Abstract
Purpose:
Achieving adequate levels of illumination to stimulate the circadian system can be difficult in a nursing home. The aim of this study was to examine the impact that a 4-week cycled lighting intervention had on activity, sleep, and mood in older adults living in a nursing home.
Patients and methods:
Ten residents were given an activity monitor to objectively measure activity and sleep, and subjective mood scores were also recorded during the study period. The cycled lighting intervention was designed to mimic normal natural daylight.
Results:
Some participants responded positively to the lighting intervention showing improvements in activity levels, sleep, and mood, while others showed no change or a continued decline.
Conclusion:
Although the results are inconclusive, a cycled lighting intervention remains a potentially promising intervention in the nursing home setting. Further studies with more robust measurements and a larger, more homogeneous cohort are required to investigate this further.
Keywords: sleep, activity, mood, light, circadian rhythms, older adult
Introduction
The body’s internal clock, known as the circadian system, regulates the timing and expression of many physiological and behavioral processes, most notable being the sleep–wake cycle. Circadian rhythm, roughly a 24-hour rhythm is controlled by the suprachiasmatic nucleus (SCN) located in the hypothalamus of the brain (Schibler & Sassone-Corsi, 2002). Circadian rhythm is synchronized by many factors, with light being the most important exogenous stimulus (Duffy et al., 1996). Light at the right time in the morning has a positive effect on the daily rhythm, whereas light late in the evening has a negative effect. The luminous excitation is related not only to the intensity of the light but also to its spectrum. The circadian system is maximally sensitive to short-wavelength (blue) light, with a peak spectral sensitivity at around 460 nm, which is highly prevalent during daylight (Brainard et al., 2008).
Many physiological changes occur with aging, including the circadian system which undergoes significant changes affecting rhythms of behaviors, temperature regulation, and hormone release (Hood & Amir, 2017). These changes may result in disturbances in sleep such as fragmented nocturnal sleep with multiple and prolonged awakenings and increased daytime napping (McCurry et al., 2011). These abnormalities are more frequent and pronounced in older adults with Alzheimer’s disease and related dementia (ADRD) (McCurry et al., 2011). It is thought that degenerative changes in the SCN result in these more pronounced circadian disturbances (Prinz et al., 1984).
Bright light during the day and dim light at night is suggested to entrain natural circadian rhythms. However, achieving adequate levels of natural illumination can be difficult, particularly in a nursing home environment where the light sources used usually do not provide adequate stimulation. It is a challenge for many older adults, especially those with impaired mobility or impaired cognitive functioning to get outside and get the daylight required to achieve a stable circadian rhythm.
There is a large and growing body of evidence supporting the therapeutic application of light. Figueiro (2008) proposed a cycled lighting scheme for older adults with cool, high light levels for high circadian stimulation during the daytime, and warm, low light levels for reduced circadian stimulation in the evening. This lighting intervention was shown to increase sleep efficiency (Figueiro et al., 2015) and to decrease depression and agitation scores (Figueiro et al., 2014) in persons with ADRD living in long-term care facilities. More recently, researchers investigated whether a lighting intervention impacted upon circadian rhythm in patients in intensive care and discovered exposure to bright white light during the day was shown to improve rest–activity patterns (Engwall et al., 2017). However, others have reported no improvements in measures of sleep or daytime alertness in nursing home residents with increased exposure to bright light (Ancoli-Israel et al., 2002; Dowling et al., 2005).
This work seeks to add to research in this field. The overarching aim of this research was to evaluate the effects that a cycled lighting intervention had on sleep, mood, and activity in older adults living in a nursing home. It was hypothesized that the lighting intervention would increase physical and social activities during the day and result in greater fatigue, providing in turn more restorative sleep at night and resultantly an overall improvement in the well-being of residents.
Material and Methods
This pilot study was a pragmatic control trial enrolling older adult residents living in a nursing home in Ireland. This study spanned an 8-week period between January 2019 and March 2019: 2 weeks of baseline measurements, a 4-week intervention period, and a 2-week follow-up period. This study was reviewed and approved by the School of Health and Science Ethics Committee in Dundalk Institute of Technology, Dundalk, Ireland.
