Abstract
Asthma evidence-based interventions (EBI) are implemented in the home, school, community or primary care setting. Although families are engaged in one setting, they often have to navigate challenges in another setting. Our objective is to design and implement a comprehensive plan which integrates EBI’s and connects the four sectors in underserved communities such as Philadelphia. September 2015-April 2016 we implemented a three-pronged strategy to understand needs and resources of the community including 1) focus groups and key informant interviews, 2) secondary data analysis and 3) pilot testing for implementation to determine gaps in care, and opportunities to overcome those gaps. Analysis of the focus group and key informant responses showed themes: diagnosis fear, clinician time, home and school asthma trigger exposures, school personnel training and communication gaps across all four sectors. EBI’s were evaluated and selected to address identified themes. Pilot testing of a community health worker (CHW) intervention to connect home, primary care and school resulted in an efficient transfer of asthma medications and medication administration forms to the school nurse office for students with uncontrolled asthma addressing a common delay leading to poor asthma management in school. Thus far there has been limited success in reducing asthma disparities for low-income minority children. This study offers hope that strategically positioning CHWs may work synergistically to close gaps in care and result in improved asthma control and reduced asthma disparities.
Keywords: asthma, community health workers, integration, pediatrics, implementation science
INTRODUCTION
Asthma is the most common physical health condition in school-age children with prominent racial disparities in prevalence, morbidity, and death (1, 2). It is also the leading cause of school absenteeism (3). Asthma-related school absences are more common among lower-income families and black and Hispanic children (4). The high asthma burden experienced by poor minority children is attributed to multiple ecological factors, the relationship of multiple environments that affect children, where they live, learn, and play (5–6). Fragmented attention to these ecological factors across settings results in inconsistent asthma management and fosters persistent disparities in asthma outcomes (7).
While poor access to high quality health care is one well-described driver of health disparities, factors that pervade a school-aged child’s home and school, two places where they spend the majority of their time, are both equally critical to identify and address. These include substandard home and school built environments (8–10). Poor housing conditions including overcrowding, economic isolation (11) and the high cost of home maintenance contribute to the exposure of children to common triggers such as cockroaches, dust, pets, mice, and mold (12, 13). Local public schools are often older buildings riddled with allergens and under-resourced to provide optimal support for students with asthma (14). Yet school interventions which include asthma self-management have been found to reduce asthma healthcare utilization and number of restricted activity days (15). Further, environmental interventions in schools have been demonstrated to reduce exposures to known allergens (16).
The potential synergistic strength of integrating interventions across multiple sectors has not been fully leveraged despite knowledge that multi-pronged interventions are most effective (17). Currently evidence-based interventions (EBI) for asthma are implemented in the home, school, or primary care setting, but not in a coordinated child-centered manner. Even when caregivers are engaged in asthma interventions in one setting, they must often navigate challenges in other settings, i.e. an under-resourced home, non-supportive school, or disengaged healthcare provider. In one study, a comprehensive school nurse management program to promote care coordination and better asthma management was unsuccessful due to additional responsibilities for the school nurse in the absence of creating buy-in from the primary care practice (18). Thus, asthma interventions tailored to families’ characteristics, social environments, and health beliefs and also connected across sectors may reduce the burden of caring for children with asthma.
We describe the three-phase process used to identify asthma-related risks, resources, and barriers with the overarching goal to create a comprehensive plan to implement evidence-based asthma interventions that span multiple sectors through utilization of Community Health Workers (CHWs).
METHODS
For the past twenty years, the Community Asthma Prevention Program (CAPP) has utilized a community participation research strategy to implement eleven asthma community-based interventions. Building upon this success, CAPP assembled the West Philadelphia Asthma Care Collaborative (WePACC) including partners from all four sectors of a child’s life, caregivers, school professionals, community organizations and healthcare professionals, to guide the development of a multi-sector asthma program.
Setting
We chose West Philadelphia due to high asthma prevalence of 25% (compared to 9% nationally) (19), and poverty status. West Philadelphia, according to US Census 2015, has approximately residents, including roughly 49,000 children 0-17 years. Seventy-four percent of residents identify as Black/African American. Thirty-two percent of children live below the federal poverty level, 98% of children have health insurance, and 100% of parents report their child receives regular health care. Children’s Hospital of Philadelphia (CHOP) is the primary source of emergency and hospital care for West Philadelphia providing primary care for over 40,000 children.
