Abstract
In adults with autism spectrum disorder (ASD), co-occurring psychiatric conditions are prevalent, and depression is one of the most common co-occurring disorders. The current study examined the relationship between depression and cognitive ability, autistic symptom severity, and self-reported social impairments in ASD. Thirty-three adults with ASD and 28 adults with typical development (TD) completed a standardized psychiatric interview, cognitive test, measure of clinician-rated autism symptom severity, and self-report of social impairments. Nine participants with ASD (27%) met criteria for a depressive disorder (ASD+DEP). Relatively more females with ASD had a co-occurring depressive disorder. The TD group had a higher IQ than the ASD group, but the ASD+DEP did not differ from the TD or ASD group. While the ASD+DEP group had lower clinician-rated autism symptom severity than the ASD group, the ASD+DEP group reported more social impairments than the ASD group. Self-reported social impairments predicted depression in adults with ASD when accounting for symptom severity and cognitive ability. These findings suggest that more self-perceived social impairments are related to depressive disorders in ASD, and may help clinicians identify individuals who are vulnerable in developing a co-occurring depressive disorder. Future directions include follow-up studies with larger cohorts and longitudinal designs to support inferences regarding directionality of these relationships.
Background
Autism spectrum disorder (ASD) is defined by impairments in social communication and the presence of restricted and repetitive behaviors and atypical response to sensory information (American Psychiatric Association, 2013). In addition to these core symptoms, co-occurring psychiatric conditions are common in ASD throughout adolescence and adulthood (Buck et al., 2014; Croen et al., 2015; Ghaziuddin & Zafar, 2008; Lever & Geurts, 2016; Lugnegård, Hallerbäck, & Gillberg, 2011; Moseley, Tonge, Brereton, & Einfeld, 2011). Depression is one of the most commonly observed co-occurring conditions in adults with ASD (Ghaziuddin, Ghaziuddin, & Greden, 2002; Lever & Geurts, 2016; Lugnegård et al., 2011; Roy, Prox-Vagedes, Ohlmeier, & Dillo, 2015). The lifetime prevalence of depression in ASD is estimated to be 14 percent, and the current prevalence is higher than adults with typical development (TD; Hudson et al., 2018) as well as those with other psychiatric conditions (Joshi et al., 2013). A recent study following individuals up to the age of 27 years found approximately 20% of individuals with ASD had a diagnosis of depression compared to 6% of the general population (Rai et al., 2018). In the general population, depression is noted to exert a greater health burden among women (Kuehner, 2017; Kuehner, 2003), but sex differences in ASD are unclear, with some studies suggesting increased depressive symptoms in females (Gotham, Brunwasser, & Lord, 2015) and others indicating similarities among males and females (De-la-Iglesia & Olivar, 2015; Hudson et al., 2018).
Depression exerts significant impact on daily functioning. In the general population, depressive disorders affect 322 million people (World Health Organization, 2017), and are a leading cause of health burden (Ferrari et al., 2013). Depressive disorders are the largest global contributor of Years Lived with Disability (YLD), a measure of functional impairment due to a disease (World Health Organization, 2017). Depressive symptoms are often accompanied by impairments in psychosocial functioning, affecting one’s occupation and relationships (Godard, Baruch, Grondin, & Lafleur, 2012). Even when depressive symptoms remit, impairments in psychosocial functioning may remain (Kennedy et al., 2007; Marangell et al., 2009). In ASD, co-occurring psychiatric conditions are also related to poorer psychosocial outcomes in both children (Chiang & Gau, 2016) and adults (Gillberg, Helles, Billstedt, & Gillberg, 2016; Hofvander et al., 2009). A specific relationship is observed between depression and poorer adaptive functioning in ASD (Kraper et al., 2017; Stewart et al., 2006). Co-occurring psychopathology contributes to a larger discrepancy between adaptive functioning and IQ for young adults with ASD (Kraper et al., 2017). A better understanding of the etiology, course, and treatment of co-occurring disorders in ASD offers a promising avenue to improve psychosocial outcomes, adaptive functioning, and quality of life for adults with ASD.
In addition to poorer adaptive functioning and psychosocial outcomes, depression is associated with increased mortality. In the general population, suicide was the leading cause of death globally among 15 to 29 year olds in 2015 and accounted for close to 1.5% of deaths worldwide (World Health Organization, 2017). Individuals with ASD and co-occurring depression are at higher risk for suicidal ideation and behavior (Hedley & Uljarević, 2018) with depression representing the most common risk factor for suicidal attempts (Zahid & Upthegrove, 2017). Understanding predisposing factors and the presentation of depressive disorders in ASD holds promise to identify vulnerable individuals and to connect them to treatment, offering potentially life-saving intervention (Hedley & Uljarević, 2018).
Proposed risk factors for co-occurring depressive disorders in ASD include biological, psychological, and social factors, such as family history, gender, age, genetic factors, social relationships, and life events (for a full review, see Ghaziuddin, Ghaziuddin, & Greden, 2002; De-la-Iglesia & Olivar, 2015). Another proposed risk factor is awareness of social impairments (De-la-Iglesia & Olivar, 2015; Wing, 1981; Wing, 1996) which is described as being aware of one’s disability and differences from other groups of people. Depression in ASD has been examined in relation to cognitive ability and autism symptomology since these two variables may influences one’s perception of their social impairments (Sterling, Dawson, Estes, & Greenson, 2008) and may act as proxy measures of “self-awareness.” Investigations into these relationships have yielded mixed results.