Population
A sample of convenience of older adult residents in the nursing home was enrolled. As this was an exploratory pilot study, formal sample size calculations were not performed and the sample size selected was based on the number of participants that could be conveniently recruited.
Residents and family members were informed about this study by way of information posters placed on the notice boards throughout the nursing home. An information letter was also sent to the designated next of kin of all residents and enclosed an expression of interest form. Interested residents were screened for their suitability to take part by a member of the research team. A pragmatic approach to participant eligibility was adopted so as to maximize the number of participants enrolled. The only exclusion criteria was if a resident was bed bound or deemed too ill by nursing staff to attend an activity room in the nursing home. Written informed consent was obtained from residents/next of kin before any assessment was performed.
Intervention
Two of the communal rooms in the study site have a Human Centric Lighting (HCL) system (Glamox Ireland Limited, Dublin, Ireland) installed to deliver the intervention. The cycled lighting intervention delivered in this study was designed to mimic normal natural daylight. The lighting intervention was delivered through recessed ceiling-mounted white luminaires for 11 hours per day (9 a.m. to 8 p.m.) for 4 weeks. During this 4-week intervention period, the system automatically cycled from a spectrum correlated to a color temperature of 6,500 kelvin (K) (delivering a cool, bluish light for high circadian stimulation—Figure 1a) between 9 a.m. and 3 p.m., and then back to 2,700–3,000 K (warm, yellowish light for reduced circadian stimulation—Figure 1b) from 3 p.m. to 8 p.m. The parameters of the lighting intervention are summarized in Table 1.
Figure 1.
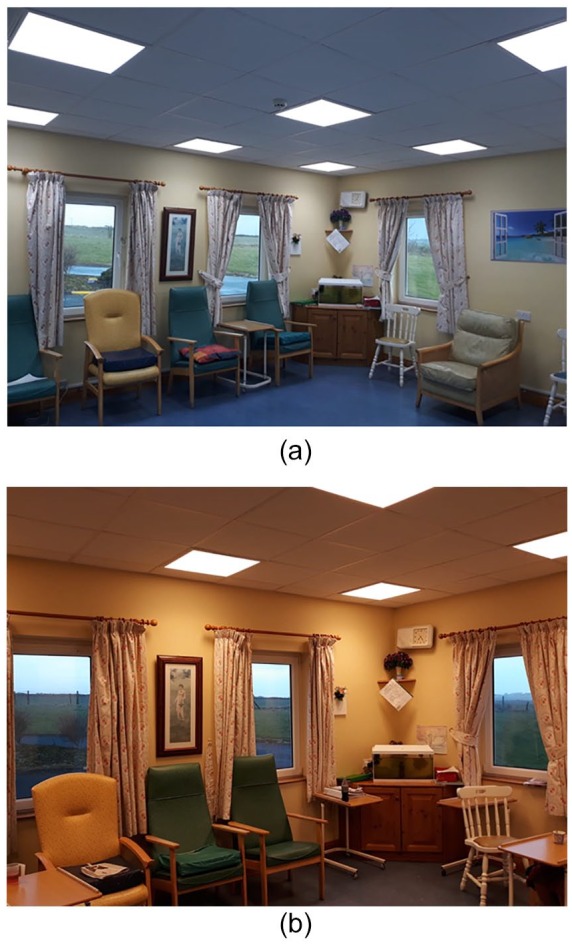
(a) Cool, bluish light for high circadian stimulation. (b) Warm, yellowish light for reduced circadian stimulation.
Table 1.
Cycled Lighting Intervention Parameters.
| Time (24-hour clock) | 09.00 to 15.00 | 15.00 to 20.00 |
|---|---|---|
| Cylindrical illuminance Ez | 1200 lx at 1.2 m | 1200 lx at 1.2 m |
| Correlated color temperature (CCT) | 6,500 kelvin (K) | 2700–3,000 kelvin (K) |
According to the nursing home staff, residents habitually use the same communal room every day; therefore, those who normally frequent either of the two communal rooms where the HCL system is installed were classified as being in the “exposed to the HCL intervention” group. The remaining residents were not exposed to any intervention during the study period. Any changes/deviations in communal room usage during the study period by a resident were recorded by staff. There were no other changes in residents’ schedules during the course of the study.
