Abstract
Background
Autonomic nervous system (ANS) dysfunction appears in the course of both chronic heart failure (CHF) and depression. Comprehensive cardiac rehabilitation (CCR), apart from improving physical capacity, can reduce depressive symptoms and leads to the restoration of ANS function among CHF patients.
The purpose was to evaluate the influence of the reversion of depression (measured by Beck Depression Inventory [BDI] score, cut point <10) and the physical capacity improvement (measured by peak oxygen consumption [peak VO2; ml/kg per minute]) on the sympathovagal balance (measured by low/high frequency ratio [LF/HF]) after CCR in CHF patients.
Methods
The study group comprised 111 CHF patients (New York Heart Association II–III; left ventricular ejection fraction ≤ 40%). Patients were randomized (2:1) to 8‐week CCR based on Nordic walking training (five times weekly) at 40–70% of maximal heart rate, training group (TG) n = 77, or to control group (CG) n = 34. The effectiveness of CCR was assessed by changes—delta (Δ) in LF/HF, BDI score, and peak VO2, as a result of comparing these parameters from the beginning and the end of the program.
Results
Eventually, 46 patients in TG and 23 patients in CG were eligible for simultaneous ANS and psychological status analysis. Only in TG the LF/HF decreased 2.06 ± 1.14 versus 1.19 ± 0.80 (P < 0.0001) and peak VO2 increased 16.83 ± 3.72 versus 19.14 ± 4.20 ml/kg per minute (P < 0.0001). Favorable results in CG were not observed. The differences between TG and CG were significant: Δpeak VO2 (P < 0.0001); ΔLF/HF (P = 0.0001). Depressive symptoms were substantially reduced in both groups (TG, P = 0.0006; CG, P = 0.0490). Nevertheless, the greatest improvement of sympathovagal balance was observed in patients whose depression was reversed, thanks to the CCR in comparison to other patients from TG and the entire CG.
Conclusion
Positive effect of the sympatho‐parasympathetic balance obtained during the home CCR based on Nordic walking training results from the additive effects of the reversion of depression and physical capacity improvement in CHF patients.
Keywords: heart rate variability, depression, exercise training
Autonomic nervous system (ANS) dysfunction appears in the course of both chronic heart failure (CHF) and depression.1 On the contrary, depression is a common comorbidity among CHF patients with prevalence between 13% and 60%.2 In addition, heart failure is characterized by reduced exercise tolerance.3 Moreover, the following three factors reflect poor prognosis in CHF patients and lead to increased morbidity and mortality: altered ANS activity, depression, and decrease of physical capacity.1, 2, 3 Most of the data available on the subject prove that comprehensive cardiac rehabilitation (CCR) which includes, among others, exercise training and psychological support not only improves physical capacity, but also can reduce depressive symptoms.4, 5 This, on the contrary, leads to the restoration of ANS function among CHF patients.6, 7, 8 The Nordic walking training, apart from its obvious beneficial effects on general health, is well accepted and positively affects the mental state and motivation of patients, especially those suffering from depression, in which case its psychological repercussions are essential.9, 10, 11
No articles evaluating simultaneously the influence of Nordic walking training on ANS activity, physical capacity, and psychological distress in CHF patients have been published so far. Therefore, the objective of this study was to investigate and evaluate the influence of the reversion of depression and the physical capacity improvement on the sympatho‐parasympathetic balance after the comprehensive cardiac telerehabilitation based on Nordic walking training in CHF patients.
METHODS
The present study formed part of a single‐center, prospective, parallel‐group, randomized (2:1), controlled trial of home telemonitored CCR based on Nordic walking training (training group [TG]) versus usual care (control group [CG]) in CHF patients who also met the criteria for heart rate variability (HRV) assessment and correctly filled out the Beck Depression Inventory (BDI) questionnaire. For this study, we recruited consecutive patients hospitalized between December 2009 and June 2012 in the Department of Cardiac Rehabilitation, Institute of Cardiology, Warsaw, Poland, for the inclusion in the cardiac rehabilitation. The study was approved by the local Ethics Committee. Each patient gave written informed consent.
We included patients of either sex with any etiology of left ventricular systolic HF as defined in the European Society of Cardiology (ESC) guidelines3 diagnosed at least for 3 months; with a left ventricular ejection fraction (LVEF) < 40% on echocardiography; classified in New York Heart Association (NYHA) as class II or III; patients who were clinically stable and receiving an optimal and stable medication regimen for at least 4 weeks before enrollment; patients who had no contraindications to exercise training according to current recommendation for HF patients12; patients with sinus rhythm and those who correctly filled out the BDI questionnaire.
The exclusion criteria were a history of an acute coronary syndrome within the last month, coronary artery bypass grafting within the last 2 months, or initiation of cardiac resynchronization therapy within the last 6 months, or implantation of a pacemaker and/or implantable cardioverter‐defibrillator (ICD) within the last 6 weeks; atrial fibrillation or flutter, atrial and/or ventricular permanent pacing; symptomatic and/or exercise‐induced cardiac arrhythmia or conduction disturbances; valvular or congenital heart disease requiring surgical treatment; hypertrophic cardiomyopathy; severe pulmonary hypertension or other severe pulmonary disease; uncontrolled hypertension; anemia; acute and/or decompensated noncardiac disease; physical disability related to severe musculoskeletal or neurological problems; patient refusal to participate.
