Abstract
Background:
Adolescent athletes who sustain an anterior cruciate ligament (ACL) tear have significantly reduced activity levels during recovery. Activity level is linked to body mass index (BMI); however, it is unclear how recovery from an ACL reconstruction (ACLR) affects relative BMI and whether these changes persist after return to activity.
Hypothesis:
Patients’ BMI percentile will significantly increase after ACLR, but will trend toward baseline after return to activity.
Study Design:
Cross-sectional study.
Level of Evidence:
Level 3.
Methods:
A retrospective review of 666 pediatric and adolescent patients who underwent ACLR was performed. Body mass was assessed by evaluating change in BMI percentile at 8 standard-of-care time windows relative to BMI percentile at time of surgery. Linear regression and bivariate and multivariate analyses were used to assess the effect of time window and other demographic factors on the change in BMI percentile. These analyses were rerun after dividing patients by clinical obesity categorization (underweight, normal, overweight, or obese) at time of surgery to assess the effect of preinjury body mass levels.
Results:
BMI percentile of all BMI categories tended to increase postoperatively, peaking 6 to 9 months after surgery, with a median increase of 1.83 percentile points. After this peak, BMI approached baseline but remained elevated at 0.95 percentile points 2 years postoperatively. Beginning 3 months after surgery, the normal-weight group had significantly larger changes in BMI percentile at each time window, peaking at 4.15 points above baseline at 9 months. This BMI increase among normal-weight patients persisted in the second postoperative year, with a median percentile increase of 2.63 points.
Conclusion:
Pediatric and adolescent patients, especially those with a normal BMI, undergo significant changes to their BMI during recovery from ACLR.
Clinical Relevance:
Patients’ failure to return to their presurgical BMI percentile 2 years postoperatively suggests that ACLR may have long-reaching and often unappreciated effects on body mass.
Keywords: anterior cruciate ligament (ACL), body mass index (BMI), rehabilitation, weight gain
Anterior cruciate ligament (ACL) tears are increasingly common in pediatric patients, given the rise in competitive youth sports participation and early sports specialization.4,5,8,12,18 While several courses of treatment exist, recent literature has favored early surgical intervention to prevent longer-term consequences, such as osteoarthritis.2,10,11,17,22,23,26 Although outcomes from ACL reconstruction (ACLR) are usually positive, patients undergoing this surgery face a lengthy recovery process.1,10,17,23,24 Most patients return to full activity in the long run, but rehabilitation typically entails a dramatic decrease in activity levels for about 12 weeks after surgery.7,11,15,22 This is followed by a slow increase in activity levels, with a gradual release to activity beginning at 6 to 9 months postreconstruction.7,11,20,22 The rehabilitation period for ACLR does involve significant physical therapy and strengthening work, but given that this injury often occurs in athletic individuals, many patients face a large disparity between pre- and postoperative activity levels.5,6,12
Weight and body mass index (BMI) are influenced by many intrinsic and extrinsic factors, including activity level, and increased BMI can have long-term health implications, such as heart disease and higher rates of musculoskeletal injuries.9,25,27,30 Studies comparing inactive and physically active youth have shown the latter to have higher fitness levels and lower BMI, among other health advantages.9,16,21,27 Given this lower typical baseline activity level, it is likely that overweight and obese youth who suffer an ACL rupture may face only minimal changes to their activity level during the intense rehabilitation period when compared with the highly active youth who frequently endure ACL injuries.9,16,21,27
Despite these acknowledged changes in activity level, it is unclear how recovery from an ACLR affects BMI and whether these changes persist after return to activity. In addition, no study has examined the role of a patient’s initial BMI in predicting the change in weight or BMI after such a surgery. This study seeks to describe the postoperative changes in BMI at each stage of the rehabilitation process for pediatric and adolescent patients recovering from ACL surgery with particular emphasis on the influence of initial BMI and obesity categorization on these changes.