In children, higher IQ was related to more depressive symptoms (Mazurek et al., 2010; Mayes et al., 2011), yet another study did not show a relationship between IQ and depression (Strang et al., 2012). In terms of autism severity, one study reported lower symptom severity was related to more depressive symptoms (Mazurek et al., 2010), yet other studies revealed higher symptom severity was related to depression (Rai et al., 2018; Mayes et al., 2011), and another study demonstrated no relationship between symptom severity and depression (Strang et al., 2012). In a review examining depression in children and adults with ASD, samples that included individuals with an intellectual disability revealed a significantly higher rate of depression in individuals with ASD and without an intellectual disability (Hudson et al., 2018).
In studies on adults, similar inconsistencies have emerged; some studies indicated higher IQ was related to more depressive symptoms (Sterling et al., 2008; Chandrasekhar & Sikich, 2015) while other studies reported no relationship between IQ and depression (Gotham, Unruh & Lord, 2015; Cederlund et al., 2010). In reviews on adults specifically, adults with ASD and without an intellectual disability were more likely to have depression than adults with an intellectual disability (Hollocks et al., 2019; Rai et al., 2018). Regarding autism severity, one study reported lower symptom severity was related to more depressive symptoms (Sterling et al., 2008).
These discrepancies may be due to the different ages studied, children versus adults, as well as the differences in the population studied, whether or not individuals with an intellectual disability were included. Another factor that may contribute to these discrepancies is the varying modalities of assessing autism severity, e.g., clinician or parent report. In addition to cognitive ability and clinician report, the self-perception of social difficulties may be a clinically useful predictor of depression in ASD. Studies using self-report measures indicate that greater self-perceived autistic impairments in young adults (Gotham, Bishop, Brunwasser, & Lord, 2014) and lower self-perceived social competence in adolescents (Vickerstaff, Heriot, Wong, Lopes, & Dossetor, 2007) were related to higher depressive symptoms. Notably, discrepancies have been observed between clinicians and parents, but using both parent report and clinician observation is the gold standard for diagnosing ASD (Lemler, 2012). Thus, comparing self-report to clinician report may be clinically useful since emerging evidence suggests discrepant reports may better predict outcomes and provide valuable additional information (Ward, Sullivan, & Gilmore, 2018; Lerner, Calhoun, Miakmi, & De Los Reyes, 2012; Kanne, Abbacchi, & Constantino, 2009, Hurtig et al., 2009).
The current study sought to address observed inconsistencies in prior research by studying depression in ASD in relation to self-perceived versus clinician-rated social impairments and in the context of cognitive ability. We utilized standardized clinician-administered interviews to assess autistic and depressive symptomatology and a self-report measure of social impairments to examine standardized clinician-rated symptomatology and self-perceived social impairments. Because most studies examining depression in ASD have focused on children and adolescents (Wigham et al., 2017), we studied adults with ASD, a particularly relevant group given that average age of onset for depression ranges from 25 to 32 years old in the general population (Kessler et al., 2005). Based on previous literature examining cognitive ability and clinician ratings in relation to depressive symptoms, we predicted that adults with ASD and depressive disorders would exhibit higher verbal cognitive ability and lower clinician-rated autism symptom severity. In addition, we predicted adults with ASD and co-occurring depression would have more self-reported social impairments.
Methods
Participants
These data were collected as part of a larger study examining social functioning, eye-tracking, and electroencephalography across neurodevelopmental disorders in adults (R01 MH107426, James McPartland, PI). Clinical assessments and self-report measures reported here were collected over two to three days in this context. All participants were recruited from the greater New Haven area through flyers. In addition, participants with ASD were recruited through autism related events and re-contacting individuals from the Yale Autism Program Research Registry with a focus on recruiting females with ASD to permit comparisons by sex. All participants were evaluated by a trained clinical psychologist or by a master’s level clinician under the supervision of a trained clinical psychologist. Inclusion and exclusion criteria were more stringent than many clinical studies because participants were recruited according to criteria for neuroscience research. All participants were between 18 to 36 years old and had a full-scale IQ of 70 or higher. Adults with TD were included if they did not meet criteria for any psychiatric conditions based on the Mini-International Neuropsychiatric Interview (MINI, described more below) and clinical judgment. Individuals with ASD were included if they met DSM-5 clinical criteria for ASD, received a calibrated severity score (CSS) of four or higher on the Autism Diagnostic Observation Schedule (ADOS, described more below), and had no history of genetic medical conditions etiologically related to ASD. Exclusionary criteria across groups included alcohol use in the preceding 24 hours, recreational drug use in the preceding 48 hours, chronic drug abuse, medication changes within the prior two weeks, any history of seizures (except for febrile infantile seizures), tic disorders or tremors, history of electroconvulsive therapy, bipolar disorder, and uncorrected visual, auditory, sensory-motor difficulties, neurological disorder, brain damage, or head injury. The final TD (n = 28) and ASD (n = 33) groups did not differ on gender [χ(1) = 1.63, p > .10] or age [t(59) = 0.55, p > .10]. Though the ASD group had a mean IQ within the average range (M = 104, SD = 16), their full-scale IQ was lower than the TD group (M = 116, SD = 15), [t(58) = 3.08, p< .01]. All procedures were conducted with the consent of participants and with approval of the Yale School of Medicine Human Investigation Committee.