The qualified patients in both groups underwent the following assessments at entry and after completing the 8‐week program: clinical examination, two‐dimensional echocardiography, cardiopulmonary exercise test, 24‐hour Holter ECG monitoring with HRV assessment and psychological status (BDI) evaluation.
Echocardiography
Two‐dimensional echocardiography was performed using standard parasternal, apical, and subcostal views (VIVID 4 GE Medical System with a 2.5 MHz transducer). LVEF was calculated on the basis of conventional apical two‐chamber and four‐chamber images using the biplane Simpson technique.
24‐Hour Holter ECG Monitoring and HRV Analysis
HRV was measured using a 24‐hour Holter ECG, recorded with a 3‐channel Spacelabs Lifecard system (Spacelabs, Del Mar Reynolds, Hertford, United Kingdom). HRV indices were calculated after prospective interactive ECG analysis, using the Impresario Space software (Del Mar Reynolds). The measurements of HRV included time domain—standard deviation of all normal RR intervals (SDNN) and frequency domain indices, which were calculated after fast Fourier transformation of five 10‐minute ECG segments, recorded between 2 a.m. and 6 a.m. The highest and lowest values were excluded, and the three remaining values were averaged. The power spectrum density of low frequency (LF) 0.04–0.15 Hz, high frequency (HF) 0.15–0.4 Hz, and the low frequency to high frequency ratio (LF/HF) was calculated using standard methodology.13 The LF and HF were presented as logarithmic values (log LF, log HF). The influence of Nordic walking training on HRV was assessed by changes—delta (Δ) in log LF, log HF, and LF/HF ratio, resulting from the comparison of these parameters from the beginning and the end of the program.
Cardiopulmonary Exercise Treadmill Test
The symptom limited cardiopulmonary exercise treadmill test (CPET) according to a ramp protocol and ESC recommendations14 was performed using a Schiller treadmill (Doral, FL, USA) which was connected to a computerized breath‐by‐breath spiroergometry system (ZAN 600, ZAN Messgeräte GmbH, Nuremberg, Germany). Oxygen consumption was measured continuously using breath‐by‐breath analysis and used as an index of exercise capacity. Peak VO2 was defined as the highest oxygen uptake level achieved during the final 30 seconds of CPET.
Depression Assessment
The BDI, a 21‐item questionnaire, was administered to assess the subject's self‐reported depression symptoms. In general terms, BDI scores range from 0 to 63, and the lower the score, the better the condition of the patient. Patients with BDI scores ≥ 10 were considered affected by depression. The lower BDI score, even though in some cases it did not reach the cut point (<10) implying the reversion of depression, was qualified as the decrease of depression symptoms.
Comprehensive Cardiac Telerehabilitation Program
Home‐based telerehabilitation was performed as a comprehensive procedure which included all core components of cardiac rehabilitation (education, exercise training based on Nordic walking, psychological care, diet, and lifestyle recommendation).
Exercise Training
Exercise training was planned in line with the current guidelines for HF patients.12 The chosen workload reflected individual effort tolerance with regard to perceived exertion according to the Borg scale16 and the training heart rate (HR) range established individually for each patient. The training HR was calculated using the method known as HR reserve. This method uses a percentage of the difference between the maximum HR and the resting HR rate, and adds this value to the resting HR. The target training HR was 40–70% of the HR reserve. Patients underwent an 8‐week home‐based telerehabilitation program. The training session consisted of three parts: a warm‐up lasting 5–10 minutes (breathing and light resistance exercises, calisthenics), a 15–45‐minute Nordic walking training, and a 5‐minute cool‐down. Patients trained five times a week, and specific details of training methodology were prescribed previously.11
The exercise training effectiveness was assessed by changes—Δ in LF/HF, BDI score, and peak VO2 in CPET, resulting from the comparison of these parameters from the beginning and the end of the program. The methodology of telerehabilitation model was described previously.17, 18, 19
In brief, all patients in the TG received a special remote device for telemonitored and telesupervised exercise training—telerehabilitation set (Pro Plus Company, Poland), which consists of EHO mini device and blood pressure measuring and weighing machine. The EHO mini device enabled of the ECG data from three precordial leads to be recorded and transmitted via a mobile phone to the monitoring center.
Psychological Support
Patients from both groups had individual meetings with a psychologist once a day during the first 5 days. Topics which the consultation included are as follows: disease‐related problems, patient's mood, and the approval for further rehabilitation. In addition, TG patients who expressed the need for psychological support could provided with individually tailored psychological care over telephone conversations. During these calls patients received practical information on coping with chronic disease and support in terms of everyday challenges of being affected by such disease. They were also motivated to carry on with the telerehabilitation and advised to include relaxation training into their daily routine.
