Abstract
Background:
Digital self-monitoring, such as through smartphone applications (apps) or activity trackers, could be applied to monitor the health of people with multiple sclerosis (MS). This self-monitoring could facilitate personalized therapies and self-management of MS. The acceptance of digital self-monitoring tools by patients depends on them being able and willing to use these tools in their daily lives.
Methods:
In-depth interviews were conducted with seven adults with MS before and after participation in a study in which they used an activity tracker and an MS-specific smartphone app for 4 weeks. We inquired about experiences with the tools in daily life and needs and wishes regarding further development and implementation of digital self-monitoring for people with MS.
Results:
The smartphone app and the activity tracker increased respondents' awareness of their physical status and stimulated them to act on the data. Challenges, such as confrontation with their MS and difficulties with data interpretation, were discussed. The respondents desired 1) adaptation of digital self-monitoring tools to a patient's personal situation, 2) guidance to increase the value of the data, and 3) integration of digital self-monitoring into treatment plans.
Conclusions:
These findings show that patients can provide detailed descriptions of their daily life experiences with new technologies. Mapping these experiences could help in better aligning the development and implementation of digital self-monitoring tools, in this case smartphones and activity trackers, with the needs and wishes of people with MS.
Keywords: Activity trackers, Digital health, Multiple sclerosis (MS), Qualitative study, Self-monitoring, Smartphone apps
In recent years there has been an increase in digital health solutions for multiple sclerosis (MS) to support disease monitoring, self-management, treatment, and rehabilitation.1 These solutions include smartphone applications (apps) and activity trackers, which can be used for digital self-monitoring, ie, collecting personal health data on, for example, physical activity, mental status, and sleep.2
One assumption is that through monitoring of longitudinal, real-world health data of people with MS, disease progression can be tracked and more information will be available to adapt treatment decisions to the individual patient.1 However, thus far most digital self-monitoring devices have unknown reliability and validity, with a lack of evidence for the effectiveness of these technologies.3,4 So, before digital self-monitoring of MS through smartphones and activity trackers could become common practice, the validity and reliability of these technologies, including their responsiveness to changes in disease status, need to be proved in real-world settings.5
Another assumption is that smartphone apps and activity trackers could contribute to patient empowerment, with patients taking a more active role in the self-management of chronic diseases, for example through symptom monitoring and adopting lifestyle measures.6,7 Nevertheless, this assumption is based on an “ideal situation” in which patients have the adequate knowledge and skills for using digital self-monitoring tools in their daily lives.8
For smartphone apps and activity trackers to become adopted by people with MS, patients will need to experience the value of these tools and feel well equipped to use the tools in their daily lives.6 Therefore, we focus on the daily life experiences, needs, and wishes of people with MS regarding digital self-monitoring through smartphone apps and activity trackers.
Thus far, there has been low adoption of digital self-monitoring technologies by patients with chronic diseases, which can partly be explained by an inappropriate fit of these technologies with patients' daily lives and the high patient burden associated with using digital self-monitoring.9 Including the experiences, needs, and wishes of people with MS in the development and implementation of smartphone apps and activity trackers is, therefore, crucial to reduce the inconvenience of using these tools in daily life.
Some studies have inquired into the attitudes of people with MS toward using smartphone apps, including the importance of clear use benefits and of tailoring apps to the specific patient.10,11 However, these studies were not focused on self-monitoring and did not deal with patients' actual experiences. Ayobi et al12 conducted interviews with patients with MS who engaged in self-monitoring, including using smartphones and activity trackers. Patients expressed that self-monitoring can contribute to self-management of MS in their daily lives but also mentioned undesired confrontation with their MS, obsessive symptom monitoring, and a pressure to achieve lifestyle goals set by the activity-tracking tools.
The aim of this study was to build on the work of Ayobi et al12 but by taking a different angle. Whereas Ayobi et al studied people with MS who used smartphone apps and activity trackers on their own initiative, we investigated patient perspectives in the context of a defined study, the MS Self study. The overall aim of the MS Self study was to assess the validity, reliability, and responsiveness of a combination of an activity tracker and an MS-specific smartphone app. The first results of the MS Self study have been presented at the 2018 European Committee on Treatment and Research in MS (ECTRIMS) Congress,13 and the manuscript for a full-length article is in preparation.
The present article focuses on the results of the interviews with MS Self study participants, aiming to answer the following research questions: 1) How do people with MS experience the smartphone app and the activity tracker in their daily lives? 2) What are the needs and wishes of people with MS regarding the further development and implementation of digital self-monitoring tools for MS?
