Abstract
BACKGROUND: The effect of chemotherapy in metastatic bone sarcomas is poor and the condition is invariably fatal. Therefore, new treatment modalities are intensely needed. Pazopanib is a selective multitargeted tyrosine kinase inhibitor that has proven to be effective in the treatment of metastatic soft tissue sarcomas. The objective of this study was to evaluate the off-label use of pazopanib in patients with metastatic bone sarcomas who failed standard chemotherapy. METHODS: All patients with metastatic bone sarcomas treated with pazopanib between October 1st, 2011 and October 1st, 2017 at the Department of Oncology, Aarhus University Hospital were evaluated. Demographics, treatment, and survival outcomes were collected and analyzed. RESULTS: Nineteen patients were identified. The median age was 38 years (range 18–62). Most of the patients (50%) were diagnosed with osteosarcoma. All patients had documented disease progression at the time of initiating pazopanib treatment. The median overall survival was 11 months. Median progression free survival was 5.4 months. Out of 19 patients, 13 (68%) had either partial response or stable disease. In five patients, the dose of pazopanib was reduced because of toxicity. CONCLUSION: Off-label use of pazopanib is effective in the treatment of metastatic bone sarcomas of different histologies. Pazopanib was well tolerated in the treatment of patients with refractory bone sarcomas. Studies examining the effect of pazopanib alone or in combination with chemotherapy or other targeted therapies are needed.
Introduction
Bone sarcoma is a rare and heterogeneous group of mesenchymal cancers. Patients with advanced bone sarcoma have a poor prognosis, and less than 25% of these patients become long-term survivors [1]. Even though different treatment modalities have been tested, no standard regimen is recommended for second-line treatment of metastatic osteosarcoma [2]. Therefore, new treatment modalities are needed.
Pazopanib is a second-generation selective receptor tyrosine kinase inhibitor (TKI) with high affinity for vascular endothelial growth factor receptor (VEGFR), activity against platelet-derived growth factor receptor (PDGFR), against tyrosine-protein kinase kit (KIT) and a modest activity against fibroblast growth factor receptor (FGFR) [3]. Pazopanib is approved for second-line treatment in nonadipocytic soft tissue sarcoma after failure of standard chemotherapy [4]. This approval is based on the PALETTE study, a global, double blind, randomized, Phase 3 trial comparing the efficacy of pazopanib versus placebo for the treatment of metastatic STS. The result of the study was a prolonged PFS for patients treated with pazopanib (median 18 weeks) compared with placebo (median 6 weeks). In addition, the increased PFS for patients with soft tissue sarcoma treated with pazopanib did not compromise patient quality of life [5].
Investigation of tissue samples from osteosarcoma patients have shown that the vascular endothelial growth factor (VEGF) and the mitogen-activated protein kinase (MAPK) pathway are critical signaling pathway for the overall survival (OS) of these patients [6]. Also, the platelet-derived growth factor receptors (PDGFRs) [7,8] and the signal transduction pathways of phosphatidylinositol 3′-kinase/mammalian target of rapamycin (PI3K/mTOR) [9] play a role in the prognosis of osteosarcoma patients. For chondrosarcoma, different isoforms for VEGFR are involved in the tumor development [10]. Sorafenib is an orally active multikinase inhibitor that targets MAPK, VEGFRs, and PDGFRs, which has been demonstrated to be effective in patient with high-grade osteosarcoma after failure of standard treatments [[11], [12], [13]]. All these studies are small and investigate only a few patients.
A few case reports have demonstrated an effect of pazopanib in bone sarcoma. One study has investigated the effect on refractory Ewing sarcoma [14] and two other on metastatic osteosarcoma [15,16] both with promising results.
Treatment of bone sarcoma with pazopanib is an example for off-label use of an experimental drug which can be approved by the Danish Medical Council on doctors' request. In this article, we report our experience on treating metastatic bone sarcoma with pazopanib as an experimental drug.