Methods
After institutional review board approval, a retrospective review of adolescent patients between the ages of 8 and 18 years who underwent ACL surgery between 2009 and 2016 at a large tertiary referral pediatric sports medicine center was performed. Out of 1117 potential participants, a total of 666 patients were included in the final analysis. There were 451 patients excluded from analysis based on the following criteria: no date of injury reported, 3 months or more between reported date of injury and surgery, second orthopaedic surgery within 3 months of initial surgery, maximum follow-up date less than 6 months from surgery, evident initial BMI calculation error, or no calculated BMI percentile on the day of surgery. Additional patient observations were excluded if they came subsequent to a second knee surgery. The data were then divided into 8 time windows from time of surgery until 2 years after surgery based on standard-of-care follow-up intervals (day of surgery, 2 weeks, 3 months, 6 months, 9 months, 1 year, and 2 years). Each patient was permitted only 1 observation per time window, which was selected by choosing the individual appointment with closest to optimal time-since-surgery for that follow-up time point. BMI percentile was used to account for normal changes in BMI during growth, and change in BMI percentile relative to initial BMI at the time of surgery was calculated for each observation. Finally, 10% (top 5% and bottom 5%) of the observations were trimmed based on change in BMI percentile since surgery to account for outliers and spurious data points.
A Shapiro-Wilk test indicated that the data were not normally distributed at almost any time window, and as such, nonparametric tests were used throughout for successive bivariate and multivariate analyses of potential confounding factors. Nonparametric tests and conventions were used for the time windows with nonsignificant Shapiro-Wilk tests to maintain consistency in data portrayal.
Mann-Whitney U tests were used to assess the dichotomous variables: sex, Medicaid status, and subsequent knee surgery on record. A Spearman correlation was used to evaluate the influence of age. A Kruskal-Wallis test was used to evaluate the influence of obesity categorization and race at each time window. Obesity categorizations were assigned based on Centers for Disease Control and Prevention guidelines for BMI percentiles: less than the 5th percentile were categorized as underweight, 5th to less than the 85th percentile were categorized as normal weight, 85th to less than 95th percentile were considered overweight, and 95th percentile and above were categorized as obese.3 A Kruskal-Wallis test was used to evaluate the influence of time window on change in BMI percentile for the entire data set.
To analyze the change in BMI percentile over time, median and interquartile ranges were calculated for change in BMI percentile at each time window for the overall data set. In addition, given that the linear regression analysis indicated obesity categorization as a significant factor in change in BMI percentile, all statistical tests were repeated after subdividing the data set by obesity categorization at the time of surgery. Underweight patients were excluded from this analysis due to their small sample size (22 total observations in all time windows).
Finally, linear regression of change in BMI percentile based on time window, obesity categorization, and the other demographics listed above was performed to assess the role of each factor. Statistical significance was defined at the level of P < 0.05. All analyses were computed using Stata 14 (College Station, TX).
Results
A total of 2911 observations were available from 666 patients. Patients ranged in age from 8 to 18 years at the time of surgery, with an average age of 15.1 years (interquartile range [IQR], 13.8-16.5 years). The median time between injury and surgery was 47 days, or 1.6 months (Table 1). The median height, weight, and BMI at time of surgery were 166 cm, 62 kg, and 22, respectively (Table 1). BMI percentile at time of surgery ranged from 1.5% to 99.8%, with a median percentile of 74.7% (IQR: 53.1%-89.1%). Of the 666 analyzed patients, 48% were male and 52% were female (Table 1). At the time of surgical reconstruction, 1% of patients were underweight, 66% had a normal BMI, 20% were overweight, and 14% were obese. Almost three quarters (73%) of the patients were white, 17.6% black or African American, and 10% of another race (Table 1).
Table 1.
Patient demographics: patient characteristics at time of surgery
| Percentage of Population | Median (IQR) | |
|---|---|---|
| Age, y | — | 15.1 (13.8-16.5) |
| Injury to surgery, mo | — | 1.6 (1.2-2.0) |
| Height, cm | — | 166 (159-173) |
| Weight, kg | — | 62.0 (53.0-72.0) |
| BMI, kg/m2 | — | 22.0 (19.9-24.6) |
| BMI percentile, % | — | 74.7 (53.1-89.1) |
| Sex | ||
| Male | 48.05 | — |
| Female | 51.95 | — |
| Initial BMI | ||
| Underweight | 0.60 | — |
| Normal BMI (485) | 65.77 | — |
| Overweight (149) | 19.97 | — |
| Obese (100) | 13.66 | — |
| Race | ||
| Asian/Pacific Islander | 2.3 | — |
| Black/African American | 17.6 | — |
| Hispanic or Latino | 0.8 | — |
| White | 73.0 | — |
| Other/none specified | 6.5 | — |
BMI, body mass index; IQR, interquartile range; —, not applicable.