Study Assessments and Procedures
Basic demographic data (age, height, weight, etc.), clinical status, and physical functioning were recorded at baseline and follow-up in a case report form.
Actigraphy
A consumer grade wrist-worn activity monitor, the Fitbit Alta HR (Fitbit Inc., San Francisco, CA, USA) was used to objectively measure sleep and activity during the 8-week study period. The devices were worn continuously (24 hr/day, removed for showering and for charging) over the course of the 8-week study period. The device was worn on the left wrist, and the nursing and care staff in the nursing home were given instructions to ensure that the device was worn continuously and in the correct manner. For each Fitbit device, a smart phone was provided to synchronize the data with the Fitbit dashboard. The nursing and care staff were responsible for charging the device and smartphone and for ensuring the Fitbit device was synced daily.
Structured behavioral observations
A study diary was used to record mood during the study period. Recordings were made by the nursing staff daily. A member of the research team instructed the clinical nurse manager on how to complete the study diary, who in turn instructed the nursing staff. Residents graded their mood score using a numerical rating scale (1 = low mood, 10 = excellent mood), with the assistance of the nursing staff. Staff graded the mood score for those with a more severe cognitive impairment. The diary was also used to document time spent in the communal rooms and to document any changes in diet, medication, and so on. Staff were not compensated for their involvement in the study.
Data Analysis
Data were analyzed at three time-points during the study period: Week 1 (W1)—baseline; Week 6 (W6)—post intervention; and Week 8 (W8)—follow-up. Activity and sleep data were extracted from the Fitbit dashboard and collated using Microsoft Office Excel. Sleep metrics extracted were total time in bed (in minutes) and total sleep time (in minutes) per 24-hour calendar day. Sleep efficiency was calculated by dividing the total sleep time by the total amount of time in bed. The weekly average for each sleep metric was calculated. For activity, daily step counts were calculated and the total weekly count was reported. Mood scores were extracted from the study diary and collated using Microsoft Office Excel, and the weekly average morning (AM) and afternoon (PM) mood score were calculated. Descriptive statistics (mean and standard deviation [SD]) were used to describe the group data. Inferential statistical tests were not appropriate due to the small sample size in this study.
Results
Ten residents (seven female, three male; age: 80.8 ± 6.6 years; height: 165.4 ± 11.1 cm; weight: 65.5 ± 18.1 kg) were enrolled in the study (six exposed to the intervention, four not exposed). One resident from the non-exposed group was hospitalized on a number of occasions during the study period and was therefore excluded from the analysis. A profile of each of the remaining study participants is detailed in the supplementary data file.
Group mean (SD) measures of sleep, activity, and mood at W1, W6, and W8 are presented in Table 2. In the residents exposed to the lighting intervention, there was no improvement observed in sleep metrics from W1 to W6. In those who were not exposed, there was a marginal improvement in measures of sleep from W1 to W6, and there was a further improvement at W8. Activity data are only presented for four participants in the exposed group as two were immobile. These data revealed a decline in mobility from W1 to W6; however, there was a substantial increase in activity levels from W6 to W8. A similar trend was observed in those not exposed to the lighting intervention. Morning mood scores were largely unchanged in the group exposed to the lighting intervention; however, a small decline in afternoon mood scores was observed from W1 to W6 and from W6 to W8. In the non-exposed group, a modest increase in morning mood scores was observed from W1 to W6; however, afternoon mood scores had decreased from W1 to W6. Individual participant data are presented in the supplementary data file.
Table 2.
Measures of Sleep, Activity, and Mood for the Exposed and Non-exposed Group at Week 1 (W1)—Baseline, Week 6 (W6)—Post Intervention, and Week 8 (W8)—Follow-Up.
