Abstract
Obesity prevalence is rapidly increasing worldwide. With the discovery of brown adipose tissue (BAT) in adult humans, BAT activation has emerged as a potential strategy for increasing energy expenditure. Recently, the presence of a third type of fat, referred to as beige or brite (brown in white), has been recognized to be present in certain kinds of white adipose tissue (WAT) depots. It has been suggested that WAT can undergo the process of browning in response to stimuli that induce and enhance the expression of thermogenesis: a metabolic feature typically associated with BAT. MicroRNAs (miRNAs) are small transcriptional regulators that control gene expression in a variety of tissues, including WAT and BAT. Likewise, it was shown that several food compounds could influence miRNAs associated with browning, thus, potentially contributing to the management of excessive adipose tissue accumulation (obesity) through specific nutritional and dietetic approaches. Therefore, this has created significant excitement towards the development of a promising dietary strategy to promote browning/beiging in WAT to potentially contribute to combat the growing epidemic of obesity. For this reason, we summarize the current knowledge about miRNAs and food compounds that could be applied in promoting adipose browning, as well as the cellular mechanisms involved.
Keywords: miRNAs, browning, BAT, WAT, food compounds
1. Brown and Beige Adipose Tissue in Energy Balance
BAT is a type of adipose tissue characterized by multilocular lipid droplets, the abundance of mitochondria, and a high rate of fatty acid oxidation and glucose uptake. It secretes batokines and exhibits endocrine, paracrine, and autocrine actions. In addition, it plays an important role in energy expenditure and non-shivering thermogenesis and is considered to have potential implications for the treatment of obesity [1].
Moreover, brown adipocyte-like cells, beige or brite adipocytes, are a specialized cell type derived from white-adipocyte precursor cells that display thermogenic capacity [2]. Functionally, brite adipocytes have the ability to efficiently oxidize glucose and lipids [3] to produce heat under certain stimuli [4] (see Figure 1 and below). Further, providing their thermogenic capacity, stimulation of these brite adipocytes (widely known as beiging or browning) has eventually been considered as an interesting strategy against excessive energy accumulation observed in obesity [5]. From a morphological point of view, brite adipocytes appear within white adipose tissue depots (mainly in the subcutaneous depot), have multilocular smaller lipid droplets (as compared to white adipocytes), display medium mitochondrial density, and express (inducible) uncoupling protein-1 (Ucp-1) [2].
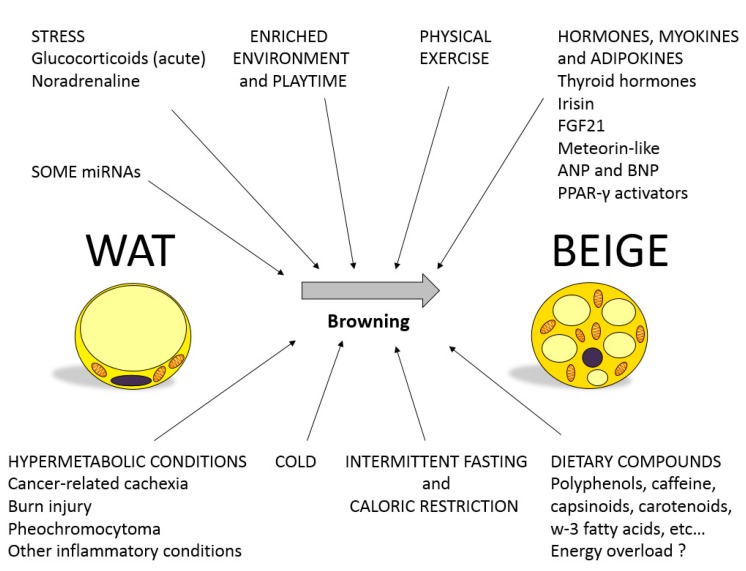
Figure 1.
Most relevant environmental, behavioral, and physiological factors that regulate white adipose tissue (WAT) browning. miRNAs, microRNAs; FGF21, Fibroblast growth factor 21; ANP, atrial natriuretic peptide; BNP, brain-type natriuretic peptide; PPAR-γ, Peroxisome proliferator-activated receptor gamma.
The myogenic factor 5 (Myf5) give rise to brown adipocytes and also a subset of white adipocytes. Individual brown and white adipocytes contain a mixture of adipocyte progenitor cells derived from Myf5+ and Myf5neg lineages, which varies depending on the depot location [6]. Thus, adipose tissue development towards a more white/brite phenotype depends on a complex interaction/combination between environmental and transcriptional factors, including epigenetic mechanisms such as miRNAs [7] and dietary bioactive compounds such as polyphenols [8].
As explained in Figure 1, multiple factors have been related to browning activation in WAT [4], a negative energy balance being a common trait to many of them. Among the most relevant ones, this includes physical exercise, cold, stress hormones (noradrenaline and glucocorticoids), caloric restriction, and intermittent fasting. In this context, it has been speculated whether, in some cases, WAT browning is a negative adverse side effect given that it has been observed in severe-wasting situations such as burn-injured individuals, cancer-associated cachexia, or pheochromocytoma [9]. However, in general, the browning process is considered a promising strategy to revert the positive energy balance typical of obesity, and many studies have been devoted in the last years to study hormones, miRNAs, and physiological stimuli (i.e., physical activity and social stimulation) that are able to activate browning, including also dietary compounds that are involved in trans-differentiation from white to beige adipocytes.
2. MicroRNAs as Regulators of Gene Function and Metabolism
MiRNAs are non-coding ribonucleotid acid (RNA) molecules that regulate gene expression. To clarify, MiRNAs are short, approximately 20 to 22 nucleotides in length, double stranded RNAs that usually down-regulate gene expression at the post-transcriptional level [10]. For the last decade, many hundreds of miRNAs have been identified with highly conservative sequences between species. Moreover, this high conservation degree shows important roles of miRNAs in the regulation of tissue development, phenotype, and cell physiology [11], including adipose tissue [12,13,14].
In most cases, miRNAs repress gene transcription through specific and direct interaction of miRNA and mRNA. This miRNA–mRNA interaction is based on base pair complementarity, and usually, miRNAs interact with target mRNAs at their 3′UTR region [10,11]. However, other non-canonical regions for miRNA interaction have also been described, such as the coding region or the 5′UTR [15]. The canonical miRNA mechanism of action involves a perfect base pair complementarity within the “seed” sequence, framed within base pairs 2–8 of the mature miRNA strand, with the target mRNAs sequence. Additionally, some mismatches could be present within the non-seed sequence of the miRNA strand for the regulation of gene transcription. Indeed, one single miRNA can regulate many mRNAs, and at the same time, one mRNA could be regulated by several miRNAs and, thus, affect different cell functions [10,11,16,17,18]. Even so, this suggests that miRNAs constitute a wide and open system for transcriptional regulation of gene expression in mammals. The biological impact of gene transcription regulation through miRNAs demonstrates the plasticity of this system to finely tune gene expression under environmental changes.
3. Involvement of miRNAs in the Regulation of Browning: Role of Nutritional Factors
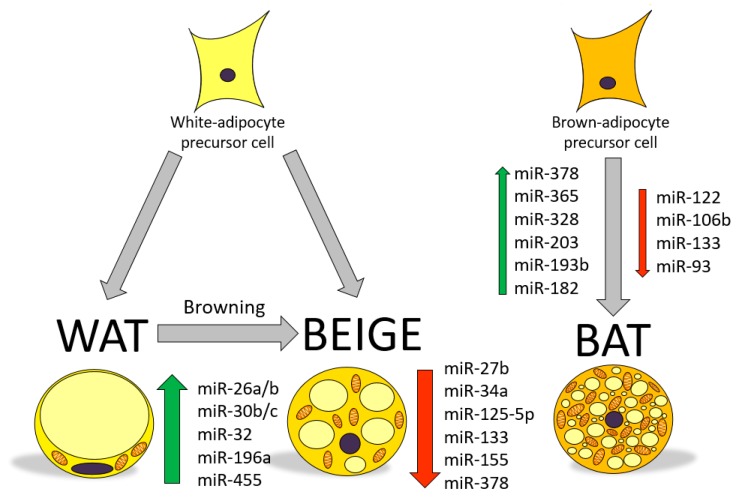
In recent years, many studies have demonstrated the involvement of miRNAs in the regulation of adipose tissue function and adipose tissue formation (adipogenesis) [12,13,19]. Of particular relevance, miRNAs regulating brite adipocyte development and function have been a topic of interest for obesity research [20]. Therefore, identification of specific miRNAs regulating brite/brown adipocyte function could be envisaged as a potential therapeutic tool to improve the excess of WAT associated to obesity and to stimulate energy dissipation as heat [21]. The role of miRNAs in the modulation of browning relies on their ability to tiny regulate gene transcription, while some miRNAs have been found to be positive regulators of brite/brown adipocytes (activators), others have shown to be potent inhibitors of adipocyte browning [22,23]. Figure 2 displays some of the miRNAs found to regulate brite/brown function that are briefly described in this review.
Figure 2.
MicroRNAs involved in WAT browning and beige and brown adipocyte regulation. ↑, upregulated; ↓, downregulated.
Importantly, several studies have also shown that nutritional and dietary factors could influence miRNAs associated with browning, thus, potentially contributing to the treatment of excessive adipose tissue accumulation (obesity) through specific nutritional and dietetic approaches. Table 1 and Table 2 illustrate the most important nutritional factors that regulate browning as well as brown and brite adipocyte-related miRNAs, respectively, as observed in human samples and cells. Table 3 shows additional information about these miRNAs in animal and murine cell models.
Table 1.
Main miRNAs involved in brown adipocyte regulation and nutritional factors that regulate their expression in human samples/cells.
| Effect on Browning | miRNA | Model and/or Tissue Sample | Nutritional Factors | Effect of the Nutritional Factor on the Expression of the miRNA | Reference |
|---|---|---|---|---|---|
| Positive (+) | |||||
| 203 | Human colon adenocarcinoma cells (Caco-2) | Selenium (depletion/accurate levels) | ↓ miR-203 expression in Se depletion | [24] | |
| 193b | Human plasma | Weight loss dietary treatment (RESMENA trial) | ↑ miR-193b levels (and hypomethylated) in high responders to weight loss | [25] | |
| 365 | Human adipocytes | Obesity/adipose (WAT) hypertrophy | ↑ miR-365 in WAT hypertrophy | [26] | |
| Negative (−) | |||||
| 106b | Lung cancer cells | Seed procyanidin extract (GSE) cells | ↓ miR-106b in lung neoplastic cells | [27] | |
| LT97 cells (colon adenoma cells) | Butyrate (and trichostatin A) as histone deacetylase inhibitors | ↓ miR-106b levels: affects cycle-relevant genes and thus, cell proliferation | [28] | ||
| Plasma | Hyperlipidemia status/coronary artery disease (CAD) | ↓ miR-106b in patients with CAD. MiR-106b levels positively correlate with HDL-c & ApoA-I |
[29] | ||
| Human colon adenocarcinoma cells (Caco-2) | Selenium (depletion/accurate levels) | ↓ miR-106b expression in Se depletion | [24] | ||
| HCT116 (colon cancer cells) | Butyrate (short chain FA) | ↓ miR-106b expression | [30] | ||
| Prostate cancer cells | Resveratrol treatment | ↓ miR-106b expression | [31] | ||
| 93 | Human hepatocellular carcinoma (HCC) | Nonalcoholic fatty liver disease (NAFLD) | ↑ miR-93 expression | [32] | |
| Human colon adenocarcinoma cells (Caco-2) | Low-selenium environment | ↓ miR-93 expression levels in low selenium | [33] | ||
| 122 | Exosomes from healthy males aged 20–30 y.o. | Fat mass/BAT activity | ↓ Exosomal miR-122-5p levels in high BAT activity group. Exosomal miR-12anti-obesityp correlates negatively with: BAT activity, serum HDL-cholesterol. Exosomal miR-122-5p correlates positively with: age, BMI, body fat mass, total cholesterol, and serum triglycerides. |
[34] | |
| Plasma | Type 2 diabetes with/without NAFLD | ↑ miR-122 expression in T2DM patients with NAFLD as compared to those without NAFLD | [35] | ||
| Serum | Breast cancer patients (survivors) with different BMI ranges (obesity, weight gain) | miR-122 expression associated with BMI | [36] | ||
| Liver samples | Patients with alcoholic liver diseases (ALD) | miR-122 levels ↓ in liver samples from ALD patients ↑ levels of miR-122 target HIF1-α |
[37] | ||
| Liver samples | Obese women following bariatric surgery with or without NAFLD | ↓ miR-122 in obese subjects with NAFLD ↓ miR-122 in liver associated with impaired FA usage |
[38] | ||
| Plasma | Maternal (pre-gestational and gestational) obesity | ↓ miR-122 levels in pre-gestational obesity and gestational obesity | [39] | ||
| Human liver cancer cells (HepG2) | Flavonoid compounds (nobiletin, tangeretin, and hesperidin) from citrus peel | ↓ miR-122 expression and thus, affect FAS and CPT-1α, decreasing lipid accumulation | [40] | ||
| Serum and plasma | Individuals with risk factors for metabolic syndrome, T2D, CVD (Bruneck study) | Circulating miR-122 associated with ↑ levels of liver enzymes, adiposity, inflammation, and insulin resistance and an adverse lipid profile Circulating miR-122 levels correlated with lipid subspecies (monounsaturated and saturated fatty acids) and cholesterol esters | [41] |
↑, upregulated; ↓, downregulated.
Table 2.
Main miRNAs involved in brite adipocyte regulation and WAT browning and nutritional factors that regulate their expression in human samples/cells.
| Effect on Browning | miRNA | Tissue Sample | Nutritional Factor | Effect of the Nutritional Factor on the Expression of the miRNA | Reference |
|---|---|---|---|---|---|
| Positive (+) | |||||
| 196a (specific) | Pancreatic cancer cells | Dietary phytochemicals (garcinol) | Modulated miR-196a expression | [42] | |
| 26a/b | Formalin-fixed paraffin-embedded lung cancer (144 adenocarcinomas and 120 squamous cell carcinomas) | Intake of quercetin-rich foods (evaluated through a food-frequency questionnaire) | miR-26 expression differentially expressed between highest and lowest quercetin consumers | [43] | |
| Liver (human) | HFD/obesity | ↓ miR-26 expression | [44] | ||
| 32 | Healthy human colorectal epithelium | Non-digestible carbohydrates (resistant starch and polydextrose) supplementation | ↑ miR-32 expression in rectal mucosa | [45] | |
| 455 | Human adipose tissue and blood cells | Obesity & T2D (computational framework miR-QTL-Scan) | BAT specific miR-455 play a role in adipogenesis | [46] | |
| Human adipose tissue (BAT and WAT) from neck | HFD/Obesity and cold-induced thermogenesis | MiR-455 identified as a BAT marker in humans | [47] | ||
| Negative ( − ) | |||||
| 125-5p (specific) | Blood from T2DM and obese patients | Meta-analysis including lifestyle intervention studies | ↓ miR-125-5p in obese patients | [48] | |
| 34a | Human sc WAT (48 subjects) | Three calorie-restricted diets (different amount and quality of carbohydrates): low glycemic index, high glycemic index, and low fat | ↓ miR-34a in waist circumference stratified (tertiles) cohort No changes on miRNA levels between the intervention groups. |
[49] | |
| Liver of male Sprague-Dawley rats | High-fat high-cholesterol (WD) diet supplemented with fish oil (FOH) | ↓ miR-34a in FOH vs. WD | [50] | ||
| Huh-7 (human liver) cells | Cholesterol accumulation associated to nonalcoholic fatty liver disease (NAFLD) | ↑ miR-34a expression in liver | [51] | ||
| 155 | THP-1 (human) monocytes/macrophages | Oleic acid | ↑ miR-155 expression in monocytes (vs. DHA) | [52] | |
| 378 | Patients with NASH (liver biopsies) Human HepG2 with accumulated lipid (oleate) |
N.A. Oleate |
↑ miR-378 expression ↑ miR-378 expression |
[53,54] | |
| Muscle biopsies of healthy males | Single bout of concurrent resistance exercise (8 × 5 leg extension, 80% 1RM) + 30 min at ~70% VO2peak with either post-exercise (whey) protein (25 g) or placebo | ↑ miR-378 expression at 4 h post-exercise with protein | [55] |
↑, upregulated; ↓, downregulated.
Table 3.
