Abstract
Penile metastasis of adenocarcinoma of prostate is an extremely rare clinical entity and even less of such cases presenting with malignant priapism. Management of priapism with penile shunting is recommended in this case. No consensus beyond personal recommendation from other studies found in this case due to the relative rarity of the disease and the associated lack of data. In this study, we present a case of malignant priapism due to penile metastasis of adenocarcinoma of the prostate, an extremely rare clinical entity and a more uncommon site of metastasis.
Keywords: Malignant priapism, Penile metastasis, Prostate adenocarcinoma
Introduction
Priapism is defined as a sustained, undesirable erection lasting greater than 4 hours which is not associated with stimulation or sexual interest. The etiology of priapism is usually categorized as high-flow or low-flow states with idiopathic or pharmacologic causes in most cases.1 Adenocarcinoma of prostate may prone to metastasize to other organs, such as lungs and bladder. Despite the rich vascular network of penis, metastasis of adenocarcinoma of prostate to penis happens very rarely, with only about 400 cases of such reported from its first discovery in 19th centuries.1 We present a case of malignant priapism due to metastatic primary adenocarcinoma of the prostate.
Case presentation
A male patient, 67 years old, complaint of painful and persistent erection since 12 hours prior admission (Fig. 1). Patient had underwent prostate biopsy 2 weeks ago. The pathology anatomy result was Adenocarcinoma prostate Gleason score 9 (5 + 4). Androgen deprivation therapy (ADT) was initiated after pathological result was confirmed.
Fig. 1.
Priapism at the emergency, Foley catheter was attached before admittance due to previous history of urinary retention.
Patient was fully conscious with vital sign within normal limit. Penis was fully erected with EHS Score 4. Digital rectal examination has revealed asymmetrical prostate with nodules on the surface of right prostate. The blood laboratory test indicative of anemia and elevated of creatinine level. PSA level was 313 ng/dl.
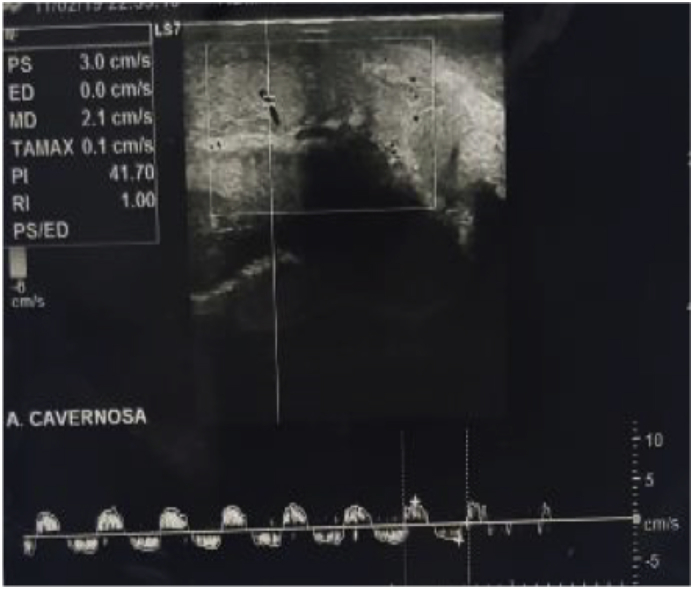
Penile Doppler ultrasonography (USG) was performed on penis and found decreased of end diastolic volume cavernosa artery (Fig. 2). Abdominal USG were suggestive of chronic kidney disease due to obstructive uropathy from prostate adenocarcinoma and bilateral hydronephrosis.
Fig. 2.
Penile Doppler Ultrasound revealed decreased of end diastolic volume cavernosal artery.
The histological examination has revealed ovoid, hyperplastic, dense, and clumping tumor cells. The biopsy results confirmed of prostate adenocarcinoma, with Gleason score 9 (5 + 4) and grade group 5. Based on the history taking, physical examination, and other examinations, the working diagnosis of this case was malignant low-flow priapism with adenocarcinoma prostate Gleason Score 9 (5 + 4), Anemia and chronic kidney disease.
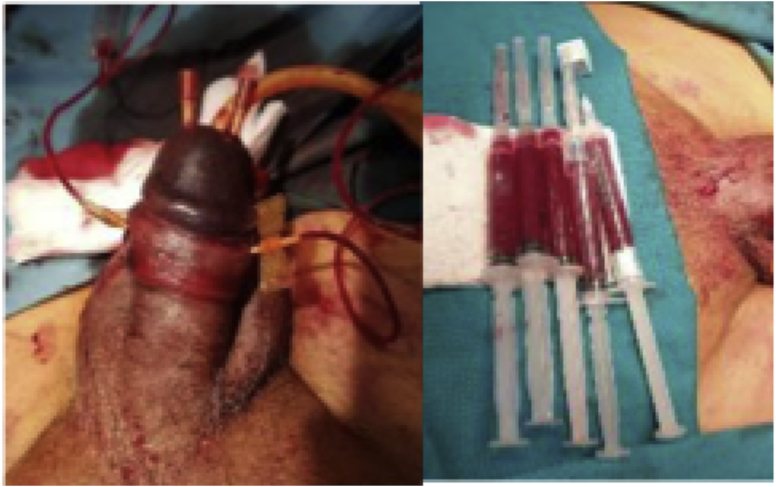
The patient was managed operatively using distal shunt on glans penis and distal shaft with local anesthesia (Fig. 3). The procedure was done in 1 h. Blood samples from penis were collected and sent to laboratory for examination. Blood gas analysis result was PH: 7142; PCO2; 26,9; PO2: 111,8; HCO3: 9,3. The result was metabolic acidosis. After procedure, it resulted in the simultaneous detumescence of the penis.