Apart from being given the initial support from a psychologist, TG patients received mental and motivational support to a healthy lifestyle and exercise training by the entire team involved in the home‐based telerehabilitation (nurse, physiotherapist, physician). This support consisted in day‐to‐day telephone conversations with a nurse and a physiotherapist. The nurse asked the patients about their mood, worrying symptoms (short breathness, chest pain, etc.), confirmed that patients took their medication and asked about their rehabilitation‐related doubts and problems. The physiotherapist was available to consult the exercise routine before the training session and afterward called the patient again to discuss the training and evaluate the rating of perceived exertion according to Borg scale. If necessary, the patients could also get in touch with the physician.
After the completion of the telerehabilitation (TG) and observation (CG), the psychologist conducted two individual meetings with all the patients regarding their feelings, needs, well‐being, and other aspects of their mood.
Usual Care
Patients in CG receiving “usual care” did not receive a formal exercise training prescription and did not undergo supervised rehabilitation.
All patients, independent from the treatment group, were given recommendations for appropriate lifestyle changes and self‐management according to ESC guidelines.3
Statistical Analysis
Statistical analyses were performed using SAS software (version 9.2; Cary, NC, USA). The normality of distributions was verified using the Shapiro‐Wilk test. To compare normally distributed continuous variables, the paired and unpaired t‐tests were used. To compare changes of variables in time between training and CGs, the general linear model with repeated measures adjusted for age, sex, diabetes, and undergone myocardial infarction, coronary artery bypass grafting was used. The signed‐rank test (for changes over time) and the Wilcoxon or Kruskal‐Wallis tests (to compare groups) were used for continuous variables that were not distributed normally. Correlations between peak VO2 and LF/HF ratio changes were tested in accordance with Spearman‐Pearson test. The correlation analysis between indicators of depression and multivariate regression of BDI and peak VO2 on LF/HF ratio were also conducted. The chi‐squared or Fisher's exact tests were used for categorical variables. P values <0.05 were considered significant.
RESULTS
Of the 111 patients randomized, 77 were assigned to the TG and 34 to the CG.
Forty‐six patients in TG and 23 patients in CG (Fig. 1) were eligible for simultaneous HRV and psychological status analysis. At baseline, the groups were comparable in terms of clinical data including HRV indices, BDI score, prevalence of depression, pharmacotherapy, and demographic characteristics except for age. The baseline clinical characteristics of patients are shown in Table 1.
Figure 1.
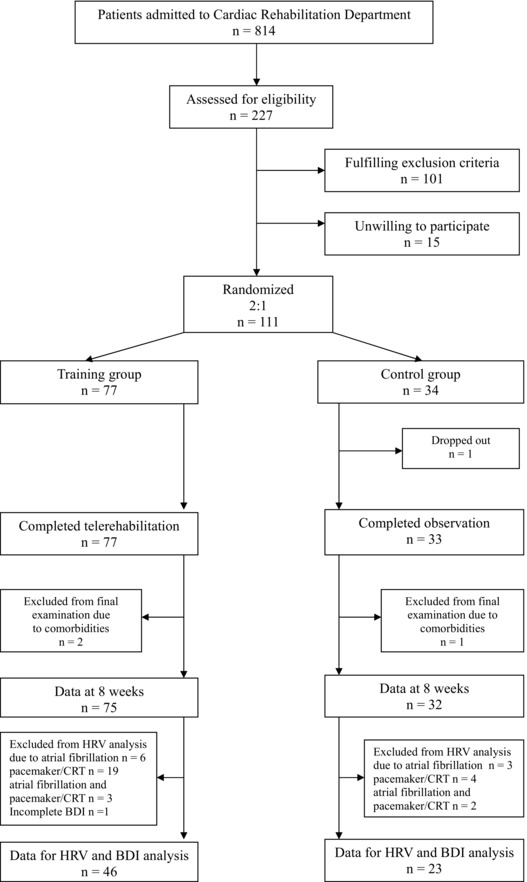
Figure flow of patients through the study. HRV = heart rate variability; BDI = Beck Depression Inventory; CRT = cardiac resynchronization therapy.
Table 1.
