Abstract
Objectives
The aim of this study was to evaluate the prognostic value of fragmented QRS (fQRS) on electrocardiography (ECG) patients with acute ST‐segment elevation in myocardial infarction (STEMI), who are undergoing primary percutaneous coronary intervention (PCI).
Methods
We prospectively enrolled 414 consecutive STEMI patients (mean age of 55.2 ± 12.2 years old, range of 26–91‐years old) undergoing primary PCI. The study patients were divided into two groups according to the presence or absence of fQRS as shown by ECG in the first 48 hours. The presence of fQRS group was defined as fQRS(+) (n = 91), and the absence of fQRS group was defined as the fQRS(–) (n = 323) group. Clinical characteristics and the one‐year outcome of the primary PCI were analyzed.
Results
The patients in the fQRS(+) group were older (mean age 60.7 ± 12.5 vs. 53.6 ± 11.6 years old, P < 0.001). Higher one‐year all‐cause mortality rates were observed in the fQRS group upon ECG (23.1% vs. 2.5%, P < 0.001, respectively). When using the Cox multivariate analysis, the presence of fQRS on the ECG was found to be a powerful independent predictor of one‐year all‐cause mortality (hazard ratio: 5.24, 95% confidence interval: 1.43–19.2, P = 0.01).
Conclusions
These results suggest that the presence of fQRS on ECG was associated with an increased in‐hospital cardiovascular mortality, and one‐year all‐cause mortality in patients with STEMI who are under primary PCI.
Keywords: ST elevation myocardial infarction, primary angioplasty, fQRS
Coronary artery disease (CAD) remains a leading cause of human morbidity and mortality. Consequently, the risk stratification is a very important issue in healthcare to prevent and manage CAD. 1, 2, 3
Improved electrocardiographic criteria for the early diagnosis of myocardial infarction (MI) episodes are needed. These include Q wave, QRS disturbances, persistent ST‐segment elevations, and bundle branch blockages.4 However, the prognostic significance of these findings for adverse cardiovascular outcomes has not been fully clarified for post‐MI.5 In this study, we researched the value of the fragmented QRS (fQRS) on ECG patients with ST segment elevation myocardial infarctions (STEMI), for subsequent adverse cardiovascular events. It is likely that the fQRS reflects the varied conduction abnormalities and the delay of peri‐infarct conductions due to myocardial necrosis or scarring.6, 7, 8 A few good studies have shown that fQRS appears approximately 24–48 hours after the onset of symptoms or after diagnosis and subsequently to MI necrosis.6 Recent studies have also reported that fQRS is an indicator of adverse cardiac events in patients with CAD.9, 10 Likewise, the relationships between structural heart disease, cardiac arrhythmias, and the presence of fQRS on the ECG were shown in many studies.7, 8, 11 Based on the results of these studies, the fQRS may be included as a new risk factor for patients with ACS.
To the best of our best knowledge, the prognostic significance of fQRS on ECG in patients with STEMI has not been evaluated prospectively with a large study and long term follow‐up. In this potential study, we hypothesized that the presence of fQRS would be associated with in‐hospital and one‐year adverse outcomes after primary PCIs for STEMI.
METHODS
Patient Population
In this prospective observational study, we included 532 consecutive patients with acute STEMI presenting to the Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Center, Training and Research Hospital, between December 2010 and March 2012. The study inclusion criteria were as follows: electrocardiography (ECG) revealing STEMI, which was defined as >30 minutes of continuous typical chest pain and ST‐segment elevation ≥2 mm in two contiguous ECG leads within 12 hours of symptom onset or for up to 18 hours if there was evidence of continuing ischemia or hemodynamic instability. We excluded 118 patients from our analysis; no indication for PCI (n = 10); not suitable for PCI (n = 8); a previous MI history (n = 82), or a history of sudden death patients (under cardiopulmonary resisutasyon) died within the first hours in the catheter room and therefore we had no chance to obtain a good ECG that can be evaluated for fQRS on the 12 leads ECG (n = 3), and presence of complete or incomplete bundle branch block and paced rhythm (n = 15). Therefore, the final study population consisted of 414 patients. Study patients were divided into two groups according to the presence or absence of fQRS on ECG at first 48th hours. Presence fQRS group (n = 323) was defined as a fQRS(+), and a absence fQRS group (n = 91) was defined as a fQRS(–) groups.
