Summary
The use of ultrasound in regional anaesthesia has expanded our understanding of regional anaesthesia techniques and allowed for the development of novel strategies to achieve blockade of the trunk. Several alternatives to paravertebral block have recently been proposed, but none of these new techniques have yet been shown to provide surgical anaesthesia equivalent to a paravertebral block. This case report describes the successful use of the mid‐point transverse process to pleura (MTP) block as the sole anaesthetic technique for a patient undergoing breast surgery.
Introduction
The use of paravertebral blockade alone 1, or in combination with a PECS II block 2, has been described for general anaesthesia‐free breast surgery. Despite the efficacy and benefits of paravertebral blockade, the potential for complications, particularly pneumothorax, continues to be a limit for their more widespread use in clinical practice.
Recently, several new thoracic wall blocks have been described as alternatives to paravertebral blockade, although evidence of analgesic equivalence is currently lacking. Previously, we proposed the retrolaminar, intercostal/paraspinal, midpoint transverse process to pleura (MTP) and erector spinae plane (ESP) blocks as ‘paravertebral by proxy’ 3. Although there is evidence for surgical anaesthesia for paravertebral blockade, this is not currently the case for the paravertebral by proxy blocks. We have described the MTP block 4 as an alternative end‐point for ultrasound‐guided thoracic paravertebral blockade and this technique has not been previously described for surgical anaesthesia.
Report
A 53‐year‐old woman presented for radioactive seed‐guided excision of left breast tissue and duct exploration. Her weight was 105.7 kg, height 172.7 cm, with a body mass index of 35.4 kg.m−2. Her past medical history included hypertension, obstructive sleep apnoea, right hemidiaphragm paralysis of unknown aetiology and alcohol consumption of 4–6 units per day. Given her history of obstructive sleep apnoea and right hemidiaphragm paralysis, the patient was interested in general anaesthesia‐free breast surgery. The patient was, therefore, offered to have the procedure performed under MTP block, to which she consented.
After applying full monitoring as per Association of Anaesthetists guidelines 5, vascular access was achieved with a 20‐G peripheral venous cannula. The MTP block was performed with the patient in a sitting position. The T4 and T5 transverse processes were sonographically identified and then the level was determined by counting from the twelfth rib. This was also verified by counting down from the first rib. Using a high‐frequency HFL‐50 15–6 MHz linear transducer (Sonosite M‐Turbo, Bothell, WA, USA) with a parasagittal scan, a single‐level MTP block was carried out with a 80‐mm, 22‐G SonoTAP block needle (Pajunk, Geisingen, Germany), as per our previously described technique 4. 1% ropivacaine 10 ml was mixed with 2% lidocaine 10 ml for a final concentration of ropivacaine 0.5% and lidocaine 1%. Adrenaline was added to achieve a concentration of 1:400,000. Twenty millilitres of this solution was injected at the level of the T4 nerve root, between the T4 and T5 transverse processes. Upon injection, local anaesthetic spread was noted in the area midway between the transverse process and pleura, with posterior spread towards the posterior border of the transverse processes, without any evidence of spread in the ESP and minimal pleural depression (Fig. 1). Following the injection, slight downward displacement of the pleura was noted at the T4 and T5 levels.
Figure 1.
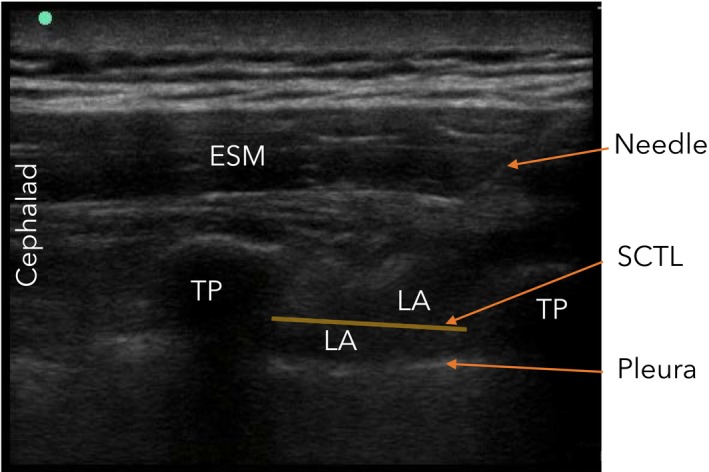
Parasagittal ultrasound image of an MTP block at T4/5 level. ESM, Erector spinae muscle; LA, local anaesthetic; TP, transverse process; SCTL, superior costo‐transverse ligament.
Due to time constraints, the block was carried out in the operating room immediately before surgery, with a plan for supplementation with local anaesthetic infiltration by the surgeon or conversion to general anaesthesia, if required. Sedation for surgery consisted of intravenous midazolam 1 mg before the block, ketamine 10 mg before the start of surgery and an additional ketamine 10 mg intraoperatively. A propofol infusion at 40 μg.kg−1.min−1 was commenced at the beginning of surgery and reduced intraoperatively to 30 μg.kg−1.min−1. There was no sensation to pinprick in the area of surgery before knife incision. The surgery was completed in 38 min without any local supplementation by the surgeon, and with the patient intermittently sleeping. At the completion of surgery, the patient had a demonstrable block in the T4 and T5 distribution. She described having no discomfort throughout the surgery, apart from the discomfort of the blood pressure cuff intermittently inflating.
