a 20-item self-report scale that measures self-esteem, a proposed mediator in the model. Participants are asked to rate items on a 7-point response scale ranging from “Never” to “Always”. Responses are summed to produce an overall score, with higher scores representing higher self-esteem. Internal consistency reliability was strong in this study (Cronbach’s α = 0.92).
General Self-Efficacy Scale (GSES; Chen, Gully, & Eden, 2001):
The GSES is an 8- item measure used to assess self-efficacy, the degree to which the respondent perceives himself or herself as capable of attaining goals, overcoming challenges, and performing well on tasks. Respondents rate items on a 5-point response scale from “Strongly disagree” to “Strongly agree”. Responses are averaged to produce an overall score, which was used as a mediator in the hypothesized models. The GSES has strong psychometric properties, performing favorably when compared to other measures of the same construct (Chen et al., 2001; Scherbaum, Cohen-Charash, & Kern, 2006). Cronbach’s alpha in the current sample was 0.89.
Maryland Assessment of Recovery in Serious Mental Illness Scale (MARS; Drapalski et al., 2012; Drapalski, Medoff, Dixon, & Bellack, 2016):
The MARS is a 25-item self-report measure of recovery in people with SMI. Recovery orientation was used as an outcome variable in the current analyses. Items are rated on a 5-point scale from “Not at all” to “Very much”. An overall score is calculated by summing item responses. The MARS has demonstrated excellent internal consistency and test-retest reliability, as well as strong validity (Drapalski et al., 2016). Cronbach’s alpha in the current sample was 0.95.
Brief Quality of Life Scale (BQOL: Lehman, 1995):
The BQOL assesses perceived quality of life in a number of domains. It consists of objective and subjective measures of 8 domains: living situation, daily activities and functioning, family relations, social relations, finances, work and school, legal and safety issues, and health status. In the current analyses, we used one item, “How do you feel about your life in general?” to measure perceived quality of life, an outcome variable in the models. Participants rated this item on a 7-point scale from “Terrible” to “Delighted”.
Social Functioning Scale (SFS; Birchwood, Smith, Cochrane, Wetton, & Copestake, 1990):
The SFS is a self-assessment of social functioning for individuals with SMI, covering five sub-domains: performance of daily living skills, social engagement/withdrawal, interpersonal communication, recreation, and prosocial behavior. In this study, we used the 5- item Social Engagement/Withdrawal subscale (SFS-SW) to assess social withdrawal as an outcome variable. Its items assess waking time on weekends and weekdays, time spent alone each day, frequency of initiating conversation at home, frequency of leaving home, and reactions to the presence of strangers. Higher scores indicate greater engagement (i.e., lower social withdrawal). All items were converted to a four-point response scale as the scale varies for each item and then summed to provide a final score. Due to the nature of the constituent items we did not calculate Cronbach’s alpha for the sample.
Data Analysis
Preliminary testing for univariate and multivariate outliers was performed prior to conducting analyses; univariate outliers were adjusted to within three standard deviations of the mean. No cases met criteria as multivariate outliers. We also screened for multicollinearity using variance inflation factors and found no evidence of multicollinearity among variables in the models. Serial mediation analyses, also referred to as multiple-step multiple mediation models (e.g., Hayes, Preacher, & Myers, 2011), were conducted using the PROCESS macro for SPSS, which is a bootstrapped regression-based model for assessing direct and indirect effects (Hayes, 2013). This procedure utilizes the product of path coefficients to calculate indirect effects and bootstraps estimates of the indirect effects to approximate the sampling distribution (Hayes, 2013). Though total and direct effects are also provided by this analysis, results are based on the indirect effects. Unlike older models of mediation, which require a significant total effect and then a reduction in significance for the direct effect when mediators are included, the product of path coefficients method of mediation does not require a significant total effect. Parameters were estimated with 5,000 bootstrap samples and 95% bias-corrected confidence intervals (CIs; Preacher & Hayes, 2008). If zero is not included in the CI, the indirect effect is considered statistically significant. The analysis provides estimates and tests not only of the hypothesized three mediator indirect path of the full serial mediation model (i.e., X→M1→M2→M3→Y), but also for each possible indirect path with one or two mediators (e.g., X→M1 →Y, X→M2→M3→Y). With three mediators, this results in seven potential indirect paths per analysis. We selected Hayes’ (2013) serial mediation approach over path analysis, a type of structural equation modeling without latent variables, due to sample size. Guidelines for path analysis recommend 10 to 20 participants per free parameter in the model (e.g., Kline, 1998); with the large number of parameters in the model, our sample size was not adequate to meet this.