All primary PCI procedures were performed in a single high‐volume tertiary care center (>3000 PCI/year) by expert operators who carry out an average of >75 PCI/year. The study protocol was approved by the hospital's Ethics Committee.
Analysis of Patient Data
On admission, the patients’ medical histories and a special questionnaire on lifestyle and risk factors were taken. Reperfusion time and door‐to‐balloon time were also recorded. And also complete blood counts and other serum values were determined on admission before catheterization procedures. A 12‐lead ECG was recorded in each patient just after hospital admission, and the MI type was also obtained from the ECGs. At 24 to 72 hours after revascularization, a transthoracic echocardiographic study was performed using a GE Vivid S6 Vingmed S5 (Horten, Norway) with a 1.7/3.4 MHz phased‐array transducer, and the left ventricular ejection fraction (LVEF) was calculated using the biplane Simpson method.12 The GFR was estimated by the simplified Modification of Diet in Renal Disease (MDRD) equation.13
Electrocardiography
A 12‐derivations surface ECG was obtained from all patients in the supine position immediately after their admission to the emergency room. ECG records were taken by Nihon Kohden – cardiofax S(ECG‐1250K, filter range 0.5 Hz to 150 Hz, AC filter 60 Hz, at a speed of 25 mm/s and an amplitude of 10 mm/mV) at first 48th hours.
The presence or absence of a fQRS was evaluated by means of the examination of ECG records by two independent readers blinded to cardiac markers, coronary angiography, and clinical outcomes. The interobserver concordance rate with regard to detecting the presence of fQRS was 96.8% (j = 0.93) between the two readers. The intraobserver concordance rate was 98.9% (j = 0.97). If two independent observers could not reach to an agreement, the third independent observer was included in the decision making, and two out of three agreement was accepted as the final decision.
fQRS was defined as the presence of an extra R wave (R1) in a 12‐lead ECG, the presence of notching on an R wave, the presence of notching on an S wave, or presence of more than one R1 wave in two adjacent derivations corresponding to the feeding area of one of the major coronary arteries.6 An example of fQRS on 12‐lead ECG was showed in Figure 1. Complete and incomplete bundle branch block and paced rhythm were excluded from the definition of fQRS.
Figure 1.
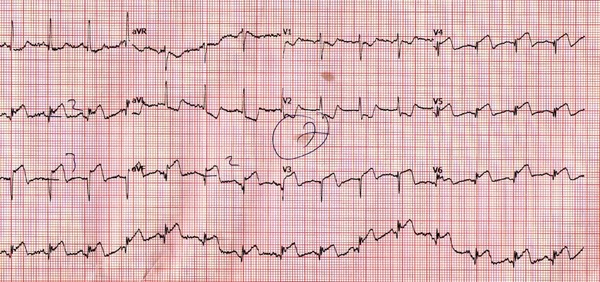
A 73‐year‐old woman died on the 29th day after discharge. fQRS could be seen in lead D2, D3, AVF, V4, V5, and V6.
Coronary Angiography, Primary Angioplasty, and Stenting
All patients received a chewable 300 mg aspirin and clopidogrel (600 mg loading dosage) before coronary angiography. Angiographic data of the patients were evaluated from catheter laboratory records. Emergency coronary angiography and angioplasty were performed by the percutaneous femoral approach. A nonionic, iso‐osmolal contrast media was used in all patients. The artery that was presumed to be unobstructed was injected first. Blood flow in the infarct‐related artery (IRA) was graded according to the Thrombolysis in Myocardial Infarction (TIMI) classification.14 Heparin (100 IU/kg) was administered when the coronary anatomy was first defined.