Material and Method
Study Cohort
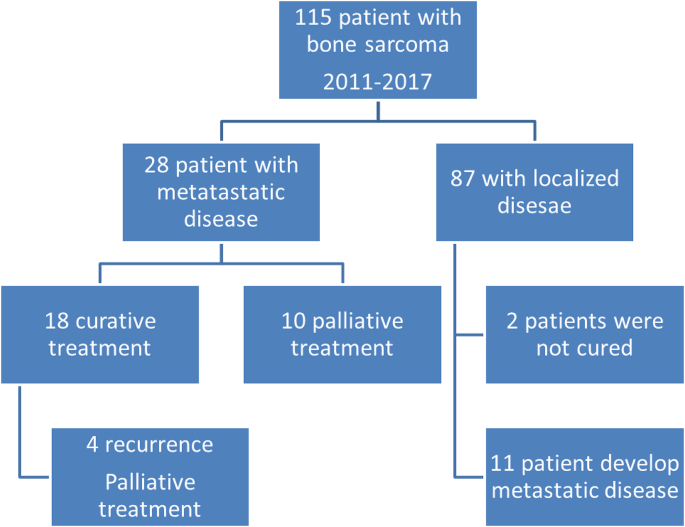
All patients diagnosed with bone sarcoma and treated with pazopanib for metastatic disease at Aarhus Sarcoma Centre were included in the study. The first patient was treated on October 1st, 2011, and the study period ended October 1st. 2017 to ensure a proper follow-up time for all patients included. Patients with extraskeletal bone sarcoma were excluded from the analysis. This resulted in a cohort of 21 patients. However, two patients were excluded because of death before pazopanib treatment was initiated. See Figure 1 for potential candidate for pazopanib treatment and reason for exclusion.
Figure 1.
A total of 27 patients could potentially have been treated with pazopanib in the study period. The total number of patients with bone sarcoma were identified in the national quality sarcoma database including all patient treated in Denmark. These data represent patient form one of the two sarcoma centres in Denmark. However, the reasons for not offering the patient pazopanib were as followed. Two patients died who before treatment were initiated. Three patients had giant cell histology and three chordoma patients were not considered.
Data Sources
Clinical data were obtained from the newly validated population-based Aarhus Sarcoma Registry (ASR) and the National Quality Sarcoma Database [17], which contains comprehensive clinical information on each sarcoma patient from 1979 to 2019.
Treatment
Patients were diagnosed and treated, according to national guidelines, by an experienced multidisciplinary sarcoma team. The decision of using off-label pazopanib was made by the consultant in charge of bone sarcoma treatment. The study drug was taken orally once daily. The patients were seen on day 10, at week 4, and every 12 weeks thereafter. Treatment continued until disease progression according to RECIST criteria, unacceptable toxic effects, or death. Twelve-lead electrocardiograms and a multigated acquisition (MUGA) scan were assessed before the start of treatment. Only grade 3 or 4 toxicities are reported in this study and no differentiation between grade 3 and 4 toxicities are made.
Data Analysis and Statistics
The primary endpoint was progression free survival (PFS) defined as time from start of pazopanib treatment to either disease progression or death from any cause. Patients alive at the time of analysis were censored. Secondary endpoint was OS. The study period ended October 1st, 2017. However, the patients were followed until February 1st, 2019. Patients alive at this date were censored. Descriptive data are presented and PFS is illustrated using a Kaplan–Meier plot. All statistical analyses were performed by using Stata version 15.
Ethics
The Ethics Committee of Denmark (1-10-72-233-12) and the Danish Agency of Data Protection (1-16-02-677-15) have approved the study.
Results
From October 2011 to October 2017, 19 patients from Aarhus Sarcoma Centre were treated with pazopanib for metastatic bone sarcoma. The median age at the beginning of pazopanib treatment was 39 years (range 18–62 year) and median duration between the diagnosis of bone sarcoma and the beginning of pazopanib was 2.7 years (range 0.8–38 year). A median of two prior treatment modalities of chemotherapy (range 0–6) was administrated before start of pazopanib and all patients had radiological progression disease at the start of pazopanib. For patient, tumor and treatment characteristic at the time of diagnosis, see Table 1, at start of pazopanib treatment, see Table 2.