Methods
MS Self Study
The MS Self study was approved by the medical-ethical committee METC Brabant (Tilburg, the Netherlands). Participants had to use a Fitbit Charge 2 (Fitbit Inc, San Francisco, CA) activity tracker and the Mijn Kwik (MS sherpa BV, Nijmegen, the Netherlands) smartphone app for 4 weeks (Figure 1). The Mijn Kwik app is the precursor of the MS Sherpa app (MS sherpa BV) and was made available only for research purposes.13 An overview of the data collected through the activity tracker and smartphone app is presented in Table 1.
Figure 1.
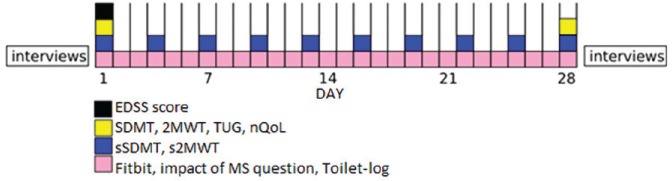
Timeline of the 4-week MS Self study
At start of study, Expanded Disability Status Scale (EDSS),14 Two-Minute Walk Test (2MWT),15 Symbol Digit Modalities Test (SDMT),16 Timed Up and Go (TUG) test,17 and Nocturia Quality-of-Life (nQoL) questionnaire18 scores were collected. All these scores, except for EDSS score, were also collected at end of study. Daily actions during study were wearing a Fitbit Charge 2 (continuously, charging once every 5 days), answering a smartphone question about impact of multiple sclerosis during that day, and filling out paper-based Toilet-log about how often participant woke up at night to go to toilet. Once every 3 days, participants performed smartphone versions of SDMT (sSDMT) and 2MWT (s2MWT). Interviews were scheduled before start and after end of study with seven participants.
Table 1.
Overview of digital self-monitoring data collected during MS Self study
| Data | Method of measurement | Frequency |
|---|---|---|
| Physical activity | Activity tracker measurement of steps walked, number of floors climbed, distance walked, calories burned, and active minutes | Continuously |
| Heart rate | Activity tracker measurement of heart rate per minute | Continuously |
| Sleeping pattern | Activity tracker measurement of duration and quality of sleep | Continuously |
| Physical functioning | Smartphone app 2MWT15 | Once every 3 d |
| Cognitive functioning | Smartphone app SDMT16 | Once every 3 d |
| Impact of MS | Question in smartphone app at end of day: “How much influence did MS have on your functioning today?” scored from 0 (no impact) to 10 (very heavy impact) | Daily |
Abbreviations: app, application; MS, multiple sclerosis; SDMT, Symbol Digit Modalities Test; 2MWT, Two-Minute Walk Test.
The MS Self study investigated patients with relapsing-remitting MS (RRMS), which is the most common form of MS and is characterized by alternating periods of relapse and recovery.19 Participants had to have an Expanded Disability Status Scale (EDSS) score14 less than 6.5 because patients with higher scores were expected to be unable to perform the self-monitoring tasks. Healthy controls, matched on age, sex, and education as much as possible, were included in the study to assess the validity and reliability of the digital self-monitoring tools. Study participants had to be aged 20 to 50 years and were recruited by the Dutch National MS Foundation. Participants provided written informed consent before the start of the study. Twenty-five people with MS and 21 healthy controls participated in the study between May 1, 2017, and July 31, 2018.
Data Collection
Before the start of the MS Self study, ten of the 25 participants with MS were randomly contacted by mail. Interviews were scheduled with seven participants before and after the study (Figure 1), resulting in 14 interviews. With the other three participants it was not possible to schedule an interview before the start of the study.
We conducted in-depth, semistructured interviews because this enabled us to ask follow-up questions and acquire a rich insight into patients' perspectives. An interview guide was developed iteratively with input from the multidisciplinary project team and with knowledge of the existing literature on digital self-monitoring for patients with chronic diseases. The interviews were conducted by telephone, which allowed for more flexibility in scheduling them, and were audiotaped with verbal permission from the respondents.
The first interviews ranged from 40 to 70 minutes and took place a few days before the participants started in the MS Self study. These interviews focused on the participants' expectations and previous experience regarding digital self-monitoring. The second interviews, which form the main focus of this article, were scheduled within a month after the participants had completed the 4-week study and ranged from 60 to 100 minutes. The focus of these interviews was on participants' experiences with the smartphone app and the activity tracker and their needs and wishes regarding digital self-monitoring for MS.