The patient remained in the postoperative anaesthesia care unit for 2 h, followed by 2 h in the surgical day care unit as per institutional policy for patients with obstructive sleep apnoea. In the postoperative anaesthesia care unit, she was fully awake and alert on arrival and with a pain score of 0 out of 10. This remained the case at 15–30‐min intervals throughout her recovery room stay. There were no episodes of nausea or vomiting. She continued to have a pain score of 0 out of 10 for the 2 h subsequently spent in the surgical day care unit. No narcotics were administered in the operating room, or in the postoperative anaesthesia care unit.
Discussion
The MTP block is thought to act via paravertebral spread through septations and fenestrations in the superior costotransverse ligament, as well as medial to the free edge of the superior costotransverse ligament 4, thus achieving a paravertebral block without placing the needle tip in the paravertebral space. Surgical anaesthesia with paravertebral block alone 1 has previously been described, however, there is insufficient evidence for the efficacy of the paravertebral by proxy blocks as a surgical anaesthetic.
Although the ESP block has gained widespread popularity, it has been described for analgesia rather than surgical anaesthesia. Attempts to fully delineate the mechanism of action of ESP blockade have yielded conflicting results with regard to the reliability of paravertebral spread 6, 7, 8, with two cadaver studies suggesting paravertebral spread as a mechanism of action 6, 7, and one cadaver study not supporting this mechanism of action 8. Regardless of the mechanism of action, there is only one case report describing the use of the ESP block for providing complete surgical anaesthesia for mastectomy and axillary dissection 9.
This is the first description of the MTP block being used for surgical anaesthesia. In this case, the plan was for a paravertebral block for surgical anaesthesia, in accordance with the patient's request to avoid a general anaesthetic. As the superior costotransverse ligament was not easily visualised due to the patient's increased BMI, a decision was made to perform an MTP block instead of aiming to place the needle tip in close proximity to the pleura with suboptimal imaging.
Additionally, a single injection covered the dermatomes required for the surgical procedure, indicating that a single‐level injection may have a multilevel spread. In this particular surgery, the amount of tissue to be removed was not large and did not require blockade of more than two or three levels. Our clinical experience with the MTP block so far has suggested reliable spread at the level of injection, but somewhat unreliable spread to adjacent levels with larger volumes. The extent of dermatomal sensory block with a single‐level injection using a larger local anaesthetic volume has not been described. In conclusion, the use of the MTP block for general anaesthesia‐free surgery may be feasible and warrants further exploration.
Acknowledgements
Patient's written consent was obtained for publication. No external funding or competing interests declared.
References
- 1. Simpson J, Ariyarathenam A, Dunn J, Ford P. Breast surgery using thoracic paravertebral blockade and sedation alone. Anesthesiology Research and Practice 2014; 204: 127467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pawa A, Wight J, Onwochei DN, et al. Combined thoracic paravertebral and pectoral nerve blocks for breast surgery under sedation: a prospective observational case series. Anaesthesia 2018; 73: 438–43. [DOI] [PubMed] [Google Scholar]
- 3. Costache I, Pawa A, Abdallah FW. Paravertebral by proxy – time to redefine the paravertebral block. Anaesthesia 2018; 73: 1185–8. [DOI] [PubMed] [Google Scholar]
- 4. Costache I, de Neumann L, Ramnanan CJ, et al. The midpoint transverse process to pleura (MTP) block: a new endpoint for thoracic paravertebral block. Anaesthesia 2017; 72: 1230–6. [DOI] [PubMed] [Google Scholar]
- 5. Checketts MR, Alladi R, Ferguson K, et al. Recommendations for standards of monitoring during anaesthesia and recovery 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia 2016; 71: 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yang HM, Choi YJ, Kwon HJ, O J, Cho TH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spine plane blocks in the thoracic region: a cadaveric study. Anaesthesia 2018; 73: 1244–50. [DOI] [PubMed] [Google Scholar]
- 7. Adhikary S, Bernard S, Lopez H, Chin K. Erector spinae plane block versus retrolaminar block: a magnetic resonance imaging and anatomical study. Regional Anesthesia and Pain Medicine 2018; 43: 756–62. [DOI] [PubMed] [Google Scholar]
- 8. Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spine blockade. Regional Anesthesia and Pain Medicine 2018; 43: 567–71. [DOI] [PubMed] [Google Scholar]
- 9. Kimachi PP, Martins EG, Peng P, Forero M. The erector spine plane block provides complete surgical anesthesia in breast surgery: a case report. Anesthesia and Analgesia Practice 2018; 11: 186–8. [DOI] [PubMed] [Google Scholar]