After visualizing the left and right coronary arteries, 2.5 μg of nitrate was selectively injected into the IRA to rule out a possible coronary spasm. An angiographic evaluation was made by visual assessment. Primary angioplasty (including balloon angioplasty and/or stent implantation) was performed only for IRA according to lesion type. For each procedure, interventional success at the acute phase was defined as reducing to <30% of obstruction and stenosis of the IRA with TIMI 3 flow just after primary angioplasty. After angioplasty, all patients were admitted to the coronary care unit, where 100 mg aspirin and 75 mg clopidogrel were continued in all patients. The use of glycoprotein IIb/IIIa inhibitors was left to the discretion of the operator.
DEFINITION
Reperfusion time was measured as the time from symptom onset until coronary reperfusion was obtained with balloon inflation. The door‐to‐balloon time was defined as the time between hospital admission and balloon inflation. Patients were evaluated according to the Killip clinical examination classification.15 Advanced heart failure was defined as New York Heart Association (NYHA) classification ≥3. Anemia was set as a baseline hemoglobin concentration <13 g/dL in males and <12 g/dL in females. Renal failure was defined as a GFR <60 mL/min per 1.73m2, which was estimated by the MDRD equation.13 Patients with diabetes mellitus (DM) were determined to be those with documented DM currently using either oral hypoglycemic agents or insulin treatment at admission. Cardiovascular mortality was defined as unexplained sudden death, death due to acute STEMI, heart failure, or arrhythmia. We set the repeat target vessel revascularization (TVR) as the need for PCI or coronary surgery because of restenosis or reocclusion of the IRA. Major adverse cardiac events (MACE) were defined as cardiovascular mortality, reinfarction, or repeat TVR (percutaneous or surgical). Reinfarction was described as an universal definition of MI. 16
Follow‐Up
Follow‐up data were obtained from hospital records or by interviewing (directly or by telephone) patients, their families, or their personal physicians.
Statistical Analysis
Quantitative variables were expressed as mean value ± SD, and qualitative variables were shown as a percentage (%). The comparison of parametric values between the two groups was performed using a two‐tailed Student's t‐test. Categorical variables were compared by the likelihood‐ratio χ2 test or the Fisher's exact test. Target sample size for the study was found by using a two‐sided test for a statistical power (1–ß) of 80% and an α of 0.05. To assure these goals, we calculated that the sample size should be 400 patients. The cumulative survival curve for one‐year all‐cause mortality was constructed using the Kaplan‐Meier method, with differences assessed with log‐rank tests. A backward stepwise Cox multivariate analysis, which included variables with P < 0.1, was performed to identify independent predictors of one‐year all‐cause mortality. And also a backward stepwise logistic multivariate regression analysis, which included variables with P < 0.1, was performed to identify independent predictors of in‐hospital cardiovascular mortality. A P‐value <0.05 was considered statistically significant. All statistical studies were carried out with the Statistical Package for the Social Sciences (SPSS) software program (version 15.0, SPSS, Chicago, IL, USA).
RESULTS
Baseline Characteristics
The baseline characteristics of patients are listed in Table 1. Patients in the fQRS(+) group were older (mean age 60.7± 12.5 vs. 53.6± 11.6, P < 0.001). Compared to the fQRS(–) group, female gender, DM, HT, HL, and Killip class >1 at admission were more prevalent in the fQRS(+) group. PCI history, bypass history, anterior MI, reperfusion time, and door to balloon time were not statistically different between the two groups. QRS duration was significantly higher in fQRS(+) group.
Table 1.
