Abstract
The anterior cruciate ligament (ACL) is the most common ligamentous knee injury and often is encountered in those participating in multidirectional sports. ACL reconstruction is the most commonly performed knee ligament reconstruction and employs a variety of surgical techniques but still is challenged by residual laxity and graft rupture. To help address and prevent future ACL failures, new repair and reconstruction techniques have been employed that incorporate suture augmentation (InternalBrace; Arthrex, Naples, FL), which protects the graft during healing and ligamentization. Our goal of this article is to provide a surgical technique of suture augmentation with ACL reconstruction.
The anterior cruciate ligament (ACL) is the most common ligamentous knee injury and often is encountered in those participating in multidirectional sports.1, 2 Injuries to the ACL can leave the patient with a greater risk of meniscal tears, chondral injury, and progression to osteoarthritis, with continued play.3
ACL reconstruction is the most commonly performed knee ligament reconstruction and employs a variety of surgical techniques.4 However, despite high success rates, it is still challenged by residual laxity and graft rupture.5
To help address and prevent future ACL failures, new repair and reconstruction techniques have been employed that incorporate suture augmentation.6, 7, 8 The goal of augmentation is to protect the newly repaired or reconstructed ligament during rehabilitation.9, 10, 11 Studies and results are, however, sparse in the literature and more specifically have mainly been used for repair.12 To our knowledge, only one publication has evaluated the use of suture tape augmentation with reconstruction.7 Our goal of this article is to provide a surgical technique for suture tape augmentation in ACL reconstruction.
Surgical Technique
Examination under anesthesia demonstrates ACL insufficiency. A standard arthroscopy is performed, and ACL tear is confirmed (Video 1).
Graft Preparation
A standard bone patellar tendon bone autograft is harvested through an anterior incision using 20- to 25-mm bone plugs for autografts. Alternatively, for allograft, Achilles allograft with bone block is obtained. The graft is then sized and prepared by drilling a 2-mm hole through the superior plug (and inferior bone plugs for autograft). Suture tape is then tied around the distal end of the femoral bone block and passed to the planned anterior aspect of the graft with a free needle. These tails will serve as our suture tape augmentation. A second suture tape is then passed through the superior holes (and inferior bone block for autograft) to assist in graft passage (Figs 1 and 2).
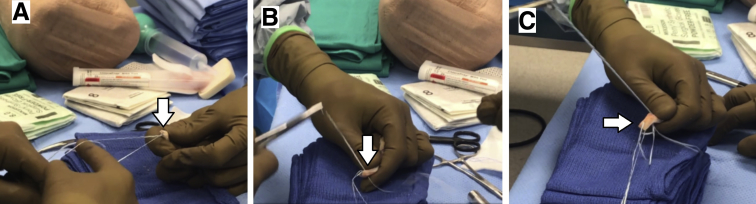
Fig 1.
Patient in supine position, right knee, viewing from the anterior lateral portal. (A) Suture tape is passed through the predrilled, 2-mm hole on the planned femoral aspect of the bone block and tied around the planned proximal posterior end of the bone block. (B) A separate passing suture is passed through the same 2-mm planned femoral bone block hole. (C) The tails of the suture tape from (A) are passed back through the graft, as seen in the image. These tails will be fixed in the tibial tunnel, whereby they will span the graft and function as the suture augmentation.
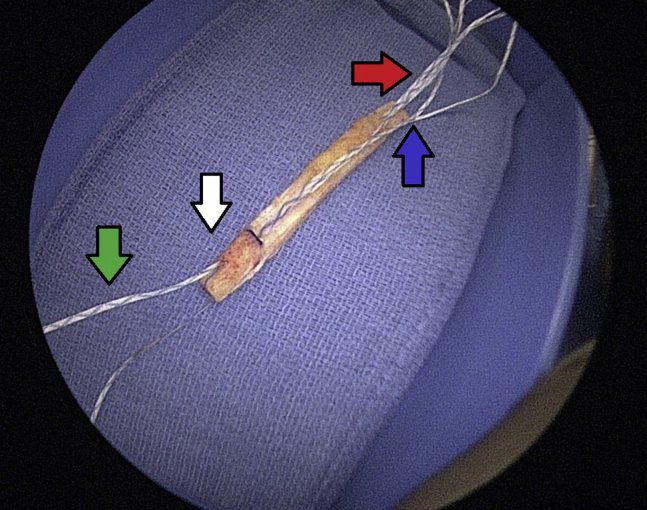
Fig 2.
The final ACL graft with suture augmentation construct. White arrow: The planned femoral aspect of the graft. Green arrow: Passing sutures of the planned femoral aspect of the graft. Red arrow: Passing suture of the planned tibial aspect of the graft. Blue arrow: Tails of the suture augmentation. (ACL, anterior cruciate ligament.)
Graft Passage
A standard femoral tunnel is made through the anterior medial portal and antegrade drilling is used for the tibia. The graft is then passed through the tibial tunnel and secured with an interference screw into the femur. The suture tape augmentation tails (previously marked) are then retrieved from the anterior medial portal. The graft is then cycle and isometric point is confirmed. The knee is the placed into near full extension with posterior drawer. The tibial side of the graft is then secured with interference screw while maintaining appropriate tension (Fig 3).