Main miRNAs involved in brown adipocyte regulation and nutritional factors that regulate their expression in animal and murine cell models.
| Effect on browning | miRNA | Tissue sample | Nutritional factor | Effect of the nutritional factor on the expression of the miRNA | Reference |
|---|---|---|---|---|---|
| Positive (+) | |||||
| 196a (specific) | Adipose tissue (sc and visceral) of lambs | DHA-G diet: barley-based finishing diet where algae meal (DHA-Gold; Schizochytrium spp.) replaced flax oil | ↑ miR-196a expression in SAT vs. PAT (perirenal) in DHA-G diet. Differential miRNA expression in each tissue depot depending on diet |
[56] | |
| Bovine adipose tissue (sc and visceral) from cattle | HFD | ↓ miR-196a in HFD and higher expression in visceral tissue depot | [57] | ||
| 26a/b | Goat milk | Milk (fatty acid) composition | miR-26 expression associated with total fat yield and short-, medium and long-chain fatty acid content. No association with lactose or milk protein content. Positive correlation miR-26a family and C16:1 and C18:3 in milk fat. |
[58] | |
| Liver and adipose tissue (pregnant) rats | Diets with different fatty acid types: soybean (SO), olive (OO), fish (FO), linseed (LO), or palm-oil (PO) diets from conception to day 12 of gestation and standard diet thereafter | MiR-26 (among others) differentially modulated by the different fatty acids during early pregnancy. | [59] | ||
| Liver (human) & mice | HFD/obesity | ↓ miR-26 expression (humans and two obesity mice models) | [44] | ||
| 30b/c | Cortex and cerebellum of middle-aged C57Bl/6J mice | Extra-virgin olive oil rich in phenols feeding for 6 months (H-EVOO, phenol dose/day: 6 mg/kg) vs. the same olive oil deprived of phenolics (L-EVOO) | ↓ miR-30 expression in H-EVOO ↑ miRNAs in old L-EVOO animals compared to young. |
[60] | |
| Rainbow trout eggs | Trout egg quality and production (characterization of miRNA profile) | miR-30 among top-10 most abundant miRNAs | [61] | ||
| Mice adipose tissue macrophages (ATMs) | HFD (12 wk) in combination with CB1 antagonist AM251 (4 wk, 10 mg/kg) | ↑ miR-30e-5p in ATMs from HFD + AM251 mice | [62] | ||
| Male C57BL/6J mice | HFD (16 wk) | ↓ miR-30a, -30c, -30e expression in ATM from HFD mice vs. NCD through epigenetic (methylation) modifications | [63] | ||
| 455 | Male C57BL/6J (B6) mice | HFD (45% kcal fat) supplemented with EPA (6.75% kcal EPA) for 11 wk. | ↑ miR-455 expression in BAT | [64] | |
| Murine adipose tissue (BAT and WAT) | HFD/Obesity and cold-induced thermogenesis | MiR-455 identified as a BAT marker in rodents | [47] | ||
| Negative ( − ) | |||||
| 27b | Milk samples from rats (lactation) | Cafeteria and post-cafeteria diet | MiR-27 levels in milk decrease throughout lactation. | [65] | |
| Cortex and cerebellum of middle-aged C57Bl/6J mice | Extra-virgin olive oil rich in phenols feeding for 6 months (H-EVOO, phenol dose/day: 6 mg/kg) vs. the same olive oil deprived of phenolics (L-EVOO) | ↓ miR-27 levels in H-EVOO | [60] | ||
| 34a | Breast cancer cells and carcinogenesis model in rats | 3,6-dihydroxyflavone (flavonoid) | ↑ miR-34a in breast carcinogenesis | [66] | |
| Liver of male Sprague-Dawley rats | High-fat high-cholesterol (WD) diet supplemented with fish oil (FOH) | ↓ miR-34a in FOH vs. WD | [50] | ||
| Mice liver | Three dietary interventions affecting lifespan (LS): caloric restriction (CR), low fat or high fat plus voluntary exercise or 30% CR | ↑ miR-34a in livers of two models of obesity MiR-34a fold change negatively correlated with LS |
[67] | ||
| Mouse pancreatic β-cells | Saturated fatty acids | ↑ miR-34a expression | [68,69] | ||
| 133 | C57BL/6 male mice | High fat diet concomitant with miR-133 ASO (anti-miR-133) | ↑ miR-133 expression in HFD ↓ miR-133 expression in cold-exposed mice HFD and miR-133 antagonism ↑ BAT activity |
[70] | |
| 155 | 3T3-L1 (mouse) adipocytes | Resveratrol (25 µM) | ↑ miR-155 expression | [71] | |
| FVB mice (colon mucosa) | High fat diet (45%) and 30% caloric restriction (CR) | ↑ miR-155 expression in colon mucosa in HFD mice | [72] | ||
| RAW264.7 macrophages (LPS activated) | 10 µM quercetin, quercetin-3-glucuronide (Q3G) and isorhamnetin | ↓ miR-155 expression by quercetin and Q3G | [73] | ||
| 378 | Livers of dietary obese mice | HFD (60% cal.) | ↑ miR-378 expression | [53,54] | |
| Milk samples from dairy cows in mid lactation | Control diet (total mixed ration of corn:grass silages) for 28 days followed by a treatment period (control diet supplemented with 5% linseed or safflower oil) of 28 days. | ↑ miR-378 expression by both treatments | [74] | ||
| Mice livers Mouse primary hepatocytes |
Fasting & re-feed Palmitic acid (PA), linoleic acid (LA), oleic acid (OA) |
↑ miR-378 expression in fasting & ↓ miR-378 upon re-feeding ↑ miR-378 expression |
[29] | ||
| Mice liver | Fisetin (a flavonoid): normal diet, HFD, HFD + fisetin | ↑ miR-378 expression by HFD & ↓ miR-378 by fisetin sup. | [75] | ||
| Mice brown adipocytes Brown fat (BAT) from mice |
Omega-3 eicosapentaenoic acid (EPA) Low fat diet (LF), iso-caloric high fat (HF, 50% cal.) enriched with palm oil (HF + PO), olive oil (HF + OO), fish oil (HF + FO) for 12 wk. |
↑ miR-378 expression by EPA during brown differentiation ↑ miR-378 expression in iBAT from mice treated with HF + FO vs. HF + OO or HF + PO. |
[76] |
↑, upregulated; ↓, downregulated.
4. Food Compounds Related to the Browning Process
Evidence has shown that some food compounds could be promising candidates to target different molecular mechanisms and dietary strategies in the management of obesity, and, even more, some of them have the potential ability to promote the browning process in WAT. For instance, some of the most studied compounds are spices, green tea, polyunsaturated fatty acids (PUFA´s), carotenoids, and citrus fruits, among others.
4.1. Spices
4.1.1. Chili Peppers
Capsaicin (trans-8-methyl-N-vanillyl-6-nonenamide) is a bioactive component of chili peppers [77,78], and is also the major pungent component of red-hot chili peppers. Additionally, chili peppers contain non-pungent capsinoids analogs, which include: capsiate, dihydrocapsiate, and nordihydrocapsiate [78,79]. It is widely accepted that capsaicin and capsinoids activate BAT and increase thermogenesis, as well as energy expenditure in both rodents and humans [79,80,81,82]. In addition, there is increasing evidence regarding the browning effect of capsaicin and capsinoids.
Baboota et al. [83] reported that male Swiss albino mice fed a high-fat diet (HFD) receiving 2 mg/kg body weight of capsaicin (orally administered on alternate days; capsaicin was dissolved in 0.9% saline with 3% ethanol and 10% Tween 80) for 12 weeks had an induction of the browning phenotype in subcutaneous WAT, but not in the visceral WAT, and showed increased on thermogenesis and mitochondrial biogenesis genes expression in BAT.
Baboota et al. [84] also showed that 3T3-L1 adipocytes treated with 1 µM of capsaicin increased the expression of Ucp-1, Pgc-1α, Prmd16, Dio2, Pparα, and Foxc2, not only suggesting that capsaicin induced a brown-like phenotype but that this effect was via the transient receptor potential vanilloid subfamily 1 (TRPV1)-dependent mechanism.
Baskaran et al. [85] confirmed in mice that the activation of TRPV1 channels by capsaicin triggers browning of WAT. Adult male TRPV1-/- mice were fed an HFD with added capsaicin (0.01%) from week 6 to week 32. Dietary capsaicin increased the expression of Ucp-1, Pgc-1α, Sirt-1, and Prdm16 in WAT wild type mice. Hence, capsaicin had no effect on the expression of these genes in TRPV1-/- mice. Thus, TRPV1 protein may have a central role in capsaicin-mediated browning of WAT.
Mosqueda et al. [86] described that adult male Wistar rats that were fed a Western diet for eight weeks and treated daily with capsaicin (4 mg/kg/day) induced in retroperitoneal WAT the emergence of multilocular brown-like adipocytes that were positive for UCP-1 and CIDEA. In addition, the increased expression of Prdm16 was observed in the inguinal WAT of these animals.
Fan et al. [87] reported that mature 3T3-L1 adipocytes were tested with a combination of capsaicin (25 µM) and capsiate (25 µM) for 48 h increased the expression of Tbx1, Tmem26, Cd40, Ucp-1, and Prdm16, in 3T3-L1 adipocytes and also increased the protein levels of UCP-1, PGC-1α, and PRMD16. The induction of browning in white adipocytes by a combination of capsaicin and capsiate could be mediated via activation of the peroxisome proliferator-activated receptor gamma/beta3 adrenoreceptors (PPARγ/β3-AR) signaling pathway.
Ohyama et al. [88] described a synergistic anti-obesity effect by a combination of capsinoids and mild cold exposure promoting beige adipocyte biogenesis. Adult male C57BL/6J mice were fed a high-fat diet with 0.3% (w/w) of capsinoids (62.7% of capsiate, 32.2% of dihydrocapsiate, and 5.5% nordihydrocapsiate) for eight weeks. Due to a mild cold exposure, 17% of these animals had increased expression of Ucp-1, Pgc-1α, and Cidea, in the inguinal WAT when compared with vehicle-treated mice and mice kept under room temperature. Cells treated with nonivamide (the less pungent capsaicin-analog), decreased the adipogenesis process through an increase in the expression of the miRNA mmu-let7d-5p, which has been associated with decreased PPARg levels [89].
4.1.2. Turmeric
Curcumin is a polyphenol isolated from the rhizomes of the plant Curcuma longa, commonly known as turmeric, a member of the ginger family (Zingiberaceae). It is widely used as a spice in Asian cuisine [90,91]. Curcumin is practically insoluble in water [92] and has poor absorption into the gastrointestinal tract in rats, displaying a low oral bioavailability [93]. In vitro and animal studies support the hypothesis that curcumin may promote thermogenesis and/or the browning process. For instance, Wang et al. [94] reported that mice treated with curcumin (50 or 100 mg/kg/day) for 50 days displayed a lower body weight gain and lower fat mass without any effect of food intake, and also showed better tolerance to cold exposure. Particularly, in these animals, curcumin induced browning of the WAT but in a depot-dependent manner, since increased mitochondrial biogenesis and increased expression of Ucp-1 and other brown-fat specific genes were found in inguinal but no in epididymal WAT (eWAT). In addition, these animals presented higher circulating levels of norepinephrine and increased expression of the β3-AR in the inguinal WAT, suggesting that the browning of the inguinal WAT (iWAT) is mediated by the norepinephrine-β3-AR pathway. Moreover, Nishikawa et al. [95] also reported that the oral administration of curcumin formulations with higher bioavailability than native curcumin increased browning in iWAT tissue of mice. Song et al. [96] reported that male C57BL/6J mice fed with a high-fat diet plus 1% of curcumin presented higher thermogenic capacity in response to a cold challenge, already evident after two weeks of treatment. In addition, a long-term dietary intervention (17 weeks) did not affect iWAT browning but increased Ucp-1, Ppara, and Pmrd16 expression in the BAT. About miRNAs, there are no reports concerning the browning process; however, it has been seen that curcumin markedly increased the content of miRNA-34a in SGC-7901 cells, inhibited proliferation, migration, and invasion. As described above, miRNA-34a has been studied in human WAT and expressed negatively with waist circumference [49,97].
In vitro studies have shown that curcumin also induces browning and mitochondrial biogenesis in 3T3-L1 cell line and primary inguinal white adipocytes [98,99]. Curcumin significantly increased several brown fat markers in both adipocytes in a dose-dependent manner (doses ranged from 1 to 20 µM). In fact, this effect seems to be mediated via the AMP-activated protein kinase (AMPK) pathway [99]. In addition, a proteome analysis of primary inguinal white adipocytes treated with 20 µM curcumin for six to eight days revealed that curcumin increased protein levels related to fatty acid oxidation, lipolysis, and browning-specific markers [98].
4.1.3. Thyme
Thymol (2-Isopropyl-5-methylphenol) is monoterpene phenol, and the major constituent of essential oils isolated from plants belonging to the Lamiaceae family such as Thymus (Thymus vulgaris) [100,101]. Thymus vulgaris is a native plant of Mediterranean regions traditionally used as a culinary herb and also in traditional medicine [101]. Not to mention, it is also used in the food industry for its flavoring and preservative properties [100]. Therefore, it has not been deeply studied regarding its effect on body weight control, thermogenesis, or browning effect, and, in addition, there is no evidence related to any miRNA. However, Choi et al. [102] described that thymol might promote fat browning and lipid metabolism in 3T3-L1 adipocytes. Meanwhile, adipocytes treated with 20 µM of thymol increased mRNA and protein levels of PGC-1α, PRMD16, and UCP-1. In addition, there is a synergic increase of Fgf21, Pgc-1α, Prdm16, Tmem26, and Ucp-1 (brow fat-specific genes) in the presence of 20 µM of thymol together with 50 nM triiodothyronine and 1 µM rosiglitazone (browning cocktail). Overall, the authors suggest that thymol might promote the browning of white adipocytes via activation of the β3-AR pathway.
4.1.4. Cinnamon
Cinnamon is produced from the bark of trees from the genus Cinnamomum and belongs to the family Lauraceae [103]. The major components are cinnamaldehyde and cinnamic acid [104]. Regarding the bioactive compounds of cinnamon, recent studies showed biological effects of cinnamaldehyde, such as anti-inflammatory, antioxidant, and anti-obesity properties [105]. Also, several hydroxycinnamic acid derivatives, such as cinnamic acid, ameliorated the obesity induced by an HFD in rats [106]. Furthermore, trans-cinnamic acid (tCA), as an analog of cinnamon, demonstrated beneficial properties on body weight and blood lipids in obese rats [104]. In this context, regarding the molecular mechanisms of cinnamon and its bioactive compounds, several in vitro studies have been developed on murine adipocytes and found that cinnamaldehyde (40 µM) prevents adipocyte differentiation through the downregulation of Ppar-γ and Ccat-enhancer-binding protein alpha (C/EBPα) [107]. Regarding the browning process, Prdm16 interacts directly with Ppar-γ and plays an important role in the thermogenesis process [108]. Thus, in an in vitro study, tCA induced browning in 3T3-L1 cells in a concentration of 200 µM upregulated protein expression of PGC-1α, PRDM16, and UCP-1 and upregulated genes involved in the browning process and beige-fat-specific like Pgc1-α, Prdm16, and Ucp-1 [104]. Similarly, in an in vivo study, cinnamaldehyde supplementation (10 mg/kg BW) downregulated adipogenic genes and promoted lipolysis and brown adipose tissue activity. These results led to decreased body weight gain and fat accumulation after 14 weeks of treatment [107]. Likewise, another study showed that cinnamaldehyde supplementation (40 mg/kg/day) decreased body weight by inducing the browning of WAT in HFD-fed mice [108]. However, although the effects of cinnamon and its bioactive compounds on the browning process have been identified, to date, the relationship with miRNAs has not been described. Not only was it not directly in an obesity model, but a recently published article also showed that cinnamaldehyde regulates inflammation in macrophages through the suppression of miR-21 and miR-155 [109]. Not to mention, the study focused on inflammatory bowel disease and ulcerative colitis. As a result, a relationship has been found with the suppression of miR-155 in the process of browning [110].
4.1.5. Garlic
Bioactive compounds from garlic (Allium sativum L.) have been studied for their possible anti-obesity effect in in vitro models, animal models, and clinical trials [107]. The most abundant biocompounds present in garlic are allicin, alliin, diallyl sulphide, diallyl disulphide, diallyl trisulfide, ajoene, and S-allyl-cysteine [111]. In this context, some of these compounds have been shown to exert effects on lipid accumulation, such as ajoene, in concentrations from 25 µM to 200 µM in 3T3-L1 cells [112]. Furthermore, other in vitro studies have been developed to investigate the effects of garlic-derived organo-sulfur compounds. Thus, the results report a decrease in intracellular triglycerides after diallyl trisulphide in adipocytes [107]. Additionally, the authors highlighted the possible molecular mechanisms to decrease gene expression related to adipogenesis, as well as the increase in genes related to fatty acid oxidation, such as Ucp-1 [107]. Also, in relation to garlic biocompounds and its anti-obesity properties, it has been identified that thiacremonone enhanced the mRNA level of uncoupling protein-2 (Ucp-2) in 3T·-L1 cells [113]. Similar results have been found in in vivo studies, suggesting an anti-obesity effect of garlic supplementation. In this regard, M. Kim and Kim demonstrated a potential anti-obesity effect of garlic (2% or 4%) in obese mice, downregulating adipogenic genes. Likewise, in another study with obese mice treated with garlic powder (2% or 5%) for seven weeks, lower body weight, WAT, and adipogenic gene expression was found in WAT and increased Ucps mRNA levels and AMPK activity in BAT [114]. All these studies have demonstrated the effect of garlic and its biocompounds on the browning process in different in vitro and in vivo models. However, although the modulation of miRNAs by garlic has been identified, its effects have not been related, so far, with the browning process. More studies are needed to highlight the effect of garlic and its biocompounds on miRNAs and BAT.
4.1.6. Onion
Quercetin is one of the most abundant flavonoids present in food (onions, apples, tea, and red wine) [115] and is the aglycone form of other glycosidic flavonoids. In this context, as an example, onion (Allium cepa L.) is a natural source rich in phenolic compounds, fructans, and organosulfur compounds. Phenolic compounds from onion, especially flavonols such as quercetin, are secondary metabolites that have been widely studied for the anti-obesity effects [116]. Possible anti-obesity mechanisms of quercetin could involve AMPK and mitogen-activated protein kinase (MAPK) signaling pathways. AMPK is a key regulator of energy balance inducing mitochondrial biogenesis and, therefore, promoting BAT. In this context, Lee et al. [117] showed increased expression of genes related with brown adipocyte development, such as Prmd16, Ucp-1, and Pgc1-α in retroperitoneal white adipose tissue (rWAT) of mice fed with HFD supplemented with 0.5% onion peel extract (OPE) for eight weeks. In addition, the same authors demonstrated the conversion of white to brown adipocytes in 3T3-L1 cells cultivated with 50 µM of quercetin during the differentiation process (6 days) [117]. Also, another in vivo study found lower triglycerides levels in mice fed HFD supplemented with quercetin (0.1% w/w) for 12 weeks. This result may be mediated by the increased expression of Ucp-1 in sWAT [118]. Although the role of miRNAs as a potential mechanism involved in the regulation of the browning process has not been specially described, some miRNAs could be implicated in the inflammatory response [119]. In a recent study, the effect of quercetin on miR-155 expression in RAW264.7 macrophages stimulated with lipopolysaccharide (LPS) was evaluated. Thus, they demonstrated that treatment with quercetin (10 µM) down-regulated the expression of miR-155 in LPS-stimulated macrophages [73]. Another study showed that quercetin and isorhamnetin (a quercetin metabolite) improved the inflammatory status induced by LPS in murine macrophages, and suggested miR-155 as a regulatory inflammatory mediator [120]. Although, in these studies, miR-155 was related to the macrophage response to various types of inflammatory markers. Likewise, other studies described that the inhibition of miR-155 could enhance brown adipocyte differentiation through the browning process [110,121]. On the other hand, a recent study identified an upregulated miR-369-3p expression level in dendritic cells treated with quercetin. The foregoing led to the down-regulation of C/ebp-β, which resulted in a lower production of inflammatory cytokines [122].
