Abstract
Patient-centered care seeks to improve healthcare quality by engaging patients in their health management. Hospitals are employing strategies to enhance patient engagement to improve care quality, as measured by patient satisfaction through the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. Tablets are one tool hospitals use to increase patient engagement during hospitalization, as tablets can provide patients with access to both entertainment options and personal health information through patient portals. To explore the association between tablet access and patient satisfaction, data on tablet provisioning were linked to patient HCAHPS scores. Patients who were provided a tablet had higher HCAHPS scores in a subset of satisfaction measures, as compared with patients who were not provided a tablet, suggesting that tablets could positively influence patients' satisfaction with their hospital stay. Future studies are warranted to understand the specific ways in which tablet use improves the patient experience during hospitalization.
Keywords: inpatient, hospital care, patient-centered care, patient engagement, patient satisfaction, tablet computers, health information technology, personal health records, patient portals
Introduction
Hospitals are continually striving to improve the quality of patient care while reducing costs. Patient-centered care is one focus of quality improvement, aiming to deliver care that is driven by the needs and preferences of each individual patient.1 Increasing patients' engagement in their healthcare is therefore an important factor in attempts to improve quality by making care more patient-centered.2
The quality of patient-centered care can be evaluated indirectly by examining patient satisfaction, a measure of patients' perspectives about their healthcare experience.3 Although the relationship between patient-centered care, quality of care, and patient satisfaction is complex,4 the measurement of patient satisfaction as a means to quantify healthcare quality has been widely adopted as a means to both evaluate hospital performance and identify opportunities for improvement in care processes.5 As a result, improving patient satisfaction is advantageous to patients as well as hospital systems, since patient satisfaction greatly affects the business of healthcare. Satisfied patients are more likely to be loyal patients, meaning that they are more likely to be repeat customers and refer other potential patients to the hospital system.6 In contrast, dissatisfied patients may not return to that healthcare system for future care; Reichheld and Sasser refer to this as “customer defections.”7 These defections have a significant impact on the profitability of healthcare organizations because long-term customers generate additional revenue through referrals and price premiums. For example, loyal, long-term patients may be willing to pay more to continue seeing a doctor they trust, rather than switching to a new, less expensive doctor.8
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey is designed to collect patients' perspectives about their healthcare experience during their inpatient hospital stay. This survey assesses patients' experiences regarding communication with nurses and doctors, responsiveness of hospital staff, pain management, communication about medicines, discharge planning, care transition, the hospital environment, and overall impression of the hospital. Asking patients for their perspectives may provide information about aspects of the hospital stay that are not otherwise measurable. For example, hospital readmission rates were found to be significantly lower for congestive heart failure patients who reported higher satisfaction with discharge planning.9 Hospital readmission rates were not, however, significantly different when compared according to the completeness of discharge instructions provided to the patient, as reported in their medical record, suggesting that patients' reports about their experience provide a unique perspective about the quality of care that is received. Overall patient satisfaction with the hospital stay, as well as patient satisfaction with discharge planning, has also been found to be negatively correlated with readmission rates in patients with acute myocardial infarction, heart failure, and pneumonia.10
Beginning in 2008, the US Department of Health and Human Services began publicly reporting HCAHPS survey results. Public reporting of this survey data encourages critical comparisons among hospitals and affects hospital reimbursement by the Centers for Medicare and Medicaid Services (CMS).11 Hospitals are therefore strongly motivated to improve patient satisfaction scores, not only to reflect high quality of care, but to attract and retain patients and to secure hospital revenue by maximizing CMS reimbursements and avoiding penalties.