Examples of interview questions for the first research question of this article were “How do you currently deal with the MS in daily life?” and “What insights have you gained from using the smartphone app and activity tracker in your daily life?” Regarding the second research question, interview questions included “Are you willing to use digital self-monitoring tools for a longer period of time and why (not)?” and “What could be improved in digital self-monitoring tools to facilitate long-term use in your daily life?”
Data Analysis
The interviews were transcribed verbatim. The transcripts were uploaded to the qualitative data analysis software ATLAS.ti version 8 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany) and subjected to thematic content analysis.20 An initial codebook was developed by the first author (K.W.), structured according to the topics from the interview guide. The codebook was refined through iterative reading of the interview transcripts. Final agreement on the codebook was achieved through discussion between K.W. and the last author (L.K.), who was also familiar with the data. After coding the interview transcripts, K.W. started clustering the codes into subthemes, which were subsequently clustered into major themes. Consensus on (sub)themes was reached through discussion with L.K.
Results
Interview Respondents
The seven interviewed respondents were all women aged 34 to 50 years (Table 2). Their EDSS scores ranged from 2.0 to 5.5, which are all in the low to middle range (EDSS score <6.0).
Table 2.
Demographic and disease characteristics of interview respondents, including their experience with digital self-monitoring tools before MS Self study
| Respondent No. | Age, y | MS diagnosis year | EDSS score | Experience with digital self-monitoring |
|---|---|---|---|---|
| MS1 | 43 | 2015 | 3.0 | Abandoned use of self-monitoring apps (food intake, physical activity) |
| MS2 | 34 | 2010 | 5.5 | Abandoned use of self-monitoring apps (sleep, physical activity) |
| MS3 | 44 | 2007 | 3.5 | Current use of self-monitoring apps (walking tracker) |
| MS4 | 46 | 2011 | 2.0 | No experience |
| MS5 | 50 | 2005 | 3.0 | No experience |
| MS6 | 48 | 2016 | 2.5 | Current use of self-monitoring apps (walking tracker) |
| MS7 | 47 | 2004 | 3.0 | Current use of self-monitoring apps (physical activity) |
Abbreviations: app, application; EDSS, Expanded Disability Status Scale; MS, multiple sclerosis.
All the respondents owned a smartphone, as this was a prerequisite for study participation. None of them had used an activity tracker before their participation in the MS Self study. Five respondents had some experience with using self-monitoring smartphone apps (Table 2). Two of them had used apps to self-monitor physical activity, sleep, or food intake but had abandoned the use due to a lack of interest and time. Two other respondents sometimes used walking tracker apps to monitor the distance and time they had walked. Finally, one respondent used a smartphone app to track her steps daily.
Adherence of the respondents was very high, with 90% to 100% of smartphone test measurements being performed as instructed and the Fitbit activity tracker being worn for more than 90% of the time. These high adherence rates are representative of the entire participant group of the MS Self study.
The major themes and subthemes that emerged from the interviews are shown in Table 3. Quotations translated from Dutch are used throughout the Results section to illustrate the findings.
Table 3.
Overview of themes and subthemes in relation to the two research questions
| Main theme | Subtheme |
|---|---|
| How do people with MS experience smartphone app and activity tracker in their daily lives? | |
| Increased awareness | Higher awareness of physical status Better disease understanding Higher awareness of MS Data overload |
| Acting on the data | Lifestyle support Pressure to achieve good results Difficulties with data interpretation Difficulties with acting on data |
| What are needs and wishes of people with MS regarding further development and implementation of digital self-monitoring tools for MS? | |
| Personalization | Personalized lifestyle goals Patient-specific tests Flexible use, depending on disease status |
| Providing guidance | Guidance built into smartphone app Guidance by MS health care professionals |
| Integration into treatment plans | A more complete picture of patient Lifestyle as part of treatment plans Personalized treatment plans |
Abbreviations: app, application; MS, multiple sclerosis.
Experiences with Smartphone App and Activity Tracker in Daily Life
Throughout the first interviews we found that respondents already engage in self-management of their MS in daily life, mainly through (online) information seeking and lifestyle measures, including physical exercise and nutrition. Respondents also described the highly variable impact of MS on their daily lives and how they wanted to think as little as possible about the limitations caused by their MS. These findings can be seen as the interpretative framework that shapes the respondents' experiences with the smartphone app and the activity tracker in their daily lives.