Measures
Clinical assessments of depression, cognitive ability, and clinician-rated autism symptom severity were collected in addition to self-report of social impairments.
WASI-II
The Wechsler Abbreviated Scale of Intelligence, Second Edition (WASI-II) is an abbreviated measure of cognitive ability for individuals aged 6 to 90 years. Full-scale IQ was calculated based on administration of all four subtests (FSIQ-4). Since individuals with ASD often display discrepant verbal and performance IQ scores, the verbal and performance subtests were examined in addition to the full-scale IQ (Wechsler, 2011).
ADOS-2 Module 4
The Autism Diagnostic Observation Schedule, 2nd edition (ADOS-2) is a semi-structured autism diagnostic observation with increasing modules for increasing verbal and development levels. For the verbally fluent adults in this sample, Module 4 was employed (Lord et al., 2012). The calibrated severity score (CSS), a calibrated measure of ASD symptom severity that can be compared across modules (Hus & Lord, 2014), was calculated, and individuals with a CSS of 4 or greater were included in the study.
SRS-2
The adult self-report measure, the Social Responsiveness Scale 2nd edition (SRS-2), was administered as a self-report of social impairments in ASD. The social communication and interaction (SCI) and restricted and repetitive behavior (RRB) sections align with DSM-5 ASD criteria and, together, yield a total score (Constantino & Gruber, 2012). To examine the relationship between depression and self-reported social impairments in ASD, the SCI t-score was utilized.
MINI
The Mini-International Neuropsychiatric Interview (MINI) is a brief, structured, diagnostic interview for DSM-IV and ICD-10 psychiatric disorders. Major depressive disorder and dysthymic disorder are evaluated in the past two weeks and past two years, respectively (Hergueta, Baker, & Dunbar, 1998). No participants with TD met criteria for any psychiatric disorders on the MINI. Participants with ASD were placed in the ASD and depressive disorder group (ASD+DEP) if they met MINI criteria for Major Depressive Episode, Current; Major Depressive Episode, Recurrent; Major Depressive Episode with Melancholic Features, Current; or Dysthymia, Current.
Statistical Approach
Differences between the ASD, ASD+DEP, and TD groups were examined utilizing a chi-square test for sex, and one-way analysis of variance (ANOVA) with effect sizes, eta-squared (η2), and Bonferroni adjusted post-hoc tests for significant findings for IQ, CSS, and SCI t-score. Since the test is sensitive to outliers, the one-way ANOVAs were examined with and without outliers. Outliers were identified as 1.5 times the interquartile range (IQR) above the third quartile or below the first quartile. A multivariate logistic regression was run to determine whether variables of interest, cognitive ability, clinician-rated autism severity, and self-reported social impairments, predicted depression status in adults with ASD.
Results
ASD and Depression
Of 33 participants with ASD, nine (27.3%) met criteria for at least one of the depressive disorders on the MINI (Table 1). Because of the small sample size, these findings are considered exploratory. There was a significant difference in sex between the groups [χ(2) = 6.0, p< .05]. Follow-up chi-squared tests revealed the ASD group had significantly fewer females (n = 4) than the TD (n = 12, p < .05) and ASD+DEP (n = 5, p< .05) groups (Table 1). Five out of nine females with ASD (56%), compared to four out of 24 (17%) of males with ASD, had co-occurring depression. Groups did not differ on age [F(2, 58) = 0.26, p > .10, η2 = .01], and age was not correlated with behavioral measures (Table 2).
Table 1.
Sex and Age in the ASD, ASD+DEP, and TD groups
| ASD | ASD+DEP | TD | |
|---|---|---|---|
| Total (n) | 24 | 9 | 28 |
| Female (n, (%)) | 4* (17%) | 5* (56%) | 12* (43%) |
| Age (M, (SD)) | 23.7 (4.7) | 24.5 (5.9) | 24.5 (4.0) |
Note. The ASD group had significantly fewer females than the ASD+DEP group and the TD group.
p< .05
Table 2.
Spearman’s Rank Correlations across the ASD and ASD+DEP groups.
| Age | ADOS CSS | Verbal IQ | Performance IQ | Full-scale IQ | |
|---|---|---|---|---|---|
| ADOS CSS | 0.19 | – | |||
| Verbal IQ | 0.15 | −0.44* | – | ||
| Performance IQ | −0.16 | −0.17 | 0.50** | – | |
| Full-scale IQ | 0.02 | −0.38* | 0.91** | 0.81** | – |
| SRS SCI t-score | 0.21 | −0.03 | −0.12 | 0.01 | −0.07 |
Note.
p< .05,
p< .01
Differences in Cognitive Ability, Clinician-Rated Autism Severity, and Self-Reported Social Impairments between the TD, ASD, and ASD+DEP Groups
One-way ANOVAs with diagnosis (ASD, ASD+DEP, TD) as a between-subjects factor were carried out to determine whether differences between IQ, clinician-rated autism severity, or self-reported social impairments were present (Table 3, Figure 1). Differences in all domains emerged (ps < .05).
Table 3.
