Abstract
Technology is intended to assist with diagnosing, treating, and monitoring patients remotely. Little is known of its impact on health outcomes or how it is used for obesity management. This study reviewed the literature to identify the different types of technologies used for obesity management and their outcomes. A literature search strategy using PubMed, CINAHL, Scopus, Embase, and ABI/Inform was developed and then was vetted by two pairs of researchers. Twenty-three studies from 2010 to 2017 were identified as relevant. Mobile health, eHealth, and telehealth/telemedicine are among the most popular technologies used. Study outcome measurements include association between technology use and weight loss, changes in body mass index, dietary habits, physical activities, self-efficacy, and engagement. All studies reported positive findings between technology use and weight loss; 60 percent of the studies found statistically significant relationships. Knowledge gaps persist regarding opportunities for technology use in obesity management. Future research needs to include patient-level outcomes, cost-effectiveness, and user engagement to fully evaluate the feasibility of continued and expanded use of technology in obesity management.
Keywords: health information technology, mobile health, eHealth, telehealth/telemedicine, health outcomes, obesity management
Methods
Search Strategy
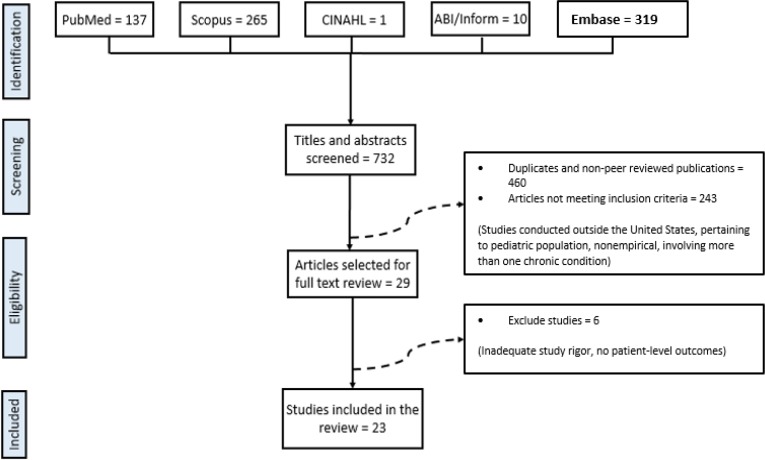
The literature search process was conducted based on the PRISMA model, a preferred guide for reporting items for systematic reviews and meta-analyses.9 A comprehensive search was conducted using five electronic databases (PubMed, Scopus, CINAHL, Embase, and ABI/Inform) to identify eligible studies related to the use of technology in the treatment and management of obesity published between 2010 to 2017. The search was conducted using medical subheading (MeSH) terms related to telemedicine and wearable technology, such as “telehealth,” “telemedicine,” “mHealth,” “eHealth,” and “mobile health,” in combination with terms such as “obesity” and “morbid obesity.”
Inclusion and Exclusion Criteria
The selected studies were included if they
were empirical studies published in English-language peer-reviewed journals from January 2010 to December 2017;
included adult participants (aged 18 years or older); and
used some form of digital technology, such as mobile phone, smartphone, or telehealth, in the management of obesity.
Studies were excluded if they
were conducted outside the United States;
examined specific patient populations, such as children, or adults with cognitive impairments; or
had a sample size smaller than 10.
Review Process
The initial searches yielded 732 articles across the selected databases. After duplicates and non-peer-reviewed articles were eliminated, 272 studies were reassessed to check for eligibility. Application of the inclusion and exclusion criteria to these 272 studies yielded 29 studies, which were independently reviewed by a pair of researchers to check for study design and content quality. Thus, studies were further eliminated from the review if they did not employ a rigorous study design, did not measure the impact of technology use in managing obesity, did not include patient-level outcomes, or contained more than one chronic condition. The review conducted by the original pair of researchers was reevaluated by a second pair of researchers to verify adherence to protocol and study selection. This process resulted in the 23 studies selected for inclusion in the review. A summary of the selection process is shown in Figure 1.
Figure 1.
Study Selection Flow Diagram
Results
All 23 studies were conducted in the United States. The study sample sizes ranged from 20 to nearly 2,500 participants. More than two-thirds of these studies (16 of 23 studies) used a randomized controlled design with a control group and one or more intervention groups, while the remaining 7 studies involved either observational, retrospective cohort, or pretest/posttest designs.
Technology Used
The most common type of technology used for the management of obesity was mobile devices, such as mobile phone applications and text messages (11 studies; 48 percent). Five studies (22 percent) used telehealth and telemedicine components, such as telephone counseling, videoconferencing, and interactive telemonitoring; six studies (26 percent) relied on eHealth in the form of websites and internet-based programs; and one study (4.3 percent) monitored weight loss using a wearable device. Table 1 outlines the different types of technologies used in the reviewed studies and our definitions of each type of technology.
Table 1.