Themes
Increased Awareness. Before the MS Self study, some respondents did not have any expectations about the value that the smartphone app and the activity tracker could have for them. Other respondents expected that these self-monitoring tools could provide insight into their physical status.
Indeed, respondents became more aware of their physical status, for example noticing high variability in physical performance between good and bad days, ie, days when their MS had a low or high impact. Although many of the digital self-monitoring insights were confirming what the respondents already knew or thought about their body, new insights were also gained, particularly regarding sleep. Respondent MS2 stated: “Suddenly you get insight into something that has never worried you. You go to bed and you sleep and you wake up and you continue with your day. But now I saw: okay, I went to bed at half past ten and I fell asleep at five past eleven and then I slept very deeply for 2 hours.”
Respondents expressed a positive attitude toward having quantitative data about their physical status, such as their walking performance or sleep quality. They saw these data as an objective measurement that could confirm their feelings. Respondent MS6: “I just really like getting more quantitative data about how I am doing. I think it gives me a lot of peace. Sometimes you notice things, but now you really see that it also comes true. That you are supported a bit in how you are doing.” Moreover, the respondents thought that the increased awareness of their physical status helped them understand their disease better by finding patterns and relationships, for example why on some days they felt more tired or were less active than on other days.
Respondents expressed that the increased awareness of physical status also resulted in a higher awareness of their MS. Respondent MS7: “Because you look at that thing every day. You look at your schemes every day. Because of that you are more concerned with it for a while. Because you know that you move less and can do less than someone else because of the MS.” Having a higher awareness of MS could be quite daunting, for example when respondents were unable to reach their physical activity goals or had lower test scores on days that were heavily influenced by the MS. Also, the daily question “How much influence did MS have on your functioning today?” that was built into the design of the app made respondents more aware of their MS. Because of this question, they had to think about the impact of MS, and they experienced this as something negative because they wanted to focus on their possibilities rather than on their limitations.
Related to the increased awareness brought about by use of the activity tracker and the smartphone app, some respondents experienced data overload, ie, confrontation with too much personal health data. Respondent MS5: “I thought all those data, such as how many hours you sleep and how many calories you burn. I thought that was interesting. But on the other hand, you think: well, sometimes, I really do not want to know it.”
Acting on Data. The respondents found that they were stimulated to act on the digital self-monitoring data. Multiple respondents noticed that the Fitbit data on physical activity and sleep motivated them to increase their physical activity or to go to bed earlier. Respondent MS1: “It was also due to the fact that it was being monitored. That you think: statistically I have had too little sleep. That because of that you are more motivated to go to bed earlier.” Respondents talked about having set lifestyle goals, such as taking a minimum number of steps a day. They liked being challenged to reach these goals and being congratulated by the Fitbit when they reached their targets.
Some respondents experienced pressure to achieve their Fitbit targets or to achieve good results on the walking and cognition tests that were part of the smartphone app. Respondent MS2: “That I thought: but yesterday or 2 days ago I walked much more, so I have to cover the same distance. Then there is a test attached to it and then I think: I have to perform.”
Although the respondents acknowledged that increased awareness of their physical status could result in purposeful actions such as adapting their lifestyle or visiting a health care provider, they also expressed difficulties in acting on the data from the smartphone app and activity tracker. Interpretation of the data proved not to be straightforward. For example, respondents wondered whether a certain test score or a certain sleep pattern was normal or something to worry about. Respondent MS2: “Suddenly you saw your own sleep rhythm. Then I thought: well, is this okay, is this not okay? To whom should I compare this?” Moreover, respondents mentioned that not all insights could be acted on. One respondent, for example, wanted to increase her physical activity based on the self-monitoring data but was physically unable to do so. Another respondent, MS4, became aware that she had poor sleep quality but according to her there was nothing she could do about it: “Well, some things you simply cannot adapt. I simply have to work at a certain time. And you can also not plan when you have to go to the toilet. So, no, there is not a lot that I can do about it.”
Needs and Wishes for Digital Self-monitoring of MS
Five of the seven respondents stated that they were interested in using smartphone apps and activity trackers long-term. All the respondents provided pointers for how to increase the value of digital self-monitoring tools for MS in daily life.