Health information technology (HIT) has been widely implemented by hospitals, often with the intent of increasing patient satisfaction. At the simplest level, HIT such as a tablet computer offering mobile applications can be a source of entertainment for patients, reducing anxiety during their hospitalization.12 The use of HIT can also influence patient satisfaction by increasing patients' engagement in their care, as patients who are more activated and invested in their health generally report better healthcare experiences.13 Patient portals are an example of HIT that may include features that increase patient engagement, including access to a patient's medical record, health education material, appointment scheduling, prescription requests, test results, and secure messaging with their providers.14 Although the majority of patient portals are currently implemented in outpatient settings, portals are increasingly being introduced in inpatient care. In this context, a patient portal offers features that are tailored to the hospital stay, including the ability for patients to view their daily schedule, order meals, check test results, and communicate with their care team. Available via a tablet computer, inpatient portals have the potential to improve patient satisfaction through their influence on patient engagement; however, the effects of both tablets and patient portals on patient engagement, and the implications of this use of HIT on patient satisfaction, remain to be fully elucidated.15
At a large midwestern academic medical center, inpatients are offered Android tablets during their hospital stay. Through these tablets, patients have access to an inpatient portal, MyChart Bedside (Epic Systems), as well as access to the internet and applications such as Facebook, Hulu, Solitaire, and Pandora.16 We investigated the HCAHPS scores of patients who were provided tablets during their inpatient stay, compared with patients who did not receive tablets, in an effort to understand whether and how tablets are associated with patient satisfaction during hospitalization.
Methods
HCAHPS Survey
The HCAHPS survey contains questions that are aggregated into composite measures related to nine dimensions of patient satisfaction:
nurse communication,
doctor communication,
responsiveness of hospital staff,
communication about medication,
pain management,
discharge information,
care transition,
cleanliness of the hospital environment, and
quietness of the hospital environment.17
In addition to the composite measures, the HCAHPS survey also collects two global measures of the hospital experience:
hospital rating, and
likelihood to recommend the hospital to a friend or family member.18
Our analysis focused on the HCAHPS measures that may be best linked to patient experience related to tablet use; as a result, we excluded the measures related to satisfaction with the hospital facility (i.e., cleanliness and quietness of the hospital environment). We also did not report the results for pain management as we were unable to obtain scores for this measure during the study period because of an institutional decision to not collect this information. The survey questions attributed to the HCAHPS measures assessed in our study are listed in the Appendix.
The HCAHPS survey questions have various response formats, including definitely no, probably no, probably yes, definitely yes; never, sometimes, usually, always; yes, no; strongly disagree, disagree, agree, strongly agree; and a score of 0 to 10. We focus on the top-box scores (i.e., the most positive responses), which are based on the percentage of patients that indicate definitely yes, always, yes, strongly agree, or a score of 9 or higher for a specific measure.19 We also record the top-box rollup percentiles, which indicate hospital performance in reference to the representative scores from a national sample of hospitals. The HCAHPS scores are collected on a rolling basis at the medical center and were aggregated by calendar year over the time frame of our study.
Data Source and Study Sample
Data on tablet provisioning was extracted from the medical center's information warehouse for January 2016 through December 2017; this time range reflects the period after the systemwide implementation of the MyChart Bedside patient portal, when the tablets were introduced. The data indicated whether or not a patient received a tablet during their hospital stay. Some patients were excluded from tablet provisioning, including patients who were less than 18 years old, unable to speak or read English, or involuntarily confined or detained. Additionally, the HCAHPS survey excluded patients with less than an overnight stay in the hospital, patients with a principal psychiatric diagnosis, or patients who were not alive at the time of discharge. Other criteria that would exclude a patient from the HCAHPS survey are discussed elsewhere.20 Among the 117,074 eligible patients during our study period, 32,909 patients (28.1 percent) received a tablet, and 84,165 patients (71.9 percent) did not receive a tablet.
Each patient visit across the medical center's six hospitals was recorded using a unique encounter number. The HCAHPS scores were linked by this number to patients who did or did not receive a tablet, as long as patients met the inclusion criteria. Response rates for the HCAHPS survey was 16.5 percent for patients receiving tablets (5,435 of 32,909 patients) and 11.9 percent for patients not receiving a tablet (10,041 of 84,165 patients).
A sensitivity analysis was also conducted for the period from January 2017 to December 2017, when use of the tablets and MyChart Bedside was stable following the initial rollout in 2016. Among the 60,222 eligible patients during this period, 21,429 patients (35.6 percent) received tablets and 38,793 patients (64.4 percent) did not receive tablets. Response rates for the HCAHPS survey in this period was 15.8 percent for the patients with tablets (3,390 of 21,429 patients) and 11.8 percent for the patients without tablets (4,576 of 38,793 patients).