Baseline Characteristics
| Training Group | Control Group | ||
|---|---|---|---|
| (n = 46) | (n = 23) | P | |
| Males, n (%) | 39 (84,78) | 22 (95,65) | ns |
| Age (years), mean ± SD | 54.3 ± 10.38 | 60.4 ± 11.9 | 0.0205 |
| Left ventricular ejection fraction (%), mean ± SD | 31 ± 7 | 33 ± 7 | ns |
| Etiology of heart failure, n (%) | |||
| Ischemic | 34 (73.91) | 20 (86.96) | ns |
| Nonischemic | 12 (26.09) | 3 (13.04) | ns |
| Medical history, n (%) | |||
| Myocardial infarction | 32 (69.57) | 20 (86.96) | ns |
| Angioplasty | 25 (54.35) | 17 (73.91) | ns |
| Coronary artery bypass grafting | 10 (21.74) | 7 (30.43) | ns |
| Stroke | 1 (2.22) | 2 (8.70) | ns |
| Diabetes | 10 (21.74) | 6 (26.09) | ns |
| Hyperlipidemia | 26 (56.52) | 15 (65.22) | ns |
| Functional status | |||
| NYHA II, n (%) | 36 (78.26) | 16 (69.57) | ns |
| NYHA III, n (%) | 10 (21.74) | 7 (30.43) | ns |
| Depressed, n (%) | 16 (34.78) | 11 (47.83) | ns |
| Nondepressed, n (%) | 20 (65.22) | 12 (52.17) | ns |
| Beck Depression Inventory Questionnaire (score) | 8.76 ± 6.73 | 11.56 ± 8.18 | ns |
| Heart rate variability, mean ± SD | |||
| SDNN (ms) | 120 ± 28 | 126 ± 32 | ns |
| Log low frequency (ms2 Hz) | 5.93 ± 0.87 | 5.81 ± 0.77 | ns |
| Log high frequency (ms2 Hz) | 5.36 ± 1.02 | 5.33 ± 0.83 | ns |
| Low‐to‐high frequency ratio | 2.06 ± 1.14 | 2.01 ± 1.35 | ns |
| Cardiopulmonary exercise test, mean ± SD | |||
| Peak VO2 (ml/kg per minute) | 16.83 ± 3.73 | 17.89 ± 3.50 | ns |
| Treatment, n (%) | |||
| Beta‐blocker | 36 (100) | 15 (100) | ns |
| Angiotensin converting enzyme inhibitors | 40 (86.96) | 19 (82.61) | ns |
| Angiotensin receptor blockers | 6 (13.04) | 3 (13.04) | ns |
| Loop diuretics | 27 (58.70) | 13 (56.52) | ns |
| Aspirin | 36 (78.26) | 18 (78.26) | ns |
| Anticoagulants | 10 (21.74) | 6 (26.09) | ns |
| Statins | 37 (80.43) | 19 (82.61) | ns |
| Implantable cardioverter‐defibrillator | 29 (63.04) | 11 (47.83) | ns |
SD = standard deviation; ns = nonsignificant; NYHA = New York Heart Association class; SDNN = standard deviation of all normal RR intervals; log = logarithm; LF = low frequency; HF = high frequency; LF/HF = low‐to‐high frequency ratio; Peak VO2 = peak oxygen consumption; bpm = beat per minute.
Effects of Comprehensive Cardiac Telerehabilitation on HRV Parameters
There was a significant increase in vagal tone assessed by log HF (P = 0.0211), and significant decrease of sympathetic activity assessed by log LF (P = 0.0129) and in consequence improvement in sympathovagal balance evaluated by LF/HF ratio (P < 0.0001) only in the TG. We did not observe these favorable effects in the CG. Log HF and LF/HF ratio were statistically significant in between‐group analysis after adjustment for age, sex, diabetes, and undergone myocardial infarction, coronary artery bypass grafting (P = 0.0384 and <0.0001, respectively). The details are shown in Table 2.
Table 2.
Comparison of Outcomes before and after Comprehensive Cardiac Telerehabilitation Based on Nordic Walking Training in the Training Group (p1) and before and after Observation in the Control Group (p2) and between Groups—Group x Time Adjusted for Age, Sex, Diabetes, and Undergone Myocardial Infarction and Coronary Artery Bypass Grafting (p3)
| Training Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|
| Before | After | Before | After | ||||
| Training | Training | p 1 | Observation | Observation | p 2 | p 3 | |
| 24‐hour Holter ECG monitoring | |||||||
| SDNN (ms) | 120 ± 28 | 124 ± 27 | ns | 126 ± 32 | 126 ± 23 | ns | ns |
| Log LF (ms2/Hz) | 5.93 ± 0.87 | 5.67 ± 0.98 | 0.0129 | 5.81 ± 0.77 | 5.93 ± 0.87 | ns | ns |
| Log HF (ms2/Hz) | 5.36 ± 1.02 | 5.68 ± 0.94 | 0.0211 | 5.33 ± 0.83 | 5.24 ± 1.07 | ns | 0.0384 |
| LF/HF | 2.06 ± 1.14 | 1.19 ± 0.80 | <0.0001 | 2.01 ± 1.35 | 2.42 ± 1.39 | ns | <0.0001 |
| Beck Depression Inventory Questionnaire | |||||||
| BDI (score) | 8.76 ± 6.73 | 6.70 ± 5.53 | 0.0006 | 11.57 ± 8.18 | 9.09 ± 7.34 | 0.0490 | ns |
| Cardiopulmonary exercise test | |||||||
| peak VO2 (mL/kg per minute) | 16.83 ± 3.72 | 19.14 ± 4.20 | <0.0001 | 17.89 ± 3.50 | 17.63 ± 3.71 | ns | 0.0012 |
| HR rest (bpm) | 67 ± 10 | 67 ± 10 | ns | 67 ± 10 | 68 ± 10 | ns | ns |
| HR max (bpm) | 113 ± 17 | 122 ± 19 | 0.0001 | 120 ± 19 | 117 ± 15 | ns | 0.0088 |
| SBP rest (mm Hg) | 110 ± 14 | 113 ± 13 | ns | 113 ± 13 | 116 ± 14 | ns | ns |
| DBP rest (mm Hg) | 74 ± 8 | 75 ± 7 | ns | 75 ± 7 | 75 ± 6 | ns | ns |
| SBP max (mm Hg) | 134 ± 23 | 140 ± 22 | 0.0047 | 144 ± 24 | 142 ± 22 | ns | ns |
| DBP max (mm Hg) | 77 ± 9 | 78 ± 7 | ns | 80 ± 9 | 80 ± 6 | ns | ns |
Data presented are mean values ± standard deviation; statistical significance: P < 0.05; ns = nonsignificant; SDNN = standard deviation of all normal RR intervals; Log = logarithmic; LF = low frequency; HF = high frequency; LF/HF = low‐to‐high frequency ratio; Peak VO2 = peak oxygen consumption; HR = heart rate; bpm = beat per minute; SBP = systolic blood pressure; DBP = diastolic blood pressure.