Types of Technologies Used in the Management of Obesity
| Technology Type | Description | Studies Reviewed (N = 23) | Studies |
|---|---|---|---|
| Telehealth/telemedicine | Use of video and telephone-based technologies to provide health education, provide health coaching, and encourage behavior modification | 5 (21.7%) | Sherwood et al. 2010, Kim et al. 2010, Gerber et al. 2013, Ahrendt et al. 2014, Pronk et al. 2011 |
| Wearable technology | A wearable device that provides information and feedback on daily physical activity and energy expenditure and is typically used in conjunction with a web-based platform for easy recording of data | 1 (4.3%) | Archer et al. 2012 |
| eHealth | Use of internet- and website-based applications to provide an interactive platform for communication and education on diet, physical activity, and exercise | 6 (26.1%) | Bennett et al. 2012, Watson et al. 2012, Thomas et al. 2015, Gregoski et al. 2016, Johnston et al. 2012, Joseph et al. 2016 |
| Mobile health | Use of smartphones, cellphones, and other handheld mobile devices and applications used to track and monitor diet and physical activity; may also include the use of text messages and SMS to provide reminders or encourage certain behaviors | 11 (47.8%) | Burke et al. 2012, Shapiro et al. 2012, Allen et al. 2013, Bouhaidar et al. 2013, Spring et al. 2013, Steinberg et al. 2013, Thomas and Wing 2013, Turner-McGrievy et al. 2013, Svetkey et al. 2015, Kim et al. 2017, Stephens et al. 2017 |
Sources: Ahrendt, A. D., K. K. Kattelmann, T. S. Rector, and D. A. Maddox. “The Effectiveness of Telemedicine for Weight Management in the Move! Program.” Journal of Rural Health 30, no. 1 (2014): 113–19.
Allen, J. K., J. Stephens, C. R. Dennison Himmelfarb, K. J. Stewart, and S. Hauck. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment.” Journal of Obesity (2013): article 151597.
Archer, E., E. J. Groessl, X. Sui, A. C. McClain, S. Wilcox, G. A. Hand, R. A. Meriwether, and S. N. Blair. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.” American Journal of Preventive Medicine 43, no. 2 (2012): 176–82.
Bacigalupo, R., P. Cudd, C. Littlewood, P. Bissell, M. S. Hawley, and H. Buckley Woods. “Interventions Employing Mobile Technology for Overweight and Obesity: An Early Systematic Review of Randomized Controlled Trials.” Obesity Reviews 14, no. 4 (2013): 279–91.
Bennett, G. G., E. T. Warner, R. E. Glasgow, S. Askew, J. Goldman, D. P. Ritzwoller, K. M. Emmons, B. A. Rosner, and G. A. Colditz. “Obesity Treatment for Socioeconomically Disadvantaged Patients in Primary Care Practice.” Archives of Internal Medicine 172, no. 7 (2012): 565–74.
Bouhaidar, C. M., J. P. Deshazo, P. Puri, P. Gray, J. L. W. Robins, and J. Salyer. “Text Messaging as Adjunct to Community-based Weight Management Program.” CIN—Computers Informatics Nursing 31, no. 10 (2013): 469–76.
Burke, L. E., M. A. Styn, S. M. Sereika, M. B. Conroy, L. Ye, K. Glanz, M. A. Sevick, and L. J. Ewing. “Using mHealth Technology to Enhance Self-monitoring for Weight Loss: A Randomized Trial.” American Journal of Preventive Medicine 43, no. 1 (2012): 20–26.
Davis, F. D. “A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results.” Doctoral dissertation, Sloan School of Management, Massachusetts Institute of Technology, 1986.
Davis, F. D. “Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology.” MIS Quarterly 13, no. 3 (1989): 319–40.
Gerber, B. S., L. Schiffer, A. A. Brown, M. L. Berbaum, J. H. Rimmer, C. L. Braunschweig, and M. L. Fitzgibbon. “Video Telehealth for Weight Maintenance of African-American Women.” Journal of Telemedicine and Telecare 19, no. 5 (2013): 266–72.
Gregoski, M. J., J. Newton, C. G. Ling, K. Blaylock, S. A. O. Smith, J. Paguntalan, and F. A. Treiber. “Effective Weight-Loss Using an e-Health Delivered Physical Activity and Dietary Intervention: A Federal Credit Union Pilot Study.” Work 54, no. 1 (2016): 127–34.
Hartz, J., L. Yingling, and T. M. Powell-Wiley. “Use of Mobile Health Technology in the Prevention and Management of Diabetes Mellitus.” Current Cardiology Reports 18 (2016): 130.
Haugen, H. A., Z. V. Tran, H. R. Wyatt, M. J. Barry, and J. O. Hill. “Using Telehealth to Increase Participation in Weight Maintenance Programs.” Obesity 15, no. 12 (2007): 3067–77.