4.2. Other Herbal and Food Compounds
4.2.1. Magnolia Officinalis
Magnolol (5,5′-diallyl-2,2′-dihydroxybiphenyl) is a hydroxylated biphenyl active compound isolated from Magnolia officinalis [123,124]. In fact, a range of biological activities has been attributed to magnolol, such as antiinflammation, antioxidation, antiangiogenesis, and anticancer activities [123,124]. In addition, it has been described that long-term supplementation of magnolol (17 mg/kg BW per day for 16 weeks) ameliorates body fat accumulation, insulin resistance, and adipose inflammation in HFD fed male C57BL/6J mice [125]. Moreover, regarding the thermogenic or browning effect in the adipocytes, Parray et al. [126] described that 3T3-L1 adipocytes treated with 5–20 µM of magnolol during differentiation displayed a dose-dependent increase in the protein level UCP-1, PGC-1α, PRMD16, and PPARγ. The addition of 20 µM of magnolol in the presence of a 50 nM triiodothyronine with 1 µM rosiglitazone from day six to eight of differentiation in 3T3-L1 cells increased the expression of specific browning markers such as Ucp-1, Pgc-1α, Prmd16, Cd137, Tbx1, and Cidea. In sum, these results suggest that magnolol might promote the browning of 3T3-L1 adipocytes. Also, magnolol increases UCP-1, PGC-1α, and PRDM16 in HIB1B brown adipocytes.
Honokiol ((3′,5-di-(2-propenyl)-1,1′-biphenyl-2,2′-diol) is a phenylpropanoid molecule found in several species belonging to the genus Magnolia [127,128]. Firstly, it presents a structural homology with magnolol [129], and magnolol is a structural isomer of honokiol [124]. Secondly, among the different effects attributed to honokiol, it has been suggested that it may promote neuroprotection [127,129] and may exert an anticarcinogenic effect [130]. Furthermore, there is scarce literature on the effect of honokiol on body weight control or its effect on thermogenesis, at least in vivo. Also, in vitro studies on 3T3-L1 adipocytes pointed out an induction of brown adipocyte-like phenotype in white adipocytes by honokiol. In addition, these cells presented a dose-dependent (1–20 µM) increase in the protein levels of PGC-1α, PRDM16, and UCP-1. Moreover, 3T3-L1 adipocytes grown on a media containing 20 µM of honokiol from day six to eight of differentiation presented increased mRNA levels of Cidea, Cox8, Fgf21, Pgc-1α, and Ucp1 (genes characteristics of brown adipocytes) and increased protein levels of C/EBPβ, PPARγ, and peroxisome proliferator-activated receptor delta (PPARδ) (key regulatory proteins for browning). In fact, the authors suggest that the induction browning in these cells could be mediated through the activation of extracellular signal-regulated kinase (ERK).
Likewise, honokiol also increased the levels of PGC-1α, PPARγ, PRDM16, and UCP-1 in HIB1B cells (at 20 µM) (when these cells are fully differentiated, they express Ucp RNA like BAT in vivo; thus, these are good cell models for studying the regulation of Ucp gene expression in BAT and metabolism [131,132]. Nowadays, it is known that the magnolol induces miR-200c expression in breast cancer cells [133], with regard to this, miR-200c is also related to the browning process in humans [121].
4.2.2. Berberine
Berberine is an isoquinoline alkaloid derived from the Chinese medicinal plant Coptis chinensis (Chinese goldthread) [134]. It has been found that berberine inhibits fat accumulation adipocytes in vitro and in diet-induced obese mice and also can induce weight loss in rodents and human subjects [135,136,137,138,139]. Henceforth, recent emerging evidence suggests that berberine increases energy expenditure, thermogenesis, and browning.
Zhang et al. [140] reported that obese db/db mice treated for four weeks with berberine (i.p, administration of 5 mg/kg/day) had higher rectal temperature and presented improved cold tolerance than control animals. In fact, berberine administration also induced the expression of Pgc-1α, Ucp-1, and Cidea, among others, in BAT of obese db/db mice. Also, berberine administration induces browning of iWAT but not in eWAT. In iWAT, obese db/db mice treated with berberine presented increased expression of Pgc-1α, Ucp-1, and Cidea. These animals also had increased mitochondrial biogenesis and a BAT-like phenotype of inguinal adipocytes.
Lin et al. [141] showed that HFD-fed C57BL/6J mice treated with berberine at 100 mg/kg/day in 0.9% saline by oral gavage had reduced obesity and were protected against the development of hyperglycemia, hyperlipidemia, and insulin resistance. In addition, berberine treatment increased oxygen consumption and the expression of Ucp-1 and tyrosine hydroxylase (rate-limiting enzyme in the heat production process) [142]. The 3T3-L1 cells treated with 5 µM berberine for 48 h had increased expression of CITED1, BMP7, PRDM16, and UCP-1. This effect may be mediated through transcription-coupled post-transcriptional regulation. In another study, a treatment with berberine revealed a decrease in miRNA-92a, which led to an increase in RNA-binding motif protein 4a (RBM4a) expression, promoting the beige adipogenesis in 3T3-L1 [141].
Wu et al. [143] reported that in 10 overweight individuals with NAFLD that received berberine for one month (0.5 g, 30 min before eating, three times a day), there was an increase in the mass and activity of BAT. In addition, HFD-induced obese mice that received berberine for six weeks (i.p, administration of 1.5 mg/kg/day) displayed enhanced BAT thermogenesis and reduced body weight gain. Therefore, these animals presented higher rectal temperature and increased expression of Ucp-1, Prdm16, Pgc-1α, Ppargc1b, and Elovl3, and higher protein levels of UCP-1 and PRDM16 in BAT compared to their controls. However, berberine administration did not induce the typical browning phenotype in iWAT or eWAT.
4.2.3. Panax ginseng
Panax ginseng is one of the most used traditional Chinese herbs and has an approximately 2500-year medicinal history in Eastern Asia, and is a slow-growing perennial plant that belongs to the genus Panax in the Araliaceae family [144]. The majority of P. ginseng contains protopanaxadiols and protopanaxatriols as dammarane type triterpene saponins [145]. Among them, ginsenoside Rb1 is the main protopanaxadiol saponin, and ginsenoside Re, Rg1, and notoginsenoside R1 are the main representative protopanaxatriol components [146]. The importance of ginseng lies in its multiple pharmacological functions, such as anticancer activity, as well as antioxidant and aging inhibitory effects [77]. Additionally, fat accumulation in obesity involves two cellular mechanisms: WAT hypertrophy and hyperplasia [147]; likewise, there are several reports showing that ginseng can reduce adipocyte size and fat storage in mice and rats fed with HFD [148]. Therefore, an effect of Rg1 has been demonstrated to suppress the accumulation of triglycerides (TG) in 3T3-L1 cells and the obesity model induced by the HFD of zebrafish [149].
AMPK, a critical regulator of energy metabolism, has been shown to play a key role in adipose tissue metabolism [150]. In fact, AMPKα1 activation has been found to be involved in the regulation of browning in iWAT of mice [151]. As a result, it has been shown that Rg1 induces BAT-like differentiation of adipocytes and thermogenic activation, which is a process that also involves the upregulation of fatty acid oxidation through the activation of AMPK. Consequently, lipid droplets take a form typical of brown adipocytes and Ucp-1 expression is induced, and mitochondrial activity increases [152]. In this sense, a study revealed that Rb2 activates BAT and induces browning of WAT, which increases energy expenditure and thermogenesis and consequently ameliorates obesity and metabolic disorders, suggesting Rb2 to be a promising beneficial compound treating obesity [153]. In diet-induced obese mice supplemented with Rb2 BAT activation and WAT browning, as shown by reducing lipid droplets, increasing Ucp-1 staining, and activating brown gene programs [154]. Thereupon, miR-27b is identified to regulate adipogenesis by targeting Ppar-γ2, and in this sense, has shown that expression levels for both of miR-27b and its primary transcript, pri-mir-27b, were found to decrease upon ginsenoside Rb1 treatment in 3T3-L1, which in turn promotes Ppar-γ expression and adipogenesis [155].
4.2.4. Mentha
The commercially important species Mentha piperita and M. arvensis are cultivated for the essential oil used in food, confection, cosmetics, alcoholic beverage, tobacco, and pharmaceutical industries [156]. The essential oil of members of the mint (Lamiaceae) family is dominated by monoterpenes. In fact, menthol is one of the major constituents of essential oil of both species. Despite the similarity in the menthol biosynthetic pathway of these two species, the compositional variations in the essential oil cannot be ignored, as M. arvensis essential oil constitutes the major trading essential oil for menthol in the world. Likewise, menthol is a chemical cooling agent naturally produced from mint oils or prepared synthetically [157]. Consequently, a cold sensation in mammals is detected by several cold-sensors; among them, the most preeminent one is the cold and menthol receptor, canonical transient receptor potential cation channel subfamily M member 8 (TRPM8) [158]. Some findings highlight the role of menthol-induced TRPM8 activation in Ucp-1 dependent thermogenesis and energy expenditure [159]. Activation of TRPM8 receptors in the gut and skin by oral and topical administration of menthol leads to an increase in serum glucagon levels, thus activating several downstream catabolic processes like the browning of WAT and activation of energy expenditure markers in WAT and BAT [160].
Some studies also demonstrated the induction of the browning process through TRPM8 activation on human WAT, highlighting the importance of the presence of TRPM8 in adipose tissue [161,162]. However, to date, no studies have been found that directly relate this species to miRNA and the browning process. Nevertheless, an in vitro study showed that L-menthol administration at bioavailable doses significantly increased browning/brite and the energy expenditure phenotype and enhanced mitochondrial activity-related gene expression [163]. In addition, an in vivo experiment has found that dietary menthol enhanced WAT browning and improved glucose metabolism in HFD-induced obesity mice, which suggests that TRPM8 might be involved in WAT browning by increasing the expression levels of genes related to thermogenesis and energy metabolism [164].
4.2.5. Chrysin
Chrysin (5,7-dihydroxyflavone) is a natural flavonoid found in honey, propolis, mushrooms, and other plant species [165,166]. Also, it has been reported that chrysin exhibits an antioxidant and anti-inflammatory effect, a protective effect against diabetes, and also possesses neuroprotective activity [165,166,167]. In fact, its role in the activation of thermogenesis or browning effect is less studied. Choi et al. [168] reported that 3T3-L1 adipocytes treated with 50 µM of chrysin in the presence of a 50 nM triiodothyronine and 1 µM rosiglitazone (a “browning cocktail”) from day six to eight of differentiation presented increased expression of proteins/genes related to lipolysis and fatty acid oxidation, and decreased the expression of proteins related to lipogenesis. Moreover, chrysin increased the expression of brown fat markers in these cells via a mechanism involving AMPK and PGC-1α. It is important to note that, like the curcumin, chrysin too has been related to the miRNA-34a.
4.2.6. Soy
Isoflavones are a subgroup of flavonoids present in soybeans and other legumes [169]. Genistein is an isoflavone widely studied in different cells and animal models. Some of the biological properties of genistein highlight its anti-obesity effect [170]. In this context, Lephart et al. [171] demonstrated significantly upregulated Ucp-1 mRNA expression levels in BAT of Long-Evans rat supplemented with soy isoflavone mixture. In a recent in vitro study, genistein programmed adipocytes to be converted into beige adipocytes. In the first place, the treatment consisted of adding genistein at concentrations of 10, 50, or 100 µM during the differentiation period. Furthermore, the molecular mechanisms involved could be a reduction in mRNA levels of genes related to lipogenesis and increased expression of genes that regulate the development of brown adipocytes such as Cebpβ and Pgc-1α [172]. On the other hand, a recent study evaluated the effect of genistein in an in vivo model in which mice were fed an HFD supplemented with genistein (0.25 g/kg diet) for eight weeks. To point out, the results showed less weight gain, sWAT weight, and free fatty acid levels in mice supplemented with genistein compared to the HFD group. Regarding the mechanisms, the authors emphasize the correlation between the differentially expressed genes in the hypothalamus and browning markers induced by genistein supplementation [173].
Daidzein is another isoflavone whose effect on body weight and lipid metabolism has been studied in WAT and BAT. In this context, rats were supplemented with daidzein (5 mg/kg and 50 mg/kg) for 10 weeks. The results showed expression changes in genes involved in adipogenesis and fatty acid oxidation. Furthermore, daidzein treatment increased UCP-1 protein expression in BAT, activating the thermogenesis [174]. Regarding miRNAs modulated by genistein, to date, there is no specific evidence on miRNAs that regulate the browning process and BAT. Nevertheless, genistein was associated with decreasing miR-155 and consequently improved inflammation in an in vitro model with human umbilical vein endothelial cells (HUVECs) [175]. In addition, another study reported the anticancer effects of genistein by modulating miR-155 in breast cancer cells [176]. However, additional studies are needed to analyze the effect of genistein on miR-155 in relation to BAT.
4.2.7. Green Tea Polyphenols
Tea polyphenols have been reported to have many health benefits, such as antioxidant and anti-inflammatory activities [177]. The predominant constituents of green tea, accounting for up to 35% of the dry weight, are the polyphenols, which include flavonols, flavones, and flavan-3-ols commonly known as catechins [178]; these are present also in fruits, such as apple, grapes and berries, beans, cocoa and red wine [179]. In fact, catechins have received much attention due to their beneficial effects on health [180]. The most abundant green tea catechin is epigallocatechin gallate (EGCG), which accounts for about 50% to 70% of green tea catechins [82]. Mice fed 0.5% polyphenolic green tea extracts rich in catechins and EGCG for eight weeks showed whitening of the BAT and induced the browning process in the WAT [181]. Meanwhile, rats supplemented with green tea extract (155 mg/kg/day for eight weeks) showed higher expression of both Ucp-1 and Ppar-γ [182]. In essence, the intake of oolong, red, and black tea has been found to reduce adiposity and foster browning of mWAT in mice, and these effects were accompanied by increased AMPK phosphorylation [183]. In fact, most studies have found greater activation of regulatory genes in the browning effect. A study on mice evaluated the influence of a single oral administration of theaflavins on energy metabolism and found an increase in Ucp-1 and Pgc-1α mRNA levels in BAT. These results indicate that theaflavin rich fraction significantly enhances systemic energy expenditure, as evidenced by an increase in the expression of metabolic genes [184]. On the other hand, 3T3-L1 preadipocyte cell showed significantly reduced intracellular lipid accumulation by targeting miR-27a and miR-27b, as well as Ppar-γ [185]. In recent years, an increasing number of clinical trials have confirmed the beneficial effects of green tea on obesity; however, the optimal dose has not yet been established. However, a clinical trial has shown that the intake of catechin (615 mg) and caffeine (77 mg) 2 times/day for five weeks increases the cold-induced thermogenesis effect [186]. Overall, most of the studies aimed to assess the impact of green tea catechins on fat oxidation rather than thermogenesis; therefore, more studies are necessary to evaluate their involvement in the browning process in humans.
4.3. PUFA’s
4.3.1. Conjugated Linoleic Acid
Conjugated linoleic acids (CLAs) are molecules mostly found in dairy products and ruminant meats [187]. CLA is a group of PUFA derived from linoleic acid (LA, C18:2 n-6), with a conjugated double bond in different cis- and trans-arrangements [188]. Additionally, twenty-eight isomers of CLA have been identified, with the predominant isomers being cis-9, trans-11-CLA (c9, t11-CLA), which represents up to 90% of total CLA in food, and trans-10, cis-12-CLA (t10,c12-CLA), present in a smaller quantity [189]. Some studies have suggested that CLA leads to weight loss by reducing the size and altering the evolution of adipocytes [190]. In fact, proposed anti-obesity mechanisms of 10, 12 CLA isomer include decreased lipogenesis and increased lipolysis [191]. Moreover, Cidea has been associated with thermoregulation [192], lipid droplet dynamics, and lipid metabolism [193]. A study in human adipocytes treated with CLA found an upregulation of Cidea and Ucp-1 genes, setting the role of Cidea in the transcriptional regulation of thermogenesis [194]. Also, it has been described that CLA induces the browning of WAT, increasing Ucp-1 and Cidea gene expression in both and iWAT, with higher Ucp-1 mRNA and protein detected in iWAT from 10,12 CLA-supplemented mice [195]. Male mice fed an HFD diet for five weeks and then switched to an LFD with or without 0.1% 10,12 CLA decreased WAT weight and increased mRNA levels of genes related to thermogenesis and fatty acid oxidation in eWAT and iWAT, including Ucp-1 and Ppar-α [196]. Nevertheless, in vitro studies indicate that direct treatment of pre-adipocytes with trans-10, cis-12 CLA increased markers of inflammation and suppressed markers of beiging or browning. A study in human adipocytes showed that 30–50 µM trans-10, cis-12 CLA consistently decreased the mRNA, protein, and activity levels of PPARγ, an adipogenic transcription factor that induces Ucp-1 expression [197]. Furthermore, in brown adipocytes isolated from hamsters, mRNA levels of Ucp-1 were increased 260% by 71.4 µM cis-9, trans-11 CLA, but were suppressed 80% by 71.4 µM trans-10, cis-12 CLA compared with the controls [198]. Most studies have been developed in in vivo models indicating positive regulation of browning markers; however, in vitro experiments indicate that the effect of 10,12 CLA is still unclear. Regarding miRNA, CLA mediates its pro-resolving effects in part via regulation of the proinflammatory miR-155, which has been associated with the WAT browning effect [199].