Table 1.
Patient Characteristic at Time of Diagnosis
| Primary Tumor n (%) | |
|---|---|
| Age | |
| Mean (range) | 35 (10–54) |
| Gender | |
| Male | 14(74) |
| Female | 5 (26) |
| Stage | |
| Localized advanced | 13(68) |
| Metastatic | 6(32) |
| Comorbidity | |
| No | 16(84) |
| Yes | 3(16) |
| Primary Location | |
| Extremities | 10(53) |
| Thorax/pelvis | 9(47) |
| Histology | |
| Osteosarcoma | 8(42) |
| Chondrosarcoma | 4(21) |
| Ewing sarcoma | 3(16) |
| Spindle cell/other | 4(21) |
| Treatment | |
| Surgery | 4(21) |
| Surgery + Cht/RT | 10(52) |
| Surgery + RT + Cht | 3(16) |
| Cht +/− RT | 2(11) |
| Primary Cured | |
| Yes | 16(84) |
| No | 3(16) |
RT: radiation therapy, Cht: Chemotherapy.
Table 2.
Patient Characteristic at Start of Pazopanib Treatment
| Start of Pazopanib n (%) | |
|---|---|
| Age | |
| Median (range) | 39(18–62) |
| Site of Metastasis | |
| Lung | 1(5) |
| Extra pulmonary | 2(11) |
| Lung and extra pulmonary | 11(58) |
| Local | 5(26) |
| Time from Diagnosis | |
| Median in year (range) | 2.67(0.8–38) |
| Treatment Before Pazopanib∗ | |
| Median number of lines | 2(0–6) |
| Median number of cycles† | 10.5(4–20) |
| Pazopanib Start Dose | |
| 800 mg | 15(79) |
| 600 mg | 1(5) |
| 400 mg | 3(16) |
| Best Response to Pazopanib | |
| Partial response | 6(32) |
| Stable disease | 7(37) |
| Progression | 4(21) |
| Not evaluable | 2(11) |
Treatment given for metastatic disease.
For patient who were treated with chemotherapy before pazopanib.
Response to Treatment
Fifteen patients started with full dose of pazopanib (800 mg daily), one with reduced dose of 600 mg daily and three patients with 400 mg daily based on physicians' evaluation of patients' performance status and comorbidity. Of the 19 patients, 13 patients had clinical benefit in the form of partial response (6 patients) or stable disease (7 patients) as best response, 4 patients had progression of the disease as best response, and 2 patients were not evaluated as they died within 8 weeks after treatment with pazopanib was initiated. All patients stop treatment because of progression at the time of evaluation.
Four patients with chondrosarcoma were included in this study, two patients had low grad tumors, one patient had intermediate grade tumor, and one patient had high-grade tumor. The two patients with low-grade tumors had stable disease as best response, whereas the patients with high- or intermediate-grade tumors both progressed and did not have any effect of Pazopanib. The rest of the patients treated with pazopanib had a high-grade malignancy.
Patients with partial response had all high-grade tumors, three patients with osteosarcoma, one patient with radiation-induced osteosarcoma, one patient with Ewing sarcoma, and one patient with spindle cell sarcoma. For these patients, the median time from the start of pazopanib treatment until progression was 8.4 months (range min–max: 2.7–19.3).
Toxicity to Treatment
Five patients did not experience any grade 3/4 toxicity during pazopanib treatment. Ten patients experienced one or two grade 3/4 toxicities and four patients had more than two grade 3/4 toxicities during pazopanib treatment. Pazopanib-related grade 3 or 4 toxicities are summarized in Table 3. No toxic deaths were reported. Five patients were reduced in pazopanib dose because of toxicity and two patients terminated treatment because of toxicity.
Table 3.