| Exposed group |
Non-exposed group |
|||||
|---|---|---|---|---|---|---|
| Measurement Variable | W1 | W6 | W8 | W1 | W6 | W8 |
| Time in bed (min) | 571.7 (239.7) | 492.9 (79.7) | 512.1 (273.8) | 422.6 (178.5) | 430.6 (226.7) | 497.9 (363.5) |
| Total sleep time (min) | 522.9 (216.2) | 452.3 (79.1) | 475.2 (258.2) | 386.3 (161.8) | 395.4 (203.2) | 450.1 (321.3) |
| Sleep efficiency (%) | 92.2 (1.7) | 92.1 (3.9) | 93.3 (2.4) | 92.4 (5.9) | 93.1 (5.0) | 92.0 (5.0) |
| Total steps/week | 5,738.8 (6,855.9) | 4,643.8 (3,733.6) | 9,070.0 (14,148.1) | 12,877.7 (17,589.9) | 7,216.7 (9,774.6) | 16,581.0 (24,873.7) |
| Mood score AM | 6.3 (1.8) | 6.4 (0.8) | 5.7 (1.0) | 5.7 (2.3) | 6.2 (1.1) | 6.2 (1.1) |
| Mood score PM | 6.9 (1.8) | 6.5 (0.8) | 5.9 (1.0) | 6.9 (1.5) | 6.3 (1.1) | 6.3 (1.1) |
Discussion
This pilot study sought to evaluate the effects that a lighting intervention has on sleep, mood, and activity in older adults living in a nursing home. Overall, the results of this pilot study were inconclusive. Some participants responded positively to the lighting intervention, while others showed no change or a continued decline in the recorded measurements of activity, mood, and sleep.
For those participants who did show improvements in sleep, these changes were not maintained at follow-up, indicating that the lighting intervention needs to be continued for any long-standing effects. The inconclusive findings of this project are in line with previous work. Some research has shown positive outcomes following a lighting intervention on sleep in older adults living in a nursing home environment (Ancoli-Israel et al., 2003; Fetveit & Bjorvatn, 2005; Fetveit et al., 2003; Fontana Gasio et al., 2003). Others however have shown no positive effect following a lighting intervention (Ancoli-Israel et al., 2002; Dowling et al., 2005).
To the authors’ knowledge this is the first report to examine the impact of a lighting intervention on the activity levels of residents in a nursing home. In the group of residents exposed to the lighting intervention, four of these were mobile at baseline, and were instrumented with a Fitbit device during the study period. However, only two out of these four residents showed an increase in activity levels from W1 baseline to the W6 post intervention follow-up. These improvements in activity were not maintained once the lighting intervention was complete, indicating that continuous light therapy may be required to produce long-lasting effects in those that respond.
There are several possible explanations as to why this study produced some conflicting results. First, this study enrolled a heterogeneous group of residents who had a variety of different conditions and comorbidities. This research did not take into account these variations in a person. A high proportion of participants in this study had ADRD, and there are some factors associated with this condition which may have caused them to respond in different ways to the lighting intervention. We did not use the mini-mental-state-examination to evaluate dementia severity; however, the level of dementia in some participants may have been more severe than others causing them to respond differently. In addition, no distinction was made between participants who had Alzheimer’s disease and those with other types of dementia. Previous research has shown that 2 weeks of morning bright exposure decreases nighttime activity in patients with vascular dementia but not in those who had Alzheimer’s disease (Mishima et al., 1998). This study should be replicated in this setting in a more homogeneous group of older adults.
In this study the lighting intervention was delivered in two communal rooms in the nursing home; however, light exposure was not tailored to the individual. Residents were free to come and go from the communal rooms as they wished. In addition residents, particularly those with ADRD, have a tendency to wander away or fall asleep during the day in the communal room. Therefore, exposure to the lighting intervention was not consistent over the course of the study. This is consistent with others who have reported similar difficulties administering lighting interventions in a nursing home setting (Ancoli-Israel et al., 2002).
A limitation of this study was the device used to measure sleep and activity. The Fitbit Alta HR was the device selected as it was readily available, and is a relatively inexpensive consumer device. The device reported sleep periods per calendar day. Total sleep time per calendar day was then calculated with no distinction made between daytime and nighttime sleep. Future work should look at classifying between periods of daytime and nighttime sleep. The cohort in this study exhibited low levels of activity and typically slow walking speeds. Only seven of the residents were able to mobilize, with many requiring the assistance of staff or a walking aid to walk. Giuliani et al. (2008) reported 0.41 m/s as the average gait speed of older adults living in residential care. At low gait speeds, the accelerations produced at the wrist during gait may not be large enough to be detected with a wrist-worn accelerometer, and therefore the number of steps could be underestimated. Previous work has shown that an ankle-worn accelerometer is the most accurate at measuring steps in slow-walking older adults and others with impaired mobility (Fulk et al., 2014; Sandroff et al., 2014; Simpson et al., 2015). However, for usability reasons a wrist-worn device is more favorable.