Analysis
We report the unadjusted top-box scores and the respective top-box rollup percentiles for the composite and global HCAHPS measures as combined scores from all of the medical center's six hospitals. We compare each of these patient satisfaction scores between patient groups that did and did not receive a tablet during their hospital stay. To identify statistical differences between top-box scores for patient groups with and without tablets, we tested the equality of proportions between these groups. Statistical analysis was performed with Stata 15 software (StataCorp). We used a similar approach for our sensitivity analysis.
Results
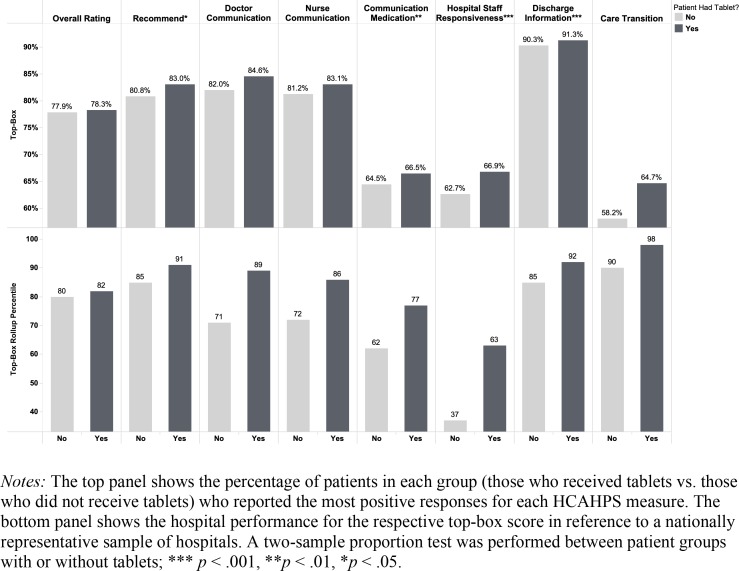
Figure 1 summarizes the results of our study. Top-box scores across all HCAHPS measures were higher for the patient group that received tablets, compared with the patient group that did not receive tablets during their hospital stay. Our statistical tests demonstrated, however, that there were significant differences between these groups for only a subset of HCAHPS measures: whether the patient would recommend the hospital; communication about medication; responsiveness of hospital staff; and discharge information. The biggest difference between the two groups was for responsiveness of hospital staff (4.2 percentage points), and the smallest difference was for discharge information (1.0 percentage point). The differences in top-box rollup percentiles for two of the statistically significant measures—communication about medication and responsiveness of hospital staff—were particularly notable, with 15 and 26 percentile ranking point differences between groups, respectively. This suggests that the statistical distribution of top-box scores for these two measures was particularly narrow across hospitals nationally. The results from our sensitivity analysis (data from 2017 only) were not notably different from those of our main analysis (data from 2016–2017), suggesting that patient satisfaction did not change appreciably with time following the beginning of tablet provisioning across the medical center's hospitals.
Figure 1.
Top-Box Scores and Top-Box Rollup Percentiles by HCAHPS Global and Composite Measures (N = 15,476)
Discussion
Significant differences in HCAHPS top-box scores indicate that patients who received tablets were more satisfied with some aspects of their hospital care. Of the two global measures in the HCAHPS survey, one was found to have significantly higher top-box scores for patients who were provided tablets. These patients were more likely to recommend the hospital to their friends and family, compared with patients who were not provided tablets, suggesting that tablets could increase overall patient satisfaction with the hospital stay. However, the second global measure—overall hospital rating—was not statistically different between patient groups, suggesting that the way in which patients are asked to assess their overall hospital satisfaction (rating or recommending) and the format in which their answers are provided (0 to 10 or definitely no to definitely yes) may influence the perceived overall satisfaction of patients.
Among the composite measures, statistical differences in top-box scores were noted between patients with and without tablets for the HCAHPS dimensions of communication about medication, responsiveness of hospital staff, and discharge information. It is encouraging to see that providing tablets is associated with higher patient satisfaction in these measures, especially those that may be tied to important clinical outcomes, such as communication about medication and discharge information, which may reduce adverse events and readmissions.21, 22 The remaining composite measures of communication with nurses, communication with doctors, and care transition did not have significant differences in top-box scores between patients who did and did not receive tablets during their hospitalization.