Themes
Personalization. Adapting smartphone apps and activity trackers to the personal situation of the patient was a widespread desire among the respondents. Because of the high heterogeneity in disease course among people with MS, the respondents expected the value of digital self-monitoring in their daily lives to increase when lifestyle goals were personalized and when tests were in line with the symptoms experienced by a specific person with MS. Respondent MS6 noted, “I think that more patient-specific tests might be more beneficial. For one person, it might be the coordination of the hands and, for another, walking distance. So, that there will be more variation and more choice. That you can have a look: what is a good test? What would be good for me?”
Furthermore, the respondents desired flexibility in their use of digital self-monitoring tools. They believed that these tools would be most valuable at times of relapse or recovery. During relapses, self-monitoring could be used to monitor decline, whereas at times of recovery, it could contribute to monitoring progress and setting lifestyle goals. Respondents wanted the intensity of digital self-monitoring to decrease during stable periods of their MS, for example by decreasing test frequency.
Providing Guidance. Because respondents experienced difficulties in acting on the data from the smartphone app and the activity tracker, they desired guidance in this respect. Such guidance could consist of additional insights and advice based on personal data. Suggestions were made to build this guidance into the design of self-monitoring apps, for example providing personal lifestyle advice or showing how one's personal data relate to the data of the general population.
Several respondents mentioned that guidance in acquiring value out of the personal data could also be a task of health care providers. In particular, MS specialist nurses were seen as professionals with whom to discuss the digital self-monitoring data. Respondent MS7: “The neurologist is more 10 minutes like: how are you doing and discussing the MRI for example. And with the MS specialist nurse you are sitting at the table for an hour and she really looks at your daily life and what you could do differently. Which paths to follow to get help and such. Those are simply different conversations.”
Integration into Treatment Plans. In the interviews before and after the MS Self study, respondents expressed that digital self-monitoring would be of more value if it is not used only in a home context but becomes an integral part of treatment plans. The added value for MS health care was seen in the additional information that health care providers would have about their patients. The respondents explained that currently health care providers acquire patient data only during the clinical consultation, through conversations and clinical tests. However, according to the respondents, digital self-monitoring would allow health care providers to obtain a more complete picture of how the patient is doing over time. Respondent MS7: “A neurologist or an MS specialist nurse sees you only a few times a year. When I am with the neurologist, I might be in really good or bad shape. But how has it been over the past half year? That can also give the neurologist insight. Otherwise it is just a snapshot. And now you get better insight over time.”
The additional data provided to MS health care professionals through digital self-monitoring was thought to have a positive effect on treatment plans. First, because digital self-monitoring provides insight into lifestyle and can support a healthy lifestyle, respondents expected more attention to be devoted to lifestyle measures, such as physical exercise and nutrition, in treatment plans. Respondent MS1: “Well, I think that doctors will then also focus more on adapting regular daily things instead of prescribing medication.” The respondents stated that currently lifestyle is an underrepresented topic in MS health care and envisioned a future in which MS health care providers support their patients in achieving lifestyle goals with the help of digital self-monitoring. Second, the respondents expected digital self-monitoring to contribute to the personalization of treatment plans, as MS health care providers would have more information on the specific disease course of someone with MS. Again, this was seen as a positive development because participants thought that current MS health care should become more personalized considering the high interindividual and intraindividual variability in the MS disease course. Respondent MS6: “I do think that you can give better individually targeted advice. Now they are doing it based on the experience of the big group, giving advice, whereas for one person the advice might have to be very different than for another. Nobody with MS follows the same pattern. And that also means that you cannot give general advice. That has to be done individually. And of course, that can be done better when you have all that kind of individual data.”
Discussion
The acceptance of digital self-monitoring through smartphone apps and activity trackers depends on patients with MS experiencing the value of these tools and feeling well equipped to use them in their daily lives. By studying first experiences of people with MS who used a smartphone app and an activity tracker, we gained insight into benefits and difficulties of using these devices for digital self-monitoring in daily life as well as needs and wishes for the further development and implementation of digital self-monitoring tools for MS. The experiences expressed by the present respondents, such as an increased awareness of physical status, feeling motivated to act on the data, and confrontation with being a patient with MS, confirm the findings from a previous study of experiences with self-monitoring in patients with MS.12
Suggested Considerations
Based on the present respondents' experiences with using the smartphone app and the activity tracker and their visions on how they would like these technologies to become embedded in their daily lives, we suggest four considerations for the further development and implementation of digital self-monitoring tools for MS.