Johnston, J. D., A. P. Massey, and C. A. Devaneaux. “Innovation in Weight Loss Programs: A 3-Dimensional Virtual-World Approach. Journal of Medical Internet Research 14, no. 4 (2012): e120.
Joseph, R. P., D. Pekmezi, G. R. Dutton, A. L. Cherrington, Y. I. Kim, J. J. Allison, and N. H. Durant. “Results of a Culturally Adapted Internet-enhanced Physical Activity Pilot Intervention for Overweight and Obese Young Adult African American Women.” Journal of Transcultural Nursing 27, no. 2 (2016): 136–46.
Kim, H., M. Faw, and A. Michaelides. “Mobile but Connected: Harnessing the Power of Self-Efficacy and Group Support for Weight Loss Success through mHealth Intervention.” Journal of Health Communication 22, no. 5 (2017): 395–402.
Kim, Y., J. Pike, H. Adams, D. Cross, C. Doyle, and J. Foreyt. “Telephone Intervention Promoting Weight-related Health Behaviors.” Preventive Medicine 50, no. 3 (2010): 112–17.
Krishna, S. “Healthcare via Cell Phones: A Systematic Review.” Telemedicine Journal and E-health 15, no. 3 (2009): 231–40.
Liberati, A., D. G. Altman, J. Tetzlaff, C. Mulrow, P. C. Gøtzsche, J. P. Ioannidis, M. Clarke, P. J. Devereaux, J. Kleijnen, and D. Moher. “The PRISMA Statement for Reporting Systematic Reviews and Meta-analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration.” PLOS Medicine 6, no. 7 (2009): e1000100.
National Heart Lung and Blood Institute Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Heart Lung and Blood Institute, 1998.
Oh, H., C. Rizo, M. Enkin, and A. Jadad. “What Is eHealth (3): A Systematic Review of Published Definitions.” Journal of Medical Internet Research 7, no. 1 (2005): e1.
Pronk, N. P., A. L. Crain, J. J. Vanwormer, B. C. Martinson, J. L. Boucher, and D. L. Cosentino. “The Use of Telehealth Technology in Assessing the Accuracy of Self-reported Weight and the Impact of a Daily Immediate-Feedback Intervention among Obese Employees.” International Journal of Telemedicine and Applications (2011): article 909248.
Shapiro, J. R., T. Koro, N. Doran, S. Thompson, J. F. Sallis, K. Calfas, and K. Patrick. “Text4Diet: A Randomized Controlled Study Using Text Messaging for Weight Loss Behaviors.” Preventive Medicine 55, no. 5 (2012): 412–17.
Shaw, R. J., D. M. Steinberg, L. L. Zullig, H. B. Bosworth, C. M. Johnson, and L. L. Davis. “mHealth Interventions for Weight Loss: A Guide for Achieving Treatment Fidelity.” Journal of the American Medical Informatics Association 21, no. 6 (2014): 959–63.
Sherwood, N. E., R. W. Jeffery, E. M. Welsh, J. Vanwormer, and A. M. Hotop. “The Drop It at Last Study: Six-Month Results of a Phone-based Weight Loss Trial.” American Journal of Health Promotion 24, no. 6 (2010): 378–83.
Spring, B., J. M. Duncan, E. A. Janke, A. T. Kozak, H. G. McFadden, A. Demott, A. Pictor, L. H. Epstein, J. Siddique, C. A. Pellegrini, J. Buscemi, and D. Hedeker. “Integrating Technology into Standard Weight Loss Treatment: A Randomized Controlled Trial.” JAMA Internal Medicine 173, no. 2 (2013): 105–11.
Steinberg, D. M., E. L. Levine, S. Askew, P. Foley, and G. G. Bennett. “Daily Text Messaging for Weight Control among Racial and Ethnic Minority Women: Randomized Controlled Pilot Study.” Journal of Medical Internet Research 15, no. 11 (2013): e244.
Stephens, J. D., A. M. Yager, and J. Allen. “Smartphone Technology and Text Messaging for Weight Loss in Young Adults: A Randomized Controlled Trial.” Journal of Cardiovascular Nursing 32, no. 1 (2017): 39–46.
Svetkey, L. P., B. C. Batch, P. H. Lin, S. S. Intille, L. Corsino, C. C. Tyson, H. B. Bosworth, S. C. Grambow, C. Voils, C. Loria, J. A. Gallis, J. Schwager, and G. G. Bennett. “Cell Phone Intervention for You (CITY): A Randomized, Controlled Trial of Behavioral Weight Loss Intervention for Young Adults Using Mobile Technology.” Obesity (Silver Spring) 23, no. 11 (2015): 2133–41.
Thomas, G., T. M. Leahey, and R. R. Wing. “An Automated Internet Behavioral Weight-Loss Program by Physician Referral: A Randomized Controlled Trial.” Diabetes Care 38, no. 1 (2015): 9–15.
Thomas, J. G., and R. R. Wing. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study.” Journal of Medical Internet Research 1, no. 1 (2013): e3.