Pazopanib Related Toxicity (Grade 3/4)
| Number (%) | |
|---|---|
| Hematological | 2(11) |
| Neutropenia | 1(5) |
| Elevated lever parameters | 2(11) |
| Elevated creatinine | 1(5) |
| Elevated blood pressure | 3(16) |
| Fatigue | 5(26) |
| Mucositis | 2(11) |
| Others | 6(32) |
| Diarrhea | 3(16) |
Follow-Up and Progression Free Survival
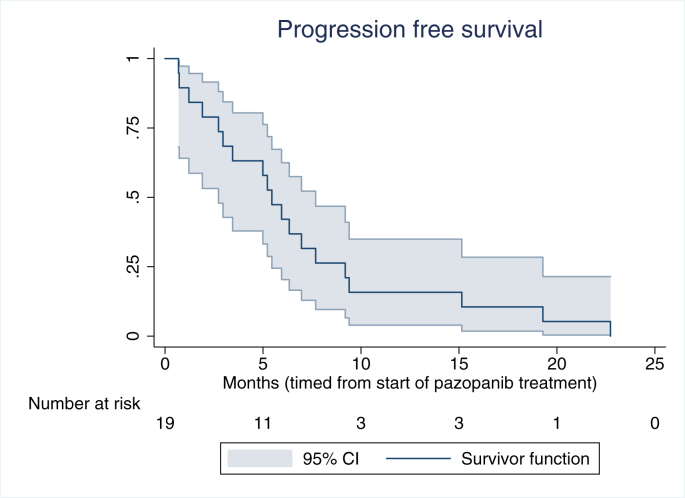
The median follow-up time after start of pazopanib treatment was 10 months (range 1.5–41 months). The median OS rate from the start of pazopanib treatment was 11 months (85% CI: 5.4–19.3). The median PFS from start of pazopanib treatment was 5.5 months (95% CI: 2.7–7.7). Figure 2 shows the PFS from start of pazopanib treatment to progression. Three patient has a PFS >15 months. None of these patients had the same histological subtype.
Figure 2.
Progression free survival for patient with metastatic bone sarcoma treated with pazopanib. The number of patients is 19. All patients have at the time of follow-up progressed.
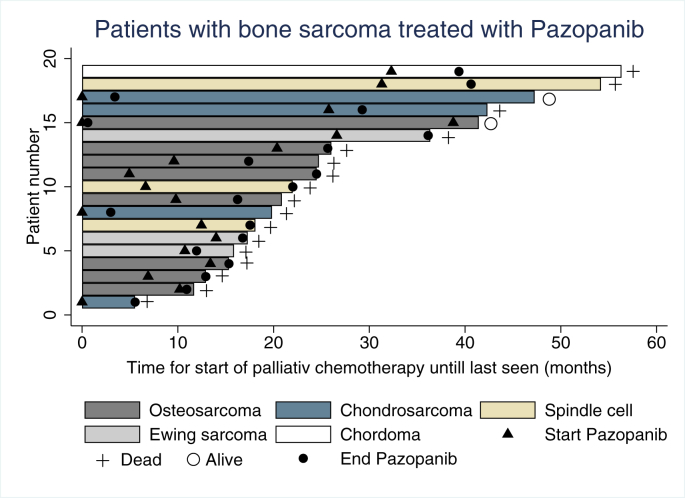
Eight patients were treated after progression of pazopanib and for eleven patients pazopanib was the last treatment received. Four patient received chemotherapy, two patient other tyrosine kinases inhibitors, and two patients received more than one treatment modalities. Figure 3 shows a swimmer plot from the start of pazopanib treatment until progression or death.
Figure 3.
Swimmers plot of patients treated with pazopanib. Illustrated from the start of palliative treatment until death or last seen. All patients ended the treatment with pazopanib because of progression.
Discussion
Despite different salvage strategies, refractory or metastatic bone sarcoma is usually fatal. Given the limited success of chemotherapy, efforts focusing on identifying targetable molecules are needed. Our results showed that pazopanib is well tolerated and seem to have a benefit in terms of PFS.