Mean Scores and Post-hoc Results in the ASD, ASD+DEP, and TD groups
|
M (SD) |
||||
|---|---|---|---|---|
| Measure | ASD | ASD+DEP | TD | Post-hoc |
| Verbal IQ | 100 (18.7) | 112 (16.7) | 118 (17.0) | ASD < TD |
| Performance IQ | 101 (15.7) | 107 (13.2) | 110 (13.4) | |
| Full-scale IQ | 101 (16.6) | 111 (14.6) | 116 (14.7) | ASD < TD |
| ADOS CSS | 7.9 (1.6) | 6.3 (1.7) | 1.4 (0.6) | TD < ASD+DEP < ASD |
| SRS SCI t-score | 57.6 (9.5) | 68.7 (10.3) | 46.9 (8.4) | TD < ASD < ASD+DEP |
Note. The post-hoc column indicates a significant difference (p< .05) between groups.
Figure 1.
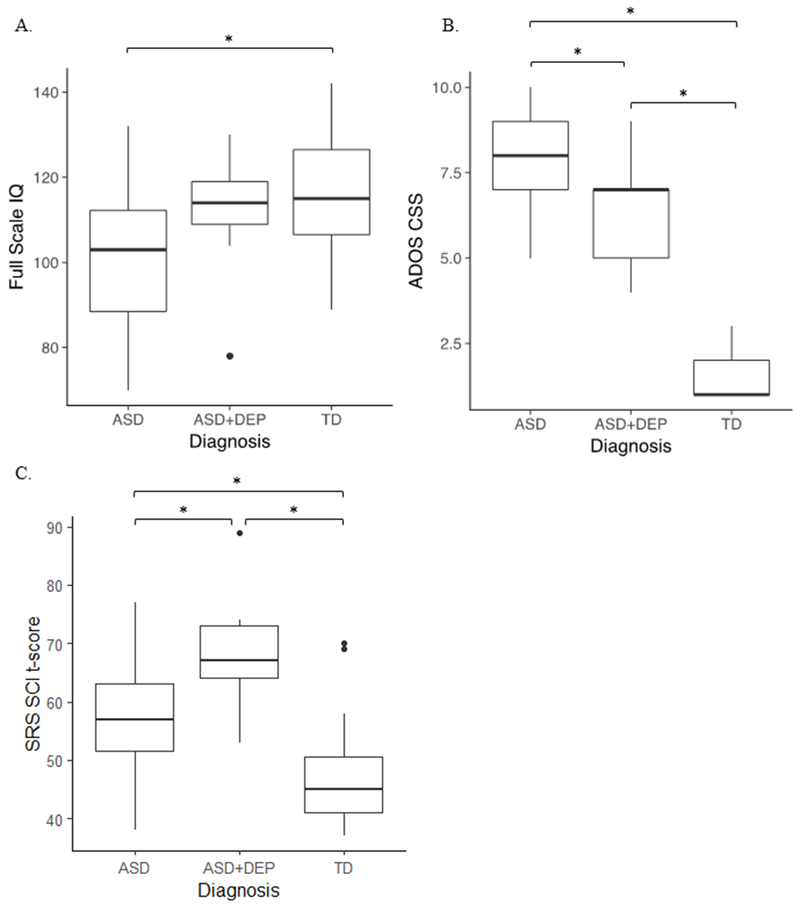
Boxplots of full-scale IQ (A), ADOS CSS (B), and SRS SCI t-score (C) by group.* p< .05.
Cognitive Ability
Differences in verbal [F(2, 57) = 6.92, p< .01, η2 = .20] and full-scale [F(2, 57) = 6.31, p< .01, η2 = .18] IQ emerged. The ASD+DEP group did not differ from the ASD or TD group on verbal or full-scale IQ (Figure 1A, ps > .10). The ASD group had significantly lower verbal and full-scale IQ than the TD group, and these findings remained significant after outliers were removed (ps < .05). No differences in performance IQ were observed [F(2, 57) = 2.45, p = .10, η2 = .08].
Clinician-Rated Autism Severity
The groups differed on CSS [F(2, 58) = 177.5, p< .01, η2 = .86] such that the TD group had significantly lower scores than both the ASD and ASD+DEP groups (Figure 1B, ps < .05), and the ASD+DEP had significantly lower scores than the ASD group (p< .05).
Self-Reported Social Impairments
On the SRS, groups differed on the SCI t-score [F(2, 57) = 21.8, p< .01, η2 = .43]. The TD group had significantly lower scores, indicating fewer self-reported social impairments compared to the ASD and ASD+DEP groups (Figure 1C, ps < .05), and the ASD group had significantly lower scores than the ASD+DEP group (p< .05). These findings remained significant after outliers were removed (ps < .05).
Relationships among Cognitive Ability, Clinician-Rated Autism Severity, Self-Reported Social Impairments, and Depression in ASD
Relationships among cognitive ability (full-scale IQ), clinician-rated autism severity (CSS), self-reported social impairments (SCI t-score), and depression were examined with multivariate logistic regression. A multivariate logistic regression was performed with the diagnosis of depression as the outcome variable, and cognitive ability, clinician-rated autism severity and self-reported social impairments in adults with ASD (Table 4) as the predictors The model indicated that self-reported social impairments were associated with depression in adults with ASD (Figure 2, p< .05) with an odds ratio of 1.16 (95% CI = 1.04 – 1.39), such that, for an increase of 1 point on the SCI t-score, the odds of having depression increased by a factor of 1.16. Clinician-rated autism severity was marginally associated with depression in adults with ASD (p = .08) with an odds ratio of .55 (95% CI = .26 – 1.01). However, there was no association with cognitive ability (p = .18) and the odds of having depression, 1.05 (95% CI = .98 – 1.14).