Patients have a desire to be informed about their diagnosis and care plan during hospitalization,23 and HIT can potentially improve patients' participation in their care through the delivery of health information and enhancement of communication.24 The expanding use of inpatient portals can increase patient access to health information pertinent to their hospital care through multiple mechanisms, including access to educational materials, daily schedules, test results, vital sign information, diagnosis lists, and secure messaging; access to this information can increase patients' understanding of their health condition and treatment.
In some of the patient satisfaction measures for which we saw statistically significant differences in top-box scores between the groups with and without tablets, it is possible that the entertainment provided by the tablets was perceived as valuable. For instance, the ability to use the tablet for entertainment could help patients pass the time while waiting for help from hospital staff, thereby increasing perceived satisfaction with hospital staff responsiveness. Also contributing to the patients' perceptions of hospital staff responsiveness could be the portal feature that offered a way for patients to make nonurgent requests to their care team without having to use their call light.
Patients reporting significantly greater satisfaction with communication about medication when they received tablets may have benefited from access to more information about their medications through the inpatient portal. In this context, MyChart Bedside offers patients information about the purpose of their medications, their dosing schedule, and potential side effects, and the availability of this information may influence their satisfaction with communication about medication. Interestingly, there were not significant differences in satisfaction with doctor or nurse communication between patients with or without tablets, despite the fact that access to the inpatient portal via the tablet offered new channels for communication between patients and providers through both secure messaging and the ability make nonurgent requests. This may reflect the complexity of the HCAHPS composite scores for doctor and nurse communication, which are based on questions evaluating providers' courtesy and listening as well as explanations of health information, not all of which can be directly affected by tablet functions.
Preparing patients for discharge could also be influenced by tablet access to inpatient portal features. Through MyChart Bedside, educational discharge instructions and medication management information can help prepare patients for expected symptom management needs and care responsibilities after they leave the hospital. These features may have contributed to the statistically significant higher patient satisfaction with discharge information among patients with tablets; however, variations in satisfaction with discharge and care transition may also be due to the design of the HCAHPS questions that are aggregated to form these composite measures, similar to the complexity of the composite scores for communication.
Several limitations of our study should be recognized. First, in seeking to understand the differences in patient satisfaction between groups with and without tablets, this study did not evaluate the ways in which the tablets were used. Once provided, tablets could be used for entertainment—to browse the internet, watch movies, or listen to music—or they could be used to access health information, communicate with providers, or order meals through the inpatient portal, MyChart Bedside. Second, our study design does not exclude the possibility of patients using their own tablets during their hospital stay. Therefore, patients in the group who were not provided tablets could have had access to their personal tablet. Third, our study presents findings from a single hospital system; nonetheless, our inclusion of all six hospitals in the medical center provides a large, diverse sample of patients and increases the generalizability of this study. Fourth, the suite of features offered on the tablets at this academic medical center may vary from those offered at other medical centers, as a single inpatient portal platform was offered throughout this particular academic medical center. While the inpatient portal platform may differ at other hospital systems, the widespread implementation of Epic Systems portals across US hospitals, as well as the similarity of features between different portal platforms, further supports the generalizability of this study.
Additional studies are warranted to specifically compare patient satisfaction between groups that use tablets to access inpatient portals and those that do not. Furthermore, the relationship between the use of different inpatient portal features (e.g., secure messaging with care team members) and their associated HCAHPS dimensions (e.g., communication with doctors or nurses) is also needed to improve our understanding of the value of individual inpatient portal features.
Conclusion
The provision of tablet computers may improve the patient experience and enhance patient engagement in the hospital setting. This study offers evidence that providing tablets to inpatients was associated with increased satisfaction in aspects of their hospital stay, suggesting that access to tablets could improve patients' impressions of the hospital, communication about medication use and side effects, timeliness of receiving help from hospital staff, and preparation for discharge. Future work will help to strengthen our understanding of how to best implement and promote tablet use to positively influence patient experiences during hospitalization.
Acknowledgments
The authors would like to acknowledge Nicholas Gibson and Kristen Johnson, both affiliated with the authors' institution, for their efforts in the acquisition of HCAHPS score data.
Appendix
HCAHPS Survey Questions Attributed to Relevant Patient Satisfaction Measures
Note: Top-box responses are bold and underlined.