4.3.2. Eicosapentaenoic Acid
Fish oil, rich in omega-3 (n-3) PUFAs such as eicosapentaenoic acid (C20:5n-3, EPA), is anti-inflammatory primarily by reducing the production of proinflammatory cytokines [200]. Furthermore, it has been suggested that EPA is able to enhance energy dissipation in subcutaneous adipose tissue to stimulate oxidative metabolism and reduces fatty acid release by facilitating fatty acid storage in mice [201]. In addition, it has been shown that EPA promoting mitochondrial biogenesis and beige-like markers in human subcutaneous adipocytes from overweight subjects [202]. For this reason, there is evidence that EPA may induce adipocytes to acquire a beige phenotype and may activate brown thermogenesis. In addition, fish oil increased thermogenic markers in the BAT, such as β3-AR and Ucp-1 [203,204]. C57BL/6 male mice fed with EPA for five weeks improved the expression of genes related to the browning of WAT, and BAT thermogenic markers such as Ppar-α, Ppar-γ, and fibronectin and fibronectin type III domain-containing 5 (FNDC5) [203]. Zhao et al. [201] reported that EPA significantly increased the expression of thermogenic genes like Ucp1-3, Cidea, and Vegfα. In addition, carnitine palmitoyltransferase 1B (Cpt1b) mediates the transport of fatty acids into the mitochondrial matrix for β-oxidation. It has been reported that EPA promotes brite adipogenesis and improves the parameters of mitochondrial function, such as increased expression of Cpt1b [205]. On the other hand, miRNAs play critical functions in BAT differentiation and maintenance. The deletion of adipose-specific dicer promotes white-like phenotypes of brown precursor cells [206]. In this context, Kim et al. [76] confirmed the association between miR-30b/378 and brown thermogenesis in C57BL/6 mice fed with fish oil.
4.3.3. Docosahexaenoic Acid
Docosahexaenoic acid (DHA) is a long-chain, highly unsaturated omega-3 (n-3) fatty acid. It has a structure that gives it unique physical and functional properties, as well as 22 carbons in its acyl chain, which includes six double bonds. DHA is found in fairly high amounts in seafood and products derived from seafood. Examples of fatty fish are mackerel, salmon, trout, herring, tuna, and sardines [207]. In fact, DHA is of particular interest, given their potential effects on adipose tissues and metabolism [208]. Also, it has shown a better anti-inflammatory effect than EPA in adipose tissue, which may be related to a more significant role of DHA in promoting Ucp-1 expression [209]. Additionally, recent studies showed that BAT activation or WAT browning of WAT by n-3 PUFAs were independent of Ucp-1 [210]. It was shown that refeeding rats a diet enriched in PUFAs, but not in saturated fatty acids, following two weeks of food restriction increased BAT mass and expression of Ucp-1 [211]. Nonetheless, the thermogenic stimuli via the intervention with DHA and their ability to induce Ucp-1 in WAT are still controversial [212].
4.4. Carotenoids
4.4.1. β-Carotene
Carotenoids are a diverse group of compounds responsible for most of the yellow, orange, and red colors in fruits and vegetables [213]. Among the six most abundant carotenoids in plasma, α-carotene, β-cryptoxanthin, lutein, zeaxanthin, lycopene, and β-carotene [214]. Carotenoids are notably stored in adipose tissue [215]. What is more, carotenoids and carotenoid conversion products impact gene expression and cell function through multiple mechanisms. The most important carotenoid is pro-vitamin A β-carotene, which is metabolized by various enzymes to generate several cleavage products, including retinoic acid (RA) [216]. The effects of carotenoids and retinoids on adipose tissue mostly rely on their ability to bind to specific nuclear receptors, namely RA receptors (RARs) and retinoid X receptors (RXRs), in order to modulate gene expression in the adipocyte [217]. However, it has been suggested that carotene within the BAT could be metabolized to a significant degree to retinoic acid and, thus, become a Ucp-1 activator [218]. Studies have also reported the effect of carotenoid-related compounds in increasing energy expenditure and thermogenesis in both WAT and BAT; nonetheless, the interaction with miRNA has not been analyzed. The participation of β-carotene in the modulation of Ucp-1 expression was established by in vitro studies [219]. Furthermore, the treatment with RA in murine BAT cells induces an overexpression of thermogenic and catabolic proteins [220].
4.4.2. Fucoxanthin
Fucoxanthin is a natural pigment that can be extracted from brown seaweeds and is rich in xanthophylls (a subset of carotenoids) [221]. Dietary fucoxanthin is mostly absorbed as fucoxanthinol, a hydrolyzed metabolite in the small intestine, and enters systemic circulation through lymph [222]. Although, it is demonstrated that fucoxanthin is involved in a variety of physiological processes in the body and have many beneficial properties, including the antioxidant and anti-inflammatory and neuroprotective effect [223]. Indeed, fucoxanthin an anti-obesity effect in both in vitro and in vivo in mice and human models [224]. In 3T3-L1 adipocytes, fucoxanthin reduced lipid accumulation accompanied by a decrease in Ppar-γ expression [225]. However, the intake of an HFD supplemented with 0.2% fucoxanthin in C57BL/6 mice increased Ucp-1 expression in both WAT and BAT [221,226]. Maeda et al. [227] indicated that fucoxanthin upregulates the expression of Ucp-1 in WAT, which may contribute to reducing WAT weight. Overall, obese mice fed with fucoxanthin showed a decrease in WAT weight as well as a significant upregulation in the expression of UCP-1 mRNA and protein in WAT, resulting in an increase in energy expenditure in the form of heat and fatty acid oxidation in WAT [227]. These studies suggest that fucoxanthin may have promising anti-obesity effects and deserve more research focus especially related to miRNAs and primarily in human subjects, as the results are still confusing. For example, Rebello et al. [228] did not find changes in the expression of genes related to WAT browning, fat oxidation, and glucose transport in vitro in primary human adipocytes treated with fucoxanthin.
4.5. Citrus Fruits
Citrus fruits are a source of numerous phenolic compounds, pectins, and vitamins such as A, C, and E [229,230]. In recent years it has been shown that a diet rich in phenolic compounds can improve health and reduce the incidence of different diseases [231]. Some of the flavonoids found in citrus sources, such as orange, grapefruit, and lemon, are naringenin and hesperetin from the flavanones group, as well as other subtypes of flavonols, such as kaempferol, and also certain hydroxycinnamic acids [232]. Regarding obesity, one study in mice (1%) for 21 days found an increase in fatty acid oxidation in hepatocytes [233]. On the other hand, another study showed anti-inflammatory activity of naringenin in in vitro macrophages [234]. In addition, a study conducted on a murine cell line treated with Citrus aurantium extract (10–50 µg/mL) found inhibition of adipocyte differentiation, preventing lipid accumulation [235]. Although there are many studies that have focused on the anti-obesity effect of the phenolic compounds from citrus fruits, the effect on BAT activation and the WAT browning process has not been fully elucidated. Furthermore, a recent study demonstrated a thermogenic effect in brown adipocytes after treatment with bitter orange possible due to AMPK activation [236]. In addition, an in vivo study evaluated the effect of immature citrus fruits (1%) in HFD fed mice for 11 weeks and found an increased expression of Ucp-1 in iWAT, thus suggesting that weight loss might be attributed to the browning process in WAT [237]. In this context, Nishikawa et al. [238] analyzed the effect of α-monoglucosyl hesperidin in mice, as a simple glycosidic flavanone, and found a significant decrease in body fat, which may be due to the activation of the browning process in iWAT. Also, another recent study evaluated the effects of naringenin on energy expenditure in human WAT (hWAT). In this context, when adipocytes were treated with naringenin for seven days, the browning process was activated through the induction of Ucp-1 as a key marker in the thermogenesis pathway [228]. Overall, some effects of citrus flavonoids on thermogenesis have been identified, but naringenin-mediated modulation of miRNAs has not been reported to date. Figure 3 displays some of the most studied food compounds, and the main candidates target genes that promote WAT browning.
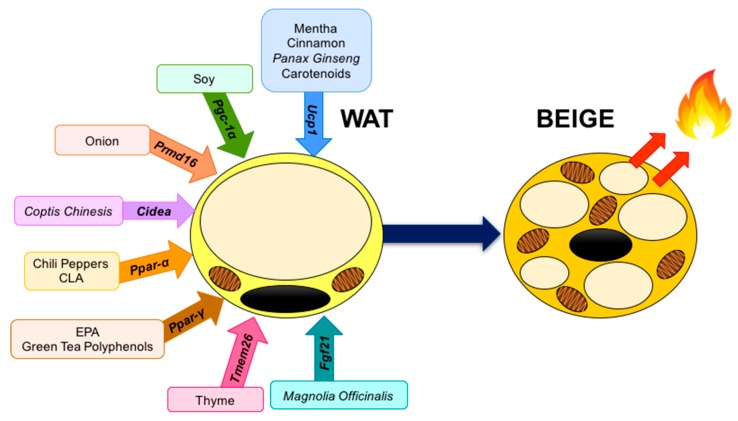
Figure 3.
Food compounds and activated genes involved in WAT browning. Fgf21, Fibroblast growth factor 21; Tmem26, Transmembrane protein 26; Pparγ, Peroxisome proliferator-activated receptor gamma; Pparα, Peroxisome proliferator-activated receptor α; Cidea, Cell death inducing DFFA like effector A; Prmd16, PR-domain containing 16; Pgc-1α, Peroxisome proliferator-activated γ receptor co-activator 1 alpha; Ucp-1, Uncoupling protein-1.
5. Conclusions
In summary, the detection of BAT in adult humans has raised the expectations for the development of novel anti-obesity treatments that can regulate brown or beige fat development. Recently, inducible brown adipocytes in WAT depots, called beige or brite cells, have gained more interest due to their increased capability of energy expenditure and their positive effect on diet-induced obesity. For instance, we focused on miRNAs and food compounds like key regulators of brown adipogenesis and the commitment of beige adipocytes to a brown phenotype during the “browning” process. Current knowledge deriving from clinical trials, cell culture, and animal models suggests that miRNAs can be implicated in the regulation of the critical genes involved in the differentiation and function of WAT and BAT, highlighting miRNAs as therapeutic targets for obesity. However, the dietary components discussed above have been shown to share common molecular targets involved in the induction of browning. In the long run, these findings need to be validated in more clinical trials by further large studies with a relatively long-term period of follow-up and taking into consideration factors such as ethnicity, genetics, and lifestyles.
Acknowledgments
We thank M.T.R and A.C.G to support involved in the grammar and syntax corrections of the manuscript
Abbreviations
| AMPK | AMP-activated protein kinase |
| AMPKα1 | 5-AMP-activated protein kinase catalytic subunit alpha-1 |
| BAT | Brown adipose tissue |
| BMP7 | Bone morphogenetic protein 7 |
| BW | Body weight |
| C/EBPα | CCAAT/enhancer binding protein alpha |
| Cd137 | 4-1BB |
| Cd40 | CD40 molecule |
| CIDEA | Cell death inducing DFFA like effector A |
| CITED1 | Cpb/P300 interacting transactivator with Glu/Asp rich carboxy-terminal |
| CLA | Conjugated linoleic acid |
| Cox8 | Cytochrome c oxidase subunit 8 |
| CPTB1β | Carnitine palmitoyltransferase I |
| DHA | Docosahexanoic acid |
| Dio2 | Iodothyronine deiodinase 2 |
| EGCG | Epigallocatechin gallate |
| Elovl3 | Elongation of very long-chain fatty acid 3 |
| EPA | Eicosapentanoic acid |
| ERK | Extracellular signal-regulated kinases |
| eWAT | Epididymal WAT |
| Fgf32 | Fibroblast growth factor 23 |
| FNDC5 | Fibronectin type III domain-containing protein 5 |
| Foxc2 | Forkhead box C2 |
| HFD | High-fat diet |
| HUVECs | Human umbilical vein endothelial cells |
| hWAT | Human white adipose tissue |
| iWAT | Inguinal WAT |
| LA | Linoleic acid |
| LFD | Low-fat diet |
| LPS | Lipopolysaccharides |
| MAPK | Mitogen-activated protein kinase |
| miRNAs | MicroRNAs |
| mWAT | Mesenteric WAT |
| Myf5 | Myogenic factor 5 |
| NAFLD | Nonalcoholic fatty liver disease |
| OPE | Onion peel extracti |
| Pgc-1α | Peroxisome proliferator-activated γ receptor co-activator 1 alpha |
| Ppargc1b | PPARG coactivator 1 beta |
| Pparα | Peroxisome proliferator-activated receptor α |
| Pparγ | Peroxisome proliferator-activated receptor gamma |
| Pparδ | Peroxisome proliferator-activated receptor delta |
| Prmd16 | PR-domain containing 16 |
| PUFA | Polyunsaturated fatty acids |
| RA | Retinoic acid |
| RAR | Retinoic acid receptor |
| RNA | Ribonucleic acid |
| rWAT | Retroperitoneal WAT |
| RXR | Retinoid X receptor |
| Sirt-1 | Sirtuin 1 |
| sWAT | Subcutaneous WAT |
| Tbx1 | T-box 1 |
| tCA | Trans-cinnamic acid |
| TG | Triglycerides |
| Tmem26 | Transmembrane protein 26 |
| TRPM8 | Transient receptor potential cation channel subfamily M (melastatin) member 8 |
| TRPV1 | Transient receptor potential vanilloid subfamily 1 |
| UCP-1 | Uncoupling protein-1 |
| UCP-2 | Uncoupling protein-2 |
| VEGFα | Vascular endothelial growth factor alpha |
| WAT | White adipose tissue |
| β3-AR | Beta3 adrenergic receptor |
Author Contributions
All authors contributed to writing and reviewing the manuscript. H.C. and K.H. edited and finalized the manuscript. All authors read and approved the final manuscript.
Funding
This research was funded by the Programa de apoyo a la publicación científica en revistas indexadas en el Journal Citation Report de la Universidad Autónoma de Nuevo León and was granted to A.L.G. and H.C.
Conflicts of Interest
The authors declare no conflict of interest. The funder had no role in the writing of the manuscript.