Our approach included three successive phases: Phase 1: map West Philadelphia asthma risks and resources; Phase 2: conduct a needs assessment with community stakeholders; and Phase 3: use the information gained to develop and conduct a pilot intervention utilizing CHWs and targeting school-age children with asthma.
Phase 1: Mapping Risks and Resources
The goal of this phase was to better understand asthma morbidity in West Philadelphia and the resources available to children and families suffering from asthma. Information was used to identify neighborhoods with high asthma morbidity and available neighborhood resources to determine the scope and ideal location of a comprehensive intervention.
We mapped asthma morbidity by extracting census tract-level asthma-specific emergency department (ED) visits for children ages 0-17 with a home address in a West Philadelphia census tract from the CHOP Data Warehouse between 2014 and 2015. ED visits were considered asthma-specific with an ICD-9 or ICD-10 diagnosis code for asthma and a medical order for an inhaled beta agonist or systemic corticosteroid.
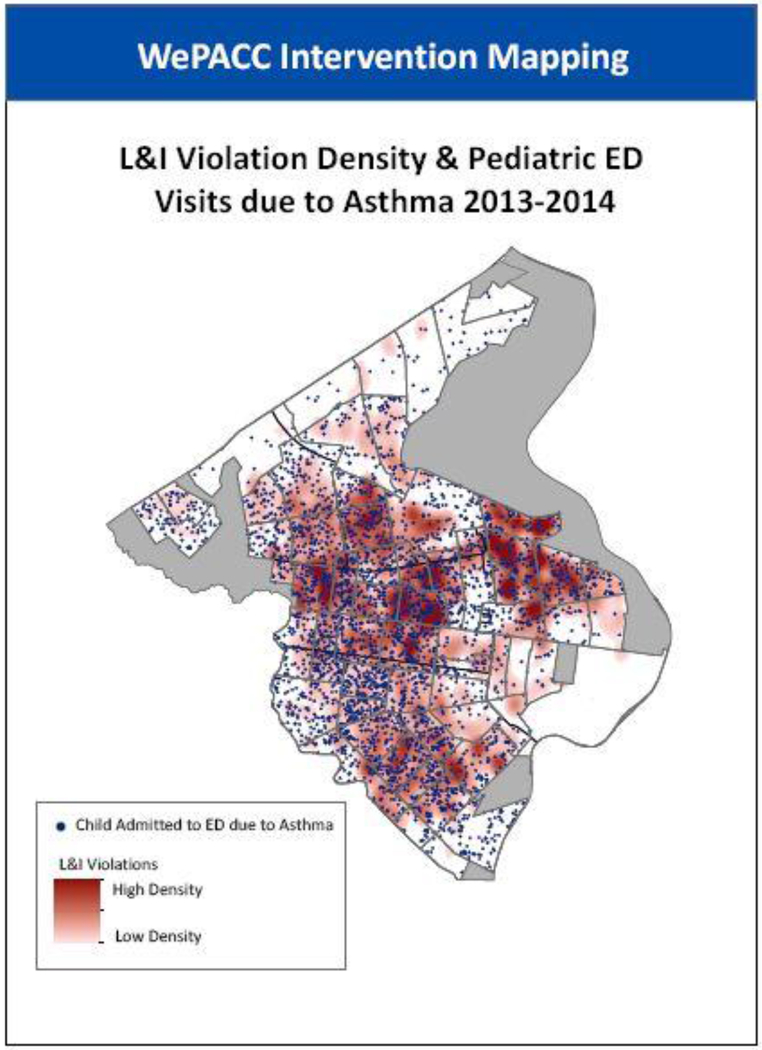
Data from Philadelphia’s Department of Licenses and Inspections (L&I) on housing code violations in 2013 and 2014 were then obtained from License to Inspect (http://lti.planphilly.com/), a web-based application that includes a searchable database of code violations. All violation types were included. Over 30,000 violations reported between 2013 and 2014 were identified; entries without an address or date were excluded.
ArcGIS mapping software was used to map the density of L&I violations across the WePACC zone. This density layer was reclassified as a binary variable, indicating either high- or low- L&I violation density. The binary high/low L&I violation layer was then overlaid on a map of asthma-specific ED visits to CHOP.