Effects of Comprehensive Cardiac Telerehabilitation on Depression Symptoms
At baseline evaluation, depression was present in 35% of patients in the TG and 48% of patients in the CG. After an 8‐week Nordic walking training, depression receded (BDI score <10) in 15% of patients. In the CG, depression receded in 13% of patients. There were no significant differences in between‐group analysis after the adjustment for age, sex, diabetes, and undergone myocardial infarction, coronary artery bypass grafting in terms of reversing depression after training and observation. Nevertheless, there was a significant reduction in BDI score (which proves a decrease of depression symptoms, yet does not imply its reversion as patients did not reach the cut point <10) in the TG (P = 0.0006) and in the CG (P = 0.0490), which were not statistically significant in between‐group analysis after adjustment for age, sex, diabetes, and undergone myocardial infarction and coronary artery bypass grafting. The details are shown in Tables 2, 3, 4.
Table 3.
Psychological Status Results in Terms of Depression in Training Group
| The Results before the Nordic Walking Training | |||
|---|---|---|---|
| Nondepressed, n (%) | Depressed, n (%) | ||
| The results after the nordic walking training | Nondepressed, n (%) | 28 (61) | 7 (15) |
| Depressed, n (%) | 2 (4) | 9 (20) | |
Table 4.
Psychological Status Results in Terms of Depression in Control Group
| The Results before Observation | |||
|---|---|---|---|
| Nondepressed, n (%) | Depressed, n (%) | ||
| The results after observation | Nondepressed n (%) | 12 (52) | 3 (13) |
| Depressed n (%) | 0 (0) | 8 (35) | |
All the patients in TG were satisfied with the support which they received during home‐based telerehabilitation from nurses, physiotherapists, and physicians. In consequence they did not express the need for additional phone consultations with the psychologist.
Relationship between HRV Indices and Depression
Statistically significant changes in ΔLF/HF have been observed in the TG only in the following patient subgroups: with depression before and after the training (ΔLF/HF = –0.13), without depression before and after the training (ΔLF/HF = –0.7), and in the subgroup where depression reversed after the training (ΔLF/HF = –2.27) (Kruskal‐Wallis test; P = 0.0003). Therefore, the greatest sympathetic–parasympathetic balance improvement was observed in patients, where depression after the CCR based on Nordic walking training was reversed.
In addition, within the TG the baseline LF/HF comparative analysis proved that there was a statistically significant difference (P = 0.0028) between the subgroup where depression was reversed (LF/HF = 3.4 ± 1.2) and the subgroups with depression before and after the training and without depression before and after the training continued (LF/HF = 1.7 ± 0.8).
In the CG, no statistically significant changes in Δ LF/HF have been observed in the following patient subgroups: with depression before and after the training (ΔLF/HF = 0.71), without depression before and after the training (ΔLF/HF = –0.09), and in the subgroup where depression was reversed after the training (ΔLF/HF = 1.61) (Kruskal‐Wallis test; P = 0.0931).
Effectiveness of Comprehensive Cardiac Telerehabilitation Based on Nordic Walking Training
Nordic walking training resulted in a significant improvement in peak VO2 16.83 ± 3.72 versus 19.14 ± 4.20 ml/kg per minute (P < 0.0001). In CG there was no significant changes in peak VO2 17.89 ± 3.50 versus 17.63 ± 3.71 (P = 0.7805). Between‐group analysis showed that the differences between TG and CG were statistically significant in terms of Δpeak VO2, after adjustment for age sex, diabetes, and undergone myocardial infarction and coronary artery bypass grafting (P = 0.0012). The details are shown in Table 2.
Within the TG, the multivariate model evaluating the interaction between (1) ΔLF/HF ratio and ΔBDI score, (2) ΔLF/HF ratio and Δpeak VO2, and finally (3) ΔLF/HF ratio and the ΔBDI score combined with Δpeak VO2 proved that there have been statistically significant relations between the variables: (1) P < 0.0001, (2) P = 0.0020, and (3) P = 0.0024, respectively. Within this model, additional variables were included: age sex, diabetes, and undergone myocardial infarction and coronary artery bypass grafting. Only in TG, the improvement in ΔLF/HF ratio was associated with the improvement in exercise capacity and the reduction of depressive symptoms. In CG, no such relationship was observed.