References
- 1.Villarroya F., Gavaldà-Navarro A., Peyrou M., Villarroya J., Giralt M. Handbook of Experimental Pharmacology. Volume 251. Springer; Basel, Switzerland: 2019. Brown Adipokines; pp. 239–256. [DOI] [PubMed] [Google Scholar]
- 2.Wu J., Boström P., Sparks L.M., Ye L., Choi J.H., Giang A.H., Khandekar M., Virtanen K.A., Nuutila P., Schaart G., et al. Beige adipocytes are a distinct type of thermogenic fat cell in mouse and human. Cell. 2012;150:366–376. doi: 10.1016/j.cell.2012.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shabalina I., Petrovic N., de Jong J.M.A., Kalinovich A., Cannon B., Nedergaard J. UCP1 in Brite/Beige Adipose Tissue Mitochondria Is Functionally Thermogenic. Cell Rep. 2013;5:1196–1203. doi: 10.1016/j.celrep.2013.10.044. [DOI] [PubMed] [Google Scholar]
- 4.Stojanović O., Kieser S., Trajkovski M. Common traits between the beige fat-inducing stimuli. Curr. Opin. Cell Biol. 2018;55:67–73. doi: 10.1016/j.ceb.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 5.Peirce V., Carobbio S., Vidal-Puig A. The different shades of fat. Nature. 2014;510:76–83. doi: 10.1038/nature13477. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez-Gurmaches J., Hung C.M., Sparks C.A., Tang Y., Li H., Guertin D.A. PTEN loss in the Myf5 lineage redistributes body fat and reveals subsets of white adipocytes that arise from Myf5 precursors. Cell Metab. 2012;16:348–362. doi: 10.1016/j.cmet.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kajimura S., Spiegelman B.M., Seale P. Brown and Beige Fat: Physiological Roles beyond Heat Generation. Cell Metab. 2015;22:546–559. doi: 10.1016/j.cmet.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silvester A.J., Aseer K.R., Jang H.J., Ryu E.Y., Kwon E.Y., Park J.G., Cho K.H., Chaudhari H.N., Choi M.S., Suh P.G., et al. Loss of DJ-1 promotes browning of white adipose tissue in diet-induced obese mice. J. Nutr. Biochem. 2018;61:56–67. doi: 10.1016/j.jnutbio.2018.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Tamucci K.A., Namwanje M., Fan L., Qiang L. The dark side of browning. Protein Cell. 2018;9:152–163. doi: 10.1007/s13238-017-0434-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartel D.P. MicroRNAs: Genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297. doi: 10.1016/S0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 11.Bartel D.P. Metazoan MicroRNAs. Cell. 2018;173:20–51. doi: 10.1016/j.cell.2018.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arner E., Mejhert N., Kulyté A., Balwierz P.J., Pachkov M., Cormont M., Lorente-Cebrián S., Ehrlund A., Laurencikiene J., Hedén P., et al. Adipose tissue microRNAs as regulators of CCL2 production in human obesity. Diabetes. 2012;61:1986–1993. doi: 10.2337/db11-1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trajkovski M., Ahmed K., Esau C.C., Stoffel M. MyomiR-133 regulates brown fat differentiation through Prdm16. Nat. Cell Biol. 2012;14:1330–1335. doi: 10.1038/ncb2612. [DOI] [PubMed] [Google Scholar]
- 14.Oskowitz A.Z., Lu J., Penfornis P., Ylostalo J., McBride J., Flemington E.K., Prockop D.J., Pochampally R. Human multipotent stromal cells from bone marrow and microRNA: Regulation of differentiation and leukemia inhibitory factor expression. Proc. Natl. Acad. Sci. USA. 2008;105:18372–18377. doi: 10.1073/pnas.0809807105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tay Y., Zhang J., Thomson A.M., Lim B., Rigoutsos I. MicroRNAs to Nanog, Oct4 and Sox2 coding regions modulate embryonic stem cell differentiation. Nature. 2008;455:1124–1128. doi: 10.1038/nature07299. [DOI] [PubMed] [Google Scholar]
- 16.Broughton J.P., Lovci M.T., Huang J.L., Yeo G.W., Pasquinelli A.E. Pairing beyond the Seed Supports MicroRNA Targeting Specificity. Mol. Cell. 2016;64:320–333. doi: 10.1016/j.molcel.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vasudevan S. Posttranscriptional upregulation by microRNAs. Wiley Interdiscip. Rev. RNA. 2012;3:311–330. doi: 10.1002/wrna.121. [DOI] [PubMed] [Google Scholar]
- 18.Treiber T., Treiber N., Meister G. Regulation of microRNA biogenesis and its crosstalk with other cellular pathways. Nat. Rev. Mol. Cell Biol. 2019;20:5–20. doi: 10.1038/s41580-018-0059-1. [DOI] [PubMed] [Google Scholar]
- 19.Arner P., Kulyté A. MicroRNA regulatory networks in human adipose tissue and obesity. Nat. Rev. Endocrinol. 2015;11:276–288. doi: 10.1038/nrendo.2015.25. [DOI] [PubMed] [Google Scholar]
- 20.Shamsi F., Zhang H., Tseng Y.H. MicroRNA Regulation of Brown Adipogenesis and Thermogenic Energy Expenditure. Front. Endocrinol. 2017;8:205. doi: 10.3389/fendo.2017.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trajkovski M., Lodish H. MicroRNA networks regulate development of brown adipocytes. Trends Endocrinol. Metab. TEM. 2013;24:442–450. doi: 10.1016/j.tem.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goody D., Pfeifer A. MicroRNAs in brown and beige fat. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2019;1864:29–36. doi: 10.1016/j.bbalip.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Lorente-Cebrián S., González-Muniesa P., Milagro F.I., Martínez J.A. MicroRNAs and other non-coding RNAs in adipose tissue and obesity: Emerging roles as biomarkers and therapeutic targets. Clin. Sci. 2019;133:23–40. doi: 10.1042/CS20180890. [DOI] [PubMed] [Google Scholar]
- 24.Maciel-Dominguez A., Swan D., Ford D., Hesketh J. Selenium alters miRNA profile in an intestinal cell line: Evidence that miR-185 regulates expression of GPX2 and SEP SH2. Mol. Nutr. Food Res. 2013;57:2195–2205. doi: 10.1002/mnfr.201300168. [DOI] [PubMed] [Google Scholar]
- 25.Garcia-Lacarte M., Martinez J.A., Zulet M.A., Milagro F.I. Implication of miR-612 and miR-1976 in the regulation of TP53 and CD40 and their relationship in the response to specific weight-loss diets. PLoS ONE. 2017;13:e0201217. doi: 10.1371/journal.pone.0201217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Belarbi Y., Mejhert N., Gao H., Arner P., Rydén M., Kulyté A. MicroRNAs-361-5p and miR-574-5p associate with human adipose morphology and regulate EBF1 expression in white adipose tissue. Mol. Cell. Endocrinol. 2018;472:50–56. doi: 10.1016/j.mce.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 27.Xue B., Liu Q.Y., Massie L., Qualls C., Mao J.T. Grape seed procyanidin extract against lung cancer: The role of microrna-106b, bioavailability, and bioactivity. Oncotarget. 2018;9:15579–15590. doi: 10.18632/oncotarget.24528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlörmann W., Naumann S., Renner C., Glei M. Influence of miRNA-106b and miRNA-135a on butyrate-regulated expression of p21 and Cyclin D2 in human colon adenoma cells. Genes Nutr. 2015;10:50. doi: 10.1007/s12263-015-0500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu W., Cao H., Ye C., Chang C., Lu M., Jing Y., Zhang D., Yao X., Duan Z., Xia H., et al. Hepatic miR-378 targets p110α and controls glucose and lipid homeostasis by modulating hepatic insulin signalling. Nat. Commun. 2014;5:5684. doi: 10.1038/ncomms6684. [DOI] [PubMed] [Google Scholar]
- 30.Hu S., Dong T.S., Dalal S.R., Wu F., Bissonnette M., Kwon J.H., Chang E.B. The Microbe-Derived Short Chain Fatty Acid Butyrate Targets miRNA-Dependent p21 Gene Expression in Human Colon Cancer. PLoS ONE. 2011;6:e16221. doi: 10.1371/journal.pone.0016221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dhar S., Hicks C., Levenson A. Resveratrol and prostate cancer: Promising role for microRNAs. Mol. Nutr. Food Res. 2011;55:1219–1229. doi: 10.1002/mnfr.201100141. [DOI] [PubMed] [Google Scholar]
- 32.De Conti A., Ortega J.F., Tryndyak V., Dreval K., Moreno F.S., Rusyn I., Beland F.A., Pogribny I.P. MicroRNA deregulation in nonalcoholic steatohepatitis-associated liver carcinogenesis. Oncotarget. 2017;8:88517–88528. doi: 10.18632/oncotarget.19774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCann M.J., Rotjanapun K., Hesketh J.E., Roy N.C. Expression profiling indicating low selenium-sensitive microRNA levels linked to cell cycle and cell stress response pathways in the Caco-2 cell line. Br. J. Nutr. 2017;117:1212–1221. doi: 10.1017/S0007114517001143. [DOI] [PubMed] [Google Scholar]
- 34.Okamatsu-Ogura Y., Matsushita M., Bariuan J.V., Nagaya K., Tsubota A., Saito M. Association of circulating exosomal miR-122 levels with BAT activity in healthy humans. Sci. Rep. 2019;9:13243. doi: 10.1038/s41598-019-49754-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ye D., Zhang T., Lou G., Xu W., Dong F., Chen G., Liu Y. Plasma miR-17, miR-20a, miR-20b and miR-122 as potential biomarkers for diagnosis of NAFLD in type 2 diabetes mellitus patients. Life Sci. 2018;208:201–207. doi: 10.1016/j.lfs.2018.07.029. [DOI] [PubMed] [Google Scholar]
- 36.Adams B.D., Arem H., Hubal M.J., Cartmel B., Li F., Harrigan M., Sanft T., Cheng C.J., Pusztai L., Irwin M.L. Excersice and weight loss interventions and miRNA expression in women with breast cancer. Breast Cancer Res. Treat. 2018;170:55–67. doi: 10.1007/s10549-018-4738-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Satishchadran A., Ambade A., Rao S., Hsueh Y.C., Iracheta-Vellve A., Tornai D., Lowe P., Gyongyosi B., Li J., Catalano D., et al. MicroRNA 122, regulated by GRLH2, protects livers of mice and patients from ethanol-induced liver disease. Gastroenterology. 2018;154:238–252. doi: 10.1053/j.gastro.2017.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Latorre J., Moreno-Navarrete J.M., Mercader J.M., Sabater M., Rovira Ò., Gironès J., Ricart W., Fernández-Real M., Ortega F.J. Decreased lipid metabolism but increased FA biosynthesis are coupled with changes in liver microRNAs in obese subjects with NAFLD. Int. J. Obes. Lond. 2017;41:620–630. doi: 10.1038/ijo.2017.21. [DOI] [PubMed] [Google Scholar]
- 39.Carreras-Badosa G., Bonmatí A., Ortega F.J., Mercader J.M., Guindo-Martínez M., Torrents D., Prats-Puig A., Martinez-Calcerrada J.M., Platero-Gutierrez E., De Zegher F., et al. Altered circulating miRNA expression profile in pregestational and gestational obesity. J. Clin. Endocrinol. Metab. 2015;100:E1446–E1456. doi: 10.1210/jc.2015-2872. [DOI] [PubMed] [Google Scholar]
- 40.Su D., Liu H., Qi X., Dong L., Zhang R., Zhang J. Citrus peel flavonoids improve lipid metabolism by inhibiting miR-33 and miR-122 expression in HepG2 cells. Biosci. Biotechnol. Biochem. 2019;83:1747–1755. doi: 10.1080/09168451.2019.1608807. [DOI] [PubMed] [Google Scholar]
- 41.Willeit P., Skroblin P., Moschen A.R., Yin X., Kaudewitz D., Zampetaki A., Barwari T., Whitehead M., Ramírez C.M., Goedeke L., et al. Circulating microRNA-122 is associated with the risk of new-onset metabolic syndrome and type 2 diabetes. Diabetes. 2017;66:347–357. doi: 10.2337/db16-0731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parasramka M.A., Ali S., Banerjee S., Deryavoush T., Sarkar F.H., Gupta S. Garcinol sensitizes human pancreatic adenocarcinoma cells to gemcitabine in association with microRNA signatures. Mol. Nutr. Food Res. 2013;57:235–248. doi: 10.1002/mnfr.201200297. [DOI] [PubMed] [Google Scholar]
- 43.Lam T.K., Shao S., Zhao Y., Marincola F., Pesatori A., Bertazzi P.A., Caporaso N.E., Wang E., Landi M.T. Influence of quercetin-rich food intake on microRNA expression in lung cancer tissues. Cancer Epidemiol. Biomark. Biomark. 2012;21:2176–2184. doi: 10.1158/1055-9965.EPI-12-0745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fu X., Dong B., Tian Y., Lefebvre P., Meng Z., Wang X., Pattou F., Han W., Wang X., Lou F., et al. MicroRNA-26a regulates insulin sensitivity and metabolism of glucose and lipids. J. Clin. Investig. 2015;125:2497–2509. doi: 10.1172/JCI75438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Malcomson F.C., Willis N.D., McCallum I., Xie L., Lagerwaard B., Kelly S., Bradburn D.M., Belshaw N.J., Johnson I.T., Mathers J. Non-digestible carbohydrates supplementation increases miR-32 expression in the healthy human colorectal epithelium: A randomized controlled trial. Mol. Carcinog. 2017;56:2104–2111. doi: 10.1002/mc.22666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gottmann P., Ouni M., Saussenthaler S., Roos J., Stirm L., Jähnert M., Kamitz A., Hallahan N., Jonas W., Fritsche A., et al. A computational biology approach of a genome-wide screen connected miRNAs to obesity and type 2 diabetes. Mol. Metab. 2018;11:145–159. doi: 10.1016/j.molmet.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang T., Cooper S., Brockdorff N. The interplay of histone modifications—Writers that read. EMBO Rep. 2015;16:1467–1481. doi: 10.15252/embr.201540945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Villard A., Marchand L., Thivolet C., Rome S. Diagnostic Value of Cell-free Circulating MicroRNAs for Obesity and Type 2 Diabetes: A Meta-analysis. J. Mol. Biomark. Diagn. 2015;6:251. doi: 10.4172/2155-9929.1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Giardina S., Hernández-Alonso P., Salas-Salvadó J., Rabassa-Soler A., Bulló M. Modulation of Human Subcutaneous Adipose Tissue MicroRNA Profile Associated with Changes in Adiposity-Related Parameters. Mol. Nutr. Food Res. 2018;62:1700594. doi: 10.1002/mnfr.201700594. [DOI] [PubMed] [Google Scholar]
- 50.Wang H., Shao Y., Yuan F., Feng H., Li N., Zhang H., Wu C., Liu Z. Fish Oil Feeding Modulates the Expression of Hepatic MicroRNAs in a Western-Style Diet-Induced Nonalcoholic Fatty Liver Disease Rat Model. BioMed Res. Int. 2017;2017:2503847. doi: 10.1155/2017/2503847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Min H.K., Kapoor A., Fuchs M., Mirshahi F., Zhou H., Maher J., Kellum J., Warnick R., Contos M.J., Sanyal A.J. Increased hepatic synthesis and dysregulation of cholesterol metabolism is associated with the severity of nonalcoholic fatty liver disease. Cell Metab. 2012;15:665–674. doi: 10.1016/j.cmet.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marques-Rocha J.L., Garcia-Lacarte M., Samblas M., Bressan J., Martínez J.A., Milagro F.I. Regulatory roles of miR-155 and let-7b on the expression of inflammation-related genes in THP-1 cells: Effects of fatty acids. J. Physiol. Biochem. 2018;74:579–589. doi: 10.1007/s13105-018-0629-x. [DOI] [PubMed] [Google Scholar]
- 53.Zhang T., Hu J., Wang X., Zhao X., Li Z., Niu J., Steer C.J., Zheng G., Song G. MicroRNA-378 promotes hepatic inflammation and fibrosis via modulation of the NF-kB-TNF-α pathway. J. Hepatol. 2019;70:87–96. doi: 10.1016/j.jhep.2018.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang T., Zhao X., Steer C.J., Yan G., Song G. A negative feedback loop between microRNA-378 and Nrf1 promotes the development of hepatosteatosis in mice treated with a high fat diet. Metabolism. 2018;85:183–191. doi: 10.1016/j.metabol.2018.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Camera D.M., Ong J.N., Coffey V.G., Hawley J.A. Selective Modulation of MicroRNA Expression with Protein Ingestion Following Concurrent Resistance and Endurance Exercise in Human Skeletal Muscle. Front. Physiol. 2016;7:87. doi: 10.3389/fphys.2016.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meale S.J., Beauchemin K.A., Hristov A.N., Chaves A.V., McAllister T.A. Board-invited review: Opportunities and challenges in using exogenous enzymes to improve ruminant production. J. Anim. Sci. 2014;92:427–442. doi: 10.2527/jas.2013-6869. [DOI] [PubMed] [Google Scholar]
- 57.Romao J.M., Jin W., He M., McAllister T., Guan L.L. Altered MicroRNA Expression in Bovine Subcutaneous and Visceral Adipose Tissues from Cattle under Different Diet. PLoS ONE. 2012;7:e40605. doi: 10.1371/journal.pone.0040605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang H., Zhong J., Chai Z., Zhu J., Xin J. Comparative expression profile of microRNAs and piRNAs in three ruminant species testes using next-generation sequencing. Reprod. Domest. Anim. 2018;53:963–970. doi: 10.1111/rda.13195. [DOI] [PubMed] [Google Scholar]
- 59.Casas-Agustench P., Fernandes F.S., Tavares do Carmo M.G., Visioli F., Herrera E., Dávalos A. Consumption of Distinct Dietary Lipids during Early Pregnancy Differentially Modulates the Expression of microRNAs in Mothers and Offspring. PLoS ONE. 2015;10:e0117858. doi: 10.1371/journal.pone.0117858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Luceri C., Bigagli E., Pitozzi V., Giovannelli L. A nutrigenomics approach for the study of anti-aging interventions: Olive oil phenols and the modulation of gene and microRNA expression profiles in mouse brain. Eur. J. Nutr. 2017;56:865–877. doi: 10.1007/s00394-015-1134-4. [DOI] [PubMed] [Google Scholar]