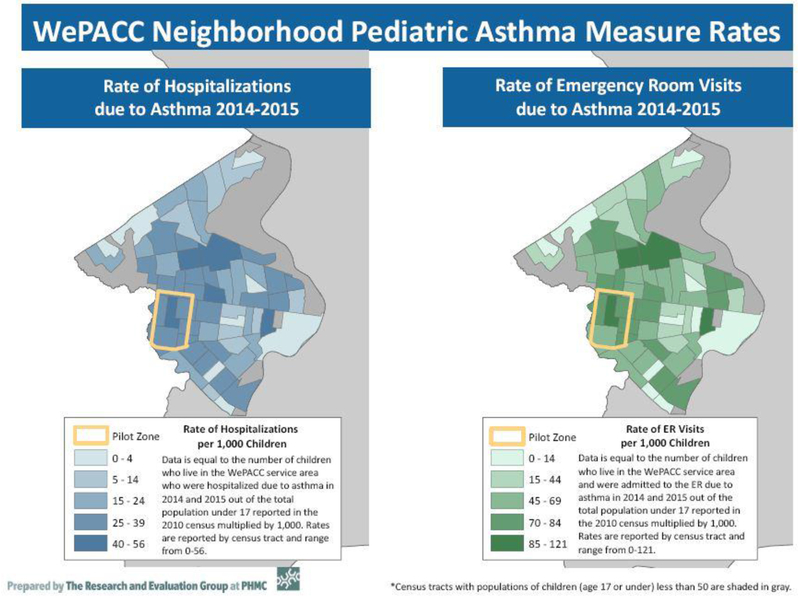
To protect patient privacy, ED data were reported in aggregate at the Census tract level (rather than street address level). Accordingly, Census tracts were classified as high- or low- density based on the number of Licensing and Inspection (L& I) violations with each ED visit represented within the census tract (Figure 1). We simultaneously mapped the rate of hospitalizations/1000 children with ED and hospitalizations for asthma revealing an overlap in healthcare utilization in the areas of high density of L& I violations (figure 2). We then mapped community resources, such as pharmacies, after school programs, day-care providers, faith-based sites, and recreation programs using ArcGIS software. We also mapped school-oriented data points (highest asthma prevalence, number of students and location) provided by the School District of Philadelphia.
Figure 1.
Licensing and Inspection violations mapped with emergency room admissions for asthma.
Figure 2.
Asthma-related Hospitalizations and Emergency Room Visits per 1000 children reported by census tract.
Phase 2: Needs Assessment
To assess the needs of children with asthma and opportunities for improved asthma care, we conducted focus groups and key informant interviews. Questionnaires were developed in an iterative process by the research team and then vetted by a community advisory group for final approval.
Participants
Parents of school-aged children with asthma were recruited from West Philadelphia primary care centers, schools, and community agencies via flyers and word of mouth. One parent focus group was held at a primary care center and two were held at schools identified by WePACC members. Children (ages 6-14 years) recruited directly by school nurses attended a focus group at school. West Philadelphia school nurses participated in a focus group during a professional development day. Questions included perspective about school asthma care, gaps in management and opportunities to close gaps in care.
Seven key informant interviews were held between May 2016 and July 2016. The participants were parents, school nurse coordinator, healthcare provider and Medicaid medical director selected via purposive sampling to obtain in-depth insights of the gaps in care and sustainability strategies in order to inform study design.
Data Collection
All participants were queried about 1) their experience with managing asthma in their setting; 2) availability of community asthma management resources; 3) challenges and barriers relating to asthma care in the four sectors; and 4) need for new asthma programs serving children in West Philadelphia 5) previous interaction with community health workers.
Key informant, semi-structured interviews were conducted in person or by phone. Although specific probes and question structures were adjusted to fit the expertise and knowledge base of each type of participant, the main interview prompts remained the same for each focus group and interview. Participants with relevant expertise were also asked to provide feedback on intervention strategies being considered.
All focus groups and key informant interviews were recorded, transcribed, and coded by trained research staff. Descriptive coding was used to identify key themes based on issues explored in the focus groups around strengths and challenges in multiple settings (e.g. clinic, school, home). Thematic analysis was conducted using NVivo software.