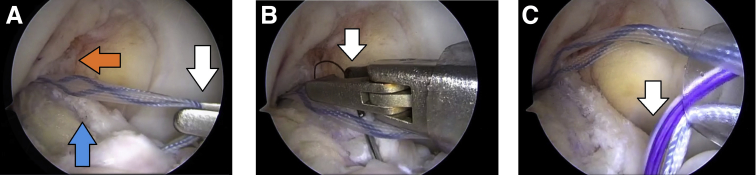
Fig 3.
These images are taken from the anterior lateral portal with the patient's right knee in 90° of flexion, patient in supine position. (A) The orange arrow points to the femoral tunnel where the ACL graft has been fixed using an interference screw. The blue arrow points to the ACL graft. The tibial tunnel is in the inferior portion of the image. The suture tape is retrieved through an anterior medial portal (white arrow). (B) A suture wire is passed through the tibial interference screw and is retrieved via the anteromedial portal. (C) The suture tape is pulled through the tibial interference screw using the suture wire. (ACL, anterior cruciate ligament.)
Suture Tape Augmentation Fixation
A nitinol suture wireloop is then inserted through the cannulation of the tibial interference screw. The suture tape augmentation tails are taken out. The internal brace sutures are then passed through the retriever and then the wire is pulled out through the tibial screw. Again, isometry is then checked, and the tails are tied over a small metal button that is place directly over the tibial interference screw within the tibial tunnel. Avoiding full extension of the knee, square knots are then placed sequentially to secure the button in a manner so as not to overconstrain the knee. The suture augmentation and graft are then checked with arthroscopy to confirm appropriate tension. The augmentation should not be tighter than the graft (Fig 4).
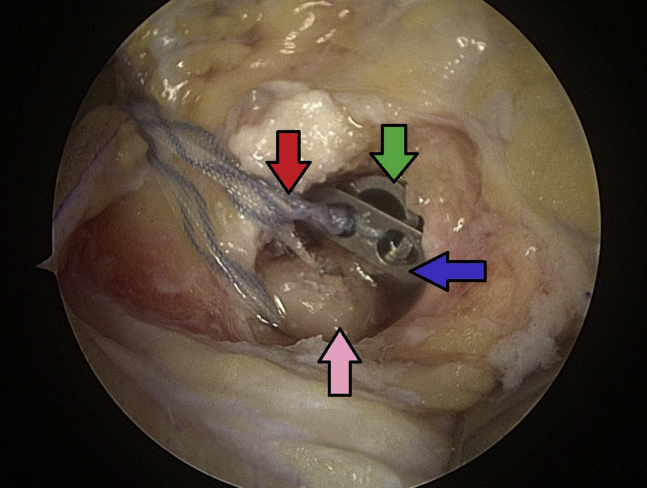
Fig 4.
Patient in supine position, right knee, viewing from the anterior lateral portal. An extra-articular image of the tibial aspect of the final construct. Pink arrow: the bone block, which has been fixed in the tibial tunnel. Green arrow: The tibial interference screw, which has fixed the bone block in place. Blue arrow: a metallic button, which rests on top of the tibial interference screw. Red arrow: The tails of the suture tape, which have been tied down over the button, and are now fixed in place.
Discussion
With ACL injuries growing more common, so too are ACL reconstructions to aid patients in returning to sporting activities. Re-ruptures and residual laxity continue to be a challenge for patients and surgeons to address. We feel that suture tape augmentation can provide added support to the reconstruction that may allow for quicker recovery without risking graft failure. The results of our suture tape augmentation demonstrate lower failure and revision surgery rates of conventional primary ACL reconstruction.13, 14 In addition, recent studies have shown improved repair with suture augmentation in the animal model as well as ankle and elbow instability.15, 16, 17 Specifically, Bachmaier et al.18 evaluated the use of suture tape augmentation in the setting of ACL reconstruction with a biomechanical study. Their group found load sharing and protective effects of the suture tape augmentation. They found the presence of the suture tape prevented graft elongation, further supporting the basis of graft protection during healing and maturation.
As the goal of this article is more a description of a surgical technique, there are limitations in its comparison and evaluation (Tables 1 and 2). There is no randomization or control group with which to compare the suture tape augmentation. Future studies can be aimed to address these limitations and provide more insight to the advantages and disadvantages of suture tape augmentation. In summary, this is a safe technique without significant added time or complications of graft failure or arthrofibrosis.
Table 1.
Advantages and Disadvantages of ACL Reconstruction Using Internal Brace Augmentation
| Advantages | Disadvantages |
|---|---|
| • Protects graft during rehabilitation • Limits peak forces on the graft • Tensioned independently from ACL reconstruction • Can be used with both autograft and allograft reconstruction |
• Theoretical risk for overconstraining if overtensioned • Graft may not see peak forces and may be shielded • No long-term comparison clinical outcome data |
ACL, anterior cruciate ligament.
Table 2.