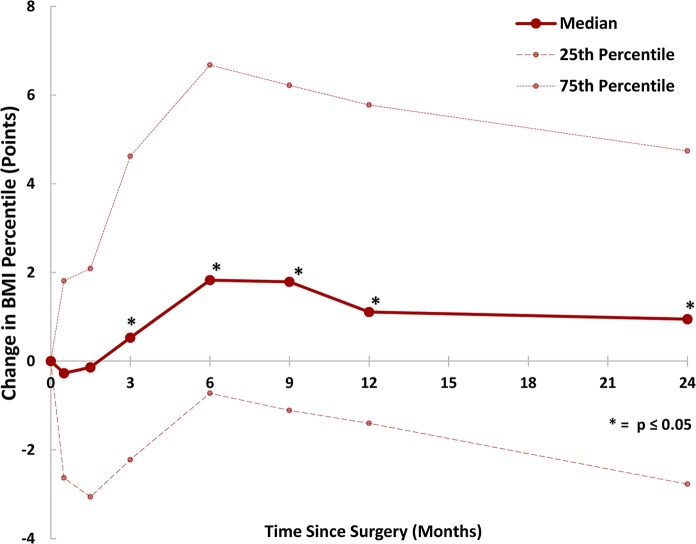
Patients showed minor BMI percentile decreases in the 6 weeks immediately after surgery, though these changes were not statistically significant with P values of 0.241 and 0.282 for the 2-week and 6-week follow-up windows, respectively. Beginning at 3 months, patients tended to increase their BMI percentile, peaking at 6 months after surgery with a median increase of 1.83 percentile points (IQR, −0.72 to 6.68). BMI trended back toward baseline after 9 months of rehabilitation. However, this trend flattened, and the BMI remained elevated in the long term with a median increase of 0.95 percentile points since surgery (IQR: −2.77 to 4.74). These data, along with medians and interquartile ranges, are presented in Figure 1 and Table 2. A Kruskal-Wallis test for BMI percentile by time window was significant (P < 0.01). Evaluation via linear regression analysis resulted in an R2 of 0.079 (P < 0.01), indicating good model fit. All time windows starting at the 3-month follow-up were statistically significant predictors of change in BMI percentile in the regression model (P < 0.01).
Figure 1.
Change in body mass index (BMI) percentile from date of surgery. The median and interquartile range for change in BMI percentile, measured in percentile points, from date of surgery to date of respective follow-up time window. These data are depicted numerically in Table 2.
Table 2.
Change in BMI percentile in all patients a
| Median (IQR) | ||||
|---|---|---|---|---|
| Overall | Normal | Overweight | Obese | |
| 2 wk | −0.27 (–2.63 to 1.18) | −0.37 (–4.18 to 3.09) | −0.52 (–1.64 to 0.42) | −0.16 (–0.59 to 0) |
| 6 wk | −0.14 (–3.06 to 2.09) | −0.15 (–4.44 to 3.41) | −0.51 (–1.47 to 0.62) | 0 (–0.23 to 0.18) |
| 3 mo | 0.53 (–2.22 to 4.62) | 2.06 (–3.85 to 6.61) | 0.17 (–1.45 to 2.67) | 0.18 (–0.25 to 0.53) |
| 6 mo | 1.83 (–0.72 to 6.68) | 3.7 (–1.04 to 8.38) | 1.83 (–0.78 to 3.19) | 0.11 (–0.25 to 0.55) |
| 9 mo | 1.79 (–1.11 to 6.22) | 4.15 (–1.27 to 9.12) | 1.65 (–1.66 to 3.11) | 0.27 (–0.39 to 0.92) |
| 1 y | 1.11 (–1.40 to 5.78) | 2.89 (–1.99 to 8.14) | 1.13 (–2.33 to 2.86) | 0.22 (–0.54 to 0.87) |
| 2 y | 0.95 (–2.77 to 4.74) | 2.63 (–2.98 to 7.57) | 1.06 (–2.06 to 3.46) | 0.09 (–1.04 to 1.33) |
BMI, body mass index; IQR, interquartile range.