Phase 3 – Develop and Conduct a Pilot Intervention
The Yes We Can™ Children’s Asthma Program, a medical-social model in place at three primary care practices at CHOP, utilizes CHWs in the clinic and home. We partnered with the School District of Philadelphia to pilot a school asthma intervention using CHWs that would address needs identified in Phase 2. We identified all public schools in West Philadelphia and used the risk and resource maps to identify a pilot school. Once identified, project staff worked with school leadership to pilot a school asthma intervention and assess the feasibility of using CHWs to bridge school nursing care with primary care practice.
RESULTS
Phase 1 – Risks and Resources
Risk of emergency care utilization and housing code violations
1,353 children residing in West Philadelphia were hospitalized for asthma, and 3,186 children had an ED visit for asthma at CHOP in 2014 and 2015. Figure 1 demonstrates the overlap of housing code violation density with ED use for asthma. Grossly similar patterns of utilization by census tract were observed for hospitalization and ED visits (Figure 2). Areas around the targeted primary care centers have higher rates of substandard housing and healthcare utilization. This supports an intervention recruiting from these offices.
Resources
We mapped hospital, pharmacies, and day care providers with after school programs and faith-based organizations in the targeted community. This map was used to identify which communities had substantial resource gaps and information was available to all stakeholders during the planning phase (Figure 2). From risks and resource information we identified an area for the pilot school intervention in phase 3 (outlined in yellow in Figure 1).
Phase 2 – Qualitative Assessment: Themes in Focus Groups and Key Informant interviews
Five focus groups (table 1) were convened between November 2015 and April 2016. Three groups consisted of parents of children with asthma (n=24), one group of children with asthma (n=7), and one group of school nurses (n= 7). Seven key informant interviews were conducted between May 2016 and July 2016. Table 3 summarizes findings, illustrative quotes and evidence-based intervention components that will be utilized to address concerns.
Table 1.
Qualitative Data and Proposed Interventions
| Participants | Common Themes | Planned Evidence Based Interventions |
|---|---|---|
| Parents (n= 24) | 1. Environmental Concerns - asthma triggers at home and school 2. Family Dynamics – children in multiple homes 3. Life Stressors, i.e. lack of employment, chronic homelessness, substance abuse 4. Understanding of asthma medications and devices 5. School Concerns – school staff knowledgeable in how to manage asthma 6. Health Care Concerns – No time for education at clinic visits, missed appointments, crowded offices 7. Fear of asthma diagnosis in children |
Yes We Can™ Children’s Asthma Program (CHW in Clinic and Home Settings) ➢ Asthma education in clinic and home (Themes 1, 4, 6, 7, 15) ➢ CHW attends clinic visits to facilitate enhanced communication between provider and caregiver, and relaying to provider any caregiver concerns, needs or fears (Themes 4, 8, 7, 15, 16, 18) ➢ Needs assessment to assist patents with identifying care coordination goals with links to resources to address stressors and barriers (Themes 2, 3, 17) ➢ Home asthma trigger evaluation with education and supplies for trigger reduction (Theme 1) ➢ Education on STAR (Stop-Think-Ask-Respond) technique to talk to children about feelings regarding asthma (Themes 8, 10) ➢ Motivate and reward children for taking medication as prescribed (Theme 8) ➢ Education on asthma care plan and asthma medications (Theme 8, 19) Open Airways for Schools® Plus (CHW in School Setting) ➢ Asthma education session scheduled for school faculty and staff in best practices for asthma managements schools (Themes 5, 12, 14) ➢ CHW conducts American Lung Association’s Open Airways for Schools (OAS) educational sessions for students with asthma (Themes 7, 8, 9, 10) ➢ Classroom asthma trigger evaluation with education and supplies for trigger reduction given to classroom teachers (Theme 1) School-Based Asthma Therapy (SBAT) (CHW Clinic and Home coordinates with CHW in School) ➢ Coordinated communication between primary care provider, school nurse and caregivers to efficiently attain medication administration forms and asthma medications at school (Themes 2, 3, 11) ➢ Students receive one dose of asthma control medication daily in school nurse office (Theme 2, 3) ➢ Health Insurance Provider establishes policy for two asthma control medications and two devices to be dispensed for use at home and school (Theme 13) |
| Children Ages 8 – 13 (n =7) | 8. Belief that they take too many asthma medications and that administration is too frequent 9. Concern that allergies often trigger asthma symptoms 10. Feeling that asthma limits activities and sadness about having asthma and their limitations |
|
| School Health Services (n=8) | 11. Difficulty obtaining completed health forms 12. Feeling that school nurses are the only staff who can care for students with asthma 13. Caregivers not having enough medication for both home and school 14. Need for asthma education tor school staff |
|
| Primary Care Providers (n=2) | 15. Parental lack of knowledge about asthma management (e.g., belief that children can outgrow asthma) 16. Poor communication with caregivers 17. Challenges with health insurance 18. Limited time at visits |
|
| Health Insurance Provider (n=1) | 19. Parental lack of knowledge about proper use of asthma medications |
Parent Focus Group
Twenty-four parents living in West Philadelphia participated in focus groups. Parents had one to three children with asthma with ages ranging from 3 years to 20 years old. Age of diagnosis ranged from “birth” to 10 years old. Children attended public and charter schools in the targeted community. Sixty-one percent of children used asthma medication at school with 57% receiving it from the school nurse. Children’s asthma varied in severity.