Fig. 3.
Winter Procedure was performed and 50 mL of initial drainage of blood was achieved.
Discussion
Priapism is defined as a persistent and painful erection lasting longer than 4 h without prior sexual stimulation. The incidence of the case is reported to be around 0.3–1.0 per 100,000 males per year. There are at least 7 articles that report priapism with prostate cancer since 2010.
Clinical management of priapism is aimed to eliminate continuous erection and preserve the ability to have erections in the future. Penile tissue damage may occur in ischemic priapism. The first line of acute management of ischemic priapism is corporal aspiration. Aspiration should be continued until the dark red venous blood becomes bright red oxygenated blood. In cases of ischemic priapism continuing for more than 48 hours, surgical management is recommended instead, by making an iatrogenic fistula to drain the deoxygenated blood from the corpora cavernosa.2 The guidelines for priapism from European Association of Urology had stated that each procedures (penile shunting) are not significantly different in outcome; although the data provided in the present is still insufficient to make any significant comparison of efficacies of each method.3
Prostate cancer is one of the most commonly occurring cancer, barring cutaneous malignancies, with approximately 160,000 males diagnosed with prostate cancer in 2017 alone in United States, adding to the existing 3.3 million survivors. Diagnostic methods, for screening and/or prognostic purposes, have been developed due to its relatively insidious development.2
Malignant priapism is first defined in 1938 by Peacock, it was described as a persistent erection, not related with sexual activity, caused by cavernous sinus and associated venous systems with malignant cells. Malignant priapism is an exceedingly rare manifestation of cancerous lesions, with 140 described cases up until 1961 and only 372 case reports malignant priapism up to 2006 from its first discoveries several centuries ago. Despite its high flow of blood, penis is a very rare site for metastasis and usually found in late stages of the disease.3 Penile metastases are most commonly from the prostate and the bladder. A case series consisted of 29 cases of metastatic prostate cancer to penis had described the most prominently occurred in patients with high Gleason score.4
Due to the rarity of the case, limited data is available to determine the most prevalent origin of penile metastasis. Lin et al. had compiled 394 cases of penile metastasis according to its point of origin. The predominant origins of penile metastasis were prostate (129 cases, 33%) and bladder (118 cases, 30%). From all the cases, only 20–50% of penile metastases present as malignant priapism. However, they concluded that prognoses are generally very poor, with the majority of patients surviving less than 18 months, with an average survival of approximately 9 months and longest survival of about 7 and 9 years. The cases analyzed in the study are managed mainly managed with palliation and improvement of quality of life, although there were some cases that had considered surgical management, such as penectomy, in order to excise the malignant lesions from penis and improve the symptoms.5
Conclusion
Penile metastasis of adenocarcinoma prostate is an extremely rare clinical entity and even less of such cases presenting with malignant priapism. Doppler ultrasound in this case indicated the patient has a low-flow (ischemic) priapism secondary to penile metastasis of primary adenocarcinoma of the prostate. Prostatic biopsy was done and high grade adenocarcinoma of the prostate was confirmed with histological examination. Penile metastasis with malignant priapism is managed with identical methods to acute management of priapism. In this case, penile shunt was used due to the history of adenocarcinoma of the prostate presenting in malignant priapism. The very limited data regarding malignant priapism secondary to penile metastasis from adenocarcinoma of the prostate causing no guideline in management of such cases.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.101102.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kitley C.A., Mosier A.D., Keylock J., Nguyen D. Malignant priapism secondary to adenocarcinoma of the prostate. BMJ Case Rep. 2010;2010 doi: 10.1136/bcr.07.2009.2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Litwin M.S., Tan H.J. The diagnosis and treatment of prostate cancer: a review. JAMA. 2017;317(24):2532–2542. doi: 10.1001/jama.2017.7248. [DOI] [PubMed] [Google Scholar]
- 3.Salonia A., Eardley I., Giuliano F. European Association of Urology guidelines on priapism. Eur Urol. 2014;65(2):480–489. doi: 10.1016/j.eururo.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Ellis C.L., Epstein J.I. Metastatic prostate adenocarcinoma to the penis: a series of 29 cases with predilection for ductal adenocarcinoma. Am J Surg Pathol. 2015;39(1):67–74. doi: 10.1097/PAS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 5.Lin Y.-H., Kim J.J., Stein N.B., Khera M. Malignant priapism secondary to metastatic prostate cancer: a case report and review of literature. Rev Urol. 2011;13(2):90–94. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.