The table presents median and IQR for change in BMI percentile compared with BMI at time of surgery for the overall data set and each BMI cohort (normal weight, overweight, and obese). The change in BMI percentile for the overall data set is depicted in Figure 1, and the change by obesity categorization is depicted in Figure 2.
Using bivariate and linear regression analysis, no consistent associations for BMI percentile were seen relative to sex, age, Medicaid status, or subsequent knee surgery. However, Kruskal-Wallis analysis for obesity categorization was significant (P < 0.05) at the 3-month, 6-month, 9-month, and 1-year time windows, showing that normal-weight patients had larger positive changes in BMI percentile at these follow-up time windows.
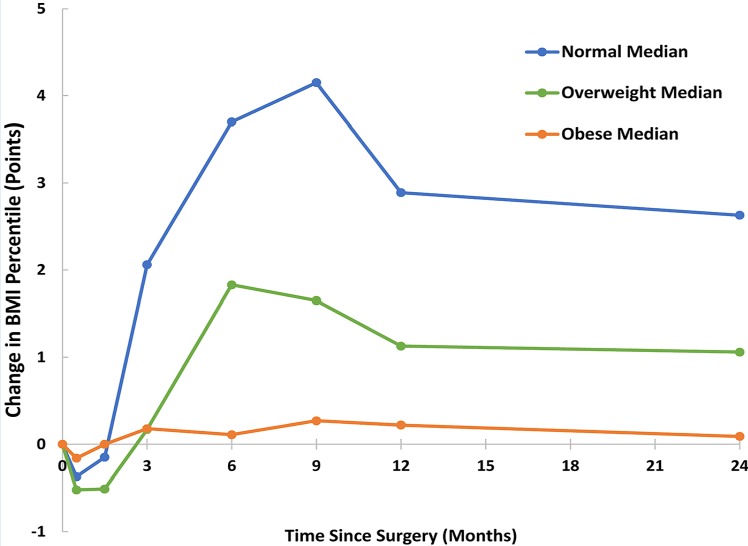
The data set was further divided into underweight, normal, overweight, and obese categories (Figure 2). All groups had similar, small decreases in BMI percentile in the 6 weeks immediately after surgery, though these decreases were not statistically significant according to linear regression analysis. Beginning 3 months after surgery, the normal weight group had significantly larger changes in BMI percentile at each time window. The normal weight group peaked with a median percentile increase of 4.15 points at 9 months after surgery (IQR, −1.27 to 9.12). As in the overall data set, the average BMI percentile for normal-weight patients decreased from its maximum at 9 months postoperatively but remained elevated even out to the second year after the operation, with a median percentile increase of 2.63 points since surgery (IQR, −2.98 to 7.57). The overweight group had a maximum increase of 1.83 percentile points 6 months after surgery (IQR, −0.78 to 3.19). The obese group had the smallest changes in BMI percentile in nearly every time window, with a maximum median BMI-percentile increase of 0.27 points 9 months after surgery (IQR, −0.39 to 0.92). At the 2-year time window, 28 patients had increased their obesity classification (ie, normal to overweight), and 11 patients had decreased their classification. When the data set was stratified by race, it was found that white, normal-weight patients had the largest change in BMI percentile of any subgroup, with an increase of 4.59 percentile points 9 months after surgery (IQR, −1.06 to 9.41), though race was not significant in the regression model or multivariate analyses.
Figure 2.
Change in body mass index (BMI) percentile from date of surgery based on initial obesity categorization. The median change in BMI percentile by obesity categorization, measured in percentile points, from date of surgery to date of respective follow-up time window. These data are depicted numerically in Table 2.