Baseline Demographic, Clinical and Laboratory Characteristics of Patients
| fQRS (–) | fQRS(+) | ||
|---|---|---|---|
| Variable | (n = 323) | (n = 91) | P Value |
| Age, years (SD) | 53.6 ± 11.6 | 60.7 ± 12.5 | <0.001 |
| Female gender, n (%) | 54 (16.7) | 32 (35.2) | <0.001 |
| DM, n (%) | 22 (6.8) | 55 (60.4) | <0.001 |
| Reperfusion time, minutes (SD) | 249.6 ± 147.3 | 244.8 ± 109.4 | 0.78 |
| Door‐to‐balloon time, minutes (SD) | 42.1 ± 15.6 | 44.1 ± 14.9 | 0.3 |
| Peak CK‐MB, IU/L (SD) | 143.2 ± 137.2 | 156.3 ± 147.8 | 0.44 |
| Culprit lesion | 0.21 | ||
| LMCA, n (%) | 0 (0) | 0 (0) | |
| LAD, n (%) | 154 (47.7) | 35 (38.5) | |
| CX, n (%) | 39 (12.1) | 9(9.9) | |
| RCA, n (%) | 128 (39.6) | 47 (51.6) | |
| Others, n (%) | 2 (0.6) | 0 (0) | |
| Three‐vessel disease, n (%) | 59 (18.3) | 38 (41.8) | 0.01 |
| Post TIMI III flow, n (%) | 301 (93.2) | 84 (92.3) | 0.34 |
| Stent usage, n (%) | 295 (91.3) | 83 (91.2) | 0.71 |
| Tirofiban usage, n (%) | 103 (31.9) | 28 (30.8) | 0.97 |
| QRS duration, msn | 88 ± 14 | 94 ± 12 | <0.001 |
CK‐MB = creatinine kinase‐MB; CX = circumflex coronary artery; DM = diabetes mellitus; HL = hyperlipidemia; LAD = left anterior descending coronary artery; LMCA = left main coronary artery; MI = myocardial infarction; PCI = percutaneous coronary intervention; RCA = right coronary artery; SD = standart deviation; TIMI = Thrombolysis in Myocardial Infarction.
Laboratory Findings
Patients’ laboratory data demonstrated in Table 1. Higher baseline blood creatinine was observed in the fQRS(+) group than fQRS(–) group. Anemia at admission and renal failure were more prevalent in fQRS(+) group compared to fQRS(–) group. Peak CK‐MB was not statistically different between the two groups.
Angiographic and Procedural Characteristics
Angiographic and procedural characteristics are depicted in Table 1. Culprit lesions were similar in the two groups. Compared to the fQRS(–) group, three‐vessel disease was more prevalent in the fQRS(+) group. Stent usage, post‐TIMI III flow, and tirofiban usage were not statistically different between the two groups.
In‐Hospital Outcomes
Table 2 presents the in‐hospital outcomes after primary PCI. The fQRS(+) group had a significantly higher incidence of in‐hospital cardiovascular mortality than the fQRS(–) group (15.4% vs. 0.6%, respectively, P < 0.001). Advanced heart failure, MACE, cardiopulmonary resuscitation, inotrop usage, cardiogenic shock, transient pace, VT/VF, intra‐aortic balloon pump usage, blood transfusion, gastrointestinal bleeding, ventilator necessity, and lower LVEF were more frequent in fQRS(+) group. Independent predictors of in‐hospital cardiovascular mortality were determined by a backward stepwise logistic regression multivariate analysis. These predictors of in‐hospital cardiovascular mortality are depicted in Table 3. fQRS(+) group, post‐TIMI III flow< III, and LVEF < 40% were found to be independent predictors of in‐hospital cardiovascular mortality.
Table 2.