For all analyses, age, sex, race, education level, depressive symptoms, and recruitment site type (VA or community-based) were included as covariates. Additionally, diagnosis was included as a covariate; one-way analyses of variance showed no significant differences in internalized stigma by diagnosis, F(6, 498) = 0.75, p = 0.613, but a significant difference in experiences of stigma by diagnosis, F(6, 493) = 2.16, p = 0.046. To test for serial mediation, recovery-related variables (i.e., recovery orientation, perceived quality of life, and social withdrawal) were entered as outcome variables in three separate models. In each model, experiences of stigma was entered as the predictor variable, and internalized stigma, self-esteem, and self-efficacy were entered as serial mediators in that order. All variables were standardized prior to inclusion in the model. The order of serial mediation was based on previous research regarding the directionality of effects among these variables and the social-cognitive model of internalized stigma (reviewed above). Ancillary analyses were conducted to test directionality by reversing the order of the mediating variables to test all possible orders (five additional models per outcome), as well as testing the mediators in parallel. These latter models provided critical tests of the hypothesized directionality among the mediating variables.
Results
Descriptive statistics and correlations are presented in Table 1. Coefficients for all paths for the full model are illustrated in Figures 2–4. The models, including all covariates and mediators, were significant for each outcome (i.e., recovery orientation, R2 = 0.61, F(11, 473) = 65.86, p < .001; perceived quality of life, R2 = 0.43, F(11, 473) = 32.04, p < .001; social withdrawal, R2 = 0.20, F(11, 431) = 9.65, p < .001). The indirect effects were estimated by multiplying the path coefficients (listed in Figures 2–4). When testing the full hypothesized serial mediation model with recovery orientation as the outcome (see Figure 2), the indirect effect was significant, b = −0.03; 95% CI = −0.05, −0.02. This was also true when testing a full model with perceived quality of life as the outcome, b = −0.02; 95% CI = −0.03, −0.01 (see Figure 3). However, when social withdrawal was the outcome variable, the hypothesized indirect effect was not significant, b = 0.00; 95% CI = −0.01, 0.01 (see Figure 4).
Table 1.
Descriptive Statistics and Correlations
| Variables | N | M/% | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (Male) | 516 | 73.3% | --- | --- | |||||||||||
| 2. Age | 516 | 48.86 | 11.75 | .175*** | --- | ||||||||||
| 3. Race (White) | 511 | 39.3% | --- | −.032 | −.111* | --- | |||||||||
| 4. Education (HS) | 514 | 80.4% | --- | .054 | .020 | .104* | --- | ||||||||
| 5. BSI-D | 515 | 1.02 | 0.90 | −.002 | −.046 | .144** | .106* | --- | |||||||
| 6. CES-QS | 510 | 18.60 | 6.03 | −.074 | −.026 | .022 | .078 | .419*** | --- | ||||||
| 7. ISMI-24 | 515 | 2.25 | 0.49 | −.090* | −.002 | .044 | −.013 | .473*** | .467*** | --- | |||||
| 8. SERS | 506 | 98.20 | 20.67 | .017 | .023 | −.146** | .005 | −.590*** | −.366*** | −.666*** | --- | ||||
| 9. GSES | 515 | 3.63 | 0.71 | .035 | −.036 | −.082 | −.027 | −.404*** | −.222*** | −.385*** | .579*** | --- | |||
| 10. MARS | 515 | 97.01 | 17.70 | .019 | −.001 | −.137** | −.011 | −.450*** | −.252*** | −.559*** | .707*** | .655*** | --- | ||
| 11. BQOL | 515 | 4.51 | 1.38 | .030 | −.006 | −.066 | −.052 | −.543*** | −.270*** | −.409*** | .562*** | .508*** | .532*** | --- | |
| 12. SFS-WD | 471 | 10.02 | 2.23 | −.110* | −.034 | .002 | −.047 | −.333*** | −.162*** | −.286*** | .380*** | .223*** | .268*** | .293*** | --- |
Note.