Turner-McGrievy, G. M., M. W. Beets, J. B. Moore, A. T. Kaczynski, D. J. Barr-Anderson, and D. F. Tate. “Comparison of Traditional versus Mobile App Self-monitoring of Physical Activity and Dietary Intake among Overweight Adults Participating in an mHealth Weight Loss Program.” Journal of the American Medical Informatics Association 20, no. 3 (2013): 513–18.
Watson, A., T. Bickmore, A. Cange, A. Kulshreshtha, and J. Kvedar. “An Internet-based Virtual Coach to Promote Physical Activity Adherence in Overweight Adults: Randomized Controlled Trial.” Journal of Medical Internet Research 14, no. 1 (2012): e1.
Outcomes
Weight loss was the primary outcome evaluated in 20 of the 23 studies (87 percent). This was measured either in the form of absolute change in body weight in pounds (lbs.) or kilograms (kgs.) or in the form of percent change in weight. Besides weight loss, changes in body mass index (BMI), physical activity, dietary intake habits, and time spent in sedentary positions were also assessed as primary outcomes. Because the management of obesity involves a lifestyle change, the studies also assessed secondary outcomes such as changes in self-efficacy, blood pressure, step count, and adherence to the prescribed technology during the study (see Table 2).
Table 2.
List of Reviewed Studies
| Technology Used | Author (Year) | Study Design | Sample Characteristics | Outcomes | Statistical Significanceb |
|---|---|---|---|---|---|
| 1. TELEHEALTH/TELEMEDICINE | |||||
| Telephone counseling | Kim et al. (2010) | RCT | • 2,470 participants randomized into self-help group (n = 1191) and self-help plus counseling group (n = 1,279) • 1,376 participants completed 6-month follow-up |
• Self-reported weight change • BMI • Servings of fruits and vegetables consumed each day • Minutes of physical activity per day |
No |
| Telephone-based weight loss program | Sherwood et al. (2010) | RCT pilot trial | • Sample drawn from university employees • 63 participants randomized into 3 groups (n = 21 each for self-directed, 10-session calls, 20-session calls) • 51 participants remaining at 6-month follow-up |
• Weight loss • Change in physical activity • Psychosocial changes • Self-monitoring behaviors |
No |
| Coaching calls, interactive telemonitoring | Pronk et al. (2011) | RCT | • 100 participants at baseline: 45 in intervention group and 55 in control group | • Weight loss • Discrepancy between self-reported and measured body weight |
Yes (only for weight loss) |
| Telephone counseling + home internet-enabled digital video recorders | Gerber et al. (2013) | RCT | • Sample restricted to African American women • 89 participants completed baseline interview • 88 completed weight-loss program |
• Weight loss • BMI • Change in: - Dieta - Physical activitya - Social supporta • Self-efficacy |
No |
| Videoconferencing | Ahrendt et al. (2014) | Retrospective cohort study | • Sample selected from VA healthcare system • 120 participants included in study: 60 in intervention and 60 in control |
• Weight loss • BMI |
Yes |
| 2. WEARABLE TECHNOLOGY | |||||
| SenseWear armband in combination with group weight-loss education | Archer et al. (2012) | RCT |
• 197 participants randomized into four groups • Standard care (n = 50) • Group weight loss (n = 49) • Armband (n = 49) • Group weight loss plus armband (n = 49) |
• Weight loss • Cost-effectiveness analysis |
Yes (significant weight loss seen in three intervention groups) |
| 3. eHealth | |||||
| Website interactive voice response system | Bennett et al. (2012) | RCT |
• Sample drawn from urban community health centers serving predominantly racial/ethnic minority patients • 365 patients randomized into intervention group (n = 180) and control group (n = 185) • 314 patients completed the study |
• Change in body weight • Change in blood pressurea |
Yes |
| Virtual world | Johnston et al. (2012) | Observational study | • 54 participants total; 33 in virtual-world intervention group and 21 in face-to-face group |
• Weight loss • Fruit and vegetable consumptiona • Moderate/vigorous physical activitya • Physical activity self-efficacya |
Yes |
| Internet-based virtual coach | Watson et al. (2012) | RCT |
• 70 participants randomized into intervention group (n = 35) and control group (n = 35) • 62 participants completed the study |
• Percent change in step count • Change in weighta • BMIa • Physical activity recalla • Self-efficacya • Program satisfaction |
No |
| Website | Thomas et al. (2015) | RCT | • 154 patients randomized into intervention group (n = 77) and control group |
• Weight loss after 3 months and 6 months • Calories |
Yes (all except fruit and vegetable consumption and |
| (n = 77) | consumeda • Decrease in fat intakea • Increase in fruit and vegetable consumptiona • Increase in exercise levelsa |
exercise levels) | |||
| Internet-based diet and exercise intervention | Gregoski et al. (2016) | Pilot pre-/posttest evaluation | • 56 participants | • Change in weight | No |