Parent focus groups revealed that parents are most concerned about asthma management in schools.
Parents identified specific strengths of their healthcare system, including a 24 hour nurse triage system; common practice of notifying the ED if a child is sent directly from a primary care center; a dedicated asthma team in the hospital; a system of clinic-based CHWs; community asthma classes; communication around follow-up visits; nurses; and comprehensive educational paperwork for parents. Parents identified needs and concerns across all sectors, with home and school concerns mentioned most frequently. Home concerns included landlord unresponsiveness, difficulty with controlling triggers such as second-hand smoke exposure and mold, parental mental health issues, children living in multiple homes, and difficulty using medication.
School system concerns were numerous. Parents reported inconsistent care because of school nurse presence or absence, lack of communication, teacher’s lack of knowledge about asthma and the school building environment. Parents felt that funding is an issue making it difficult for schools to address asthma triggers. Parents reported that they often had to send their child to school sick to avoid excessive truancy, but in doing so worried that the school had insufficient personnel to treat ongoing symptoms. This not only resulted in stress for parents but missed workdays.
I send him [to school] but sometimes I park right outside and don’t even leave because he’s going to have an issue (with his asthma). So I get him marked in and he can stay until 10, 11 but then there’s repercussions for that too because then you’re a negligent parent if you keep your child home to manage their asthma, they’ve missed too much school. If you send them to school, you’re in fear for their lives, so like what are you supposed to do? How do you work? - Parent
School Nurse Focus Group
School nurse concerns included a lack of full time nurses (which has since improved in the School District of Philadelphia), lack of asthma education, poor communication with both parents and physicians, indoor asthma triggers in school, missed school days due to asthma, and incomplete medication administration forms. They expressed concerns about attention to the child’s health care by caregivers, citing a lack of understanding about asthma, poor communication between parent and provider, missed appointments, medication use and difficulty controlling child’s asthma.
I don’t want a student to die on my watch but on the same token there, it’s a double edged sword, you know, you give the inhaler without the [school medication administration form], then you’re never gettin’ a medication administration form. - School Nurse
Information gained from qualitative interviews is listed in Table 1 (Figure 3).
Phase 3: Developing and Piloting the School Intervention.
A predominant recurring theme in the focus groups was lack of robust communication between children’s primary care providers and schools and lack of appropriate asthma education and care within schools. To test the feasibility of implementing an intervention to address stakeholder concerns identified in Phase 2, we piloted a CHW-oriented intervention designed to improve care coordination between these two sectors composed of elements of a more comprehensive, evidence-based school intervention implemented in Detroit (20). Our rationale for utilizing CHWs as the effector arms was that CHWs were already an accepted and effective member of the primary care health team, therefore involving CHWs at the school level may improve communications between all sectors – home, clinic, school and community. The two largest primary care practices at CHOP which serve the highest prevalence and asthma morbidity areas in West Philadelphia each employ an asthma CHW who makes home visits but does not directly connect with schools to coordinate care for children with asthma.