First, the data from the smartphone app and the activity tracker evoked emotional responses. Respondents disliked being confronted with their MS, and some felt pressure to achieve lifestyle targets or good test results. This is in line with findings from interviews with patients with multiple chronic diseases who engaged in self-monitoring.9 As noted by these authors, self-monitoring data can be emotionally charged, and patients may attribute positive or negative moral meanings to these data, such as judging their data as “good” or “bad.” When self-monitoring data have a negative emotional impact, this might hamper the adoption of digital self-monitoring tools by people with MS. Therefore, it is important to explore how digital self-monitoring tools for MS could be developed in such a way that emotional burden is reduced, for example by developing these tools in close collaboration with patients.6,9
Second, to continue using tools such as smartphone apps and activity trackers in their daily lives, the respondents desired monitoring of patient-specific parameters and flexibility in using these tools, depending on disease status. In a similar vein, a review on user perspectives of self-monitoring apps concluded that customization options increase apps' usability and decrease their user burden.6 Furthermore, in a study on the attitudes of patients with MS and health care providers toward smartphone apps for monitoring physical activity, customization was mentioned as a facilitator for the adoption of such apps.11 This finding suggests that to increase usefulness and user friendliness, digital self-monitoring tools for MS should be adaptable to the patient's personal situation. Considering the high variety in MS, both within and between patients, a one-size-fits-all approach will likely not lead to long-term adherence to digital self-monitoring technologies by people with MS. Moreover, when these technologies can be adapted to the patient's specific context, this might enable people with MS and their health care providers to use digital self-monitoring as a tool to personalize the patient's treatment.6
Third, the respondents expressed difficulties in interpreting and acting on the data from the smartphone app and the activity tracker. Therefore, they would like to receive guidance, both by the technology itself and by health care providers, to maximize the value of digital self-monitoring data in their daily lives. As has been suggested by a focus group study with potential users of digital health technologies, self-monitoring data need to be placed into context and given meaning.21 Apparently, simply tracking and presenting data to a patient is not enough to capitalize on the value of digital self-monitoring tools.22 To make self-monitoring data more actionable in the everyday lives of people with MS, features such as additional information and support could be built into the design of self-monitoring apps.21
Last, the respondents not only wanted to use tools such as smartphone apps and activity trackers in their home context but also envisioned these tools as part of clinical treatment plans. Similarly, a recent study on the experiences of cancer survivors with smartphone apps to stimulate physical activity showed that the uptake of such apps was expected to increase when these would be integrated into existing care pathways and recommended by health care providers.23 This finding implies that patients' motivation to continue digital self-monitoring in their daily lives is strengthened when technologies are integrated into clinical workflows.6
For the integration of digital self-monitoring tools into clinical workflows to be successful, health care providers should be motivated and facilitated to use these tools.24 Therefore, attention should be devoted to the needs and wishes of MS health care providers.10 For example, how do MS health care providers want patient-generated data to be presented? A possible solution is to upload digital self-monitoring data into electronic medical records so that these data are readily accessible to health care providers.25–27 Other interesting questions include what data are deemed valuable by MS health care providers and what skills and knowledge they need to deal with the changing practices brought about by digital self-monitoring.
Study Limitations
Although this exploratory study provides valuable in-depth insights into the experiences, needs, and wishes of people with MS regarding digital self-monitoring through smartphone apps and activity trackers, we acknowledge that the study group is not representative of the broader MS patient population. First, the sample is small, and additional perspectives might have been gained by interviewing more MS Self study participants. Nevertheless, it has been shown that from as few as six interviews overarching themes can be distilled,28 and this was also the case in this study. Second, we interviewed only female participants, meaning that the perspective of male patients with MS remained unexplored. In fact, of the 24 MS Self study participants, only two were male. This can partly be explained by the fact that MS, and especially RRMS, is more common in females than in males.29 Third, because only patients with RRMS were studied, the results do not per se apply to patients with progressive forms of MS.
Furthermore, some remarks are required regarding the study design. First, the interviews were conducted by telephone rather than face-to-face. We are aware that the absence of visual cues can affect the interpretation of responses, as certain contextual and nonverbal data are missing. However, data from telephonic interviews are not necessarily lower in quality than data from face-to-face interviews.30 Second, the current interviews explored the experiences of people with MS who had been using a smartphone app and an activity tracker for a relatively short period of 4 weeks. Therefore, we gained insight into short-term experiences only, whereas experiences might well change when these tools are used for a longer period. Third, the perceptions of the respondents might have been affected by the fact that they used digital self-monitoring in the first place to generate data for validation of the smartphone app and the activity tracker and not with the explicit aim to engage in monitoring of their own health. Finally, we acknowledge that the experiences of the respondents might have been influenced by the specific form of digital self-monitoring that has been used in the MS Self study, through a smartphone app and an activity tracker. This form of self-monitoring consisted of continuous (activity tracker) and high frequency (smartphone app) monitoring, whereas experiences might be different when the self-monitoring measurements are less frequent.