Conclusion
This is the first research to our knowledge to be conducted in an Irish setting to examine the impact of a cycled lighting intervention on older adults living in a nursing home. Although the results are inconclusive, a lighting intervention remains a potentially promising intervention in the nursing home setting. Further studies with more robust measurements and a more homogeneous cohort are required to investigate this further.
Supplemental Material
Supplemental material, Supplementary_data for The Impact of a Cycled Lighting Intervention on Nursing Home Residents: A Pilot Study by Oonagh M. Giggins, Julie Doyle, Ken Hogan and Mable George in Gerontology and Geriatric Medicine
Acknowledgments
This project would not have been possible without the tremendous support and cooperation of the residents, families, staff, and management of Sonas Ard na Greine Nursing home. A particular thank you is extended to the residents who participated in the study and to the entire Sonas Ard na Greine team who actively engaged when the study was taking place. The authors also wish to acknowledge Des Mulligan, who was involved in the setting up of the Quality of life Committee in Sonas Ard na Greine and who was instrumental in getting the HCL (Human Centric Lighting) system installed in the nursing home.
Footnotes
IRB Protocol/Human Subjects Approval: This study was reviewed and approved by the School of Health and Science Ethics Committee in Dundalk Institute of Technology, Dundalk, Ireland.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Glamox Ireland Limited supplied the HCL (Human Centric Lighting) system used in the study to the nursing home; however, the company had no other involvement in the study.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work has been funded by the EU’s INTERREG VA program, managed by the Special EU Programs Body (SEUPB).
ORCID iD: Oonagh M. Giggins  https://orcid.org/0000-0001-7748-5446
https://orcid.org/0000-0001-7748-5446
Supplemental Material: Supplemental material for this article is available online.
References
- Ancoli-Israel S., Gehrman P., Martin J. L., Shochat T., Marler M., Corey-Bloom J., Levi L. (2003). Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behavioral Sleep Medicine, 1(1), 22–36. 10.1207/S15402010BSM0101_4 [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S., Martin J. L., Kripke D. F., Marler M., Klauber M. R. (2002). Effect of light treatment on sleep and circadian rhythms in demented nursing home patients. Journal of the American Geriatrics Society, 50(2), 282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brainard G. C., Sliney D., Hanifin J. P., Glickman G., Byrne B., Greeson J. M., . . . Rollag M. D. (2008). Sensitivity of the human circadian system to short-wavelength (420-nm) light. Journal of Biological Rhythms, 23(5), 379–386. 10.1177/0748730408323089 [DOI] [PubMed] [Google Scholar]
- Dowling G. A., Hubbard E. M., Mastick J., Luxenberg J. S., Burr R. L., Van Someren E. J. W. (2005). Effect of morning bright light treatment for rest-activity disruption in institutionalized patients with severe Alzheimer’s disease. International Psychogeriatrics, 17(2), 221–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy J. F., Kronauer R. E., Czeisler C. A. (1996). Phase-shifting human circadian rhythms: Influence of sleep timing, social contact and light exposure. The Journal of Physiology, 495(Pt. 1), 289–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engwall M., Fridh I., Jutengren G., Bergbom I., Sterner A., Lindahl B. (2017). The effect of cycled lighting in the intensive care unit on sleep, activity and physiological parameters: A pilot study. Intensive & Critical Care Nursing, 41, 26–32. 10.1016/j.iccn.2017.01.009 [DOI] [PubMed] [Google Scholar]
- Fetveit A., Bjorvatn B. (2005). Bright-light treatment reduces actigraphic-measured daytime sleep in nursing home patients with dementia: A pilot study. The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry, 13(5), 420–423. 10.1176/appi.ajgp.13.5.420 [DOI] [PubMed] [Google Scholar]