In‐Hospital Cardiac Events of All Study Patients
| fQRS | fQRS (+) | ||
|---|---|---|---|
| Variable | (n = 323) | (n = 91) | P Value |
| Cardiovascular mortality, n (%) | 2 (0.6) | 14 (15.4) | <0.001 |
| Reinfarction, n (%) | 16 (5) | 4 (4.4) | 0.84 |
| Target‐vessel revascularization, n (%) | 17 (5.3) | 4 (4.4) | 0.75 |
| MACE, n (%) | 20 (6.2) | 15 (16.5) | 0.002 |
| Stroke, n (%) | 2 (0.6) | 1 (1.1) | 0.63 |
| Cardiopulmonary resuscitation, n (%) | 6 (1.9) | 15 (16.5) | <0.001 |
| Dialysis, n (%) | 1 (0.3) | 1 (1.1) | 0.33 |
| Advanced heart failure, n (%) | 15 (4.6) | 19 (20.9) | <0.001 |
| Cardiogenic shock, n (%) | 5 (1.5) | 14 (15.4) | <0.001 |
| İnotrop usage, n (%) | 10 (3.1) | 17 (18.7) | <0.001 |
| IABP usage, n (%) | 7 (2.2) | 7 (7.7) | 0.009 |
| Transient pace, n (%) | 6 (1.9) | 6 (6.6) | 0.01 |
| Blood transfusion | 0 (0) | 2 (2.2) | 0.007 |
| Ventilator necessity | 3 (0.9) | 12 (13.2) | <0.001 |
| Acute thrombosis, n (%) | 17 (5.3) | 4 (4.4) | 0.75 |
| Gastrointestinal bleeding, n (%) | 0 (0) | 2 (2.2) | 0.007 |
| LVEF,% (SD) | 49± 8 | 43.9± 10 | <0.001 |
| VT /VF, | 19 (5.9) | 16 (17.6) | 0.01 |
IABP = intra‐aortic balloon pump; LVEF = left ventricular ejection fraction; MACE = major adverse cardiac events (cardiovascular mortality, reinfarction, target‐vessel revascularization); SD = standard deviation; VF = ventricular fibrillation; VT = ventricular tachycardia.
Table 3.
Effects of Multiple Variables on The In‐Hospital Cardiovascular Mortality in Univariate and Multivariate Logistic Regression Analyses
| Univariate OR | 95% CI | P value | Multivariate OR | 95%CI | P Value | |
|---|---|---|---|---|---|---|
| Age | 1.073 | 1.031–1.116 | 0.001 | |||
| Female gender | 4.75 | 1.67–13.5 | 0.003 | |||
| DM | 4.82 | 1.75–13.3 | 0.002 | |||
| Hypertension | 4.04 | 1.43–11.4 | 0.008 | |||
| Killip class >1 | 15.65 | 5.39–45.5 | <0.001 | |||
| Current smoker | 0.29 | 0.11–0.83 | 0.02 | |||
| fQRS (+) | 29.6 | 6.6–132.5 | <0.001 | 24.4 | 3.98–149.9 | <0.001 |
| Post‐TIMI flow < III | 9.4 | 2.96–30 | <0.001 | 9.1 | 1.54–53.7 | 0.01 |
| EF <%40 | 23.3 | 6.4–85.3 | <0.001 | 13.8 | 2.98–63.8 | <0.001 |
CI = confidence interval; DM = diabetes mellitus; fQRS = fragmented QRS complex; LVEF = left ventricular ejection fraction; OR = odds ratio; TIMI = Thrombolysis in Myocardial Infarction.
One‐Year Outcomes
One‐year outcomes are depicted in Table 4. The fQRS(+) group had significantly higher incidence of all‐cause mortality and cardiovascular mortality than the fQRS(–) group (23.1% vs. 2.5%, respectively, P < 0.001, and 24.2% vs. 2.2% respectively, P < 0.001). Fatal reinfarction, advanced heart failure, TVR, and MACE were more frequent in fQRS(+) group. And also the Kaplan‐Meier survival plot for one‐year all‐cause mortality is presented in Figure 2. Independent predictors of one‐year all‐cause mortality were determined by a backward stepwise Cox multivariate analysis. These predictors of all‐cause mortality are depicted in Table 5. Age, fQRS(+) group, post‐TIMI III flow< III, and LVEF < 40% were found to be independent predictors of one‐year all‐cause mortality.
Table 4.
One‐Year Events of All Study Patients
| fQRS (–) | fQRS (+) | ||
|---|---|---|---|
| variable | (n = 323) | (n = 91) | P Value |
| All‐cause mortality, n (%) | 8 (2.5) | 21 (23.1) | <0.001 |
| Cardiovascular mortality, n (%) | 7 (2.2) | 22 (24.2) | <0.001 |
| Noncardiac mortality, n (%) | 1 (0.3) | 1 (1.1) | 0.34 |
| Fatal reinfarction, n (%) | 4 (1.2) | 9 (9.9) | <0.001 |
| Nonfatal reinfarction, n (%) | 17 (5.3) | 10 (11) | 0.05 |
| Target‐vessel revascularization, n (%) | 30(9.3) | 16(17.6) | 0.03 |
| Stroke, n (%) | 5 (1.5) | 2 (2.2) | 0.67 |
| Advanced heart failure, n (%) | 40 (12.4) | 30 (33) | <0.001 |
| MACE, n (%) | 39 (12.1) | 37 (40.7) | <0.001 |
MACE = major adverse cardiac events (cardiovascular mortality, reinfarction, target‐vessel revascularization).
