Abstract
An isoproterenol infusion was administered during an electrophysiologic study (EPS) in a patient with a history of near syncope, left bundle branch block, and no documented atrioventricular (AV) block. Isoproterenol precipitated classic 2:1 Infra‐Hisian AV block most probably proximal to the site of recording a His–Purkinje potential consistent with right bundle branch activity. Paroxysmal AV block also occurred during isoproterenol washout at a different site located distal to the presumed right bundle branch potential. Isoproterenol may be valuable diagnostically in an occasional patient suspected of AV block in whom an EPS is unrevealing and a drug challenge is negative.
Keywords: isoproterenol, paroxysmal atrioventricular block, atrioventricular block, electrophysiologic study
Isoproterenol is primarily used for the treatment of bradycardia and atrioventricular (AV) block. Surprisingly, it may rarely precipitate AV block under certain circumstances.1, 2 Such a paradoxical response may be considered a side effect or a positive finding in a patient with a previously negative electrophysiologic study (EPS). We recently encountered a patient who presented with near syncope and left bundle branch block (LBBB) in whom AV block was never documented. A standard EPS was normal but an isoproterenol challenge induced two different forms of pathological block in the His–Purkinje system.
CASE REPORT
A 53‐year‐old woman presented with atypical chest pain and dyspnea on exertion for about 2 years. She also described dizziness with presyncopal spells but no syncope. A two‐dimensional echocardiogram was normal. The patient developed a rate‐dependent complete LBBB but no AV block during an exercise test in which the maximal heart rate was 156/min. A 72 hour Holter recording was unremarkable. Coronary angiography showed normal coronary arteries and normal left ventricular function. The patient was treated for possible microvascular angina with nitrates, diltiazem, and simvastatin but these agents were discontinued after several weeks because of side effects and lack of effectiveness. The patient continued to experience more frequent and more severe near syncope. Consequently, an EPS was performed (1 year after the initial stress test) to rule out ventricular tachycardia (VT) or AV block. At the time of the EPS, the ECG showed stable complete LBBB that was no longer rate‐dependent. The EPS revealed the following findings (Fig. 1): (1) Baseline: AH interval = 114 ms, HV interval = 65 ms (at a sinus rate of 82/min), normal corrected sinus recovery time, longest AH interval (with atrial pacing) was 214 ms with no evidence of dual AV nodal pathways, the AV Wenckebach (supra‐Hisian) point occurred at an atrial pacing cycle of 400 ms, and 2:1 supra‐Hisian AV block was observed at an atrial cycle length of 340 ms. The deflection labeled “p” is probably a potential from the right bundle branch a pV interval = 22 ms. No VT was induced by programmed stimulation. (2) Ajmaline (total dose 62.5 mg) was administered to challenge AV conduction with the resultant nondiagnostic prolongation of the HV interval from 65 to 95 ms with no AV block. (3) Isoproterenol was then administered to facilitate the induction of VT by programmed stimulation or the development of pathological second‐ or third‐degree AV block according to the work of Brembilla‐Perrot et al.1 The infusion was started at 2.0 mcg/min more than 15 minutes after ajmaline administration. Isoproterenol precipitated episodes of 2:1 infra‐Hisian block proximal to the p potential with the following findings at a sinus rate of about 115/min: AH interval = 103 ms, HV interval = 206 ms, pV interval = 72 ms (Fig. 2). The isoproterenol infusion was then discontinued and programmed stimulation for VT induction was not performed. About 4½ minutes later during 1:1 AV conduction (rate = 83/min, AH interval = 114 ms, HV interval = 92 ms, pV = 50 ms), a transient episode of complete AV block was recorded with ventricular asystole of 4.26 seconds. The last two ventricular beats are most probably not conducted. Rather, they represent ventricular escape beats generating a surface ECG different from those of conducted beats on the left of the tracing. In the last beat, the very long HV interval rules out ventricular fusion. The AH interval remained constant at 114 ms consistent with anterograde AV conduction. The HV interval of 163 ms and the pV interval of 123 ms appear to reflect the time difference between the blocked supraventricular beat and the emergence of the ventricular escape beat (Fig. 3). The same argument applies to the second last ventricular beat. Temporary ventricular pacing was initiated and a permanent dual chamber pacemaker was then implanted later. The patient has remained asymptomatic during a follow‐up period of more than 9 months.
Figure 1.