Piloting the school intervention
An asthma-trained CHW enrolled nine of 10 families identified by the school nurse at the primary care office. One family did not enroll due to inability to contact a caregiver for consent. Once enrolled, the CHW approached the primary care provider (PCP) to gather all necessary forms, medications and devices. The CHW worked directly with the school nurse, principal, and classroom teacher to implement the pilot school intervention and enhance communication between caregiver, PCP and school. Despite initial challenges such as incomplete forms, poor communication between caregiver and nurse, and no medications at school, the CHW completed the intervention for all nine children within three weeks of enrollment. Subsequent key informant interviews with caregivers, school nurses and CHW were overall positive. Caregivers and school nurse appreciated the role of the CHW who coordinated with caregivers and the school nurse to ensure that the school obtained forms, medications, and devices needed to provide asthma care for the students. This positively confirmed the feasibility of utilizing CHWs as an optimal strategy for coordinating and improving asthma care for school-aged children and encouraged our selection of School-Based Asthma Therapy for the intervention.
Under the guidance of WEPACC, we utilized needs assessment results and the feasibility pilot to inform the final study design incorporating four evidence-based interventions: Yes We Can™ Children’s Asthma Program, Community Asthma Prevention Program (CAPP) CHW Home Visit Model, Open Airways for Schools® Plus, and School-Based Asthma Therapy (Table 1). Yes We Can was selected for the medical-social model, which integrates social determinants with optimal medical management utilizing CHWs. CAPP’s home visit model is fully integrated into the primary care practices and is founded on the Inner City Asthma Study protocol (8, 12, 13).
Open Airways for Schools® Plus combines the American Lung Association’s Open Airways for Schools® curriculum with other school-focused interventions including 1) yearly orientation to asthma and control strategies for principals and counselors, 2) briefings and walk-throughs for custodial personnel regarding potential environmental triggers, and 3) communication on behalf of families with a child’s clinician regarding program and requesting completion of the child’s asthma action plan. All of these are identified by School-based Asthma Management Program (SAMPRO) guidelines as effective interventions to decrease asthma symptom days and school absences (21–23). Lastly, School-Based Asthma Therapy, students taking asthma controller medicine in school, improves the likelihood of children receiving their controller medication, which is the gold standard of asthma management for uncontrolled asthma (24).
DISCUSSION
Our goal was to collaborate with stakeholders to conduct a needs assessment and design a coordinated multi-sector intervention to implement in a larger study to measure effectiveness. Through our West Philadelphia Asthma Care Collaborative (WePACC) we were able to accomplish this by conducting a community needs assessment utilizing existing clinical and community databases and qualitative interviews of caregivers and other important stakeholders.
Through this three-step process, we identified stakeholders’ concerns and barriers to asthma control in settings occupied by school-aged children, developed an intervention, and formulated a design to test this intervention at scale. Caregivers expressed concerns about school asthma management and the school environment, yet were generally positive about their healthcare system experience. School nurses expressed feeling limited by lack of information from parents and providers in management of asthma. Although caregivers generally had positive relationships with providers, PCP’s identified caregiver lack of knowledge and connection to schools as barriers. The pilot intervention demonstrated that CHWs could successfully bridge the gap between school and primary care for asthma.
Focus groups and interviews did not identify healthcare access as a perceived problem for stakeholders and there was generally a positive attitude toward the healthcare system despite disparities in asthma-related utilization in certain census tracts. Overlaying census-tract level utilization data with city licensing and inspection violations indicated potential overlap with substandard housing conditions which was a concern for parents and a finding that has been quantified in other studies (25).
Through implementation of this comprehensive care model with child at the center of coordination and education, we plan to create an effective, sustainable intervention to eliminate asthma disparities among poor, minority children. Our strategy to address social determinants while coordinating care across multiple sectors is the utilization of CHWs. As community residents, CHWs understand the unique circumstances and attitudes of families in their community and can serve as the connectors between families and primary care (27). CHWs are most often employed to deliver home-based multi-component trigger reduction interventions creating “asthma-friendly” environments (17). In the school setting, CHWs teach asthma classes resulting in improved asthma knowledge and self-management skills (34, 35). In the primary care setting, CHWs are recognized as an integral part of the health team (26). Further, CHWs can enhance the three principles of the medical home: whole person orientation, care coordination, and quality and safety by 1) ensuring that the caregiver’s voice is heard (28–30), 2) creating “teach-back” opportunities, 3) facilitating communication between all sectors and 4) helping caregivers make and reach goals for asthma management (31–33).