DISCUSSION
We are aware of the fact that the study group was small and the results obtained represent the characteristics of a preliminary study. Nonetheless, we believe that our research hypothesis is interesting enough to present value in terms of discussion.
The main findings of this ancillary study were the demonstration that the improvement of sympatho‐parasympathetic balance obtained through CCR results from the additive effects of the reversion of depression and increased physical capacity.
The greatest improvement of sympathovagal balance was observed in patients whose depression was reversed because the CCR based on Nordic walking training. These results were qualified as excellent in the course of comparison with the results of other patients from the TG: those whose depression was not reversed thanks to the CCR program and those who did not suffer from this mental illness in the first place. The phenomenon of particularly impressive improvement of sympathovagal balance among patients whose mental illness receded was not observed in patients from the CG.
In articles published so far, the object of the evaluation was the influence of rehabilitation on ANS function and on depression separately.
Exercise Training and HRV
Although there are no articles on the influence of Nordic walking training on HRV, it would result of great value to take a closer look at works which demonstrate the influence of other modalities of exercise training on HRV in CHF patients.20, 21, 22, 23, 24, 25
Simultaneous improvement of all HRV parameters (time domain and frequency domain) was not always observed. Selig, for example, reported the decrease of LF and LF/HF, but did not observe any changes in SDNN.26 We have obtained similar results in our work.
Adamopoulos et al., on the contrary, reported that in CHF, physical training maintains and improves circadian variations in HRV measures.23 In another study, the authors demonstrated an improvement in autonomic balance (increases in HF and decreases in LF and LF/HF ratio) after 8 weeks of physical training at home.27Our results are consistent with these outcomes.
Furthermore, Ponikowski et al. proved that the ventilatory response to exercise correlated with impaired HRV in patients with CHF. These findings indicate a potential link between functional severity and sympathovagal imbalance in CHF.28
Similarly to our findings Kiilavuori et al. and Pietila et al. observed a significant increase in CHF indices after exercise training in CHF patients.29, 30
Our results are also concordant with the study conducted by Malfato et al. which showed significant improvement in both ANS function and physical capacity after cardiac rehabilitation.22
Published data indicated that exercise training restores ANS function by increasing vagal tone and decreasing sympathetic activity which lead to parasympathetic–sympathetic balance improvement in CHF patients. 20 –34
Exercise Training and Depression
Another issue is the influence of cardiac rehabilitation on patients suffering both from depression and heart failure.
The HF‐ACTION subanalysis showed that exercise training resulted in a modest reduction in depressive symptoms as evaluated by the BDI‐II score.4
Another recently published meta‐analysis on the topic has proven that exercise training had beneficial effects on freeing the CHF patients from depression symptoms.5 The influence of Nordic walking on depression symptoms in CHF patients has not been evaluated. Nevertheless, according to the studies which evaluated patient groups without heart failure, Nordic walking has proven to increase patients’ motivation to perform physical activity, enhance their fitness, and improve their mood.9 In our study we have also observed a substantial reduction of depressive symptoms (decrease in the number of points in the BDI score) within the TG and depression was reversed in 15% of patients from this group. These results were insufficient to obtain a statistically significant difference in terms of reducing depression symptoms within the TG as compared with the CG. In the CG we have also observed a significant reduction in the number of points in the BDI score and depression was reversed in 13% of the patients (cut point for depression diagnose ≥ 10 point in BDI score).
Reversion of Depression and the Improvement of the Sympatho‐Parasympathetic Balance after Comprehensive Cardiac Telerehabilitation
The articles published so far have not analyzed the additive effects resulting from the physical capacity improvement (pVO2) and recovery from depression on the sympatho‐parasympathetic balance.
The results of our study prove that the reversion of depression in the TG has significantly intensified the beneficial change of the sympathovagal balance in comparison with the rest of the patients both from the TG as well as the CG.
For this reason there seem to exist premises to believe that this phenomenon is the result of additive effects of physical capacity improvement (objectively measured by peak VO2) and the effects of the reversion of depression (i.e., achieved cut point for reversion of depression <10 point in BDI score) in the course of the CCR based on Nordic walking training.
The ANS dysfunction is affected both by the CHF advancement level as the depression which accompanies it. The pleiotropic effects of exercise training, on the contrary, encompasses both the improvement of physical capacity parameters and the improvement of the mental health, which positively affects the sympathovagal balance.
The question at hand is clearly the reason behind this phenomenon. There are three valid explanations that could be taken into consideration: (1) more intense (accumulated) disruption of the sympatho‐parasympathetic balance in the patient group with CHF and depression at the beginning of the study, (2) the influence of depression related therapy on the ANS function, and (3) the beneficial effects of a specific form of exercise training which is Nordic walking.
Our study demonstrated that in the TG subgroup of patients whose depression was reversed after the training, baseline analysis was characterized by the highest ANS dysfunction (negative additive effects of heart failure and depression). This might have been the reason why the improvement of those two negative factors after the training resulted in the positive additive effect.