When metastatic or recurrence has occurred, the prognosis is much poorer as chemotherapy resistance develops, along with the lack of a recommended second-line treatment for refractory metastatic osteosarcoma, new modalities must be explored.
Pazopanib is a second-generation selective multitargeted receptor TKI and objective responses to treatment with a vascular endothelial growth factor receptor inhibitor have been observed in patients with Ewing sarcoma, synovial sarcoma, and osteosarcoma [16,18]. A resent paper on pazopanib treatment of relapsed osteosarcoma patients find a PFS of 6 months which is in accordance with our findings [16]. A study published by Seto et al. including 18 bone sarcoma patients of different histology showed a disease control rate (DCR) for bone sarcoma of 39% [19]. Our results show a DCR of 68% which much higher. Furthermore, the response rates, progression free survival, and overall survival shown in our study are comparable with the efficacy shown using sorafenib either alone or in combination with Everolimus [[11], [12], [13]].
In terms of toxicity, pazopanib appeared to be an acceptable treatment. The toxicity profile in our cohort is in line with the PALETTE study [4].
“In 2018 Duffaud et al. published a randomized double-blinded placebo-controlled phase 2 study investigating the efficacy and safety of regorafenib in adult patients with metastatic osteosarcoma. They showed that regorafenib was well tolerated and that the PFS was 16.4 weeks with a DCR of 64% and 8% of the patients were partial responders. These results are comparable with our result on Pazopanib [20].” “However, a limitation of this study is the retrospective nature or our study, the low number of patients treated with pazopanib along with the fact that these patients represent many different histological subtypes with different prognosis. Osteosarcomas represent highly aggressive tumors and Chordomas represent slow-growing tumors. These differences should be taken into account with interpreting the results of this paper”.
Multimodal treatment including chemotherapy and/or radiation therapy might be necessary and the role for pazopanib in this setting needs further investigations in bone sarcomas. The addition of chemotherapy to Pazopanib treatment has been tested in malignant melanoma with manageable toxicity. The foremost grade 3 toxicity was increase in alanine aminotransferase [21]. The combination of radiation therapy with pazopanib had been tested in the adjuvant treatment of breast cancer patient who developed less dermatological toxicity than matched control groups treated with radiation therapy alone [22]. Furthermore, ongoing trials are currently assigning the addition of pazopanib to radiotherapy in the neoadjuvant treatment of STS [23].
Our article suggests that antiangiogenic molecules alone could be useful in the treatment of bone sarcomas and further research investigating the role of pazopanib in bone sarcoma could be investigated in a phase II trial. Future studies on Pazopanib alone or in combination with chemotherapy could with advantage be compared with regorafenib either alone or also in combination with chemotherapy in randomized trial.
In conclusion, our data suggest that pazopanib have some activity against bone sarcoma. Pazopanib is approved for STS treatment and therefore available for treating bone sarcoma. Yet, despite the evidence indicating that pazopanib can stabilize the disease, the PFS and OS are still poor for patients with metastatic bone sarcoma.
Footnotes
Support: No funding.