Table 4.
Predictors of Depression: Results From Multivariate Regression Model.
| Estimate | Standard Error | Z-Value | P-value | VIF | OR [95% CI] | |
|---|---|---|---|---|---|---|
| Intercept | −11.44 | 6.70 | −1.71 | 0.09† | 0.01 [0.01 1.35] | |
| Full-scale IQ | 0.05 | 0.04 | 1.34 | 0.18 | 1.16 | 1.05 [0.98 1.14] |
| ADOS CSS | −0.59 | 0.34 | −1.76 | 0.08† | 1.15 | 0.55 [0.26 1.01] |
| SRS SCI t-score | 0.15 | 0.07 | 2.19 | 0.03* | 1.01 | 1.16 [1.04 1.39] |
Note.
p< .10,
p< .05
Figure 2.
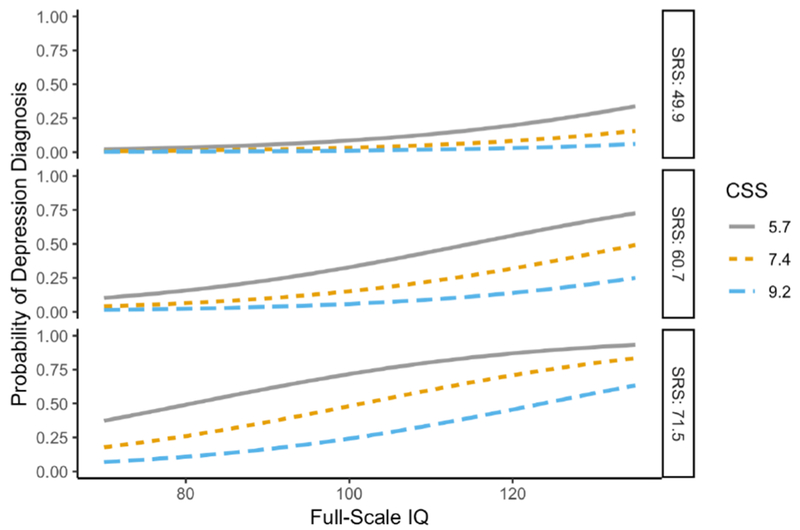
A multivariate logistic regression with depression diagnosis as the outcome variable where 0.00 indicates low probability of receiving a depression diagnosis. Full-scale IQ, CSS, and SCI t-score were the predictors. A diagnosis of depression was predicted by increasing SRS SCI t-score (p< .05), marginally predicted by decreasing CSS score (p< .10), and was not predicted by full-scale IQ (p = .18).
Discussion
This study examined the relationship between co-occurring depression and cognitive ability, clinician-rated autism severity, and self-perceived social impairments in adults with ASD. A structured diagnostic interview was utilized to determine the presence of co-occurring depressive disorders in individuals with ASD. Contrary to our hypotheses, adults with ASD and depressive disorders did not differ from either adults with ASD or adults with TD on measures of cognitive ability. However, as predicted, adults with ASD and depressive disorders exhibited lower clinician-rated autism severity yet more self-reported social impairments than adults with ASD.
The rate of depressive disorders in this sample of adults with ASD (27.3%) was consistent with a recent meta-analysis of depression in studies that used a standardized, self-reported assessment of current depressive symptoms (25.9%, 95% CI = 17.0 – 37.3; Hudson et al., 2018). While other studies have not found sex differences (De-la-Iglesia & Olivar, 2015; Hudson et al., 2018), here, we observed a greater proportion of females among individuals with depression and ASD (compared to ASD alone). Emerging evidence suggests females with ASD show a greater increase in depressive and anxiety symptoms throughout adolescence (Gotham, Brunwasser, & Lord, 2015), and a study in adults with ASD utilizing a self-report of depression found significantly more women than men had depression (Gotham, Unruh & Lord, 2015). This highlights the importance of examining sex differences after puberty since the relationship between changes in estrogen and androgen to depressive symptoms in ASD are potentially relevant but poorly understood (Ghaziuddin et al., 2002). Furthermore, in the general population (Brody, Pratt, & Hughes, 2018), the prevalence of depression in females (10%) and males (6%) is considerably lower than the rates in the current study for females with ASD (56%) and males with ASD (17%). Higher rates of depression in females is observed in the general population and the current study, and the burden of depression in ASD across sexes demonstrates the need to identify effective diagnostic measures and treatments for depression in ASD.
Cognitive ability, clinician-rated autism severity, and self-perceived social impairments in relation to depressive symptoms were also examined. Contrary to another study in adults with ASD, differences in verbal and full-scale IQ between the ASD group and ASD and depressive disorders group were not found (Sterling et al., 2008). Of note, while the ASD group did have a significantly lower IQ than the TD group, the ASD and depressive disorders group did not significantly differ from the TD group. If differences between the ASD and depressive disorders group and the ASD or TD groups exist, the current study may have been underpowered to detect these differences. The null findings in the current study may also reflect inclusion criteria since this study required IQ greater than or equal to 70 while the Sterling and colleagues study included individuals with full-scale IQ as low as 57. The failure to detect a significant relationship between cognitive ability and depression is consistent with other studies with an IQ ≥ 70 inclusion criteria (Gotham, Unruh & Lord, 2015; Cederlund et al., 2010; Strang et al., 2012).