Antidepressants capable of affecting ANS function have not been used in either group. Nevertheless, it is impossible to rule out the influence of the psychological procedures applied in the TG and not used in the CG on the effects of the study. However, taken into account the fact that the depressing symptoms receded in the CG, it is imperative to qualify it as spontaneous improvement during the study.
It is obvious that, thanks to Nordic walking, most muscles are being activated and patients obtain fitness building stimulation absent in other training modalities such as cycling or simple walking. In addition, this specific modality incorporates components of resistance training thanks to the “grip and release” of the poles technique. Moreover, during the breaks in the Nordic walking training, breathing and light stretching exercise can be performed as complementary exercise modality. There is no evidence that these specific characteristics of Nordic walking had influence on the accumulated improvement of the sympathovagal balance among patients who recovered from depression.
It needs to be emphasized, however, that the results presented in our study, because of the limited number of its participants, can be considered typical of a preliminary study, and the presented hypotheses require confirmation in the course of further studies.
Limitation
We acknowledge that it was an ancillary study, and thus the group studied was not particularly large. On one hand, this might be considered a limitation to the study; on the other, it is possible that as we were able to obtain statistically significant results it would be legitimate to conduct further research in this specific field. In order to assess HRV with precision we only focused on patients with sinus rhythm, and we excluded patients dependent on pacing, which caused that the number of patients included in the anicillary study diminished. Another limitation is the evaluation of selected parameters from 24‐hour holter ECG monitoring. We are aware that BDI questionnaire is a short and relatively old test for depression assessment and more expensive and up‐to‐date tests are available.
The training in this study lasted only 8 weeks. The majority of the study group consisted of males, and for this reason the results are not fully valid for the female population. Because we were unable to determine the number of patients who were able to maintain their improvement, it is necessary to add the lack of long term follow‐up as the final limitation.
CONCLUSION
Positive effect of the sympatho‐parasympathetic balance obtained during the home comprehensive cardiac telerehabilitation based on Nordic walking training results from the additive effects of the reversion of depression and physical capacity improvement in CHF patients.
Acknowledgments
We wish to express our thanks to psychologists, ECG technicians, and physiotherapists for their help in conducting the study.
The study was supported by the National Science Centre, Poland—Grant no. NN404 107936.
Conflict of interest: None declared.
REFERENCES
- 1. Grippo AJ, Johnson AK. Biological mechanisms in the relationship between depression and heart disease. Neurosci Biobehav Rev 2002:26:941–962. [DOI] [PubMed] [Google Scholar]
- 2. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure: A meta‐analytic review of prevalence intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006:48:1527–1537. [DOI] [PubMed] [Google Scholar]
- 3. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur Heart J 2012:33(14):1787–1869. [DOI] [PubMed] [Google Scholar]
- 4. Blumenthal JA, Babyak MA, O'Connor C, et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure: The HF‐ACTION randomized trial. JAMA 2012:308(5):465–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tu RH, Zeng ZY, Zhong GQ, et al. Effects of exercise training on depression in patients with heart failure: a systematic review and meta‐analysis of randomized controlled trials. Eur J Heart Fail 2014:16(7):749–757.. [DOI] [PubMed] [Google Scholar]
- 6. Routledge FS, Campbell TS, McFetridge‐Durdle JA, et al. Improvements in heart rate variability with exercise therapy. Can J Cardiol 2010:26(6):303–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gademan MGJ, Swenne CA, Verwey HF, et al. Effect of exercise training on autonomic derangement and neurohumoral activation in chronic heart failure. J Cardiac Fail 2007:13(4):294–303. [DOI] [PubMed] [Google Scholar]
- 8. Braith RW, Edwards DG. Neurohormonal abnormalities in heart failure: impact of exercise training. Congest Heart Fail 2003:9(2):70–76. [DOI] [PubMed] [Google Scholar]
- 9. Suija K, Pechter U, Kalda R, et al. Physical activity of depressed patients and their motivation to exercise: Nordic walking in family practice. Int J Rehabil Res 2009:32(2):132–138. [DOI] [PubMed] [Google Scholar]
- 10. Tschentscher M, Niederseer D, Niebauer J. Health benefits of Nordic walking: a systematic review. Am J Prev Med 2013:44(1):76–84. [DOI] [PubMed] [Google Scholar]
- 11. Piotrowicz E, Zieliński T, Bodalski R, et al. Home‐based telemonitored Nordic walking training is well accepted, safe, effective and has high adherence among heart failure patients, including those with cardiovascular implantable electronic devices–a randomized controlled study. Eur J Prev Cardiol. 2015: 22(11): 1368–1377. [DOI] [PubMed] [Google Scholar]