Overall Rating
Using any number from 0 to 10, where 0 is the worst hospital possible and 10 is the best hospital possible, what number would you use to rate this hospital during your stay? [Scale: 0 (Worst hospital possible), 1, 2, 3, 4, 5, 6, 7, 8, 9, 10 (Best hospital possible)]
Recommend the Hospital
Would you recommend this hospital to your friends and family? [Scale: Definitely no, Probably no, Probably yes, Definitely yes]
Doctor Communication
During this hospital stay, how often did doctors treat you with courtesy and respect? [Scale: Never, Sometimes, Usually, Always]
During this hospital stay, how often did doctors listen carefully to you? [Scale: Never, Sometimes, Usually, Always]
During this hospital stay, how often did doctors explain things in a way you could understand? [Scale: Never, Sometimes, Usually, Always]
Nurse Communication
During this hospital stay, how often did nurses treat you with courtesy and respect? [Scale: Never, Sometimes, Usually, Always]
During this hospital stay, how often did nurses listen carefully to you? [Scale: Never, Sometimes, Usually, Always]
During this hospital stay, how often did nurses explain things in a way you could understand? [Scale: Never, Sometimes, Usually, Always]
Communication about Medication
Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? [Scale: Never, Sometimes, Usually, Always]
Before giving you any new medicine, how often did hospital staff describe possible side effects in a way you could understand? [Scale: Never, Sometimes, Usually, Always]
Hospital Staff Responsiveness
During this hospital stay, after you pressed the call button, how often did you get help as soon as you wanted it? [Scale: Never, Sometimes, Usually, Always, I never pressed the call button]
How often did you get help in getting to the bathroom or in using a bedpan as soon as you wanted? [Scale: Never, Sometimes, Usually, Always]
Discharge Information
During this hospital stay, did doctors, nurses or other hospital staff talk with you about whether you would have the help you needed when you left the hospital? [Scale: Yes, No]
During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital? [Scale: Yes, No]
Care Transition
During this hospital stay, staff took my preferences and those of my family or caregiver into account in deciding what my health care needs would be when I left. [Scale: Strongly disagree, Disagree, Agree, Strongly agree]
When I left the hospital, I had a good understanding of the things I was responsible for in managing my health. [Scale: Strongly disagree, Disagree, Agree, Strongly agree]
When I left the hospital, I clearly understood the purpose for taking each of my medications. [Scale: Strongly disagree, Disagree, Agree, Strongly agree, I was not given any medication when I left the hospital]
Contributor Information
S Vink, The Ohio State University Medical Center in Columbus, OH..
N Fareed, The Ohio State University in Columbus, OH..
SR MacEwan, The Ohio State University in Columbus, OH..
AS McAlearney, The Ohio State University in Columbus, OH..
Notes
- 1.Epstein R. M., Street R. L. “The Values and Value of Patient-centered Care.”. Annals of Family Medicine. 2011;9(no. 2):100–103. doi: 10.1370/afm.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coulter A. “Patient Engagement—What Works?”. Journal of Ambulatory Care Management. 2012;35(no. 2):80–89. doi: 10.1097/JAC.0b013e318249e0fd. [DOI] [PubMed] [Google Scholar]
- 3.Sitzia J., Wood N. “Patient Satisfaction: A Review of Issues and Concepts.”. Social Science & Medicine. 1997;45(no. 12):1829–43. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- 4.Kupfer J. M., Bond E. U. “Patient Satisfaction and Patient-centered Care: Necessary but Not Equal.”. JAMA. 2012;308(no. 2):139–40. doi: 10.1001/jama.2012.7381. [DOI] [PubMed] [Google Scholar]
- 5.Epstein R. M., Street R. L. “The Values and Value of Patient-centered Care.”. doi: 10.1370/afm.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heskett J. L. “Beyond Customer Loyalty.”. Managing Service Quality. 2002;12(no. 6):355–57. [Google Scholar]
- 7.Reichheld F., Sasser Jr W. E. “Zero Defections: Quality Comes to Services.”. Harvard Business Review. 1990;68(no. 5):105–11. [PubMed] [Google Scholar]
- 8.Ibid.