There are limitations in this study. Since this project was initiated and implemented by providers and investigators in the caregivers’ healthcare system, focus group attendees and key informants may have underreported concerns about the healthcare system. The focus groups and interviews, were conducted by a third-party contractor not affiliated with the healthcare system, minimizing the extent of possible underreporting. Additionally, we focused our efforts on understanding the needs and concerns in children’s homes, schools, and clinics. While community resources were included in the needs assessment and resource mapping, community resources such as after-school programs, recreation centers, and churches, were not explicitly included in the focus groups or key informant interviews.
In the final U01 study design we propose utilizing CHWs in the home, school and primary care sectors utilizing a factorial design. The clinical CHW will be responsible for implementing home visits and clinic visits. The school CHW will be responsible for coordination of school asthma management and School-Based Asthma Therapy and implementing the Open Airway for Schools curriculum. Building on previous research demonstrating effectiveness of CHWs in single domains, this study will examine the synergistic approach of utilizing CHWs in the home, school and clinical setting simultaneously to improve asthma control for children in West Philadelphia. Supporting this study with a cost-analysis will inform managed care organizations about the sustainability of this integrative approach.
Conclusion/key findings:
Thus far there has been limited success in reducing asthma disparities for low-income minority children. This study offers hope that strategically positioning CHWs may work synergistically to close gaps in care and result in improved asthma control and reduced asthma disparities.
Acknowledgements:
The authors acknowledge all of the members of the West Philadelphia Asthma Care Collaborative for their efforts in creating an intervention to meet the needs of children with asthma who live in West Philadlephia.
Footnotes
Declaration of Interest: The authors report no conflicts of interests. The authors alone are responsible for the content and writing of the paper
REFERENCE LIST
- 1.Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akinbmai LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001-2010. JACI. 2014;134(3):547–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akinbami LJ. The state of childhood asthma, United States, 1980-2005. Adv Data 2006;(381):1–24. [PubMed] [Google Scholar]
- 4.Hsu J, Qin X, Beavers SF, Mirabelli MC. Asthma-related school absenteeism, morbidity, and modifiable factors. Am J Prev Med. 2016; 51(1): 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coordinated Federal Action Plan to Reduce Racial and Ethnic Asthma Disparities. http://www.epa.gov/childrenstaskforce/federal_asthma_disparities_action_plan.pdf Last accessed, November 5, 2012.
- 6.Daniel LC, Boergers J, Kopel SJ, Koinis-Mitchell D. Missed sleep and asthma morbidity in urban children. Ann Allergy Asthma Immunol. 2012. July;109(1):41–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koinis-Mitchell D, McQuaid EL, Kopel SJ, Esteban CA, Ortega AN, Seifer R, Garcia-Coll C, Klein R, Cespedes E, Canino G, Fritz GK. Cultural-related, contextual, and asthma-specific risks associated with asthma morbidity in urban children. J Clin Psychol Med Settings. 2010. March;17(1):38–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright RJ, Mitchell H, Visness CM, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94(4):625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright RJ. Health effects of socially toxic neighborhoods: the violence and urban asthma paradigm. Clin Chest Med. 2006;27(3):413–21. [DOI] [PubMed] [Google Scholar]
- 10.Apter AJ, Garcia LA, Boyd RC, Wang X, Bogen DK, Ten Have T. Exposure to community violence is associated with asthma hospitalizations and emergency department visits. J Allergy Clin Immunol. 2010;126(3):552–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Population Reference Bureau. The Social and Economic Isolation of Urban African Americans. prb.orghttps://www.prb.org/thesocialandeconomicisolationofurbanafricanamericans Published October 1, 2005. Accessed June 28, 2018.