- 61.Ma H., Hostuttler M., Wei H., Rexroad C.E., III, Yao J. Characterization of the Rainbow Trout Egg MicroRNA Transcriptome. PLoS ONE. 2012;7:e39649. doi: 10.1371/journal.pone.0039649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Miranda K., Mehrpouya-Bahrami P., Nagarkatti P.S., Nagarkatti M. Cannabinoid Receptor 1 Blockade Attenuates Obesity and Adipose Tissue Type 1 Inflammation Through miR-30e-5p Regulation of Delta-Like-4 in Macrophages and Consequently Downregulation of Th1 Cells. Front. Immunol. 2019;10:1049. doi: 10.3389/fimmu.2019.01049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miranda K., Yang X., Bam M., Murphy E.A., Nagarkatti P.S., Nagarkatti M. MicroRNA-30 modulates metabolic inflammation by regulating Notch signaling in adipose tissue macrophages. Int. J. Obes. 2018;42:1140–1150. doi: 10.1038/s41366-018-0114-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pahlavani M., Wijayatunga N.N., Kalupahana N.S., Ramalingam L., Gunaratne P.H., Coarfa C., Rajapakshe K., Kottapalli P., Moustaid-Moussa N. Transcriptomic and microRNA analyses of gene networks regulated by eicosapentaenoic acid in brown adipose tissue of diet-induced obese mice. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2018;1863:1523–1531. doi: 10.1016/j.bbalip.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pomar C.A., Castro H., Picó C., Palou A., Sánchez J. Maternal Overfeeding during Lactation Impairs the Metabolic Response to Fed/Fasting Changing Conditions in the Postweaning Offspring. Mol. Nutr. Food Res. 2019 doi: 10.1002/mnfr.201900504. [DOI] [PubMed] [Google Scholar]
- 66.Peng X., Chang H., Chen J., Zhang Q., Xiaoping Y., Mantian M. 3,6-Dihydroxyflavone regulates microRNA-34a through DNA methylation. BMC Cancer. 2017;17:619. doi: 10.1186/s12885-017-3638-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Green C.D., Huang Y., Dou X., Yang L., Liu Y., Han J.D.J. Impact of Dietary Interventions on Noncoding RNA Networks and mRNAs Encoding Chromatin-Related Factors. Cell Rep. 2017;18:2957–2968. doi: 10.1016/j.celrep.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 68.Lovis P., Roggli E., Laybutt D.R., Gattesco S., Yang J.Y., Widmann C., Abderrahmani A., Regazzi R. Alterations in microRNA expression contribute to fatty acid-induced pancreatic beta-cell dysfunction. Diabetes. 2008;57:2728–2736. doi: 10.2337/db07-1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Roggli E., Britan A., Gattesco S., Lin-Marg N., Abderrahmani A., Meda P., Regazzi R. Involvement of microRNAs in the cytotoxic effects exerted by proinflammatory cytokines on pancreatic beta-cells. Diabetes. 2010;59:978–986. doi: 10.2337/db09-0881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yin H., Pasut A., Soleimani V.D., Bentzinger C.F., Antoun G., Thorn S., Seale P., Fernando P., van Ijcken W., Grosveld F., et al. MicroRNA-133 controls brown adipose determination in skeletal muscle satellite cells by targeting Prdm16. Cell Metab. 2013;17:210–224. doi: 10.1016/j.cmet.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eseberri I., Lasa A., Miranda J., Garcia A., Portillo M.P. Potential miRNA involvement in the anti-adipogenic effect of resveratrol and its metabolites. PLoS ONE. 2017;12:e0184875. doi: 10.1371/journal.pone.0184875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Olivo-Marston S.E., Hursting S.D., Perkins S.N., Schetter A., Khan M., Croce C., Haris C.C., Lavigne J. Effects of calorie restriction and diet-induced obesity on murine colon carcinogenesis, growth and inflammatory factors, and microRNA expression. PLoS ONE. 2014;9:e94765. doi: 10.1371/journal.pone.0094765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Boesch-Saadatmandi C., Loboda A., Wagner A.E., Stachurska A., Jozkowicz A., Dulak J., Döring F., Wolffram S., Rimbach G. Effect of quercetin and its metabolites isorhamnetin and quercetin-3-glucuronide on inflammatory gene expression: Role of miR-155. J. Nutr. Biochem. 2011;22:293–299. doi: 10.1016/j.jnutbio.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 74.Li Y., Croucher N.J., Thompson C.M., Trzciński K., Hanage W.P., Lipsitch M. Identification of pneumococcal colonization determinants in the stringent response pathway facilitated by genomic diversity. BMC Genom. 2015;16:369. doi: 10.1186/s12864-015-1573-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jeon T.I., Park J.W., Ahn J., Jung C.H., Ha T.Y. Fisetin protects against hepatosteatosis in mice by inhibiting miR-378. Mol. Nutr. Food Res. 2013;57:1931–1937. doi: 10.1002/mnfr.201300071. [DOI] [PubMed] [Google Scholar]
- 76.Kim J., Okla M., Erickson A., Carr T., Natarajan S.K., Chung S. Eicosapentaenoic Acid Potentiates Brown Thermogenesis through FFAR4-dependent Up-regulation of miR-30b and miR-378. J. Biol. Chem. 2016;291:20551–20562. doi: 10.1074/jbc.M116.721480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thiele R., Mueller-Seitz E., Petz M. Chili pepper fruits: Presumed precursors of fatty acids characteristic for capsaicinoids. J. Agric. Food Chem. 2008;56:4219–4224. doi: 10.1021/jf073420h. [DOI] [PubMed] [Google Scholar]
- 78.Luo X.J., Peng J., Li Y.J. Recent advances in the study on capsaicinoids and capsinoids. Eur. J. Pharmacol. 2011;650:1–7. doi: 10.1016/j.ejphar.2010.09.074. [DOI] [PubMed] [Google Scholar]
- 79.El Hadi H., Di Vicenzo A., Vettor R., Rossato M. Food Ingredients Involved in White-to-Brown Adipose Tissue Conversion and in Calorie Burning. Front. Physiol. 2018;9:1954. doi: 10.3389/fphys.2018.01954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yoneshiro T., Aita S., Kawai Y., Iwanaga T., Saito M. Nonpungent capsaicin analogs (capsinoids) increase energy expenditure through the activation of brown adipose tissue in humans. Am. J. Clin. Nutr. 2012;95:845–850. doi: 10.3945/ajcn.111.018606. [DOI] [PubMed] [Google Scholar]
- 81.Bonet M.L., Oliver P., Palou A. Pharmacological and nutritional agents promoting browning of white adipose tissue. Biochim. Biophys. Acta. 2013;1831:969–985. doi: 10.1016/j.bbalip.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 82.Okla M., Kim J., Koehler K., Chung S. Dietary Factors Promoting Brown and Beige Fat Development and Thermogenesis. Adv. Nutr. 2017;8:473–483. doi: 10.3945/an.116.014332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Baboota R.K., Murtaza N., Jagtap S., Singh D.P., Karmase A., Kaur J., Bhutani K.K., Bishnoi M. Capsaicin-induced transcriptional changes in hypothalamus and alterations in gut microbial count in high fat diet fed mice. J. Nutr. Biochem. 2014;5:893–902. doi: 10.1016/j.jnutbio.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 84.Baboota R.K., Singh D.P., Sarma S.M., Kaur J., Sandhir R., Boparai R.K., Kondepudi K.K., Bishnoi M. Capsaicin induces “brite” phenotype in differentiating 3T3-L1 preadipocytes. PLoS ONE. 2014;9:e103093. doi: 10.1371/journal.pone.0103093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baskaran P., Krishnan V., Ren J., Thyagarajan B. Capsaicin induces browning of white adipose tissue and counters obesity by activating TRPV1 channel-dependent mechanisms. Br. J. Pharmacol. 2016;173:2369–2389. doi: 10.1111/bph.13514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mosqueda-Solís A., Sánchez J., Portillo M.P., Palou A., Picó C. Combination of Capsaicin and Hesperidin Reduces the Effectiveness of Each Compound to Decrease the Adipocyte Size and To Induce Browning Features in Adipose Tissue of Western Diet Fed Rats. J. Agric. Food Chem. 2018;66:9679–9689. doi: 10.1021/acs.jafc.8b02611. [DOI] [PubMed] [Google Scholar]
- 87.Fan L., Xu H., Yang R., Zang Y., Chen J., Qin H. Combination of Capsaicin and Capsiate Induces Browning in 3T3-L1 White Adipocytes via Activation of the Peroxisome Proliferator-Activated Receptor gamma/beta3-Adrenergic Receptor Signaling Pathways. J. Agric. Food Chem. 2019;67:6232–6240. doi: 10.1021/acs.jafc.9b02191. [DOI] [PubMed] [Google Scholar]
- 88.Ohyama K., Nogusa Y., Shinoda K., Suzuki K., Bannai M., Kajimura S. A Synergistic Antiobesity Effect by a Combination of Capsinoids and Cold Temperature Through Promoting Beige Adipocyte Biogenesis. Diabetes. 2016;65:1410–1423. doi: 10.2337/db15-0662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rohm B., Holik A.K., Kretschy N., Somoza M.M., Ley J.P., Widder S., Krammer G.E., Marko D., Somoza V. Nonivamide enhances miRNA let-7d expression and decreases adipogenesis PPARγ expression in 3T3-L1 cells. J. Cell. Biochem. 2015;116:1153–1163. doi: 10.1002/jcb.25052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shishodia S., Sethi G., Aggarwal B.B. Curcumin: Getting back to the roots. Ann. N. Y. Acad. Sci. 2005;1056:206–217. doi: 10.1196/annals.1352.010. [DOI] [PubMed] [Google Scholar]
- 91.Aggarwal B.B., Sundaram C., Malani N., Ichikawa H. CURCUMIN: THE INDIAN SOLID GOLD. In: Aggarwal B.B., Surh Y.J., Shishodia S., editors. Advances in Experimental Medicine and Biology. Volume 595. Springer; Boston, MA, USA: 2007. [DOI] [PubMed] [Google Scholar]
- 92.Tønnesen H.H., Másson M., Loftsson T. Studies of curcumin and curcuminoids. XXVII. Cyclodextrin complexation: Solubility, chemical and photochemical stability. Int. J. Pharm. 2002;244:127–135. doi: 10.1016/S0378-5173(02)00323-X. [DOI] [PubMed] [Google Scholar]
- 93.Yang K.Y., Lin L.C., Tseng T.Y., Wang S.C., Tsai T.H. Oral bioavailability of curcumin in rat and the herbal analysis from Curcuma longa by LC-MS/MS. J. Chromatogr. B Analyt. Technol. Biomed. Life. Sci. 2007;853:183–189. doi: 10.1016/j.jchromb.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 94.Wang S., Wang X., Ye Z., Xu C., Zhang M., Ruan B., Wei M., Jiang Y., Zhang Y., Wang L., et al. Curcumin promotes browning of white adipose tissue in a norepinephrine-dependent way. Biochem. Biophys. Res. Commun. 2015;466:247–253. doi: 10.1016/j.bbrc.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 95.Nishikawa S., Kamiya M., Aoyama H., Nomura M., Hyodo T., Ozeki A., Lee H., Takahashi T., Imaizumi A., Tsuda T. Highly Dispersible and Bioavailable Curcumin but not Native Curcumin Induces Brown-Like Adipocyte Formation in Mice. Mol. Nutr. Food Res. 2018;62:1700731. doi: 10.1002/mnfr.201700731. [DOI] [PubMed] [Google Scholar]
- 96.Song Z., Revelo X., Shao W., Tian L., Zeng K., Lei H., Sun H.S., Woo M., Winer D., Jin T. Dietary Curcumin Intervention Targets Mouse White Adipose Tissue Inflammation and Brown Adipose Tissue UCP1 Expression. Obesity. 2018;26:547–558. doi: 10.1002/oby.22110. [DOI] [PubMed] [Google Scholar]
- 97.Sun C., Zhang S., Liu C., Liu X. Curcumin promoted miR-34a expression and suppressed proliferation of gastric cancer cells. Cancer Biother. Radiopharm. 2019 doi: 10.1089/cbr.2019.2874. [DOI] [PubMed] [Google Scholar]
- 98.Kim S.W., Choi J.H., Mukherjee R., Hwang K.C., Yun J.W. Proteomic identification of fat-browning markers in cultured white adipocytes treated with curcumin. Mol. Cell. Biochem. 2016;415:51–66. doi: 10.1007/s11010-016-2676-3. [DOI] [PubMed] [Google Scholar]
- 99.Lone J., Choi J.H., Kim S.W., Yun J.W. Curcumin induces brown fat-like phenotype in 3T3-L1 and primary white adipocytes. J. Nutr. Biochem. 2016;27:193–202. doi: 10.1016/j.jnutbio.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 100.Marchese A., Orhan I.E., Daglia M., Barbieri R., Di Lorenzo A., Nabavi S.F., Gortzi O., Izadi M., Nabavi S.M. Antibacterial and antifungal activities of thymol: A brief review of the literature. Food Chem. 2016;210:402–414. doi: 10.1016/j.foodchem.2016.04.111. [DOI] [PubMed] [Google Scholar]
- 101.Salehi B., Mishra A.P., Shukla I., Sharifi-Rad M., Contreras M.D.M., Segura-Carretero A., Fathi H., Nasrabadi N.N., Kobarfard F., Sharifi-Rad J. Thymol, thyme, and other plant sources: Health and potential uses. Phytother. Res. 2018;32:1688–1706. doi: 10.1002/ptr.6109. [DOI] [PubMed] [Google Scholar]
- 102.Choi J.H., Kim S.W., Yu R., Yun J.W. Monoterpene phenolic compound thymol promotes browning of 3T3-L1 adipocytes. Eur. J. Nutr. 2017;56:2329–2341. doi: 10.1007/s00394-016-1273-2. [DOI] [PubMed] [Google Scholar]
- 103.De la Garza A.L., Milagro F.I., Boque N., Campión J., Martínez J.A. Natural inhibitors of pancreatic lipase as new players in obesity treatment. Planta Med. 2011;77:773–785. doi: 10.1055/s-0030-1270924. [DOI] [PubMed] [Google Scholar]
- 104.Kang N.H., Mukherjee S., Yun J.W. Trans-Cinnamic Acid Stimulates White Fat Browning and Activates Brown Adipocytes. Nutrients. 2019;11:577. doi: 10.3390/nu11030577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Huang B., Yuan H.D., Kim D.Y., Quan H.Y., Chung S.H. Cinnamaldehyde Prevents Adipocyte Differentiation and Adipogenesis via Regulation of Peroxisome Proliferator-Activated Receptor-γ (PPARγ) and AMP-Activated Protein Kinase (AMPK) Pathways. J. Agric. Food Chem. 2011;59:3666–3673. doi: 10.1021/jf104814t. [DOI] [PubMed] [Google Scholar]
- 106.Mnafgui K., Derbali A., Sayadi S., Gharsallah N., Elfeki A., Allouche N. Anti-obesity and cardioprotective effects of cinnamic acid in high fat diet- induced obese rats. J. Food Sci. Technol. 2015;52:4369–4377. doi: 10.1007/s13197-014-1488-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lu M., Cao Y., Xiao J., Song M., Ho C.T. Molecular mechanisms of the anti-obesity effect of bioactive ingredients in common spices: A review. Food Funct. 2018;9:4569–4581. doi: 10.1039/C8FO01349G. [DOI] [PubMed] [Google Scholar]
- 108.Zuo J., Zhao D., Yu N., Fang X., Mu Q., Ma Y., Mo F., Wu R., Ma R., Wang L., et al. Cinnamaldehyde Ameliorates Diet-Induced Obesity in Mice by Inducing Browning of White Adipose Tissue. Cell. Physiol. Biochem. 2017;42:1514–1525. doi: 10.1159/000479268. [DOI] [PubMed] [Google Scholar]
- 109.Qu S., Shen Y., Wang M., Wang X., Yang Y. Suppression of miR-21 and miR-155 of macrophage by cinnamaldehyde ameliorates ulcerative colitis. Int. Immunopharmacol. 2019;67:22–34. doi: 10.1016/j.intimp.2018.11.045. [DOI] [PubMed] [Google Scholar]
- 110.Chen Y., Siegel F., Kipschull S., Haas B., Fröhlich H., Meister G., Pfeifer A. miR-155 regulates differentiation of brown and beige adipocytes via a bistable circuit. Nat. Commun. 2013;4:1769. doi: 10.1038/ncomms2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shang A., Cao S.Y., Xu X.Y., Gan R.Y., Tang G.Y., Corke H., Mavumengwana V., Li H.B. Bioactive Compounds and Biological Functions of Garlic (Allium sativum L.) Foods Basel Switz. 2019;8:246. doi: 10.3390/foods8070246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ambati S., Yang J.Y., Rayalam S., Park H.J., Della-Fera M.A., Baile C.A. Ajoene exerts potent effects in 3T3-L1 adipocytes by inhibiting adipogenesis and inducing apoptosis. Phytother. Res. 2009;23:513–518. doi: 10.1002/ptr.2663. [DOI] [PubMed] [Google Scholar]
- 113.Kim E.J., Lee D.H., Kim H.J., Lee S.J., Ban J.O., Cho M.C., Jeong H.S., Yang Y., Hong J.T., Yoon D.Y. Thiacremonone, a sulfur compound isolated from garlic, attenuates lipid accumulation partially mediated via AMPK activation in 3T3-L1 adipocytes. J. Nutr. Biochem. 2012;23:1552–1558. doi: 10.1016/j.jnutbio.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 114.Kim M., Kim H. Effect of garlic on high fat induced obesity. Acta Biol. Hung. 2011;62:244–254. doi: 10.1556/ABiol.62.2011.3.4. [DOI] [PubMed] [Google Scholar]
- 115.Torres-Villarreal D., Camacho A., Milagro F.I., Ortiz-Lopez R., de la Garza A.L. Quercetin-3-O-glucoside improves glucose tolerance in rats and decreases intestinal sugar uptake in caco-2 cells. Nat. Prod. Commun. 2017;12:1709–1712. doi: 10.1177/1934578X1701201112. [DOI] [Google Scholar]
- 116.Peñarrieta M., Tejeda L., Mollinedo P., Vila J., Bravo J. Phenolic Compounds in Food. Rev. Boliv. Quím. 2014;31:68–81. [Google Scholar]
- 117.Lee S.G., Parks J.S., Kang H.W. Quercetin, a functional compound of onion peel, remodels white adipocytes to brown-like adipocytes. J. Nutr. Biochem. 2017;42:62–71. doi: 10.1016/j.jnutbio.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 118.Kuipers E.N., Dam A.D.V., Held N.M., Mol I.M., Houtkooper R.H., Rensen P.C.N., Boom M.R. Quercetin Lowers Plasma Triglycerides Accompanied by White Adipose Tissue Browning in Diet-Induced Obese Mice. Int. J. Mol. Sci. 2018;19:1786. doi: 10.3390/ijms19061786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Akbari Kordkheyli V., Khonakdar Tarsi A., Mishan M.A., Tafazoli A., Bardania H., Zarpou S., Bagheri A. Effects of quercetin on microRNAs: A mechanistic review. J. Cell. Biochem. 2019;120:12141–12155. doi: 10.1002/jcb.28663. [DOI] [PubMed] [Google Scholar]