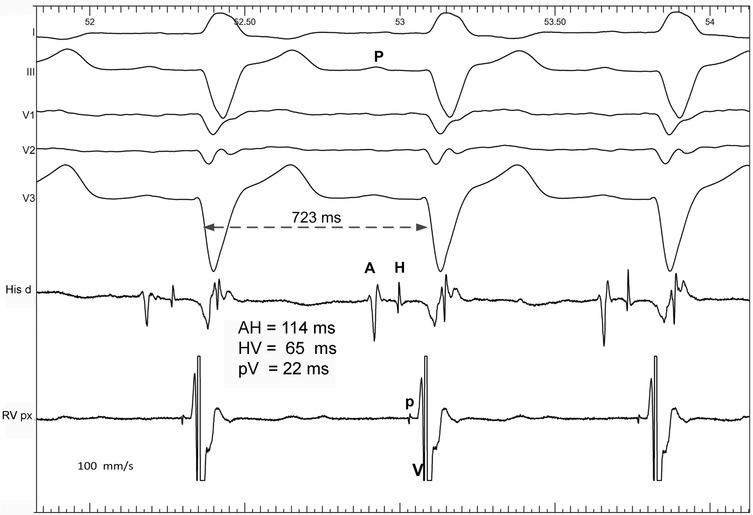
Basal His bundle recordings. Top: ECG leads I, III, V1–V3, A = atrial deflection, H = His bundle potential, V = ventricular potential, p = probable right bundle branch potential or Purkinje potential, P = P wave, pV = interval from p to V, His d = channel recording from distal His bundle, RVp = channel recording from the proximal right ventricular site.
Figure 2.
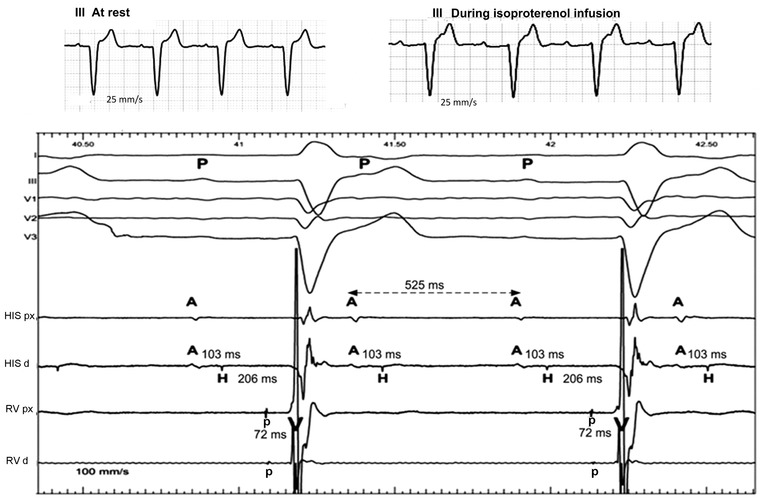
His bundle recordings during Isoproterenol infusion precipitating 2:1 AV block at a sinus rate of about 115/min (PP = 525 ms). Top: Lead III ECG (recorded with an electrocardiograph at 25 mm/s) before and after isoproterenol infusion. Under the slow ECG on top, the ECG leads I, III, and V1–V3 were recorded at 100 mm/s. A = atrial deflection, H = His bundle potential, V = ventricular potential, RV = right ventricular, p = right bundle branch or Purkinje potential, P = P wave, pV = interval from p to V, His px = channel recording from proximal His bundle, His d = channel recording from distal His bundle, RVp = channel recording from proximal RV, RVd = channel recording from distal RV. This represents classic infra‐Hisian AV block. During AV block, the p potential is absent indicating block between the His bundle and the p potential. See text for details.
Figure 3.