Conclusion
The aforementioned considerations could help in better aligning the development and implementation of digital self-monitoring tools, such as smartphones and activity trackers, with patients' perspectives. When the needs, wishes, and experiences of patients are articulated, as has been the case in this study, these can function as pointers for the embedding of digital self-monitoring tools into the daily lives of people with MS.
PRACTICE POINTS
Digital self-monitoring of health in people with MS through smartphone apps and activity trackers could support self-management of MS and contribute to personalized health care. However, the acceptance of smartphone apps and activity trackers by patients depends on them experiencing the value of these tools and feeling well equipped to use the tools in their daily lives.
After using an activity tracker and a smartphone app for 4 weeks, people with MS reported feeling ambivalent about them. They valued being supported in the self-management of MS but also experienced challenges, such as confrontation with their disease and difficulties with data interpretation.
To increase the value of digital self-monitoring of MS through activity trackers and smartphone apps, it is recommended that these tools 1) are adaptable to the patient's personal situation, 2) support patients in making sense of the self-monitoring data, and 3) become integrated into clinical treatment plans.
Financial Disclosures
Dr. van Oirschot is employed by Orikami/MS sherpa BV (manufacturer of the Mijn Kwik app). Dr. Jongen received honoraria from Bayer for educational or consultancy activities and from MS sherpa BV for consultancy activities. The other authors declare no conflicts of interest.
Funding/Support
This work received financial support from the Dutch National MS Foundation, the Netherlands Organisation for Scientific Research (NWO Data2Person Project 628.011.025), and the European Regional Development Fund (EFRO OPOost Project 00217).
References
- 1.Marziniak M, Brichetto G, Feys P et al. The use of digital and remote communication technologies as a tool for multiple sclerosis management: narrative review. JMIR Rehabil Assist Technol. 2018;5:e5. doi: 10.2196/rehab.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lupton D. Quantifying the body: monitoring and measuring health in the age of mHealth technologies. Crit Public Health. 2013;23:393–403. [Google Scholar]
- 3.Tomlinson M, Rotheram-Borus MJ, Szwartz L, Tsai AC. Scaling up mHealth: where is the evidence? PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001382. e1001382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.West P, Van Kleek M, Giordano R et al. Information quality challenges of patient-generated data in clinical practice. Front Public Health. 2017;5:284. doi: 10.3389/fpubh.2017.00284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun R, McGinnis R, Jacob J. Novel technology for mobility and balance tracking in patients with multiple sclerosis: a systematic review. Expert Rev Neurother. 2018;18:887–898. doi: 10.1080/14737175.2018.1533816. [DOI] [PubMed] [Google Scholar]
- 6.Birkhoff SD, Smeltzer SC. Perceptions of smartphone user-centered mobile health tracking apps across various chronic illness populations: an integrative review. J Nurs Scholarsh. 2017;49:371–378. doi: 10.1111/jnu.12298. [DOI] [PubMed] [Google Scholar]
- 7.Piwek L, Ellis DA, Andrews SA, Joinson A. The rise of consumer health wearables: promises and barriers. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1001953. e1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabriels K, Moerenhout T. Exploring entertainment medicine and professionalization of self-care: interview study among doctors on the potential effects of digital self-tracking. J Med Internet Res. 2018;20:e10. doi: 10.2196/jmir.8040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ancker JS, Witteman HO, Hafeez B et al. You get reminded you're a sick person: personal data tracking and patients with multiple chronic conditions. J Med Internet Res. 2015;17:e202. doi: 10.2196/jmir.4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Griffin N, Kehoe M. A questionnaire study to explore the views of people with multiple sclerosis of using smartphone technology for health care purposes. Disabil Rehabil. 2018;40:1434–1442. doi: 10.1080/09638288.2017.1300332. [DOI] [PubMed] [Google Scholar]