p < .05.
p < .01.
p < .001.
Descriptive statistics and correlations provided prior to standardization. Sex (0 = Female, 1 = Male). Age reported in years. Race (0 = Non-White, 1 = White). Education (0 = Less than 12 years, 1 = 12 or more years). BSI-D: Depression subscale score from Brief Symptom Inventory. CES-QS: Consumer Experiences of Stigma Questionnaire, Stigma Experiences subscale total score. ISMI-24: 24-item Internalized Stigma of Mental Illness Inventory (excluding stigma resistance) total score. SERS: Self-Esteem Rating Scale–Short Form total score. GSES: General Self-Efficacy Scale total score. MARS: Maryland Assessment of Recovery in Serious Mental Illness Scale total score. BQOL: Score on one item (“How do you feel about your life in general?”) of Brief Quality of Life Scale. SFS-WD: Social engagement/withdrawal subscale score from the Social Functioning Scale.
Figure 2.
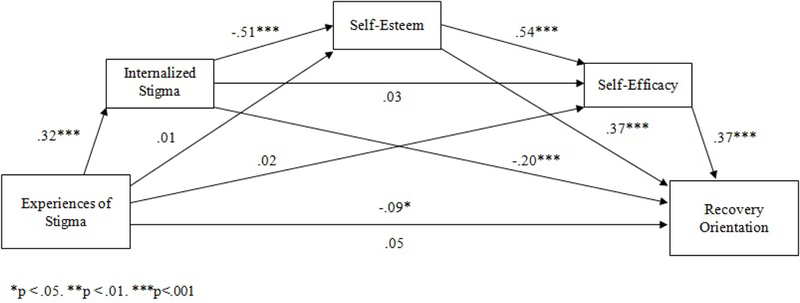
A serial multiple mediation model with internalized stigma, self-esteem, and self-efficacy as proposed mediators of the effect of experience of stigma on recovery orientation.
Figure 4.
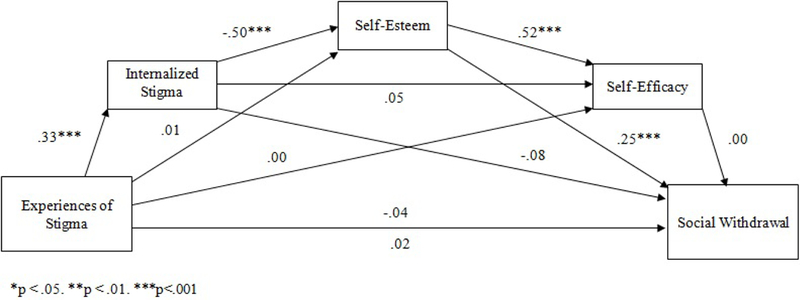
A serial multiple mediation model with internalized stigma, self-esteem, and self-efficacy as proposed mediators of the effect of experience of stigma on social withdrawal
Figure 3.