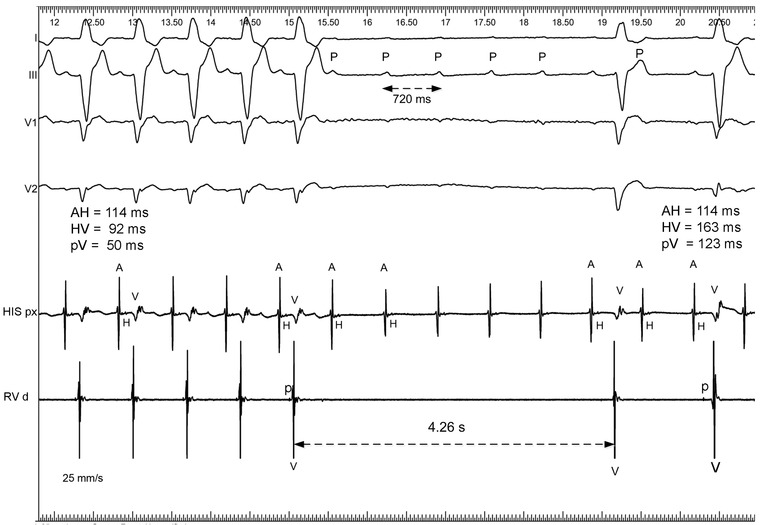
Paroxysmal AV block induced by isoproterenol infusion at a sinus rate of about 83/min (PP = 720 ms). ECG leads I, III, V1–V3. A = atrial deflection, H = His bundle potential, V = ventricular potential, RV = right ventricular, p = Purkinje or right bundle potential, P = P wave, pV = interval from p to V, His p = channel recording from proximal His bundle, RVp = channel recording from proximal RV. This form of AV block is different from that in Figure 2 because the Purkinje p potentials were recorded during AV block so that the block appeared distal to the p or right bundle branch potential. All the AH intervals are constant and indicate supraventricular conduction. The last two ventricular beats are probably ventricular escape beats. They are most probably not conducted and are unlikely to represent ventricular fusion. See text for details
DISCUSSION
The package insert of isoproterenol states the following: “In a few patients presumably with organic disease of the AV node and its branches, isoproterenol hydrochloride injection has been reported to precipitate Adam–Stokes seizures during normal sinus rhythm or transient AV block.”2 Isoproterenol may induce transient second‐ or third‐degree AV block by several mechanisms that include myocardial ischemia, the Bezold–Jarisch reflex, and latent abnormalities in the His–Purkinje system either by permitting 1:1 conduction of sinus tachycardia faster than the maximum rate obtained by pacing and/or by producing an altered electrophysiologic milieu of the heart not necessarily associated with a marked increase in the sinus rate.
The mechanism of isoproterenol‐induced AV block in our patient is unclear, but it resembles the observations of Brembilla‐Perrot et al.1 who studied the effect of isoproterenol in 765 patients undergoing an EPS. These workers observed the paradoxical effect of isoproterenol in eight patients (65 ± 11 years) with exercise‐ or stress‐related dizziness/syncope. Six patients had no heart disease, one had myocardial ischemia, and one had idiopathic dilated cardiomyopathy. They all exhibited normal AV conduction in the basal state and a normal standard EPS. The administration of isoproterenol during an EPS precipitated second‐degree AV block that was supra‐Hisian and spontaneous in four patients. In the other four patients, the block was infra‐Hisian. In the latter, the induction of AV block in two patients occurred only after atrial pacing at a rate <160/min. None of the AV blocks was characterized in terms of type I or II forms.
In Figure 2, 2:1 AV block was classic infra‐Hisian block between the His bundle and the Purkinje potential (p probably the right bundle potential) yet, in Figure 3 during the isoproterenol washout, the AV block was below the p potential. The observations suggest the occurrence of His–Purkinje block at two different sites. Because ajmaline has an ultrashort half‐life, we believe that the administration of isoproterenol was primarily responsible for precipitating the conduction disorders with a questionable small additive effect from ajmaline administered before isoproterenol. The induction of AV block by isoproterenol may be explained by a number of mechanisms but the most probable cause is enhancement of conduction proximal to a site of diseased His–Purkinje tissue with latent block either in the His bundle and/or the right bundle branch. These circumstances produced block distal to the His bundle (as in Fig. 2) or distal to the right bundle branch (as in Fig. 3) the latter being associated with more distal disease in the His–Purkinje system.
CONCLUSION
Our observations suggest that the administration of isoproterenol may be valuable diagnostically in an occasional patient suspected of AV block (especially in the His–Purkinje system) in whom an EPS is unrevealing and a drug challenge (procainamide, ajmaline, etc.) is negative. EPS with isoproterenol may precipitate classic and/or paroxysmal AV block as in our patient but their mechanisms remain to be elucidated.
REFERENCES
- 1. Brembilla‐Perrot B, Muhanna I, Nippert M, Popovic B, Beurrier D, Houriez P, Terrier de la Chaise A, Claudon O, Louis P, Abdelaal A, State S, Andronache M, Suty‐Selton C. Paradoxical effect of isoprenaline infusion. Europace 2005;7:621–627. [DOI] [PubMed] [Google Scholar]
- 2. Hospira, Inc. ISUPREL (isoproterenol hydrochloride) injection, solution. Available at: http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=c4288d64-4f76-44f8-d097-4bd3955f5676 Accessed January 2, 2014.