Regarding the relationship between clinician-rated autism severity and depression, we found lower clinician-rated autism severity as measured by the ADOS-2 CSS in adults with ASD and depressive disorders compared to adults with ASD. A similar relationship between lower autism severity and depression was also found in prior samples of children and adolescents (Mazurek & Kanne, 2010) and adults (Sterling et al., 2008). Because the CSS can be scored across modules and relative to language and age level, future longitudinal studies examining the development of depression in ASD can utilize the CSS to determine the direction of the relationship between autism symptom severity and depression.
Finally, our results indicated that greater self-reported social impairments were predictive of depression. Notably, the mean SRS SCI t-score for the ASD group was in the normal range, while the mean score of the ASD and depressive disorders group was in the moderate range, i.e., symptoms are “clinically significant and lead to substantial interference with everyday social interactions” (Constantino & Gruber, 2012). Interference with social interactions has been studied in children, indicating children with low self-perceived social competence have more depressive symptoms (Vickerstaff et al., 2007). This may signify that depressive symptoms lowers the view of one’s social abilities as indiciated by more self-reported social difficulties. Yet the current results demonstrate a contradictory pattern between self-reported versus clinician-rated autism severity. We interpret the relationship among greater self-reported symptomatology and depression (despite lower clinician-rated severity) as evidence for the potential influence of self-perception on development of depressive symptomatology. In other words, individuals who, even potentially inaccurately, see themselves as more severely impacted, may be at greater risk for depression.
The finding that lower clinician-rated autism severity was associated with depression may, in part, reflect the specific items contributing to the clinician score. For example, “insight” is an item on the ADOS-2, with a lower score indicating more typical understanding of social relationships. An individual with a better understanding of typical relationships and social communication may be more likely to perceive their behavior as atypical. Clinicians working with individuals who report more social impairments should be vigilant for depressive problems even if clinician perception of autistic symptoms indicates reduced severity. The cross-sectional nature of this study precludes verification of this interpretation, so we consider this interpretation hypothesis-generating and requiring confirmation in studies designed to support directional influence.
We identified a number of factors related to co-occurring depression in ASD including female sex, lower clinician-rated autism severity, and more self-reported social impairments in adulthood. Using widely administered measures, the ADOS-2 and SRS-2, these findings are readily translatable for future studies in larger cohorts and longitudinal samples. Furthermore, the pattern of lower severity as per clinician report and higher self-perceived difficulties may represent a potential clinical marker indicating risk for depressive disorders. Given the link between depressive disorders and reduced adaptive function and increased suicide risk, understanding the presentation of depression in ASD may yield significant public health benefits, including improvement in psychosocial outcomes and adaptive functioning.
The current study had a number of limitations. As previously mentioned, the study is cross-sectional; therefore, longitudinal studies are necessary to determine the directionality of these relationships. For example, we found a relationship between self-reported social impairments and depression in ASD, but we cannot determine whether this self-perception preceded the development of depression or vice versa. Longitudinal or sufficiently large studies can determine whether awareness into social impairments is a risk factor for later developing depression, or a marker of current depression. Another limitation is the small sample size; thus, this study may be underpowered to detect differences (i.e., higher IQ and depression). While there was an increased odds of more self-reported social impairments in adults with ASD and depression, the confidence interval approached one, highlighting the need for larger samples to confirm this result. Larger sample sizes will also allow for more complex models to test the potential moderating effects of factors such as age, sex, and cognitive ability. In future studies a depression group is critical since it is likely more similar to the ASD+DEP group compared to the TD group, and therefore may allow for the identification of the similarities, or lack thereof, in the presentation of depression in ASD. The study excluded individuals with an IQ below 70, and required individuals to verbally express their experiences, on the MINI, and self-report, on the SRS. These requirements preclude many individuals on the spectrum therefore other risk factors for co-occurring depression should be explored for these groups.