Indications, Pearls, and Pitfalls of ACL Reconstruction With Internal Brace Augmentation
| Indications | Pearls | Pitfalls |
|---|---|---|
| • Primary ACL reconstruction with auto or allograft | • Mark suture tape to identify from graft passage sutures • Use cannula to avoid soft-tissue bridge |
• Overtensioning the internal brace |
| • Adult and adolescent patients | • Cycle, tension, and fix the graft then cycle and tension the internal brace at the isometric point | |
| • Keep internal brace anterior to graft to have better visualization to view tension |
ACL, anterior cruciate ligament.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic ACL reconstruction with suture tape reconstruction allows for protection of the graft from excessive forces during healing and ligamentization. This video demonstrates the following processes: (1) Installation of the suture tape augmentation on a standard bone patellar-tendon bone autograft. (2) Passage of the suture tape tails following standard ACL reconstruction. Video is taken from the anterolateral portal with the right knee in 90° flexion, patient in supine position. (3) Fixation of the suture tape augmentation using a metallic button. (4) Arthroscopic visualization of the completed construct and verification of proper position and tension of the suture tape augmentation. (ACL, anterior cruciate ligament.)
References
- 1.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Magnussen R.A., Granan L.P., Dunn W.R. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18:98–105. doi: 10.1007/s00167-009-0919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanders T.L., Pareek A., Kremers H.M. Long-term follow-up of isolated ACL tears treated without ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:493–500. doi: 10.1007/s00167-016-4172-4. [DOI] [PubMed] [Google Scholar]
- 4.Lyman S., Koulouvaris P., Sherman S., Do H., Mandl L.A., Marx R.G. Epidemiology of anterior cruciate ligament reconstruction: Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321–2328. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 5.Schlumberger M., Schuste P., Schulz M. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: Retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2017;25:1535–1541. doi: 10.1007/s00167-015-3699-0. [DOI] [PubMed] [Google Scholar]
- 6.Mahapatra P., Horriat S., Anand B.S. Anterior cruciate ligament repair—past, present and future. J Exp Orthop. 2018;5:20. doi: 10.1186/s40634-018-0136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith P.A., Bley B.A. Allograft anterior cruciate ligament reconstruction utilizing internal brace augmentation. Arthrosc Tech. 2016;5:e1143–e1147. doi: 10.1016/j.eats.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonkergouw A., van der List J.P., DiFelice G.S. Arthroscopic primary repair of proximal anterior cruciate ligament tears: Outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc. 2019;27:21–28. doi: 10.1007/s00167-018-5338-z. [DOI] [PubMed] [Google Scholar]
- 9.Heusdens C.H.W., Hopper G.P., Dossche L., Roelant E., Mackay G.M. Anterior cruciate ligament repair with Independent suture tape reinforcement: A case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27:60–67. doi: 10.1007/s00167-018-5239-1. [DOI] [PubMed] [Google Scholar]
- 10.Smith J.O., Yasen S.K., Palmer H.C., Lord B.R., Britton E.M., Wilson A.J. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc. 2016;24:1845–1851. doi: 10.1007/s00167-016-4150-x. [DOI] [PubMed] [Google Scholar]
- 11.van der List J.P., DiFelice G.S. Arthroscopic primary anterior cruciate ligament repair with suture augmentation. Arthrosc Tech. 2017;6:e1529–e1534. doi: 10.1016/j.eats.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Eck C.F., Limpisvasti O., ElAttrache N.S. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. 2018;46:2291–2298. doi: 10.1177/0363546517717956. [DOI] [PubMed] [Google Scholar]
- 13.Kaeding C.C., Aros B., Pedroza A. Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desai N., Andernord D., Sundemo D. Revision surgery in anterior cruciate ligament reconstruction: A cohort study of 17,682 patients from the Swedish national knee ligament Register. Knee Surg Sports Traumatol Arthrosc. 2017;25:1542–1554. doi: 10.1007/s00167-016-4399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seitz H., Pichl W., Matzi V., Nau T. Biomechanical evaluation of augmented and nonaugmented primary repair of the anterior cruciate ligament: An in vivo animal study. Int Orthop. 2013;37:2305–2311. doi: 10.1007/s00264-013-2098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoo J.S., Yang E.A. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–360. doi: 10.1007/s10195-016-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones C.M., Beason D.P., Dugas J.R. Ulnar collateral ligament reconstruction versus repair with internal bracing: Comparison of cyclic fatigue mechanics. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118755991. 2325967118755991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bachmaier S., Smith P.A., Bley J., Wijdicks C.A. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: A biomechanical full construct model. Arthroscopy. 2018;34:490–499. doi: 10.1016/j.arthro.2017.10.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic ACL reconstruction with suture tape reconstruction allows for protection of the graft from excessive forces during healing and ligamentization. This video demonstrates the following processes: (1) Installation of the suture tape augmentation on a standard bone patellar-tendon bone autograft. (2) Passage of the suture tape tails following standard ACL reconstruction. Video is taken from the anterolateral portal with the right knee in 90° flexion, patient in supine position. (3) Fixation of the suture tape augmentation using a metallic button. (4) Arthroscopic visualization of the completed construct and verification of proper position and tension of the suture tape augmentation. (ACL, anterior cruciate ligament.)