| Internet-based physical activity program | Joseph et al. (2016) | Single group pre-/posttest design | • Sample included only young adult African American women • Participants recruited from university campus • 33 participants allocated to intervention; data on 25 available for analysis |
• Physical activity • Sedentary screen time • Website utilization • Exercise session adherence • Change in BMIa |
No |
| 4. MOBILE HEALTH | |||||
| Personal digital assistant (PDA) | Burke et al. (2012) | RCT | • 210 participants randomized into control (n = 72), PDA (n = 68), and PDA + feedback (n = 70) groups | • Percentage weight change • Adherence to self-monitoring |
Yes (only for weight change in PDA + feedback group) |
| Text messaging | Shapiro et al. (2012) | RCT | • 170 participants randomized into intervention group (n = 81) and control group (n = 89) • 130 participants completed the study at 12 months |
• Weight loss • Adherence to treatment protocol • Daily step count • User satisfaction |
Yes |
| Use of a smartphone | Allen et al. (2013) | RCT pilot study | • 58 participants randomized into four groups • Intensive counseling (n = 18) • Intensive counseling + smartphone (n = 16) • Less-intensive counseling + smartphone (n = 17) |
• BMI • Waist Circumference • Dietary intake • Physical activity |
No |
| • Smartphone only (n = 17) | |||||
| SMS | Bouhaidar et al. (2013) | Pilot quasi-experimental pre-/posttest study | • 28 participants, with 14 each in control and intervention groups | • Change in body weight • Eating behaviors • Exercise and behavior self-efficacy • Attitude toward technology |
Yes |
| Personal digital assistant | Spring et al. (2013) | RCT | • 70 participants randomized into standard care (n = 35) and standard care + mobile groups (n = 35) | • Weight loss | Yes |
| Text messaging | Steinberg et al. (2013) | RCT | • Sample recruited from church-based wellness organization • Included only racial and ethnic minority women • 50 patients randomized into intervention group (n = 26) and control/education only group (n = 24) |
• Weight loss • Daily adherence to text messaging • Relationship between daily adherence to text messaging and weight loss |
No |
| Use of a smartphone | Thomas and Wing (2013) | Pilot study | • 20 participants | • Weight loss • Adherence to treatment protocol • Satisfaction with the intervention |
No |
| Mobile app | Turner-McGrievy et al. (2013) | RCT | • 96 participants randomized into behavioral weight loss intervention via an audio podcast (n = 49) and intervention + mobile diet monitoring (n = 47) | • Change in BMI • Intentional physical activity • Mean days/week of physical activity self-monitoring |
Yes |
| Use of a cellphone | Svetkey et al. (2015) | RCT | • Sample limited to 18–35 year olds • 365 participants randomized into control (n = 123), personal coaching intervention (n = 120), |
• Weight change at 6, 12, and 24 months • Percent change in weight at 6 and 12 monthsa • Weight change in |
Yes |
| and cell phone intervention (n = 122) groups • 313 participants completed the 24-month study |
subgroups defined by self-identified race, age, and sexa • Change in dietary patterna • Change in physical activitya |
||||
| Smartphone application | Kim et al. (2017) | Observational study | • 384 participants selected from mobile app (Noom) users | • Weight loss • Individual food logging • Social support |
Yes |
| Smartphone and text messaging | Stephens et al. (2017) | RCT | • Sample limited to 18–25 year olds recruited from Johns Hopkins University campuses • 62 participants randomized into control (n = 31) and smartphone + health coaching intervention (n = 31) groups |
• Change in weight • BMI • Waist circumference • Physical activity • Self-efficacy for healthy eating and exercise |
Yes |
BMI, body mass index; RCT, randomized controlled trial.
Secondary outcomes measured by study authors
Statistical significance reported only for association between use of technology and weight loss outcome.
Sources:
Ahrendt, A. D., K. K. Kattelmann, T. S. Rector, and D. A. Maddox. “The Effectiveness of Telemedicine for Weight Management in the Move! Program.” Journal of Rural Health 30, no. 1 (2014): 113–19.
Allen, J. K., J. Stephens, C. R. Dennison Himmelfarb, K. J. Stewart, and S. Hauck. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment.” Journal of Obesity (2013): article 151597.
Archer, E., E. J. Groessl, X. Sui, A. C. McClain, S. Wilcox, G. A. Hand, R. A. Meriwether, and S. N. Blair. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.” American Journal of Preventive Medicine 43, no. 2 (2012): 176–82.
Bennett, G. G., E. T. Warner, R. E. Glasgow, S. Askew, J. Goldman, D. P. Ritzwoller, K. M. Emmons, B. A. Rosner, and G. A. Colditz. “Obesity Treatment for Socioeconomically Disadvantaged Patients in Primary Care Practice.” Archives of Internal Medicine 172, no. 7 (2012): 565–74.