- 9.Jha A. K., Orav E. J., Epstein A. M. “Public Reporting of Discharge Planning and Rates of Readmission.”. New England Journal of Medicine. 2009;361:2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 10.Boulding W., Glickman S. W., Manary M. P., Schulman K. A., Staelin R. “Relationship between Patient Satisfaction with Inpatient Care and Hospital Readmission within 30 Days.”. American Journal of Managed Care. 2011;17(no. 1):41–48. [PubMed] [Google Scholar]
- 11.Giordano L. A., Elliot M. N., Goldstein E., Lehrman W. G., Spencer P. A. “Development, Implementation, and Public Reporting of the HCAHPS Survey.”. Medical Care Research and Review. 2010;67(no. 1):27–37. doi: 10.1177/1077558709341065. [DOI] [PubMed] [Google Scholar]
- 12.Prey J. E., Woollen J., Wilcox L., Sackeim A. D., Hripcsak G., Bakken S., Restaino S., Feiner S., Vawdrey D. K. “Patient Engagement in the Inpatient Setting: A Systematic Review.”. Journal of the American Medical Informatics Association. 2014;21(no. 4):742–50. doi: 10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hibbard J. H., Greene J. “What the Evidence Shows about Patient Activation: Better Health Outcomes and Care Experiences; Fewer Data on Costs.”. Health Affairs. 2013;32(no. 2):207–14. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 14.Prey J. E., Woollen J., Wilcox L., Sackeim A. D., Hripcsak G., Bakken S., Restaino S., Feiner S., Vawdrey D. K. “Patient Engagement in the Inpatient Setting: A Systematic Review.”. doi: 10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ammenwerth E., Schnell-Inderst P., Hoerbst A. “The Impact of Electronic Patient Portals on Patient Care: A Systematic Review of Controlled Trials.”. Journal of Medical Internet Research. 2012;14(no. 6):e162. doi: 10.2196/jmir.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huerta T. R., McAlearney A. S., Rizer M. K. “Introducing a Patient Portal and Electronic Tablets to Inpatient Care.”. Annals of Internal Medicine. 2017;167(no. 11):816–17. doi: 10.7326/M17-1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Medicare.gov Hospital Compare “Survey of Patients' Experiences (HCAHPS).”. Available at https://www.medicare.gov/hospitalcompare/Data/Overview.html. [Google Scholar]
- 18.Ibid.
- 19.Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) “A Note about HCAHPS ‘Boxes.’“. Available at https://www.hcahpsonline.org/en/summary-analyses/#NoteAboutBoxes. [Google Scholar]
- 20.Goldstein E., Elliott M. N., Lehrman W. G., Hambarsoomian K., Giordano L. A. “Racial/Ethnic Differences in Patients' Perceptions of Inpatient Care Using the HCAHPS Survey.”. Medical Care Research and Review. 2009;67(no. 1):74–92. doi: 10.1177/1077558709341066. [DOI] [PubMed] [Google Scholar]
- 21.Boulding W., Glickman S. W., Manary M. P., Schulman K. A., Staelin R. “Relationship between Patient Satisfaction with Inpatient Care and Hospital Readmission within 30 Days.”. [PubMed] [Google Scholar]
- 22.Phatak A., Prusi R., Ward B., Hansen L. O., Williams M. V., Vetter E., Chapman N., Postelnick M. “Impact of Pharmacist Involvement in the Transitional Care of High-Risk Patients through Medication Reconciliation, Medication Education, and Postdischarge Call-Backs (IPITCH Study).”. Journal of Hospital Medicine. 2016;11(no. 1):39–44. doi: 10.1002/jhm.2493. [DOI] [PubMed] [Google Scholar]
- 23.Woollen J., Prey J., Wilcox L., Sackeim A., Restaino S., Raza S. T., Bakken S., Feiner S., Hripcsak G., Vawdrey D. “Patient Experiences Using an Inpatient Personal Health Record.”. Applied Clinical Informatics. 2016;7(no. 2):446–60. doi: 10.4338/ACI-2015-10-RA-0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roberts S., Chaboyer W., Gonzalez R., Marshall A. “Using Technology to Engage Hospitalised Patients in Their Care: A Realist Review.”. BMC Health Services Research. 2017;17(no. 1):388. doi: 10.1186/s12913-017-2314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]