Discussion
The main findings of this study highlight another long-term consequence that pediatric and adolescent patients face as a result of their injury: a significant unfavorable change in BMI percentile. While the overall study population faced a maximum BMI-percentile increase of almost 2 points and a longer term increase of nearly 1 point, the most dramatic changes occurred in normal-weight patients. Patients in the normal-weight category gained more than 4 percentile points on average, with an upper quartile limit of over 9 points. Their initial change in relative body mass is not surprising given the expected change in activity levels. However, the observation that patients failed to return to their prior BMI percentile and maintained a 2.5-point BMI percentile elevation even 2 years out from reconstruction raises concern about significant long-term health-related issues for these patients. These findings indicate that rehabilitation programs for ACL reconstruction and related procedures may need to extend their focus beyond strengthening the knee to address significant and persistent lifestyle changes that result from such injuries.
The results in this study closely resemble those from Myer et al19 who reported a 4 BMI percentile-point increase for postoperative adolescent female soccer and basketball athletes in the year after their ACL injury. The study by Myer et al19 followed a cohort of 352 female athletes with at least 1-year follow-up evaluations of BMI and body fat percentage. During the study period, 71 athletes reported an ACL injury in the year since their last evaluation. These injured athletes had a maximum BMI increase of 3.9 percentile points at 1-year postreconstruction, which is closely in line with our findings of 2.89 to 4.15 points during the 9-month to 1-year postreconstruction period. The study by Meyer et al,19 however, was limited in its ability to assess the long-term impact of the ACL injury on BMI in these athletes, given the wide follow-up windows and low compliance, with only 31 of 71 patients returning for their 1-year assessment, and only 11 for the 2-year visit.
With 666 patients, the large cohort of patients presented in this study allowed broader assessment of a host of additional factors that may contribute to the change in BMI percentile over time. While sex, insurance status, and requirement for a second ACLR surgery did not appear to relate to a change in BMI over time, the starting BMI was correlated with differences in the change in BMI over time. Patients with a normal BMI at the time of surgery had the largest relative weight gains, while obese patients had the smallest gains over time. This significant difference in physiological responses between obesity categorizations may be due to varying activity levels before surgery for each group, as overweight and obese patients tend to have lower activity levels than average-weight patients.9,16,21,27 Thus, the change in activity level may be less extreme for initially overweight patients relative to their initially normal-weight counterparts.
Among the normal-weight patients in this study, the maximum gain of 4.15 BMI percentile points occurred after several months of limited-to-no physical activity. The change in BMI percentile did appear to decrease starting at about 9 months after surgery, with the 1-year follow-up change decreasing to only 2.89 BMI percentile points. However, this change seemed to stabilize in the second year after surgery with an average change in BMI percentile of 2.63 points. This demonstrates that while they do trend back toward their baseline BMI later in recovery, perhaps due to a resumption of normal activity, normal-BMI patients may face persistent, unfavorable changes in body mass extending beyond their rehabilitation period.
As this study lacks a true uninjured control group, percentiles from national trends, cohorts from literature, and internal controls were used as requisite comparison groups. The National Center for Health Statistics reports a trend of increasing prevalence of obesity in pediatric and adolescent populations as they age. In a 2015-2016 survey, 20.6% of 12- to 19-year-olds were obese, compared with only 18.4% of 6- to 11-year-olds.13 This suggests that the postoperative BMI increases noted in this study could be attributed not merely to the rehabilitation period but rather a wider trend of adolescent BMI increase consistent with the general population. While BMI may increase throughout adolescence, the use of a BMI percentile allows for comparison of individuals with their peer group over time. The Centers for Disease Control and Prevention incorporates these epidemiological trends into the calculation of BMI percentile, in effect, using the general population as a built-in control group. Additionally, the study by Myer et al19 mentioned above noted that their control group of uninjured athletes maintained the same BMI percentile over time, with subtle variable increases and decreases from year to year. In addition to comparison with national trends and the literature, the division of patients into obesity categorization allowed for an internal control. While the obese group still struggled with a significant knee injury, it was hypothesized that given the lower baseline activity levels of this group, pre- and postreconstructive activity levels would be similar and result in minimal changes to BMI percentile. Indeed, the obese group saw a maximum increase of only 0.27 percentile points 9 months after surgery. While this study lacks a true uninjured control group, its results remain significant against the backdrop of related uninjured control groups, national trends, and internal controls.