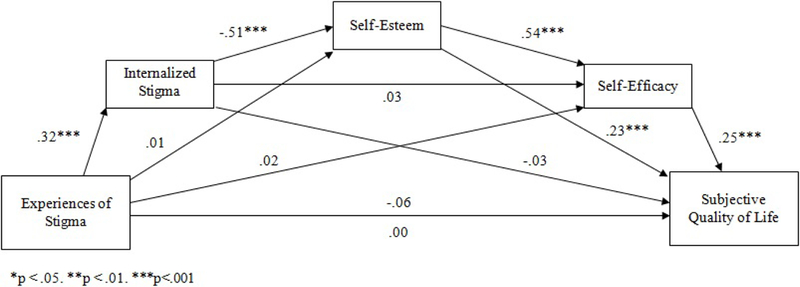
A serial multiple mediation model with internalized stigma, self-esteem, and self-efficacy as proposed mediators of the effect of experience of stigma on perceived quality of life
We then examined other orders of the mediators to test our hypothesized directionality. Four of these tests for each outcome were not significant: When internalized stigma was the second mediator (i.e., experiences of stigma → self-esteem → internalized stigma → self-efficacy → outcomes, experiences of stigma → self-efficacy → internalized stigma → self-esteem → outcomes), the models were not significant for any outcome. Similarly, when internalized stigma was the final mediator (i.e., experiences of stigma →self-esteem → self-efficacy → internalized stigma → outcomes, experiences of stigma → self-efficacy → self-esteem → internalized stigma → outcomes), the models were also not significant. However, when we tested a model in which internalized stigma was the first mediator, followed by self-efficacy and then self-esteem (switching the order self-efficacy and self-esteem from our hypothesized pathway), the indirect path was significant for all three outcomes (recovery orientation, b = −0.01; 95% CI = −0.02, −0.005; perceived quality of life, b = −0.01; 95% CI = −0.01, −0.002; social withdrawal, b = −0.01; 95% CI = −0.01, −0.002).
Parallel mediation was also tested. Parallel mediation assumes that all three mediators explain the relation between experiences of stigma and recovery-related outcomes simultaneously. These models were not superior to the serial mediation models; self-esteem was a significant mediator for all three outcomes, and internalized stigma was also a significant mediator for recovery orientation only. Findings suggested that self-efficacy alone was not a significant mediator, and only added to the predictive power of the full serial mediation model when it followed internalized stigma (data available from authors).
One caveat regarding the role of self-efficacy in the serial mediation models is notable. Removing self-efficacy did not change the statistical significance of the indirect effects for any of the outcomes. When only internalized stigma and self-esteem were entered as serial mediators, the indirect effects were significant for all three outcomes (data available from authors). Notably, this is in contrast to the full serial mediation pathway (including self-efficacy) with social withdrawal as an outcome, which was not significant. Taken together, particularly in the context of the parallel mediation findings, these results suggest that self-efficacy may not be as critical in explaining the path between experiences of stigma and recovery-related variables as the other variables.
Discussion
Previous research has identified experiences of social stigma as a barrier to recovery. The present study supports this notion by identifying a sequential chain of effects—internalized stigma, self-esteem, and self-efficacy—that mediate the relationship between experiences of stigma and the outcomes of recovery orientation and perceived quality of life. That is, one possible chain of events catalyzed by experiences of stigmatization that harms recovery outcomes. When self-efficacy was removed from the hypothesized model, the serial mediation was significant for all three outcomes, including social withdrawal. Our findings also support our hypothesis of serial mediation. That is, there appears to be a specific directionality among these variables that influences recovery outcomes, whereby experiences of stigmatization lead to internalized stigma, when then causes decrements in self-esteem, before recovery-oriented outcomes are influenced.
Experiences of stigmatization harm recovery outcomes. Consistent with the social-cognitive model (Corrigan et al., 2006), internalized stigma was a critical initial mediator between these experiences and recovery. In the model, experiences of stigma led to increased internalized stigma, which then lowered self-esteem and subsequently affected recovery-related outcomes. These findings suggest that treatments that omit internalized stigma as an explicit target and only address more downstream effects of stigma (e.g., self-esteem) may not be as effective as those primarily targeting internalized stigma or addressing both.