Bouhaidar, C. M., J. P. Deshazo, P. Puri, P. Gray, J. L. W. Robins, and J. Salyer. “Text Messaging as Adjunct to Community-based Weight Management Program.” CIN—Computers Informatics Nursing 31, no. 10 (2013): 469–76.
Burke, L. E., M. A. Styn, S. M. Sereika, M. B. Conroy, L. Ye, K. Glanz, M. A. Sevick, and L. J. Ewing. “Using mHealth Technology to Enhance Self-monitoring for Weight Loss: A Randomized Trial.” American Journal of Preventive Medicine 43, no. 1 (2012): 20–26.
Gerber, B. S., L. Schiffer, A. A. Brown, M. L. Berbaum, J. H. Rimmer, C. L. Braunschweig, and M. L. Fitzgibbon. “Video Telehealth for Weight Maintenance of African-American Women.” Journal of Telemedicine and Telecare 19, no. 5 (2013): 266–72.
Gregoski, M. J., J. Newton, C. G. Ling, K. Blaylock, S. A. O. Smith, J. Paguntalan, and F. A. Treiber. “Effective Weight-Loss Using an e-Health Delivered Physical Activity and Dietary Intervention: A Federal Credit Union Pilot Study.” Work 54, no. 1 (2016): 127–34.
Johnston, J. D., A. P. Massey, and C. A. Devaneaux. “Innovation in Weight Loss Programs: A 3-Dimensional Virtual-World Approach. Journal of Medical Internet Research 14, no. 4 (2012): e120.
Joseph, R. P., D. Pekmezi, G. R. Dutton, A. L. Cherrington, Y. I. Kim, J. J. Allison, and N. H. Durant. “Results of a Culturally Adapted Internet-enhanced Physical Activity Pilot Intervention for Overweight and Obese Young Adult African American Women.” Journal of Transcultural Nursing 27, no. 2 (2016): 136–46.
Kim, H., M. Faw, and A. Michaelides. “Mobile but Connected: Harnessing the Power of Self-Efficacy and Group Support for Weight Loss Success through mHealth Intervention.” Journal of Health Communication 22, no. 5 (2017): 395–402.
Kim, Y., J. Pike, H. Adams, D. Cross, C. Doyle, and J. Foreyt. “Telephone Intervention Promoting Weight-related Health Behaviors.” Preventive Medicine 50, no. 3 (2010): 112–17.
Pronk, N. P., A. L. Crain, J. J. Vanwormer, B. C. Martinson, J. L. Boucher, and D. L. Cosentino. “The Use of Telehealth Technology in Assessing the Accuracy of Self-reported Weight and the Impact of a Daily Immediate-Feedback Intervention among Obese Employees.” International Journal of Telemedicine and Applications (2011): article 909248.
Shapiro, J. R., T. Koro, N. Doran, S. Thompson, J. F. Sallis, K. Calfas, and K. Patrick. “Text4Diet: A Randomized Controlled Study Using Text Messaging for Weight Loss Behaviors.” Preventive Medicine 55, no. 5 (2012): 412–17.
Sherwood, N. E., R. W. Jeffery, E. M. Welsh, J. Vanwormer, and A. M. Hotop. “The Drop It at Last Study: Six-Month Results of a Phone-based Weight Loss Trial.” American Journal of Health Promotion 24, no. 6 (2010): 378–83.
Spring, B., J. M. Duncan, E. A. Janke, A. T. Kozak, H. G. McFadden, A. Demott, A. Pictor, L. H. Epstein, J. Siddique, C. A. Pellegrini, J. Buscemi, and D. Hedeker. “Integrating Technology into Standard Weight Loss Treatment: A Randomized Controlled Trial.” JAMA Internal Medicine 173, no. 2 (2013): 105–11.
Steinberg, D. M., E. L. Levine, S. Askew, P. Foley, and G. G. Bennett. “Daily Text Messaging for Weight Control among Racial and Ethnic Minority Women: Randomized Controlled Pilot Study.” Journal of Medical Internet Research 15, no. 11 (2013): e244.
Stephens, J. D., A. M. Yager, and J. Allen. “Smartphone Technology and Text Messaging for Weight Loss in Young Adults: A Randomized Controlled Trial.” Journal of Cardiovascular Nursing 32, no. 1 (2017): 39–46.
Svetkey, L. P., B. C. Batch, P. H. Lin, S. S. Intille, L. Corsino, C. C. Tyson, H. B. Bosworth, S. C. Grambow, C. Voils, C. Loria, J. A. Gallis, J. Schwager, and G. G. Bennett. “Cell Phone Intervention for You (CITY): A Randomized, Controlled Trial of Behavioral Weight Loss Intervention for Young Adults Using Mobile Technology.” Obesity (Silver Spring) 23, no. 11 (2015): 2133–41.
Thomas, G., T. M. Leahey, and R. R. Wing. “An Automated Internet Behavioral Weight-Loss Program by Physician Referral: A Randomized Controlled Trial.” Diabetes Care 38, no. 1 (2015): 9–15.