- 12.Gergen PJ, Mortimer KM, Eggleston PA, et al. Results of the National Cooperative Inner-City Asthma Study (NCICAS) environmental intervention to reduce cockroach allergen exposure in inner-city homes. J Allergy Clin Immunol. 1999;103(3 Pt 1):501–506. Accessed November 4, 2016. [DOI] [PubMed] [Google Scholar]
- 13.Rosenstreich DL, Eggleston P, Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336(19):1356–1363. [DOI] [PubMed] [Google Scholar]
- 14.Parsons Environment & Infrastructure Group Inc. School District of Philadelphia Facility Condition Assessment Summary Report. Philadelphia, PA: School District of Philadelphia; 2017. [Google Scholar]
- 15.Kneale D, Harris K, McDonald VM, Thomas J, Grigg J. Effectiveness of school-based self-management interventions for asthma among children and adolescents; findings from a Cochrane systematic review and meta-analysis. Thorax. 2019;0:1–7. [DOI] [PubMed] [Google Scholar]
- 16.Jhun I, Gaffin JM, Coull BA, Huffaker MF, Petty CR, Sheehan WJ, Baxi SN, Lai PS, Kang CM, Wolfson JM, et al. J Allergy Clin Immunol Pract. 2017;5(1): 154–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crocker DD, Kinyota S, Dumitru GG, et al. ; Task Force on Community Prevention Services. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011. ;41 (2 Suppl 1):S5–S32. [DOI] [PubMed] [Google Scholar]
- 18.Bruzzese JM, Evans D, Wiesemann S, et al. Using school staff to establish a preventive network of care to improve elementary school students’ control of asthma. J Sch Health. 2006;76(6):307–312. [DOI] [PubMed] [Google Scholar]
- 19.Bryant-Stephens T, West C, Dirl C,Banks T, Briggs V, Rosenthal M. Asthma Prevalence in Philadelphia: Description of Two community-based Methodologies to Assess Asthma Prevalence in an Inner-City Population. J of Asthma 49:6, 581–585 [DOI] [PubMed] [Google Scholar]
- 20.Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004; 125(5): 1674–9. [DOI] [PubMed] [Google Scholar]
- 21.Lemanske RF, Kakumanu S, Shanovich K, et al. Creation and implementation of SAMPRO™: A school-based asthma management program. J Allergy Clin Immunol. 2016; 138(3):711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coffman JM, Cabana MD, Yelin EH. Do school-based asthma education programs improve self-management and health outcomes? Pediatrics. 2009. August;124(2):729–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bruzzese JM, Evans D, Kattan M. School-based asthma programs. J Allergy Clin Immunol. 2009; 124:195–200. [DOI] [PubMed] [Google Scholar]
- 24.Halterman JS, Fagnano M, Tajon RS, et al. Effect of the school-based telemedicine enhanced asthma management (SB-TEAM) program on asthma morbidity: A randomized clinical trial. JAMA Pediatr. 2018;172(3):e174938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beck AF, Sandel MT, Ryan PH, et al. Mapping neighborhood health geomarkers to clinical care decisions to promote equity in child health. Health Aff (Millwood). 2017;36(6):999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campbell J, Brooks M, Hosokawa P, Robinson J, Song L, Kreiger J. Community health worker home visits for Medicaid-enrolled children with asthma: Effects on asthma outcomes and costs. Am J Public Health 2015;105(11).2366–2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allen CG, Escoffery C, Satsangi A, Brownstein IN. Strategies to improve the integration of community health workers into health care teams: “A Little Fish in a Big Pond.” Prev Chronic Dis. 2015;12:E154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bender BG. Overcoming barriers to nonadherence in asthma treatment. J Allergy Clin Immunol. 2002;109(6 Suppl):S554–S559. [DOI] [PubMed] [Google Scholar]
- 29.Blaiss MS, Kaliner MA, Baena-Cagnani CE, Dahl R, Valovirta EJ, Canonica GW. Barriers to asthma treatment in the United States: results from the global asthma physician and patient survey. World Allergy Organ J. 2009;2(12):303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boudreaux ED, Emond SD, Clark S, Camargo CA. Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status. Chest. 2003;124(3):803–812 [DOI] [PubMed] [Google Scholar]
- 31.Simon MA, Samaras AT, Nonzee NJ, et al. Patient navigators: agents of creating community-nested patient-centered medical homes for cancer care. Clin Med Insights Women’s Health. 2016;9:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Auger KA, Kahn RS, Davis MM, Beck AF, Simmons JM. Medical home quality and readmission risk for children hospitalized with asthma exacerbations. Pediatrics. 2013; 131(1):64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res. 2010;25(5):815–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kintner E, Cook G, Allen A, Meeder L, Bumpus J, Lewis K. Feasibility and benefits of a school-based academic and counseling program for older school-age students with asthma. Res Nurs Health. 2012;35(5):507–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horner SD, Fouladi RT. Improvement of rural children’s asthma self-management by lay health educators. J Sch Health. 2008;78(9):506–513. [DOI] [PMC free article] [PubMed] [Google Scholar]