- Fetveit A., Skjerve A., Bjorvatn B. (2003). Bright light treatment improves sleep in institutionalised elderly—an open trial. International Journal of Geriatric Psychiatry, 18(6), 520–526. 10.1002/gps.852 [DOI] [PubMed] [Google Scholar]
- Figueiro M. G. (2008). A proposed 24 h lighting scheme for older adults. Lighting Research & Technology, 40(2), 153–160. 10.1177/1477153507087299 [DOI] [Google Scholar]
- Figueiro M. G., Hunter C. M., Higgins P. A., Hornick T. R., Jones G. E., Plitnick B., . . . Rea M. S. (2015). Tailored lighting intervention for persons with dementia and caregivers living at home. Sleep Health, 1, 322–330. 10.1016/j.sleh.2015.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueiro M. G., Plitnick B. A., Lok A., Jones G. E., Higgins P., Hornick T. R., Rea M. S. (2014). Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clinical Interventions in Aging, 9, 1527–1537. 10.2147/CIA.S68557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontana Gasio P., Krauchi K., Cajochen C., Someren E., van Amrhein I., Pache M., . . . Wirz-Justice A. (2003). Dawn-dusk simulation light therapy of disturbed circadian rest-activity cycles in demented elderly. Experimental Gerontology, 38(1–2), 207–216. [DOI] [PubMed] [Google Scholar]
- Fulk G. D., Combs S. A., Danks K. A., Nirider C. D., Raja B., Reisman D. S. (2014). Accuracy of 2 activity monitors in detecting steps in people with stroke and traumatic brain injury. Physical Therapy, 94(2), 222–229. 10.2522/ptj.20120525 [DOI] [PubMed] [Google Scholar]
- Giuliani C. A., Gruber-Baldini A. L., Park N. S., Schrodt L. A., Rokoske F., Sloane P. D., Zimmerman S. (2008). Physical performance characteristics of assisted living residents and risk for adverse health outcomes. The Gerontologist, 48(2), 203–212. 10.1093/geront/48.2.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood S., Amir S. (2017). The aging clock: Circadian rhythms and later life. The Journal of Clinical Investigation, 127(2), 437–446. 10.1172/JCI90328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurry S. M., Pike K. C., Vitiello M. V., Logsdon R. G., Larson E. B., Teri L. (2011). Increasing walking and bright light exposure to improve sleep in community-dwelling persons with Alzheimer’s disease: Results of a randomized, controlled trial. Journal of the American Geriatrics Society, 59(8), 1393–1402. 10.1111/j.1532-5415.2011.03519.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishima K., Hishikawa Y., Okawa M. (1998). Randomized, dim light controlled, crossover test of morning bright light therapy for rest-activity rhythm disorders in patients with vascular dementia and dementia of Alzheimer’s type. Chronobiology International, 15(6), 647–654. [DOI] [PubMed] [Google Scholar]
- Prinz P. N., Christie C., Smallwood R., Vitaliano P., Bokan J., Vitiello M. V., Martin D. (1984). Circadian temperature variation in healthy aged and in Alzheimer’s disease. Journal of Gerontology, 39(1), 30–35. [DOI] [PubMed] [Google Scholar]
- Sandroff B. M., Motl R. W., Pilutti L. A., Learmonth Y. C., Ensari I., Dlugonski D., . . . Riskin B. J. (2014). Accuracy of StepWatch and ActiGraph accelerometers for measuring steps taken among persons with multiple sclerosis. PLOS ONE, 9(4), e93511 10.1371/journal.pone.0093511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schibler U., Sassone-Corsi P. (2002). A web of circadian pacemakers. Cell, 111(7), 919–922. [DOI] [PubMed] [Google Scholar]
- Simpson L. A., Eng J. J., Klassen T. D., Lim S. B., Louie D. R., Parappilly B., . . . Zbogar D. (2015). Capturing step counts at slow walking speeds in older adults: Comparison of ankle and waist placement of measuring device. Journal of Rehabilitation Medicine, 47(9), 830–835. 10.2340/16501977-1993 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_data for The Impact of a Cycled Lighting Intervention on Nursing Home Residents: A Pilot Study by Oonagh M. Giggins, Julie Doyle, Ken Hogan and Mable George in Gerontology and Geriatric Medicine