This study adds to the growing body of literature showing that knee injuries can have lasting health effects on adolescent athletes. These data demonstrate that young, normal-weight patients do not return to the same baseline BMI percentiles after an ACL injury. While they peak at a BMI increase of over 4 percentile points, they are only able to recover less than half of this weight gain more than a year later. These enduring changes to BMI percentile, paired with a significantly increased risk of knee arthritis later in life, may point to more serious long-term consequences on overall health.2,26 An analysis of data from a British 1946 cohort study28 noted that having a high BMI as a young adult was associated with higher mortality as an adult. While many of the other long-term consequences of an ACL injury, such as the development of arthritis, are inevitable, it would seem that this resulting increase in BMI may be preventable. Much of the increase in BMI may be due to patients’ continuing to eat as if they were an athlete in training for their sport and to their reduced activity levels failing to support the same level of consumption. Once weight is added, it can be exceedingly difficult to shed. Thus, it would seem that this effect might be modifiable with dietary counseling for postsurgical activity levels. These data suggest that this intervention should occur at about the 6-week mark postoperatively to blunt the marked BMI increase noted from 6 weeks to 3 months postreconstruction. In addition to nutritional guidance, future research on rehabilitation programs should also address potential psychosocial factors that may influence physiological health after ACLR, given the changes in lifestyle and social interaction many patients face.
In addition to the lack of a true control discussed above, this study has several limitations because of its retrospective nature. Most notably, few patients precisely met the recommended follow-up times, creating variation in the number of total follow-up visits and precise follow-up time within each window. In addition, height and weight were subject to human error with a number of different centers and individuals recording these measurements. The retrospective nature also prevented a more individualized approach to outliers and spurious data, which were excluded. Nevertheless, the quality of the data is likely comparable with data that would be obtained by a prospective study specifically designed to answer this clinical question. Another weakness is that the data set contained no information regarding activity level before or after surgery. While this could provide evidence for or against the hypothesis that the difference between obesity categories is due to varying activity levels, it does not negate the legitimacy of the observation. A final limitation of this analysis lies in the use of BMI percentile and obesity categorizations as a proxy for body composition, as studies have shown that BMI is limited in its ability to assess body composition and identify adolescents with cardiovascular health risks.14,29 In addition, obesity is characterized by a gradient rather than a set of strict categories, and it is possible that different divisors for these categorizations could lead to different analytical results. Despite these limitations, this study nevertheless analyzed a large data set with a final sample size of well over 600 patients, and the results illustrate a significant, lasting change in BMI percentile after reconstructive ACL surgery for all patients, with a particularly dramatic effect in normal-weight patients.
Conclusion
These significant, undesired changes to BMI after ACLR demonstrate that rehabilitation concerns after surgery should extend beyond merely rebuilding strength in the knee. Excess and prolonged weight gain should be more carefully monitored in the recovery process. In addition, early education and a revised rehabilitation program that includes greater focus on managing broader changes to lifestyle may help ACL patients minimize the long-term negative effects of weight gain that may accompany rehabilitation from ACL surgery.
Footnotes
The following author declared potential conflicts of interest: J.T.R.L. receives royalties for a patent for a distal radial fracture reduction educational materials copyright, which are paid to Sawbones Inc.