Reducing societal stigma globally and individuals’ exposure to it locally would have the largest benefit, but culture change is a long and uneven process, and individuals must navigate their current social environments in the present. Thus, more proximal interventions could aim to prevent the development of internalized stigma in the face of stigma experiences, thereby cutting off this deleterious pathway at the start. Interventions could also aim to reduce or eliminate internalized stigma and disrupt its damaging impact on self-esteem and other recovery elements. Prior studies indicate that cognitive-behavioral and narrative enhancement approaches may be effective to this end (Blinded for review, 2016; Yanos et al., 2008). Additionally, interventions aimed at reducing internalized stigma could include specific components to enhance self-esteem. Given the strong link between internalized stigma and recovery orientation, anti-stigma interventions would benefit from including psychoeducation regarding the recovery model of mental illness to instill hope and empower participants in their recovery journeys. Directly addressing these person-level harms of societal stigma may be essential to mitigating the negative effects of stigma experiences on mental health recovery.
Of the three recovery-related outcomes we examined (recovery orientation, perceived quality of life, and social withdrawal), our hypothesized serial mediation model accounted for the greatest proportion of variance in recovery orientation. Recovery orientation represents a psychological attitude in which an individual approaches his/her own mental health recovery from a place of hope and empowerment, striving to overcome psychiatric disability and live a meaningful life in the communities of his/her choice (Drapalski et al., 2012). Thus, when experiences of stigma are internalized, it leads to decrements in self-esteem that contribute to disempowerment and hopelessness, including regarding one’s potential for mental health recovery. However, there remains additional variance in the model that was not accounted for. This suggests that additional variables factor into recovery orientation and should be explored.
Although the model was also significant for the outcomes of quality of life and social withdrawal, the variance accounted for was substantially lower. Both are likely influenced by additional factors that we did not measure. The variance accounted for in the model with social withdrawal as the outcome was particularly low. Social withdrawal is likely influenced by many factors other than social and internalized stigma not included here, such as psychiatric symptoms, social skills, and coping patterns. Interventions aiming to mitigate internalized stigma should examine recovery orientation as an important and powerful proximal outcome, and consider quality of life and social isolation potentially as more indirect, distal outcomes. In addition, these relations may be stronger for perceived quality of life in specific domains that are more closely linked to self-stigma, such as family and/or social relationships, rather than a global quality of life self-rating.
The present findings also suggest the greater relative importance of self-esteem versus self-efficacy in the link between experiences of stigma, internalized stigma, and recovery outcomes, as indirect paths that excluded self-efficacy remained significant for each outcome. The relative roles of self-esteem and self-efficacy in the path from stigma to recovery have been the subject of some controversy (Brown, Rempfer, & Hamera, 2008). The present study suggests that these are distinct constructs that may uniquely contribute to mental health recovery, and that the impact of internalized stigma on recovery-related outcomes may occur chiefly through reductions in self-esteem. Notably, the self-efficacy measure used in the present study was a general one. Self-efficacy in specific areas or domains (e.g. social self-efficacy, self-efficacy with regard to treatment) may be more closely linked to mental health recovery than self-efficacy measured broadly. Future research using a self-efficacy measure more relevant to mental health recovery would help clarify these findings.
The present study had several limitations. First, it was a cross-sectional and post-hoc analysis, based on prior research and theory. Therefore, while serial mediation and our checks of alternative directional relationships do suggest directional relationships, this study cannot determine causality. Future longitudinal research would enable measurement of mediators at multiple time points, allowing for a more rigorous evaluation of the causal links in the model. Validation of the current model will also require additional replications across settings and populations. Additionally, quality of life in the present study was measured by a single item asking about overall quality of life; future research needs to assess this construct more thoroughly across specific life domains.