The current study suggests that more self-reported social impairments and lower clinician-rated autism severity are related to depression in adults with ASD. The relationship between cognitive ability and depression is still unclear since adults with ASD and depression did not differ from either adults with ASD or adults with TD. Clinicians can utilize these features, more self-reported social impairments and lower clinician-rated autism severity, to identify individuals with ASD at risk for developing depressive disorders.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub. [Google Scholar]
- Brody DJ, Pratt LA, & Hughes JP (2018). Prevalence of Depression Among Adults Aged 20 and Over: United States, 2013–2016. NCHS data brief, (303), 1–8. [PubMed] [Google Scholar]
- Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, & Bilder DA (2014). Psychiatric Comorbidity and Medication Use in Adults with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 44(12), 3063–3071. doi: 10.1007/s10803-014-2170-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cederlund M, Hagberg B, & Gillberg C (2010). Asperger syndrome in adolescent and young adult males. Interview, self- and parent assessment of social, emotional, and cognitive problems. Research in Developmental Disabilities, 31(2), 287–298. doi: 10.1016/j.ridd.2009.09.006 [DOI] [PubMed] [Google Scholar]
- Chandrasekhar T, & Sikich L (2015). Challenges in the diagnosis and treatment of depression in autism spectrum disorders across the lifespan. Dialogues in clinical neuroscience, 17(2), 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang HL, & Gau SSF (2016). Comorbid psychiatric conditions as mediators to predict later social adjustment in youths with autism spectrum disorder. Journal of Child psychology and Psychiatry, 57(1), 103–111. [DOI] [PubMed] [Google Scholar]
- Constantino JN, & Gruber CP (2012). The Social Responsiveness Scale Manual, Second Edition (SRS-2). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, & Kripke C (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. doi: 10.1177/1362361315577517 [DOI] [PubMed] [Google Scholar]
- De-la-Iglesia M, & Olivar J-S (2015). Risk Factors for Depression in Children and Adolescents with High Functioning Autism Spectrum Disorders. The Scientific World Journal, 2015, 127853. doi: 10.1155/2015/127853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJL, … Whiteford HA (2013). Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study 2010. PLoS Medicine, 10(11), e1001547. doi: 10.1371/journal.pmed.1001547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaziuddin M, Ghaziuddin N, & Greden J (2002). Depression in Persons with Autism: Implications for Research and Clinical Care. Journal of Autism and Developmental Disorders, 32(4), 299–306. doi: 10.1023/a:1016330802348 [DOI] [PubMed] [Google Scholar]
- Ghaziuddin M, & Zafar S (2008). Psychiatric comorbidity of adults with autism spectrum disorders. Clinical Neuropsychiatry, 5(1), 9–12. [Google Scholar]
- Gillberg IC, Helles A, Billstedt E, & Gillberg C (2016). Boys with Asperger Syndrome Grow Up: Psychiatric and Neurodevelopmental Disorders 20 Years After Initial Diagnosis. Journal of Autism and Developmental Disorders, 46(1), 74–82. doi: 10.1007/s10803-015-2544-0 [DOI] [PubMed] [Google Scholar]
- Godard J, Baruch P, Grondin S, & Lafleur MFJPR (2012). Psychosocial and neurocognitive functioning in unipolar and bipolar depression: a 12-month prospective study. 196(1), 145–153. [DOI] [PubMed] [Google Scholar]
- Gotham K, Bishop SL, Brunwasser S, & Lord C (2014). Rumination and perceived impairment associated with depressive symptoms in a verbal adolescent-adult ASD sample. Autism Research, 7(3), 381–391. doi: 10.1002/aur.1377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Brunwasser SM, & Lord C (2015). Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. Journal of the American Academy of Child and Adolescent Psychiatry, 54(5), 369–376. e363. doi: 10.1016/j.jaac.2015.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Unruh K, & Lord C (2015). Depression and its measurement in verbal adolescents and adults with autism spectrum disorder. Autism, 19(4), 491–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedley D, & Uljarević M (2018). Systematic Review of Suicide in Autism Spectrum Disorder: Current Trends and Implications. Current Developmental Disorders Reports, 5(1), 65–76. doi: 10.1007/s40474-018-0133-6 [DOI] [Google Scholar]
- Hergueta T, Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IVand ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20), 2233. [PubMed] [Google Scholar]
- Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, … Gillberg C (2009). Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry, 9(1), 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollocks MJ, Lerh JW, Magiati I, Meiser-Stedman R, & Brugha TS (2019). Anxiety and depression in adults with autism spectrum disorder: a systematic review and meta-analysis. Psychological medicine, 49(4), 559–572. [DOI] [PubMed] [Google Scholar]
- Hudson CC, Hall L, & Harkness KL (2018). Prevalence of Depressive Disorders in Individuals with Autism Spectrum Disorder: a Meta-Analysis. Journal of Abnormal Child Psychology. doi: 10.1007/s10802-018-0402-1 [DOI] [PubMed] [Google Scholar]
- Hurtig T, Kuusikko S, Mattila ML, Haapsamo H, Ebeling H, Jussila K, … & Moilanen I (2009). Multi-informant reports of psychiatric symptoms among high-functioning adolescents with Asperger syndrome or autism. Autism, 13(6), 583–598. [DOI] [PubMed] [Google Scholar]
- Hus V, & Lord C (2014). The autism diagnostic observation schedule, module 4: revised algorithm and standardized severity scores. Journal of Autism and Developmental Disorders, 44(8), 1996–2012. doi: 10.1007/s10803-014-2080-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, … Biederman J (2013). Psychiatric Comorbidity and Functioning in a Clinically Referred Population of Adults with Autism Spectrum Disorders: A Comparative Study. Journal of Autism and Developmental Disorders, 43(6), 1314–1325. doi: 10.1007/s10803-012-1679-5 [DOI] [PubMed] [Google Scholar]