References
- 1. Aichroth PM, Patel DV, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. J Bone Joint Surg Br. 2002;84:38-41. [DOI] [PubMed] [Google Scholar]
- 2. Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42:1049-1057. [DOI] [PubMed] [Google Scholar]
- 3. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164-S192. [DOI] [PubMed] [Google Scholar]
- 4. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139:e20161877. [DOI] [PubMed] [Google Scholar]
- 5. Caine D, Purcell L, Maffulli N. The child and adolescent athlete: a review of three potentially serious injuries. BMC Sports Sci Med Rehabil. 2014;6:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Sports-related injuries among high school athletes—United States, 2005-06 school year. MMWR Morb Mortal Wkly Rep. 2006;55:1037-1040. [PubMed] [Google Scholar]
- 7. Dekker TJ, Rush JK, Schmitz MR. What’s new in pediatric and adolescent anterior cruciate ligament injuries? J Pediatr Orthop. 2018;38:185-192. [DOI] [PubMed] [Google Scholar]
- 8. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675-680. [DOI] [PubMed] [Google Scholar]
- 9. Drake KM, Beach ML, Longacre MR, et al. Influence of sports, physical education, and active commuting to school on adolescent weight status. Pediatrics. 2012;130:e296-e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fabricant PD, Jones KJ, Delos D, et al. Reconstruction of the anterior cruciate ligament in the skeletally immature athlete: a review of current concepts: AAOS exhibit selection. J Bone Joint Surg Am. 2013;95:e28. [DOI] [PubMed] [Google Scholar]
- 11. Fabricant PD, Kocher MS. Anterior cruciate ligament injuries in children and adolescents. Orthop Clin. 2016;47:777-788. [DOI] [PubMed] [Google Scholar]
- 12. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44:2716-2723. [DOI] [PubMed] [Google Scholar]
- 13. Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017;288:1-8. [PubMed] [Google Scholar]
- 14. Javed A, Jumean M, Murad MH, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr Obes. 2015;10:234-244. [DOI] [PubMed] [Google Scholar]
- 15. Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:1019-1036. [DOI] [PubMed] [Google Scholar]
- 16. Lambourne K, Donnelly JE. The role of physical activity in pediatric obesity. Pediatr Clin North Am. 2011;58:1481-1491. [DOI] [PubMed] [Google Scholar]
- 17. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582-2587. [DOI] [PubMed] [Google Scholar]
- 18. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363-2370. [DOI] [PubMed] [Google Scholar]
- 19. Myer GD, Faigenbaum AD, Foss KB, et al. Injury initiates unfavourable weight gain and obesity markers in youth. Br J Sports Med. 2014;48:1477-1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Phillips JA, Young DR. Past-year sports participation, current physical activity, and fitness in urban adolescent girls. J Phys Act Health. 2009;6:105-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Purcell L, Micheli LJ. Current pediatric and adolescent sports medicine: an overview. In: Micheli LJ, Purcell L, eds. The Adolescent Athlete: A Practical Approach. New York, NY: Springer; 2018:1-7. [Google Scholar]
- 23. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42:2769-2776. [DOI] [PubMed] [Google Scholar]
- 24. Risberg MA, Lewek M, Snyder-Mackler L. A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Phys Ther Sport. 2004;5:125-145. [Google Scholar]
- 25. Ruiz JR, Castro-Piñero J, Artero EG, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med. 2009;43:909-923. [DOI] [PubMed] [Google Scholar]
- 26. Shelbourne KD, Benner RW, Gray T. Results of anterior cruciate ligament reconstruction with patellar tendon autografts: objective factors associated with the development of osteoarthritis at 20 to 33 years after surgery. Am J Sports Med. 2017;45:2730-2738. [DOI] [PubMed] [Google Scholar]
- 27. Sirard JR, Pfeiffer KA, Dowda M, Pate RR. Race differences in activity, fitness, and BMI in female eighth graders categorized by sports participation status. Pediatr Exerc Sci. 2008;20:198-210. [DOI] [PubMed] [Google Scholar]
- 28. Strand BH, Kuh D, Shah I, Guralnik J, Hardy R. Childhood, adolescent and early adult body mass index in relation to adult mortality: results from the British 1946 birth cohort. J Epidemiol Community Health. 2012;66:225-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Telford RD, Telford RM, Welvaert M. BMI is a misleading proxy for adiposity in longitudinal studies with adolescent males: the Australian LOOK study. J Sci Med Sport. 2019;22:307-310. [DOI] [PubMed] [Google Scholar]
- 30. Yard E, Comstock D. Injury patterns by body mass index in US high school athletes. J Phys Act Health. 2011;8:182-191. [DOI] [PubMed] [Google Scholar]