Conclusions
In conclusion, the present study provides important evidence to support the social-cognitive model of internalized stigma by indicating that internalized stigma is a critical mediator in the link between stigma experiences and recovery-related outcomes, and that the impact of internalized stigma on these outcomes occurs, at least in part, through decrements in self-esteem. The supported model provides multiple potential nodes for intervention, and suggests that treatments may need to target multiple points along the pathway from stigma to recovery outcomes to be maximally effective (Drapalski et al., 2013). Although the reduction of societal stigma regarding mental illness remains an important long-term public health target, the present study indicates that interventions focused on reducing the internalization of stigma experiences may provide more direct benefit to the recovery of individuals with SMI.
Impact and Implications:
This study found that, among people with serious mental illness, experiences of stigma impact recovery through increasing internalized stigma and reducing self-esteem. Therefore, to improve recovery in this population, individual or group interventions should target internalized stigma, as well as addressing societal mental health stigma as a public health issue.
Acknowledgments
This work was supported by NIMH 1R01MH090036–01A1, and Merit Review Award #1I01HX00279 from the Unites States Department of Veterans Affairs Health Services Research and Development Service, and the VA Capitol Network (VISN5) Mental Illness Research, Education, and Clinical Center. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. Clinicaltrials.gov identifier: NCT01259427
Contributor Information
Danielle R. Jahn, Center for Acute Recovery Empowerment, Orlando VA Medical Center, Orlando, FL
Jaclyn Leith, VA Maryland Health Care System, Baltimore, MD.
Anjana Muralidharan, Department of Veterans Affairs, VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), U.S. Baltimore, MD; Department of Psychiatry, University of Maryland School of Medicine, Baltimore, MD.
Clayton H. Brown, Department of Veterans Affairs, VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), U.S, Baltimore, MD Department of Epidemiology and Public Health, University of Maryland School of Medicine, Baltimore, MD.
Amy L. Drapalski, Department of Veterans Affairs, VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), U.S., Baltimore, MD
Samantha Hack, Department of Veterans Affairs, VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), U.S., Baltimore, MD; School of Social Work, University of Maryland, Baltimore, MD.
Alicia Lucksted, Department of Psychiatry, VA Capitol Healthcare Network (VISN 5) Mental Illness Research, Education, and Clinical Center (MIRECC), U.S. Department of Veterans Affairs, Baltimore, MD; University of Maryland School of Medicine, Baltimore, MD.
References
- American Psychological Association (2016). Stress in America: The impact of discrimination. Retrieved from https://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf
- Beacon Health Options (2016). Chapter 7: The state of Maryland’s medical necessity criteria. In Maryland Provider Manual (subsection 7.11 Psychiatric Rehabilitation Program – Adult). Retrieved from http://maryland.beaconhealthoptions.com/provider/manual/CH07_11-Psychiatric-Rehabilitation-Program-Adult.pdf [Google Scholar]
- Bellack AS (2006). Scientific and consumer models of recovery in schizophrenia: Concordance, contrasts, and implications. Schizophrenia Bulletin, 32, 432–442. doi: 10.1093/schbul/sbj044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birchwood M, Smith J, Cochrane R, Wetton S, & Copestake S (1990). The Social Functioning Scale: The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. The British Journal of Psychiatry, 157, 853–859. doi: 10.1192/bjp.157.6.853 [DOI] [PubMed] [Google Scholar]