- Kanne SM, Abbacchi AM, & Constantino JN (2009). Multi-informant ratings of psychiatric symptom severity in children with autism spectrum disorders: The importance of environmental context. Journal of autism and developmental disorders, 39(6), 856–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy N, Foy K, Sherazi R, McDonough M, & McKeon P (2007). Long‐term social functioning after depression treated by psychiatrists: a review. Bipolar Disorders, 9(1‐2), 25–37. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kraper CK, Kenworthy L, Popal H, Martin A, & Wallace GL (2017). The Gap Between Adaptive Behavior and Intelligence in Autism Persists into Young Adulthood and is Linked to Psychiatric Co-morbidities. Journal of Autism and Developmental Disorders, 47(10), 3007–3017. doi: 10.1007/s10803-017-3213-2 [DOI] [PubMed] [Google Scholar]
- Kuehner C (2017). “Why is depression more common among women than among men?” 4(2): 146–158. [DOI] [PubMed] [Google Scholar]
- Kuehner C (2003). Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatrica Scandinavica, 108(3), 163–174. [DOI] [PubMed] [Google Scholar]
- Lemler M (2012). Discrepancy between parent report and clinician observation of symptoms in children with autism spectrum disorders. Discussions, 8(2). [Google Scholar]
- Lerner MD, Calhoun CD, Mikami AY, & De Los Reyes A (2012). Understanding parent–child social informant discrepancy in youth with high functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(12), 2680–2692. [DOI] [PubMed] [Google Scholar]
- Lever AG, & Geurts HM (2016). Psychiatric Co-occurring Symptoms and Disorders in Young, Middle-Aged, and Older Adults with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 46(6), 1916–1930. doi: 10.1007/s10803-016-2722-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, & Bishop S (2012). Autism diagnostic observation schedule–2nd edition (ADOS-2). Los Angeles, CA: Western Psychological Corporation. [Google Scholar]
- Lugnegård T, Hallerbäck MU, & Gillberg C (2011). Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Research in Developmental Disabilities, 32(5), 1910–1917. doi: 10.1016/j.ridd.2011.03.025 [DOI] [PubMed] [Google Scholar]
- Marangell LB, Dennehy EB, Miyahara S, Wisniewski SR, Bauer MS, Rapaport MH, & Allen MH (2009). The functional impact of subsyndromal depressive symptoms in bipolar disorder: data from STEP-BD. Journal of affective disorders, 114(1–3), 58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Murray MJ, & Zahid J (2011). Variables Associated with Anxiety and Depression in Children with Autism. Journal of Developmental and Physical Disabilities, 23(4), 325–337. doi: 10.1007/s10882-011-9231-7 [DOI] [Google Scholar]
- Mazurek MO, & Kanne SM (2010). Friendship and internalizing symptoms among children and adolescents with ASD. Journal of Autism and Developmental Disorders, 40(12), 1512–1520. doi: 10.1007/s10803-010-1014-y [DOI] [PubMed] [Google Scholar]
- Moseley DS, Tonge BJ, Brereton AV, & Einfeld SL (2011). Psychiatric comorbidity in adolescents and young adults with autism. Journal of Mental Health Research in Intellectual Disabilities, 4(4), 229–243. [Google Scholar]
- Rai D, Heuvelman H, Dalman C, Culpin I, Lundberg M, Carpenter P, & Magnusson C (2018). Association Between Autism Spectrum Disorders With or Without Intellectual Disability and Depression in Young Adulthood. JAMA network open, 1(4), e181465–e181465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai D, Culpin I, Heuvelman H, Magnusson CM, Carpenter P, Jones HJ, … & Pearson RM (2018). Association of autistic traits with depression from childhood to age 18 years. JAMA psychiatry, 75(8), 835–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M, Prox-Vagedes V, Ohlmeier MD, & Dillo W (2015). Beyond childhood: psychiatric comorbidities and social background of adults with Asperger syndrome. Psychiatr Danub, 27(1), 50–59. [PubMed] [Google Scholar]
- Sterling L, Dawson G, Estes A, & Greenson J (2008). Characteristics Associated with Presence of Depressive Symptoms in Adults with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 38(6), 1011–1018. doi: 10.1007/s10803-007-0477-y [DOI] [PubMed] [Google Scholar]
- Stewart ME, Barnard L, Pearson J, Hasan R, & O’Brien G (2006). Presentation of depression in autism and Asperger syndrome: A review. Autism, 10(1), 103–116. [DOI] [PubMed] [Google Scholar]
- Strang JF, Kenworthy L, Daniolos P, Case L, Wills MC, Martin A, & Wallace GL (2012). Depression and anxiety symptoms in children and adolescents with autism spectrum disorders without intellectual disability. Research in Autism Spectrum Disorders, 6(1), 406–412. doi: 10.1016/j.rasd.2011.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickerstaff S, Heriot S, Wong M, Lopes A, & Dossetor D (2007). Intellectual Ability, Self-perceived Social Competence, and Depressive Symptomatology in Children with High-functioning Autistic Spectrum Disorders. Journal of Autism and Developmental Disorders, 37(9), 1647–1664. doi: 10.1007/s10803-006-0292-x [DOI] [PubMed] [Google Scholar]
- Ward SL, Sullivan KA, & Gilmore L (2018). Combining parent and clinician ratings of behavioural indicators of autism spectrum disorder improves diagnostic classification. Early Child Development and Care, 188(6), 748–758. [Google Scholar]
- Wechsler D (2011). Wechsler Abbreviated Scale of Intelligence–Second Edition (WASI-II). San Antonio, TX: NCS Pearson. [Google Scholar]
- Wigham S, Barton S, Parr JR, & Rodgers J (2017). A systematic review of the rates of depression in children and adults with high-functioning autism spectrum disorder. Journal of Mental Health Research in Intellectual Disabilities, 10(4), 267–287. [Google Scholar]
- Wing L (1981). Asperger’s syndrome: a clinical account. Psychological Medicine, 11(1), 115–129. [DOI] [PubMed] [Google Scholar]
- Wing L (1996). Autistic spectrum disorders. BMJ, 312(7027), 327–328. doi: 10.1136/bmj.312.7027.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2017). Depression and other common mental disorders: global health estimates.
- Zahid S, & Upthegrove R (2017). Suicidality in autistic spectrum disorders: A systematic review. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 38(4), 237. [DOI] [PubMed] [Google Scholar]