- 11.Giunti G, Kool J, Rivera Romero O, Dorronzoro Zubiete E. Exploring the specific needs of persons with multiple sclerosis for mHealth solutions for physical activity: mixed-methods study. JMIR Mhealth Uhealth. 2018;6:e37. doi: 10.2196/mhealth.8996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayobi A, Marshall P, Cox AL Quantifying the Body and Caring for the Mind: Self-Tracking in Multiple Sclerosis. Paper presented at: CHI 2017; Denver, CO. May 6–11, 2017. [Google Scholar]
- 13.Van Oirschot P, Heerings M, Wendrich K et al. Self-monitoring of mobility, signal processing speed, physical activity and sleep by persons with multiple sclerosis. Mult Scler. 2018;24:366. [Google Scholar]
- 14.Meyer-Moock S, Feng YS, Maeurer M et al. Systematic literature review and validity evaluation of the Expanded Disability Status Scale (EDSS) and the Multiple Sclerosis Functional Composite (MSFC) in patients with multiple sclerosis. BMC Neurol. 2014;14:58. doi: 10.1186/1471-2377-14-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kieseier BC, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012;18:914–924. doi: 10.1177/1352458512444498. [DOI] [PubMed] [Google Scholar]
- 16.Sonder JM, Burggraaff J, Knol DL et al. Comparing long-term results of PASAT and SDMT scores in relation to neuropsychological testing in multiple sclerosis. Mult Scler. 2014;20:481–488. doi: 10.1177/1352458513501570. [DOI] [PubMed] [Google Scholar]
- 17.Sebastião E, Sandroff BM, Learmonth YC, Motl RW. Validity of the Timed Up and Go Test as a measure of functional mobility in persons with multiple sclerosis. Arch Phys Med Rehabil. 2016;97:1072–1077. doi: 10.1016/j.apmr.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 18.Abraham L, Hareendran A, Mills IW et al. Development and validation of a quality-of-life measure for men with nocturia. Urology. 2004;63:481–486. doi: 10.1016/j.urology.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 19.Dutta R, Trapp BD. Relapsing and progressive forms of multiple sclerosis: insights from pathology. Curr Opin Neurol. 2014;27:271–278. doi: 10.1097/WCO.0000000000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15:398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 21.Miyamoto SW, Henderson S, Young HM et al. Tracking health data is not enough: a qualitative exploration of the role of healthcare partnerships and mHealth technology to promote physical activity and to sustain behavior change. JMIR Mhealth Uhealth. 2016;4:e5. doi: 10.2196/mhealth.4814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiauzzi E, Rodarte C, DasMahapatra P. Patient-centered activity monitoring in the self-management of chronic health conditions. BMC Med. 2015;13:77. doi: 10.1186/s12916-015-0319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roberts AL, Potts HWW, Koutoukidis DA et al. Breast, prostate, and colorectal cancer survivors' experiences of using publicly available physical activity mobile apps: qualitative study. JMIR Mhealth Uhealth. 2019;7 doi: 10.2196/10918. e10918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gagnon MP, Ngangue P, Payne-Gagnon J, Desmartis M. m-Health adoption by healthcare professionals: a systematic review. J Am Med Infrom Assoc. 2016;23:212–220. doi: 10.1093/jamia/ocv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu H, Colgan J, Reddy M, Choe EK. Sharing patient-generated data in clinical practices: an interview study. AMIA Annu Symp Proc. 2017;2016:1303–1312. [PMC free article] [PubMed] [Google Scholar]
- 26.Dunn J, Runge R, Syder M. Wearables and the medical revolution. Per Med. 2018;15:429–448. doi: 10.2217/pme-2018-0044. [DOI] [PubMed] [Google Scholar]
- 27.Wang J, Chu CF, Li C. Diabetes educators' insights regarding connecting mobile phone- and wearable tracker-collected self-monitoring information to a nationally-used electronic health record system for diabetes education: descriptive qualitative study. JMIR Mhealth Uhealth. 2018;6 doi: 10.2196/10206. e10206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guest G, Bunce A, Johnson L. How many interviews are enough? an experiment with data saturation and variability. Field Method. 2006;18:59–82. [Google Scholar]
- 29.Harbo HF, Gold R, Tintore M. Sex and gender issues in multiple sclerosis. Ther Adv Neurol Disord. 2013;6:237–248. doi: 10.1177/1756285613488434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Novick G. Is there a bias against telephone interviews in qualitative research? Res Nurs Health. 2008;31:391–398. doi: 10.1002/nur.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]