- Brown C, Rempfer M, & Hamera E (2008). Correlates of insider and outsider conceptualizations of recovery. Psychiatric Rehabilitation Journal, 32, 23–31. doi: 10.2975/32.1.2008.23.31 [DOI] [PubMed] [Google Scholar]
- Chen G, Gully SM, & Eden D (2001). Validation of a new general self-efficacy scale. Organizational Research Methods, 4, 62–83. doi: 10.1177/109442810141004 [DOI] [Google Scholar]
- Corrigan PW, Rafacz J, & Rusch N (2011). Examining a progressive model of self-stigma and its impact on people with serious mental illness. Psychiatry Research, 189, 339–343. doi: 10.1016/j.psychres.2011.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC, & Barr L (2006). The self-stigma of mental illness: Implications for self-esteem and self-efficacy. Journal of Social and Clinical Psychology, 25, 875–884. doi: 10.1521/jscp.2006.25.8.875 [DOI] [Google Scholar]
- Corrigan PW, Watson AC, & Miller FE (2006). Blame, shame, and contamination: The impact of mental illness and drug dependence stigma on family members. Journal of Family Psychology, 20, 239–246. doi: 10.1037/0893-3200.20.2.239 [DOI] [PubMed] [Google Scholar]
- Crocker J, & Quinn DM (2000). Social stigma and the self: Meanings, situations, and self-esteem In Heatherton TF, Kleck RE, Hebl MR, & Hull JG (Eds.), The Social Psychology of Stigma (pp. 153–183). New York: Guilford Press. [Google Scholar]
- Derogatis LR (1993). Brief Symptom Inventory: Administration, scoring, and procedures manual (4th ed.). Minneapolis, MN: National Computer Systems. [Google Scholar]
- Dickerson FB, Sommerville J, Origoni AE, Ringel NB, & Parente F (2002). Experiences of stigma among outpatients with schizophrenia. Schizophrenia Bulletin, 28, 143–155. doi: 10.1093/oxfordjournals.schbul.a006917 [DOI] [PubMed] [Google Scholar]
- Drapalski AL, Lucksted A, Perrin PB, Aakre JM, Brown CH, DeForge BR, & Boyd JE (2013). A model of internalized stigma and its effects on people with mental illness. Psychiatric Services, 64, 264–269. doi: 10.1176/appi.ps.001322012 [DOI] [PubMed] [Google Scholar]
- Drapalski AL, Medoff D, Dixon L, & Bellack A (2016). The reliability and validity of the Maryland Assessment of Recovery in Serious Mental Illness Scale. Psychiatry Research, 239, 259–264. doi: 10.1016/j.psychres.2016.03.031 [DOI] [PubMed] [Google Scholar]
- Drapalski AL, Medoff D, Unick GJ, Velligan DI, Dixon LB, & Bellack AS (2012). Assessing recovery of people with serious mental illness: Development of a new scale. Psychiatric Services, 63, 48–53. doi: 10.1176/appi.ps.201100109 [DOI] [PubMed] [Google Scholar]
- Green CA, Perrin NA, Leo MC, Janoff SL, Yarborough BJ, & Paulson RI (2013). Recovery from serious mental illness: Trajectories, characteristics, and the role of mental health care. Psychiatric Services, 64, 1203–1210. doi: 10.1176/appi.ps.201200545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartshorn KJS, Whitbeck LB, & Hoyt DR (2012). Exploring the relationships of perceived discrimination, anger, and aggression among North American indigenous adolescents. Society and Mental Health, 2, 53–67. doi: 10.1177/2156869312441185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis. New York: Guilford Press. [Google Scholar]
- Hayes AF, Preacher KJ, & Myers TA (2011). Mediation and the estimation of indirect effects in political communication research. In Bucy EP & Lance Holbert R (Eds), Sourcebook for political communication research: Methods, measures, and analytical techniques. (pp. 434–465). New York: Routledge. [Google Scholar]
- Hill K, & Startup M (2013). The relationship between internalized stigma, negative symptoms and social functioning in schizophrenia: The mediating role of self-efficacy. Psychiatry Research, 206, 151–157. doi: 10.1016/j.psychres.2012.09.056 [DOI] [PubMed] [Google Scholar]
- Kline RB (1998). Principles and practice of structural equation modeling. New York, NY: Guilford. [Google Scholar]
- Lehman AF (1995). Measuring quality of life in a reformed health system. Health Affairs, 14(3), 90–101. doi: 10.1377/hlthaff.14.3.90 [DOI] [PubMed] [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, & Phelan JC (2001). Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatric Services, 52(12), 1621–1626. doi: 10.1176/appi.ps.52.12.1621 [DOI] [PubMed] [Google Scholar]