References
- 1.Kager L., Zoubek A., Potschger U., Kastner U., Flege S., Kempf-Bielack B., Branscheid D., Kotz R., Salzer-Kuntschik M., Winkelmann W. Primary metastatic osteosarcoma: presentation and outcome of patients treated on neoadjuvant Cooperative Osteosarcoma Study Group protocols. J Clin Oncol. 2003;21(10):2011–2018. doi: 10.1200/JCO.2003.08.132. [DOI] [PubMed] [Google Scholar]
- 2.Group ESESNW Bone sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(Suppl 3) doi: 10.1093/annonc/mdu256. iii113-23. [DOI] [PubMed] [Google Scholar]
- 3.Schutz F.A., Choueiri T.K., Sternberg C.N. Pazopanib: clinical development of a potent anti-angiogenic drug. Crit Rev Oncol Hematol. 2011;77(3):163–171. doi: 10.1016/j.critrevonc.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 4.van der Graaf W.T., Blay J.Y., Chawla S.P., Kim D.W., Bui-Nguyen B., Casali P.G., Schoffski P., Aglietta M., Staddon A.P., Beppu Y. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet (London, England) 2012;379(9829):1879–1886. doi: 10.1016/S0140-6736(12)60651-5. [DOI] [PubMed] [Google Scholar]
- 5.Coens C., van der Graaf W.T., Blay J.Y., Chawla S.P., Judson I., Sanfilippo R., Manson S.C., Hodge R.A., Marreaud S., Prins J.B. Health-related quality-of-life results from PALETTE: a randomized, double-blind, phase 3 trial of pazopanib versus placebo in patients with soft tissue sarcoma whose disease has progressed during or after prior chemotherapy-a European Organization for research and treatment of cancer soft tissue and bone sarcoma group global network study (EORTC 62072) Cancer. 2015;121(17):2933–2941. doi: 10.1002/cncr.29426. [DOI] [PubMed] [Google Scholar]
- 6.Abdeen A., Chou A.J., Healey J.H., Khanna C., Osborne T.S., Hewitt S.M., Kim M., Wang D., Moody K., Gorlick R. Correlation between clinical outcome and growth factor pathway expression in osteogenic sarcoma. Cancer. 2009;115(22):5243–5250. doi: 10.1002/cncr.24562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGary E.C., Weber K., Mills L., Doucet M., Lewis V., Lev D.C., Fidler I.J., Bar-Eli M. Inhibition of platelet-derived growth factor-mediated proliferation of osteosarcoma cells by the novel tyrosine kinase inhibitor STI571. Clin Cancer Res. 2002;8(11):3584–3591. [PubMed] [Google Scholar]
- 8.Kubo T., Piperdi S., Rosenblum J., Antonescu C.R., Chen W., Kim H.S., Huvos A.G., Sowers R., Meyers P.A., Healey J.H. Platelet-derived growth factor receptor as a prognostic marker and a therapeutic target for imatinib mesylate therapy in osteosarcoma. Cancer. 2008;112(10):2119–2129. doi: 10.1002/cncr.23437. [DOI] [PubMed] [Google Scholar]
- 9.Manara M.C., Nicoletti G., Zambelli D., Ventura S., Guerzoni C., Landuzzi L., Lollini P.L., Maira S.M., Garcia-Echeverria C., Mercuri M., Picci P. NVP-BEZ235 as a new therapeutic option for sarcomas. Clin Cancer Res. 2010;16(2):530–540. doi: 10.1158/1078-0432.CCR-09-0816. [DOI] [PubMed] [Google Scholar]
- 10.Yukata K., Matsui Y., Goto T., Kubo T., Yasui N. Differential expression of VEGF isoforms and VEGF receptors in cartilaginous tumors. Anticancer Res. 2005;25(2A):955–957. [PubMed] [Google Scholar]
- 11.Grignani G., Palmerini E., Dileo P., Asaftei S.D., D'Ambrosio L., Pignochino Y., Mercuri M., Picci P., Fagioli F., Casali P.G. A phase II trial of sorafenib in relapsed and unresectable high-grade osteosarcoma after failure of standard multimodal therapy: an Italian Sarcoma Group study. Lancet Oncol. 2012;23(2):508–516. doi: 10.1093/annonc/mdr151. [DOI] [PubMed] [Google Scholar]