Thomas, J. G., and R. R. Wing. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study.” Journal of Medical Internet Research 1, no. 1 (2013): e3.
Turner-McGrievy, G. M., M. W. Beets, J. B. Moore, A. T. Kaczynski, D. J. Barr-Anderson, and D. F. Tate. “Comparison of Traditional versus Mobile App Self-monitoring of Physical Activity and Dietary Intake among Overweight Adults Participating in an mHealth Weight Loss Program.” Journal of the American Medical Informatics Association 20, no. 3 (2013): 513–18.
Watson, A., T. Bickmore, A. Cange, A. Kulshreshtha, and J. Kvedar. “An Internet-based Virtual Coach to Promote Physical Activity Adherence in Overweight Adults: Randomized Controlled Trial.” Journal of Medical Internet Research 14, no. 1 (2012): e1.
Nearly half of the reviewed studies (14 of 23 studies) established a statistically significant association between weight loss and the use of technology. All studies reported improvements in dietary habits and physical activity, although the association was not always statistically significant.
When the studies were categorized by the type of technology used, 73 percent (8 of 11) of the studies using mobile health devices showed statistically significant associations between weight loss and technology used, whereas only 40 percent (2 of 5) of the studies of telehealth/telemedicine and 50 percent (3 of 6) of the eHealth studies reported statistically significant differences. The one study categorized as involving wearable technology was statistically significant.
Only one of the reviewed studies10 examined the cost-effectiveness of using technology in the management of obesity. In addition to conducting a cost-effectiveness analysis, the authors of that study also found that per-patient costs and the overall weight loss were higher in the groups using technology compared with the control group (see Table 2).
Discussion
This review summarized the wide range of types of technology adopted for obesity management in studies published between 2010 and 2017. We identified positive and statistically significant findings in each of the four technology categories measured: telehealth/telemedicine, wearable technology, eHealth, and mobile health, using weight loss as the outcome measure. We expect that advances in technology will create additional ways to interact with users and capture outcomes at a more granular level.
Mobile health, eHealth, and telehealth/telemedicine were the most commonly used technologies for obesity management among the reviewed studies. The most popular technology, mobile health, with its portable, easily accessible, and ubiquitous nature, was used to monitor and promote weight loss by changing behavioral factors that contribute to a healthy lifestyle. It was supported by smartphones, cellphones, and other handheld mobile devices and applications to track and monitor diet and physical activity, and text messages/short message services (SMS) were used to provide reminders or encourage certain behaviors. Given the popularity of smartphones in the United States, the use of mobile health as an intervention device for obesity management showed continuous wide adoption, and the observed study outcomes suggest a positive future for this technology. This review study focuses on the United States; however, many other countries share widespread use of these technologies. Thus, what works in the United States may also work in other countries.
The definition of eHealth varied widely from study to study.11 Our definition of eHealth focused on internet and website applications rather than other health information technology applications, such as electronic health records or mobile devices. In the reviewed studies, eHealth involved the use of internet- and web-based applications, such as a web-based interactive voice response system, a virtual world, and internet-based virtual coaching, to provide an interactive platform for communication and education on diet, physical activity, and exercise. With advances in health information technology occurring rapidly, the definition of eHealth may change to accommodate the advances. A challenge in the labeling or grouping of technology for a literature review is to maintain the distinctions between types of technology across the study time frame or context.
Weight loss is a major outcome measurement in the reviewed studies. Other measurements include behavior changes, such as changes in step counts, physical activities, dietary contents, and eating patterns. Although a majority of the studies measured weight loss as one of the outcome measurements, only half of these studies reported statistically significant differences between weight loss and technology use. The sample size of the studies and the types of technology used may explain this result. Among the mobile health studies, the studies reporting significant weight loss differences had sample sizes ranging from 28 to 384 participants, compared with 20 to 58 participants in the studies that found no significant differences. Some of the studies had sample sizes smaller than 10 in our initial review; these studies were excluded. Future studies should address these factors as specific objectives to document potential impacts of sample size and study design issues.
The types of technology used showed an association with weight loss. Studies using mobile health showed more instances of statistically significant association with weight loss, as compared with studies using telehealth/telemedicine and eHealth. User experience and technology usability are critical factors, especially for interventional studies. The technology adoption model theory suggests that usefulness and ease of use are factors associated with technology adoption and should be identified in interventional studies.12, 13 When intervention outcome effects are examined, technology and participant acceptance should be considered. If the technology involved is difficult to use, inefficient, or ineffective, all of these could cause user dissatisfaction and noncompliance, thereby contributing to nonachievement of the goal that the study was intended to measure. Only two of the reviewed studies measured technology use and user satisfaction as outcome measures. Further study exploring associations between the user experience of technology and outcome changes could fill the gap in this area.