- Livingston JD, & Boyd JE (2010). Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine, 71, 2150–2161. doi: 10.1016/j.socscimed.2010.09.030 [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Roe D, & Yanos PT (2007). Toward understanding the insight paradox: Internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophrenia Bulletin, 33, 192–199. doi: 10.1093/schbul/sbl016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mashiach-Eizenberg M, Hasson-Ohayon I, Yanos PT, Lysaker PH, & Roe D (2013). Internalized stigma and quality of life among persons with severe mental illness: the mediating roles of self-esteem and hope. Psychiatry Research, 208, 15–20. doi: 10.1016/j.psychres.2013.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz M, Sanz M, Pérez-Santos E, & de los Ángeles Quiroga M. (2011). Proposal of a socio-cognitive-behavioral structural equation model of internalized stigma in people with severe and persistent mental illness. Psychiatry Research, 186, 402–408. doi: 10.1016/j.psychres.2010.06.019 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2017). Prevalence of serious mental illness. Retrieved from https://www.nimh.nih.gov/health/statistics/mental-illness.shtml
- Newcomb ME, & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review, 30, 1019–1029. doi: 10.1016/j.cpr.2010.07.003 [DOI] [PubMed] [Google Scholar]
- Nugent WR (2004). A validity study of two forms of the Self-Esteem Rating Scale. Research on Social Work Practice, 14, 287–294. doi: 10.1177/1049731503257890 [DOI] [Google Scholar]
- Nugent WR, & Thomas JW (1993). Validation of a clinical measure of self-esteem. Research on Social Work Practice, 3, 191–207. doi: 10.1177/104973159300300205 [DOI] [Google Scholar]
- Office of Disease Prevention and Health Promotion. (2016). Mental health and mental disorders. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/mental-health-and-mental-disorders
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. doi: 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Resnick SG, Rosenheck RA, & Lehman AF (2004). An exploratory analysis of correlates of recovery. Psychiatric Services, 55, 540–547. doi: 10.1176/appi.ps.55.5.540 [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, & Grajales M (2003). Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research, 121, 31–49. doi: 10.1016/j.psychres.2003.08.008 [DOI] [PubMed] [Google Scholar]
- Scherbaum CA, Cohen-Charash Y, & Kern MJ (2006). Measuring general self-efficacy: A comparison of three measures using item response theory. Educational and Psychological Measurement, 66, 1047–1063. doi: 10.1177/0013164406288171 [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2012). SAMHSA’s Working Definition of Recovery. Retrieved from http://store.samhsa.gov/shin/content//PEP12-RECDEF/PEP12-RECDEF.pdf
- Sue DW (2010). Microaggressions and marginality: Manifestation, dynamics, and impact. New York: John Wiley & Sons. [Google Scholar]
- Vauth R, Kleim B, Wirtz M, & Corrigan PW (2007). Self-efficacy and empowerment as outcomes of self-stigmatizing and coping in schizophrenia. Psychiatry Research, 150, 71–80. doi: 10.1016/j.psychres.2006.07.005 [DOI] [PubMed] [Google Scholar]
- Wahl OF (1999). Mental health consumers’ experience of stigma. Schizophrenia Bulletin, 25, 467–478. doi: 10.1093/oxfordjournals.schbul.a033394 [DOI] [PubMed] [Google Scholar]
- Watson AC, Corrigan P, Larson JE, & Sells M (2007). Self-stigma in people with mental illness. Schizophrenia Bulletin, 33, 1312–1318. doi: 10.1093/schbul/sbl076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanos PT, Roe D, Markus K, & Lysaker PH (2008). Pathways between internalized stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiatric Services, 59, 1437–1442. doi: 10.1176/appi.ps.59.12.1437 [DOI] [PMC free article] [PubMed] [Google Scholar]