- 12.Raciborska A., Bilska K. Sorafenib in patients with progressed and refractory bone tumors. Med Oncol (Northwood, London, England) 2018;35(10):126. doi: 10.1007/s12032-018-1180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grignani G., Palmerini E., Ferraresi V., D'Ambrosio L., Bertulli R., Asaftei S.D., Tamburini A., Pignochino Y., Sangiolo D., Marchesi E. Sorafenib and everolimus for patients with unresectable high-grade osteosarcoma progressing after standard treatment: a non-randomised phase 2 clinical trial. Lancet Oncol. 2015;16(1):98–107. doi: 10.1016/S1470-2045(14)71136-2. [DOI] [PubMed] [Google Scholar]
- 14.Alcindor T. Response of refractory Ewing sarcoma to pazopanib. Acta Oncol (Stockholm, Sweden) 2015;54(7):1063–1064. doi: 10.3109/0284186X.2014.971938. [DOI] [PubMed] [Google Scholar]
- 15.Safwat A., Boysen A., Lucke A., Rossen P. Pazopanib in metastatic osteosarcoma: significant clinical response in three consecutive patients. Acta Oncol (Stockholm, Sweden) 2014;53(10):1451–1454. doi: 10.3109/0284186X.2014.948062. [DOI] [PubMed] [Google Scholar]
- 16.Longhi A., Paioli A., Palmerini E., Cesari M., Abate M.E., Setola E., Spinnato P., Donati D., Hompland I., Boye K. Pazopanib in relapsed osteosarcoma patients: report on 15 cases. Acta Oncol. 2019;58(1):124–128. doi: 10.1080/0284186X.2018.1503714. [DOI] [PubMed] [Google Scholar]
- 17.Maretty-Nielsen K., Aggerholm-Pedersen N., Keller J., Safwat A., Baerentzen S., Pedersen A.B. Population-based Aarhus Sarcoma Registry: validity, completeness of registration, and incidence of bone and soft tissue sarcomas in western Denmark. Clin Epidemiol. 2013;5:45–56. doi: 10.2147/CLEP.S41835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fox E., Aplenc R., Bagatell R., Chuk M.K., Dombi E., Goodspeed W., Goodwin A., Kromplewski M., Jayaprakash N., Marotti M. A phase 1 trial and pharmacokinetic study of cediranib, an orally bioavailable pan-vascular endothelial growth factor receptor inhibitor, in children and adolescents with refractory solid tumors. J Clin Oncol. 2010;28(35):5174–5181. doi: 10.1200/JCO.2010.30.9674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seto T., Song M.N., Trieu M., Yu J., Sidhu M., Liu C.M., Sam D., Pan M. Real-world experiences with pazopanib in patients with advanced soft tissue and bone sarcoma in Northern California. Med Sci (Basel) 2019;7(3) doi: 10.3390/medsci7030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duffaud F., Mir O., Boudou-Rouquette P., Piperno-Neumann S., Penel N., Bompas E., Delcambre C., Kalbacher E., Italiano A., Collard O. Efficacy and safety of regorafenib in adult patients with metastatic osteosarcoma: a non-comparative, randomised, double-blind, placebo-controlled, phase 2 study. Lancet Oncol. 2019;20(1):120–133. doi: 10.1016/S1470-2045(18)30742-3. [DOI] [PubMed] [Google Scholar]
- 21.Urbonas V., Schadendorf D., Zimmer L., Danson S., Marshall E., Corrie P., Wheater M., Plummer E., Mauch C., Scudder C. Paclitaxel with or without trametinib or pazopanib in advanced wild-type BRAF melanoma (PACMEL): a multicentre, open-label, randomised, controlled phase II trial. Ann Oncol. 2019;30(2):317–324. doi: 10.1093/annonc/mdy500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goyal S., Shah S., Khan A.J., Danish H., Haffty B.G. Evaluation of acute locoregional toxicity in patients with breast cancer treated with adjuvant radiotherapy in combination with pazopanib. ISRN Oncol. 2012;2012:896202. doi: 10.5402/2012/896202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong P., Houghton P., Kirsch D.G., Finkelstein S.E., Monjazeb A.M., Xu-Welliver M., Dicker A.P., Ahmed M., Vikram B., Teicher B.A. Combining targeted agents with modern radiotherapy in soft tissue sarcomas. J Natl Cancer Inst. 2014;106(11) doi: 10.1093/jnci/dju329. [DOI] [PMC free article] [PubMed] [Google Scholar]