- 12. Piepoli MF, Conraads V, Corra U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the HFA and the EACPR. Eur J Heart Fail 2011:13(4):347–357. [DOI] [PubMed] [Google Scholar]
- 13. Schmidt G, Malik M, Barthel P, et al. Heart‐rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction. Lancet 1999:353:1390–1396. [DOI] [PubMed] [Google Scholar]
- 14. Piepoli MF, Corrà U, Agostoni PG, et al. Statement on cardiopulmonary exercise testing in chronic heart failure due to left ventricular dysfunction: Recommendations for performance and interpretation Part II: How to perform cardiopulmonary exercise testing in chronic heart failure. Eur J Cardiovasc Prev Rehabil 2006:13(3):300–311. [DOI] [PubMed] [Google Scholar]
- 15. Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual, 2 nd ed San Antonio, TX, Psychological Corp, 1996. [Google Scholar]
- 16. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982:14(5):377–381. [PubMed] [Google Scholar]
- 17. Piotrowicz E. How to do telerehabilitation in heart failure patients. Cardiol J 2012:19(3):243–248. [DOI] [PubMed] [Google Scholar]
- 18. Piotrowicz E, Baranowski R, Bilinska M, et al. A new model of home‐based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence. Eur J Heart Fail 2010:12(2):164–171. [DOI] [PubMed] [Google Scholar]
- 19. Piotrowicz E, Jasionowska A, Banaszak‐Bednarczyk M, et al. ECG telemonitoring during home‐based cardiac rehabilitation in heart failure patients. J Telemed Telecare 2012:18:193–197. [DOI] [PubMed] [Google Scholar]
- 20. Piotrowicz E, Baranowski R, Piotrowska M, et al. Variable effects of physical training of heart rate variability, heart rate recovery, and heart rate turbulence in chronic heart failure. Pacing Clin Electrophysiol 2009:32 1:S113–S115. [DOI] [PubMed] [Google Scholar]
- 21. Gademan MGJ, Swenne CA, Verwey HF, et al. Effect of exercise training on autonomic derangement and neurohumoral activation in chronic heart failure. J Cardiac Fail 2007:13:294–303. [DOI] [PubMed] [Google Scholar]
- 22. Malfatto G, Branzi G, Riva B, et al. Recovery of cardiac autonomic responsiveness with low‐intensity physical training in patients with chronic heart failure. Eur J Heart Fail 2002:4:159–166. [DOI] [PubMed] [Google Scholar]
- 23. Adamopoulos S, Ponikowski P, Cerquetani E, et al. Circadian pattern of heart rate variability in chronic heart failure patients: effects of physical training. Eur Heart J. 1995:16(10):1380–1386. [DOI] [PubMed] [Google Scholar]
- 24. Coats AJ, Adamopoulos S, Radaelli A, et al. Controlled trial of physical training in chronic heart failure. Exercise performance, hemodynamics, ventilation, and autonomic function. Circulation 1992:85(6):2119–2131. [DOI] [PubMed] [Google Scholar]
- 25. Larsen AI, Gjesdal K, Hall Ch, et al. Effect of exercise training in patients with heart failure: a pilot study on autonomic balance assessed by heart rate variability. Eur J Cardiovasc Prev Rehabil 2004:11:162–167. [DOI] [PubMed] [Google Scholar]
- 26. Selig SE, Carey MF, Menzies DG, et al. Moderate‐intensity resistance exercise training in patients with chronic heart failure improves strength, endurance, heart rate variability, and forearm blood flow. J Cardiac Fail 2004:10:21–30. [DOI] [PubMed] [Google Scholar]
- 27. Adamopoulos S., Piepoli M., McCance A. i wsp. Comparison of different methods for assessing sympathovagal balance in chronic congestive heart failure secondary to coronary artery disease.Am J Cardiol 1992:70:1576–1582. [DOI] [PubMed] [Google Scholar]
- 28. Ponikowski P, Chua TP, Piepoli M, et al. Ventilatory response to exercise correlates with impaired heart rate variability in patients with chronic congestive heart failure. Am J Cardiol 1998:82(3):338–344. [DOI] [PubMed] [Google Scholar]
- 29. Kiilavuori K, Toivonen L, Naveri H, et al. Reversal of autonomic derangements by physical training in chronic heart failure assessed by heart rate variability. Eur Heart J 1995:16:490–495. [DOI] [PubMed] [Google Scholar]
- 30. Pietilä M, Malminiemi K, Vesalainen R, et al. Exercise training in chronic heart failure: beneficial effects on cardiac (11)C‐hydroxyephedrine PET, autonomic nervous control, and ventricular repolarization. J Nucl Med 2002:43(6):773–779. [PubMed] [Google Scholar]
- 31. Murad K, Brubaker PH, Fitzgerald DM, et al. Exercise training improves heart rate variability in older patients with heart failure: a randomized, controlled, single‐blinded trial. Congest Heart Fail 2012:18(4):192–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Iellamo F, Manzi V, Caminiti G, et al. Dose‐response relationship of baroreflex sensitivity and heart rate variability to individually‐tailored exercise training in patients with heart failure. Int J Cardiol 2013:166(2):334–339. [DOI] [PubMed] [Google Scholar]
- 33. Grant CC, Viljoen M, Janse van Rensburg DCJ, et al. Heart rate variability assessment of the effect of physical training on autonomic cardiac control. Ann Noninvasive Electrocardiol 2012:17(3):219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]