- 120.Boesch-Saadatmandi C., Wagner A.E., Wolffram S., Rimbach G. Effect of quercetin on inflammatory gene expression in mice liver in vivo—Role of redox factor 1, miRNA-122 and miRNA-125b. Pharmacol. Res. 2012;65:523–530. doi: 10.1016/j.phrs.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 121.Arias N., Aguirre L., Fernández-Quintela A., González M., Lasa A., Miranda J., Macarulla M.T., Portillo M.P. MicroRNAs involved in the browning process of adipocyte. J. Physiol. Biochem. 2016;72:509–521. doi: 10.1007/s13105-015-0459-z. [DOI] [PubMed] [Google Scholar]
- 122.Galleggiante V., De Santis S., Liso M., Verna G., Sommella E., Mastronardi M., Campiglia P., Chieppa M., Serrino G. Quercetin-Induced miR-369-3p Suppresses Chronic Inflammatory Response Targeting C/EBP-β. Mol. Nutr. Food Res. 2019;63:1801390. doi: 10.1002/mnfr.201801390. [DOI] [PubMed] [Google Scholar]
- 123.Ranaware A.M., Banik K., Deshpande V., Padmavathi G., Roy N.K., Sethi G., Fan L., Kumar A.P., Kunnumakkara A.B. Magnolol: A Neolignan from the Magnolia Family for the Prevention and Treatment of Cancer. Int. J. Mol. Sci. 2018;19:2362. doi: 10.3390/ijms19082362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang J., Chen Z., Huang X., Shi W., Zhang R., Chen M., Huang H., Wu L. Insights on the Multifunctional Activities of Magnolol. BioMed Res. Int. 2019;2019:1847130. doi: 10.1155/2019/1847130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kim Y.J., Choi M.S., Cha B.Y., Woo J.T., Park Y.B., Kim S.R., Jung U.J. Long-term supplementation of honokiol and magnolol ameliorates body fat accumulation, insulin resistance, and adipose inflammation in high-fat fed mice. Mol. Nutr. Food Res. 2013;57:1988–1998. doi: 10.1002/mnfr.201300113. [DOI] [PubMed] [Google Scholar]
- 126.Parray H.A., Lone J., Park J.P., Choi J.W., Yun J.W. Magnolol promotes thermogenesis and attenuates oxidative stress in 3T3-L1 adipocytes. Nutrition. 2018;50:82–90. doi: 10.1016/j.nut.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 127.Talarek S., Listos J., Barreca D., Tellone E., Sureda A., Nabavi S.F., Braidy N., Nabavi S.M. Neuroprotective effects of honokiol: From chemistry to medicine. Biofactors. 2017;43:760–769. doi: 10.1002/biof.1385. [DOI] [PubMed] [Google Scholar]
- 128.Rauf A., Patel S., Imran M., Maalik A., Arshad M.U., Saeed F., Mabkhot Y.N., Al-Showiman S.S., Ahmad N., Elsharkawy E. Honokiol: An anticancer lignan. Biomed. Pharmacother. 2018;107:555–562. doi: 10.1016/j.biopha.2018.08.054. [DOI] [PubMed] [Google Scholar]
- 129.Woodbury A., Yu S.P., Wei L., García P. Neuro-modulating effects of honokiol: A review. Front. Neurol. 2013;4:130. doi: 10.3389/fneur.2013.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Prasad R., Katiyar S.K. Honokiol, an Active Compound of Magnolia Plant, Inhibits Growth, and Progression of Cancers of Different Organs. Adv. Exp. Med. Biol. 2016;928:245–265. doi: 10.1007/978-3-319-41334-1_11. [DOI] [PubMed] [Google Scholar]
- 131.Lone J., Yun J.W. Honokiol exerts dual effects on browning and apoptosis of adipocytes. Pharmacol. Rep. 2017;69:1357–1365. doi: 10.1016/j.pharep.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 132.Ross S.R., Choy L., Graves R.A., Fox N., Solevjeva V., Klaus S., Ricquier D., Spiegelman B.M. Hibernoma formation in transgenic mice and isolation of a brown adipocyte cell line expressing the uncoupling protein gene. Proc. Natl. Acad. Sci. USA. 1992;89:7561–7565. doi: 10.1073/pnas.89.16.7561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hagiwara K., Gailhouste L., Yasukawa K., Kosaka N., Ochiya T. A robust screening method for dietary agents that activate tumour-suppressor microRNAs. Sci. Rep. 2015;5:14697. doi: 10.1038/srep14697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hu X., Zhang Y., Xue Y., Zhang Z., Wang J. Berberine is a potential therapeutic agent for metabolic syndrome via brown adipose tissue activation and metabolism regulation. Am. J. Transl. Res. 2018;10:3322–3329. [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang Y., Li X., Zou D., Liu W., Yang J., Zhu N., Huo L., Wang M., Hong J., Wu P., et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J. Clin. Endocrinol. Metab. 2008;93:2559–2565. doi: 10.1210/jc.2007-2404. [DOI] [PubMed] [Google Scholar]
- 136.Hu Y., Davies G.E. Berberine inhibits adipogenesis in high-fat diet-induced obesity mice. Fitoterapia. 2010;81:358–366. doi: 10.1016/j.fitote.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 137.Hu Y., Fahmy H., Zjawiony J.K., Davies G.E. Inhibitory effect and transcriptional impact of berberine and evodiamine on human white preadipocyte differentiation. Fitoterapia. 2010;81:259–268. doi: 10.1016/j.fitote.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 138.Hu Y., Ehli E.A., Kittelsrud J., Ronan J., Munger K., Downey T., Bohlen K., Callahan L., Munson V., Jahnke M., et al. Lipid-lowering effect of berberine in human subjects and rats. Phytomedicine. 2012;19:861–867. doi: 10.1016/j.phymed.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 139.Zhang X., Zhao Y., Zhang M., Pang X., Xu J., Kang C., Li M., Zhang C., Zhang Z., Li X., et al. Structural changes of gut microbiota during berberine-mediated prevention of obesity and insulin resistance in high-fat diet-fed rats. PLoS ONE. 2012;7:e42529. doi: 10.1371/journal.pone.0042529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Zhang Z., Zhang H., Li B., Meng X., Wang J., Zhang Y., Yao S., Ma Q., Jin L., Yang J., et al. Berberine activates thermogenesis in white and brown adipose tissue. Nat. Commun. 2014;5:5493. doi: 10.1038/ncomms6493. [DOI] [PubMed] [Google Scholar]
- 141.Lin Y.C., Lee Y.C., Lin Y.J., Lin J.C. Berberine Promotes Beige Adipogenic Signatures of 3T3-L1 Cells by Regulating Post-transcriptional Events. Cells. 2019;8:632. doi: 10.3390/cells8060632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lin J., Cai Q., Liang B., Wu L., Zhuang Y., He Y., Lin W. Berberine, a Traditional Chinese Medicine, Reduces Inflammation in Adipose Tissue, Polarizes M2 Macrophages, and Increases Energy Expenditure in Mice Fed a High-Fat Diet. Med. Sci. Monit. 2019;25:87–97. doi: 10.12659/MSM.911849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wu L., Xia M., Duan Y., Zhang L., Jiang H., Hu X., Yan H., Gu Y., Shi H., Li J., et al. Berberine promotes the recruitment and activation of brown adipose tissue in mice and humans. Cell Death Dis. 2019;10:468. doi: 10.1038/s41419-019-1706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sanada S., Kondo N., Shoji J., Tanaka O., Shibata S. Studies on the saponins of ginseng. II. Structures of ginsenoside-Re, -Rf and -Rg2. Chem. Pharm. Bull. (Tokyo) 2008;22:2407–2412. doi: 10.1248/cpb.22.2407. [DOI] [Google Scholar]
- 145.Hong H.D., Choi S.Y., Kim Y.C., Lee Y.C., Cho C.W. Rapid determination of ginsenosides Rb 1, Rf, and Rg 1 in Korean ginseng using HPLC. J. Ginseng Res. 2009;33:8–12. [Google Scholar]
- 146.Washida D., Kitanaka S. Determination of polyacetylenes and ginsenosides in Panax species using high performance liquid chromatography. Chem. Pharm. Bull. (Tokyo) 2003;51:1314–1317. doi: 10.1248/cpb.51.1314. [DOI] [PubMed] [Google Scholar]
- 147.Jo J., Gavrilova O., Pack S., Jou W., Mullen S., Summer A.E., Cushman S.W., Periwal V. Hypertrophy and/or hyperplasia: Dynamics of adipose tissue growth. PLoS Comput. Biol. 2009;5:e1000324. doi: 10.1371/journal.pcbi.1000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lee Y.S., Cha B.Y., Yamaguchi K., Choi T., Yonezawa T., Teruya T., Nagai K., Woo J.T. Effects of Korean white ginseng extracts on obesity in high-fat diet-induced obese mice. Cytotechnology. 2010;62:367–376. doi: 10.1007/s10616-010-9288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Koh E.J., Kim K.J., Choi J., Jeon H.J., Seo M.J., Lee B.Y. Ginsenoside Rg1 suppresses early stage of adipocyte development via activation of C/EBP homologous protein-10 in 3T3-L1 and attenuates fat accumulation in high fat diet-induced obese zebrafish. J. Ginseng Res. 2017;41:23–30. doi: 10.1016/j.jgr.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bijland S., Mancini S.J., Salt I.P. Role of AMP-activated protein kinase in adipose tissue metabolism and inflammation. Clin. Sci. 2013;124:491–507. doi: 10.1042/CS20120536. [DOI] [PubMed] [Google Scholar]
- 151.Wang S., Liang X., Yang Q., Fu X., Rogers C.J., Zhu M., Rodgers B.D., Jiang Q., Dodson M.V., Du M. Resveratrol induces brown-like adipocyte formation in white fat through activation of AMP-activated protein kinase (AMPK) alpha1. Int. J. Obes. 2015;39:967–976. doi: 10.1038/ijo.2015.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Lee K., Seo Y.J., Song J.H., Lee B.Y. Ginsenoside Rg1 promotes browning by inducing UCP1 expression and mitochondrial activity in 3T3-L1 and subcutaneous white adipocytes. J. Ginseng Res. 2018 doi: 10.1016/j.jgr.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Gu X. Ginsenoside Rb2 Alleviates Obesity by Activation of Brown Fat and Induction of Browning of White Fat. Diabetes. 2019;68 doi: 10.2337/db19-1757-P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hong Y., Lin Y., Si Q., Yang L., Dong W., Gu X. Ginsenoside Rb2 Alleviates Obesity by Activation of Brown Fat and Induction of Browning of White Fat. Front. Endocrinol. 2019;10:153. doi: 10.3389/fendo.2019.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Chan L.S., Yue P.Y., Kok T.W., Keung M.H., Mak N.K., Wong R.N. Ginsenoside-Rb1 promotes adipogenesis through regulation of PPARγ and microRNA-27b. Horm. Metab. Res. 2012;44:819–824. doi: 10.1055/s-0032-1321909. [DOI] [PubMed] [Google Scholar]
- 156.Lawrence B.M. Mint: The Genus Mentha, Medicinal and Aromatic Plants—Industrial Profiles. 1st ed. CRC Press; Boca Raton, FL, USA: 2006. [Google Scholar]
- 157.Kim S., Lee J.Y. Menthol attenuates the magnitude of cold-induced vasodilation on the extremities of young females. J. Physiol. Anthropol. 2018;37:14. doi: 10.1186/s40101-018-0174-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Blanquart S., Borowiec A.S., Delcourt P., Figeac M., Emerling C.A., Meseguer A.S., Roudbaraki M., Prevarskaya N., Bidaux G. Evolution of the human cold/menthol receptor, TRPM8. Mol. Phylogenet. Evol. 2019;136:104–118. doi: 10.1016/j.ympev.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 159.Ma S., Yu H., Zhao Z., Luo Z., Chen J., Ni Y., Jin R., Ma L., Wang P., Zhu Z., et al. Activation of the cold-sensing TRPM8 channel triggers UCP1-dependent thermogenesis and prevents obesity. J. Mol. Cell Biol. 2012;4:88–96. doi: 10.1093/jmcb/mjs001. [DOI] [PubMed] [Google Scholar]
- 160.Khare P., Mangal P., Baboota R.K., Jagtap S., Kumar V., Singh D.P., Boparai R.K., Sharma S.S., Khardori R., Bhadada S.K., et al. Involvement of glucagon in preventive effect of menthol against high fat diet induced obesity in mice. Front. Pharmacol. 2018;9:1244. doi: 10.3389/fphar.2018.01244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Rossato M., Granzotto M., Macchi V., Porzionato A., Petrelli L., Calcagno A., Vencato J., De Stefani D., Silvestrin V., Rizzuto R., et al. Human white adipocytes express the cold receptor TRPM8 which activation induces UCP1 expression, mitochondrial activation and heat production. Mol. Cell. Endocrinol. 2014;383:137–146. doi: 10.1016/j.mce.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 162.Goralczyk A., van Vijven M., Koch M., Badowski C., Yassin M.S., Toh S.A., Shabbir A., Franco-Obregón A., Raghunath M. TRP channels in brown and white adipogenesis from human progenitors: New therapeutic targets and the caveats associated with the common antibiotic, streptomycin. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2017;31:3251–3266. doi: 10.1096/fj.201601081RR. [DOI] [PubMed] [Google Scholar]
- 163.Khare P., Chauhan A., Kumar V., Kaur J., Mahajan N., Kumar V., Gesing A., Chopra K., Kondepudi K.K., Bishnoi M. Bioavailable Menthol (Transient Receptor Potential Melastatin-8 Agonist) Induces Energy Expending Phenotype in Differentiating Adipocytes. Cells. 2019;8:E383. doi: 10.3390/cells8050383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Jiang C., Zhai M., Yan D., Li D., Li C., Zhang Y., Xiao L., Xiong D., Deng Q., Sun W. Dietary menthol-induced TRPM8 activation enhances WAT “browning” and ameliorates diet-induced obesity. Oncotarget. 2017;8:75114–75126. doi: 10.18632/oncotarget.20540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nabavi S.F., Braidy N., Habtemariam S., Orhan I.E., Daglia M., Manayi A., Gortzi O., Nabavi S.M. Neuroprotective effects of chrysin: From chemistry to medicine. Neurochem. Int. 2015;90:224–231. doi: 10.1016/j.neuint.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 166.Mani R., Natesan V. Chrysin: Sources, beneficial pharmacological activities, and molecular mechanism of action. Phytochemistry. 2018;145:187–196. doi: 10.1016/j.phytochem.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 167.Farkhondeh T., Samarghandian S., Roshanravan B. Impact of chrysin on the molecular mechanisms underlying diabetic complications. J. Cell. Physiol. 2019;234:17144–17158. doi: 10.1002/jcp.28488. [DOI] [PubMed] [Google Scholar]
- 168.Choi J.H., Yun J.W. Chrysin induces brown fat-like phenotype and enhances lipid metabolism in 3T3-L1 adipocytes. Nutrition. 2016;32:1002–1010. doi: 10.1016/j.nut.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 169.Ahn-Jarvis J.H., Riedl K.M., Schwartz S.J., Vodovotz Y. Design and selection of soy breads used for evaluating isoflavone bioavailability in clinical trials. J. Agric. Food Chem. 2013;61:3111–3120. doi: 10.1021/jf304699k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Savini I., Catani M.V., Evangelista D., Gasperi V., Avigliano L. Obesity-associated oxidative stress: Strategies finalized to improve redox state. Int. J. Mol. Sci. 2013;14:10497–10538. doi: 10.3390/ijms140510497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lephart E.D., Porter J.P., Lund T.D., Bu L., Setchell K.D., Ramoz G., Crowley W.R. Dietary isoflavones alter regulatory behaviors, metabolic hormones and neuroendocrine function in Long-Evans male rats. Nutr. Metab. 2004;1:16. doi: 10.1186/1743-7075-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Aziz S.A., Walkening L.A., Miwa S., Alberdi G., Hesketh J.E., Ford D. Metabolic programming of a beige adipocyte phenotype by genistein. Mol. Nutr. Food Res. 2017;61:1600574. doi: 10.1002/mnfr.201600574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zhou L., Xiao X., Zhang Q., Zheng J., Li M., Deng M. A Possible Mechanism: Genistein Improves Metabolism and Induces White Fat Browning Through Modulating Hypothalamic Expression of Ucn3, Depp, and Stc1. Front. Endocrinol. 2019;10:478. doi: 10.3389/fendo.2019.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Crespillo A., Alonso M., Vida M., Pavón F.J., Serrano A., Rivera P., Romero-Zerbo Y., Fernández-Llebrez P., Martínez A., Pérez-Valero V., et al. Reduction of body weight, liver steatosis and expression of stearoyl-CoA desaturase 1 by the isoflavone daidzein in diet-induced obesity. Br. J. Pharmacol. 2011;164:1899–1915. doi: 10.1111/j.1476-5381.2011.01477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhang H., Zhao Z., Pang X., Yang J., Yu H., Zhang Y., Zhou H., Zhao J. Genistein Protects Against Ox-LDL-Induced Inflammation Through MicroRNA-155/SOCS1-Mediated Repression of NF-ĸB Signaling Pathway in HUVECs. Inflammation. 2017;40:1450–1459. doi: 10.1007/s10753-017-0588-3. [DOI] [PubMed] [Google Scholar]
- 176.De la Parra C., Castillo-Pichardo L., Cruz-Collazo A., Cubano L., Redis R., Calin G.A., Dharmawardhane S. Soy Isoflavone Genistein-Mediated Downregulation of miR-155 Contributes to the Anticancer Effects of Genistein. Nutr. Cancer. 2016;68:154–164. doi: 10.1080/01635581.2016.1115104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Thielecke F., Boschmann M. The potential role of green tea catechins in the prevention of the metabolic syndrome—A review. Phytochemistry. 2009;70:11–24. doi: 10.1016/j.phytochem.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 178.Nutrient Data Laboratory; Food Composition Laboratory; Beltsville Human Nutrition Research Center; Nutrient Data Laboratory; [(accessed on 20 September 2019)]. USDA Database for the Flavonoid Content of Selected Foods. Available online: http://www.ars.usda.gov/SP2UserFiles/Place/12354500/Data/Flav/Flav02-1.pdf. [Google Scholar]
- 179.Ahmad M., Ahmad I., Chattopadhyay D. New Look to Phytomedicine: Advancements in Herbal Products as Novel Drug Leads. 1st ed. Academic Press; London, UK: 2019. [Google Scholar]
- 180.Wolfram S. Effects of green tea and EGCG on cardiovascular and metabolic health. J. Am. Coll. Nutr. 2007;26:373S–388S. doi: 10.1080/07315724.2007.10719626. [DOI] [PubMed] [Google Scholar]