This literature review limited the search to studies conducted in the United States and published in the English language. Therefore, we have no basis of comparison to similar studies conducted in other countries. In addition, our study was limited to the empirical studies that were published in the five identified databases. Some study outcomes in other sources, such as conference proceedings, nonempirical study reports, or unpublished studies, may have been overlooked in our study. The last limitation is related to the definition of the technology used. Because definitions for categorizing technology have not been fully standardized, our definitions, such as that of eHealth, may not be the same as those used in other studies.
Future research needs to include patient-level outcomes as well as cost-effectiveness and user engagement of technology to fully evaluate the feasibility of continued and expanded use of technology in obesity management. Future studies should also identify consumers' individual and environmental factors, including consumers' motivation to use a given technology, in order to evaluate whether these factors are correlated with the technology used and with weight loss. In addition, sustainability and weight loss maintenance with the use of different types of technology should also be explored. Likewise, because some studies may use more than one type of technology as an intervention approach, the use of multiple technologies and their outcomes should be explored.
Conclusion
Adoption of technology such as mobile health, eHealth, and telehealth/telemedicine in obesity management has shown positive outcomes and wide usage. Weight loss and behavior changes are among the measurements evaluated in studies of technology use for obesity intervention. In an environment of continual development and refinement of technology, and the advent of new software to apply those developments, this field of research has a positive future. Appropriate and effective technology use, in the hands of skilled researchers, promises more positive outcomes in obesity management and intervention. The greatest need ahead is for these positive research findings to be applied and developed in the field of practice.
Acknowledgments
This work was funded by the National Science Foundation's Center for Healthcare Organization and Transformation (CHOT) Project 10-06181.
Contributor Information
SH Houser, Department of Health Services Administration, Health Informatics Program at the University of Alabama in Birmingham, AL..
R Joseph, Department of Health Services Administration at the University of Alabama in Birmingham, AL..
N Puro, Health Administration Program at the Florida Atlantic University in Boca Raton, FL..
DE Burke, Department of Health Services Administration at the University of Alabama in Birmingham, AL..
Notes
- 1.Centers for Disease Control and Prevention “Adult Obesity Facts.”. 2017 Available at https://www.cdc.gov/obesity/data/adult.html. [Google Scholar]
- 2.Centers for Disease Control and Prevention “Adult Obesity Causes & Consequences.”. 2017 Available at https://www.cdc.gov/obesity/adult/causes.html. [Google Scholar]
- 3.National Heart Lung and Blood Institute Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults . Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Heart Lung and Blood Institute; 1998. [Google Scholar]
- 4.Bacigalupo R., Cudd P., Littlewood C., Bissell P., Hawley M. S., Buckley Woods H. “Interventions Employing Mobile Technology for Overweight and Obesity: An Early Systematic Review of Randomized Controlled Trials.”. Obesity Reviews. 2013;14(no. 4):279–291. doi: 10.1111/obr.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krishna S. “Healthcare via Cell Phones: A Systematic Review.”. Telemedicine Journal and E-health. 2009;15(no. 3):231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 6.Shaw R. J., Steinberg D. M., Zullig L. L., Bosworth H. B., Johnson C. M., Davis L. L. “mHealth Interventions for Weight Loss: A Guide for Achieving Treatment Fidelity.”. Journal of the American Medical Informatics Association. 2014;21(no. 6):959–63. doi: 10.1136/amiajnl-2013-002610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haugen H. A., Tran Z. V., Wyatt H. R., Barry M. J., Hill J. O. “Using Telehealth to Increase Participation in Weight Maintenance Programs.”. Obesity. 2007;15(no. 12):3067–77. doi: 10.1038/oby.2007.365. [DOI] [PubMed] [Google Scholar]
- 8.Hartz J., Yingling L., Powell-Wiley T. M. “Use of Mobile Health Technology in the Prevention and Management of Diabetes Mellitus.”. Current Cardiology Reports. 2016;18:130. doi: 10.1007/s11886-016-0796-8. [DOI] [PubMed] [Google Scholar]
- 9.Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P., Clarke M., Devereaux P. J., Kleijnen J., Moher D. “The PRISMA Statement for Reporting Systematic Reviews and Meta-analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration.”. PLOS Medicine. 2009;6(no. 7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Archer E., Groessl E. J., Sui X., McClain A. C., Wilcox S., Hand G. A., Meriwether R. A., Blair S. N. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.”. American Journal of Preventive Medicine. 2012;43(no. 2):176–82. doi: 10.1016/j.amepre.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 11.Oh H., Rizo C., Enkin M., Jadad A. “What Is eHealth (3): A Systematic Review of Published Definitions.”. Journal of Medical Internet Research. 2005;7(no. 1):e1. doi: 10.2196/jmir.7.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis F. D. “A Technology Acceptance Model for Empirically Testing New End-User Information Systems: Theory and Results.”. Doctoral dissertation, Sloan School of Management, Massachusetts Institute of Technology. 1986 [Google Scholar]
- 13.Davis F. D. “Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology.”. MIS Quarterly. 1989;13(no. 3):319–40. [Google Scholar]