- 181.Neyrinck A.M., Bindels L.B., Geurts L., Van Hul M., Cani P.D., Delzenne N.M. A polyphenolic extract from green tea leaves activates fat browning in high-fat-diet-induced obese mice. J. Nutr. Biochem. 2017;49:15–21. doi: 10.1016/j.jnutbio.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 182.Chen L.H., Chien Y.W., Liang C.T., Chan C.H., Fan M.H., Huang H.Y. Green tea extract induces genes related to browning of white adipose tissue and limits weight-gain in high energy diet-fed rat. Food Nutr. Res. 2017;61:1347480. doi: 10.1080/16546628.2017.1347480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Yamashita Y., Wang L., Wang L., Tanaka Y., Zhang T., Ashida H. Oolong, black and pu-erh tea suppresses adiposity in mice via activation of AMP-activated protein kinase. Food Funct. 2014;5:2420–2429. doi: 10.1039/C4FO00095A. [DOI] [PubMed] [Google Scholar]
- 184.Kudo N., Arai Y., Suhara Y., Ishii T., Nakayama T., Osakabe N. A Single Oral Administration of Theaflavins Increases Energy Expenditure and the Expression of Metabolic Genes. PLoS ONE. 2015;10:e0137809. doi: 10.1371/journal.pone.0137809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zhu W., Zou B., Nie R., Zhang Y., Li C.M. A-type ECG and EGCG dimers disturb the structure of 3T3-L1 cell membrane and strongly inhibits its differentiation by targeting peroxisome proliferator-activated receptor γ with miR-27 involved mechanism. J. Nutr. Biochem. 2015;26:1124–1135. doi: 10.1016/j.jnutbio.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 186.Yoneshiro T., Matsushita M., Hibi M., Tone H., Takeshita M., Yasunaga K., Katsuragi Y., Kameya T., Sugie H., Saito M. Tea catechin and caffeine activate brown adipose tissue and increase cold-induced thermogenic capacity in humans. Am. J. Clin. Nutr. 2017;105:873–881. doi: 10.3945/ajcn.116.144972. [DOI] [PubMed] [Google Scholar]
- 187.Pang K., Zhu Z., Zhu S., Han L. A high dose of conjugated linoleic acid increases fatty liver and insulin resistance in lactating mice. PLoS ONE. 2019;14:e0214903. doi: 10.1371/journal.pone.0214903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Roura-Guiberna A., Hernandez-Aranda J., Ramirez-Flores C.J., Mondragon-Flores R., Garibay-Nieto N., Queipo-Garcia G., Laresgoiti-Servitje E., Soh J.W., Olivares-Reyes J.A. Isomers of conjugated linoleic acid induce insulin resistance through a mechanism involving activation of protein kinase Cε in liver cells. Cell Signal. 2019;53:281–293. doi: 10.1016/j.cellsig.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 189.Bhattacharya A., Banu J., Rahman M., Causey J., Fernandes G. Biological effects of conjugated linoleic acids in health and disease. J. Nutr. Biochem. 2006;17:789–810. doi: 10.1016/j.jnutbio.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 190.Brown J.M., McIntosh M.K. Conjugated linoleic acid in humans: Regulation of adiposity and insulin sensitivity. J. Nutr. 2003;133:3041–3046. doi: 10.1093/jn/133.10.3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Shen W., Chuang C.C., Martinez K., Reid T., Brown J.M., Xi L., Hixson L., Hopkins R., Starnes J., McIntosh M. Conjugated linoleic acid reduces adiposity and increases markers of browning and inflammation in white adipose tissue of mice. J. Lipid Res. 2013;54:909–922. doi: 10.1194/jlr.M030924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.McDonald M.E., Li C., Bian H., Smith B.D., Layne M.D., Farmer S.R. Myocardin-related transcription factor A regulates conversion of progenitors to beige adipocytes. Cell. 2015;160:105–118. doi: 10.1016/j.cell.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Barneda D., Planas-Iglesias J., Gaspar M.L., Mohammadyani D., Prasannan S., Dormann D., Han G.S., Jesch S.A., Carman G.M., Kagan V., et al. The brown adipocyte protein CIDEA promotes lipid droplet fusion via a phosphatidic acid-binding amphipathic helix. eLife. 2015;4:e07485. doi: 10.7554/eLife.07485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Jash S., Benerjee S., Lee M.J., Farmer S.R., Puri V. CIDEA transcriptionally regulates UCP1 for britening and thermogenesis in human fat cells. iScience. 2019;20:73–89. doi: 10.1016/j.isci.2019.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Den Hartigh L.J. Conjugated Linoleic Acid Effects on Cancer, Obesity, and Atherosclerosis: A Review of Pre-Clinical and Human Trials with Current Perspectives. Nutrients. 2019;11:E370. doi: 10.3390/nu11020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Shen W., Baldwin J., Collins B., Hixson L., Lee K.T., Herberg T., Starnes J., Cooney P., Chuang C.C., Hopkins R., et al. Low level of trans-10, cis-12 conjugated linoleic acid decreases adiposity and increases browning independent of inflammatory signaling in overweight Sv129 mice. J. Nutr. Biochem. 2015;26:616–625. doi: 10.1016/j.jnutbio.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kennedy A., Martinez K., Chung S., LaPoint K., Hopkins R., Schmidt S.F., Andersen K., Mandrup S., McIntosh M. Inflammation and insulin resistance induced by trans-10, cis-12 conjugated linoleic acid depend on intracellular calcium levels in primary cultures of human adipocytes. J. Lipid Res. 2010;51:1906–1917. doi: 10.1194/jlr.M005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Metges C.C., Lehmann L., Boeuf S., Petzke K.J., Müller A., Rickert R., Franke W., Steinhart H., Nümberg G., Klaus S. cis-9,trans-11 and trans-10,cis-12 CLA affect lipid metabolism differently in primary white and brown adipocytes of Djungarian hamsters. Lipids. 2003;38:1133–1142. doi: 10.1007/s11745-003-1171-0. [DOI] [PubMed] [Google Scholar]
- 199.Bruen R., Fitzsimons S., Belton O. miR-155 in the Resolution of Atherosclerosis. Front. Pharmacol. 2019;10:463. doi: 10.3389/fphar.2019.00463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Albracht-Schulte K., Kalupahana N.S., Ramalingam L., Wang S., Rahman S.M., Robert-McComb J., Moustaid-Moussa N. Omega-3 fatty acids in obesity and metabolic syndrome: A mechanistic update. J. Nutr. Biochem. 2018;58:1–16. doi: 10.1016/j.jnutbio.2018.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Zhao M., Chen X. Eicosapentaenoic acid promotes thermogenic and fatty acid storage capacity in mouse subcutaneous adipocytes. Biochem. Biophys. Res. Commun. 2014;450:1446–1451. doi: 10.1016/j.bbrc.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 202.Laiglesia L.M., Lorente-Cebrián S., Prieto-Hontoria P.L., Fernández-Galilea M., Ribeiro S.M.R., Sáinz N., Martínez J.A., Moreno-Aliaga M.J. Eicosapentaenoic acid promotes mitochondrial biogenesis and beige-like features in subcutaneous adipocytes from overweight subjects. J. Nutr. Biochem. 2016;37:76–82. doi: 10.1016/j.jnutbio.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 203.Bargut T.C., Silva-e-Silva A.C., Souza-Mello V., Mandarim-de-Lacerda C.A., Aguila M.B. Mice fed fish oil diet and upregulation of brown adipose tissue thermogenic markers. Eur. J. Nutr. 2016;55:159–169. doi: 10.1007/s00394-015-0834-0. [DOI] [PubMed] [Google Scholar]
- 204.Kim M., Goto T., Yu R., Uchida K., Tominaga M., Kano Y., Takahashi N., Kawada T. Fish oil intake induces UCP1 upregulation in brown and white adipose tissue via the sympathetic nervous system. Sci. Rep. 2015;5:18013. doi: 10.1038/srep18013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Fleckenstein-Elsen M., Dinnies D., Jenelik T., Roden M., Romacho T., Eckel J. Eicosapentaenoic acid and arachidonic acid differentially regulate adipogenesis, acquisition of a brite phenotype and mitochondrial function in primary human adipocytes. Mol. Nutr. Food Res. 2016;60:2065–2075. doi: 10.1002/mnfr.201500892. [DOI] [PubMed] [Google Scholar]
- 206.Mori M.A., Thomou T., Boucher J., Lee K.Y., Lallukka S., Kim J.K., Torriani M., Yki-Järvinen H., Grinspoon S.K., Cypress A.M., et al. Altered miRNA processing disrupts brown/white adipocyte determination and associates with lipodystrophy. J. Clin. Investig. 2014;124:3339–3351. doi: 10.1172/JCI73468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Calder P.C. The DHA content of a cell membrane can have a significant influence on cellular behavior and responsiveness to signals. Ann. Nutr. Metab. 2016;69:8–12. doi: 10.1159/000448262. [DOI] [PubMed] [Google Scholar]
- 208.Juárez-Hernández E., Chávez-Tapia N.C., Uribe M., Barbero-Becerra V.J. Role of bioactive fatty acids in nonalcoholic fatty liver disease. Nutr. J. 2016;15:72. doi: 10.1186/s12937-016-0191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Zhuang P., Lu Y., Shou Q., Mao L., He L., Wang J., Chen J., Zhang Y., Jiao J. Differential Anti-Adipogenic Effects of Eicosapentaenoic and Docosahexaenoic Acids in Obesity. Mol. Nutr. Food Res. 2019:e1801135. doi: 10.1002/mnfr.201801135. [DOI] [PubMed] [Google Scholar]
- 210.Oliveira T.E., Castro É., Belchior T., Andrade M.L., Chaves-Filho A.B., Peixoto A.S., Moreno M.F., Ortiz-Silva M., Moreira R.J., Inague A., et al. Fish Oil Protects Wild Type and Uncoupling Protein 1-Deficient Mice from Obesity and Glucose Intolerance by Increasing Energy Expenditure. Mol. Nutr. Food Res. 2019;63:e1800813. doi: 10.1002/mnfr.201800813. [DOI] [PubMed] [Google Scholar]
- 211.Crescenzo R., Mazzoli A., Cancelliere R., Bianco F., Giacco A., Liverini G., Dullo A.G., Iossa S. Polyunsaturated fatty acids stimulate de novo lipogenesis and improve glucose homeostasis during refeeding with high fat diet. Front. Physiol. 2017;8:178. doi: 10.3389/fphys.2017.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Kuda O., Rossmeisl M., Kopecky J. Omega-3 fatty acids and adipose tissue biology. Mol. Aspects Med. 2018;64:147–160. doi: 10.1016/j.mam.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 213.Eggersdorfer M., Wyss A. Carotenoids in human nutrition and health. Arch. Biochem. Biophys. 2018;652:18–26. doi: 10.1016/j.abb.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 214.Coronel J., Pinos I., Amengual J. β-carotene in Obesity Research: Technical Considerations and Current Status of the Field. Nutrients. 2019;11:E842. doi: 10.3390/nu11040842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Landrier J.F., Marcotorchino J., Tourniaire F. Lipophilic micronutrients and adipose tissue biology. Nutrients. 2012;4:1622–1649. doi: 10.3390/nu4111622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Gerhard G.S., Styer A.M., Strodel W.E., Roesch S.L., Yavorek A., Carey D.J., Wood G.C., Petrick A.T., Gabrielsen J., Ibele A., et al. Gene expression profiling in subcutaneous, visceral and epigastric adipose tissues of patients with extreme obesity. Int. J. Obes. 2014;38:371. doi: 10.1038/ijo.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Bonet M.L., Canas J.A., Ribot J., Palou A. Carotenoids and their conversion products in the control of adipocyte function, adiposity and obesity. Arch. Biochem. Biophys. 2015;572:112–125. doi: 10.1016/j.abb.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 218.Shabalina I.G., Backlund E.C., Bar-Tana J., Cannon B., Nedergaard J. Within brown-fat cells, UCP1-mediated fatty acid-induced uncoupling is independent of fatty acid metabolism. Biochim. Biophys. Acta. 2008;1777:642–650. doi: 10.1016/j.bbabio.2008.04.038. [DOI] [PubMed] [Google Scholar]
- 219.Serra F., Bonet M.L., Puigserver P., Oliver J., Palou A. Stimulation of uncoupling protein 1 expression in brown adipocytes by naturally occurring carotenoids. Int. J. Obes. Relat. Metab. Disord. 1999;23:650–656. doi: 10.1038/sj.ijo.0800897. [DOI] [PubMed] [Google Scholar]
- 220.Guo H., Foncea R., O’Byrne S.M., Jiang H., Zhang Y., Deis J.A., Blaner W.S., Bernlohr D.A., Chen X. Lipocalin 2, a regulator of retinoid homeostasis and retinoidmediated thermogenic activation in adipose tissue. J. Biol. Chem. 2016;291:11216–11229. doi: 10.1074/jbc.M115.711556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Maeda H. Nutraceutical effects of fucoxanthin for obesity and diabetes therapy: A review. J. Oleo Sci. 2015;64:125–132. doi: 10.5650/jos.ess14226. [DOI] [PubMed] [Google Scholar]
- 222.Sugawara T., Baskaran V., Tsuzuki W., Nagao A. A Brown algae fucoxanthin is hydrolyzed to fucoxanthinol during absorption by Caco-2 human intestinal cells and mice. J. Nutr. 2002;132:946–951. doi: 10.1093/jn/132.5.946. [DOI] [PubMed] [Google Scholar]
- 223.Peng J., Yuan J.P., Wu C.F., Wang J.H. Fucoxanthin, a marine carotenoid present in brown seaweeds and diatoms: Metabolism and bioactivities relevant to human health. Mar. Drugs. 2011;9:1806–1828. doi: 10.3390/md9101806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Abidov M., Ramazanov Z., Seifulla R., Grachev S. The effects of Xanthigen in the weight management of obese premenopausal women with non-alcoholic fatty liver disease and normal liver fat. Diabetes Obes. Metab. 2010;12:72–81. doi: 10.1111/j.1463-1326.2009.01132.x. [DOI] [PubMed] [Google Scholar]
- 225.Maeda H., Hosokawa M., Sashima T., Takahashi N., Kawada T., Miyashita K. Fucoxanthin and its metabolite, fucoxanthinol, suppress adipocyte differentiation in 3T3-L1 cells. Int. J. Mol. Med. 2006;18:147–152. doi: 10.3892/ijmm.18.1.147. [DOI] [PubMed] [Google Scholar]
- 226.Kim S.M., Jung Y.J., Kwon O.N., Cha K.H., Um B.H., Chung D., Pan C.H. A potential commercial source of fucoxanthin extracted from the microalga Phaeodactylum tricornutum. Appl. Biochem. Biotechnol. 2012;166:1842–1855. doi: 10.1007/s12010-012-9602-2. [DOI] [PubMed] [Google Scholar]
- 227.Maeda H., Hosokawa M., Sashima T., Funayama K., Miyashita K. Fucoxanthin from edible seaweed, Undaria pinnatifida, shows antiobesity effect through UCP1 expression in white adipose tissues. Biochem. Biophys. Res. Commun. 2005;332:392–397. doi: 10.1016/j.bbrc.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 228.Rebello C.J., Greenway F.L., Lau F.H., Lin Y., Stephens J.M., Johnson W.D., Coulter A.A. Naringenin Promotes Thermogenic Gene Expression in Human White Adipose Tissue. Obesity. 2019;27:103–111. doi: 10.1002/oby.22352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Favela-Hernández J.M., González-Santiago O., Ramírez-Cabrera M., Esquivel-Ferriño P., Camacho-Corona M. Chemistry and Pharmacology of Citrus sinensis. Mol. Nutr. Food Res. 2016;21:247. doi: 10.3390/molecules21020247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Zou Z., Xi W., Hu Y., Nie C., Zhou Z. Antioxidant activity of Citrus fruits. Food Chem. 2015;196:885–896. doi: 10.1016/j.foodchem.2015.09.072. [DOI] [PubMed] [Google Scholar]
- 231.De la Garza A.L., Etxeberria U., Haslberger A., Aumueller E., Martínez J.A., Milagro F.I. Helichrysum and Grapefruit Extracts Boost Weight Loss in Overweight Rats Reducing Inflammation. J. Med. Food. 2015;18:890–898. doi: 10.1089/jmf.2014.0088. [DOI] [PubMed] [Google Scholar]
- 232.Nakajima V.M., Macedo G.A., Macedo J.A. Citrus bioactive phenolics: Role in the obesity treatment. LWT Food Sci. Technol. 2014;59:1205–1212. doi: 10.1016/j.lwt.2014.02.060. [DOI] [Google Scholar]
- 233.Huong D.T.T., Takahashi Y., Ide T. Activity and mRNA levels of enzymes involved in hepatic fatty acid oxidation in mice fed citrus flavonoids. Nutrition. 2006;22:546–552. doi: 10.1016/j.nut.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 234.Alam M.A., Subhan N., Rahman M.M., Uddin S.J., Reza H.M., Sarker S.D. Effect of citrus flavonoids, naringin and naringenin, on metabolic syndrome and their mechanisms of action. Adv. Nutr. 2014;5:404–417. doi: 10.3945/an.113.005603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Kim G.S., Park H.J., Woo J.H., Kim M.K., Koh P.O., Min W., Ko Y.G., Kim C.H., Won C.K., Cho J.H. Citrus aurantium flavonoids inhibit adipogenesis through the Akt signaling pathway in 3T3-L1 cells. BMC Complement. Altern. Med. 2012;12:31. doi: 10.1186/1472-6882-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Park J., Kim H.L., Jung Y., Ahn K.S., Kwak H.J., Um J.Y. Bitter Orange (Citrus aurantium Linné) Improves Obesity by Regulating Adipogenesis and Thermogenesis through AMPK Activation. Nutrients. 2019;11:1988. doi: 10.3390/nu11091988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Chou Y.C., Ho C.T., Pan M.H. Immature Citrus reticulata Extract Promotes Browning of Beige Adipocytes in High-Fat Diet-Induced C57BL/6 Mice. J. Agric. Food Chem. 2018;66:969–9703. doi: 10.1021/acs.jafc.8b02719. [DOI] [PubMed] [Google Scholar]
- 238.Nishikawa S., Hyodo T., Nagao T., Nakanishi A., Tandia M., Tsuda T. α-Monoglucosyl Hesperidin but Not Hesperidin Induces Brown-Like Adipocyte Formation and Suppresses White Adipose Tissue Accumulation in Mice. J. Agric. Food Chem. 2019;67:1948–1954. doi: 10.1021/acs.jafc.8b06647. [DOI] [PubMed] [Google Scholar]