Figure 2.
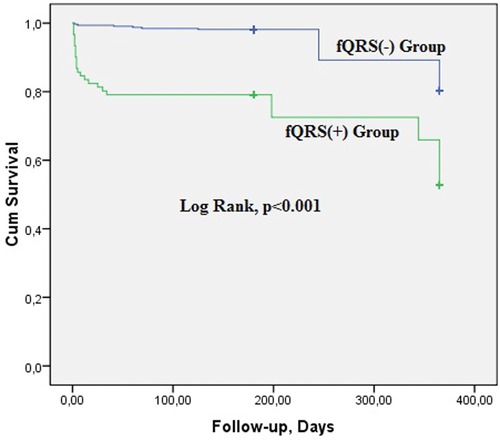
All‐cause mortality ratios of subgroups in one‐year follow‐up.
Table 5.
Effects of Multiple Variables on the One‐Year All‐Cause Mortality in Univariate and Multivariate Cox Regression Analyses
| Univariate HR | 95% CI | P Value | Multivariate HR | 95%CI | P Value | |
|---|---|---|---|---|---|---|
| Age | 1.063 | 1.034–1.093 | <0.001 | 1.045 | 1–1.093 | 0.05 |
| Female gender | 2.85 | 1.36–5.97 | 0.005 | |||
| DM | 3.3 | 1.57–6.9 | 0.002 | |||
| Hypertension | 2.2 | 1.06–4.55 | 0.03 | |||
| Killip class >1 | 10.4 | 4.93–21.7 | <0.001 | |||
| Current smoker | 0.34 | 0.16–0.72 | 0.005 | |||
| fQRS (+) | 10.6 | 4.71–24 | <0.001 | 5.24 | 1.43–19.2 | 0.01 |
| Post‐TIMI flow < III | 5.1 | 2.07–12.5 | <0.001 | 6.7 | 1.95–23.1 | 0.002 |
| Renal failure | 4.66 | 1.71–12.7 | 0.003 | |||
| EF <%40 | 13.1 | 5.17–33.3 | <0.001 | 8.9 | 2.7–29.5 | <0.001 |
| Anemia | 3.18 | 1.4–7.2 | 0.006 |
CI = confidence interval; DM = diabetes mellitus; fQRS = fragmented QRS complex; HR = hazard ratio; LVEF = left ventricular ejection fraction; TIMI = Thrombolysis in Myocardial Infarction.
Predictive Value
Presence of fQRS has a strong negative predictive value in predicting in hospital cardiovascular mortality and one‐year all‐cause mortality (Table 6).
Table 6.
Sensitivity, Specificity, Positive Predictive, and Negative Predictive Value for In‐Hospital Cardiovascular Mortality and On‐Year All‐Cause Mortality
| In‐Hospital | All‐Cause | |
|---|---|---|
| Cardiovascular | One‐Year | |
| Mortality | Mortality | |
| Sensitivity | 87.5 | 74.2 |
| Specificity | 81.9 | 82.2 |
| Positive predictive value | 15.4 | 25.3 |
| Negative predictive value | 99.4 | 97.5 |
DISCUSSION
The main findings of the present single‐center study are as follows:
The patients in the fQRS(+) group were predominately female with a higher prevalence of DM, hypertension (HT), hyperlipidemia (HL), renal failure, lower LVEF, higher serum glucose level at admission, three‐vessel disease, anemia upon admission, a history of blood transfusion, ventricular tachycardia/ventricular fibrillation (VT/VF), and advanced Killip class.
The presence of the fQRS was associated with a remarkable increase in in‐hospital cardiovascular mortality (15.4% vs. 0.6%), one‐year cardiovascular mortality (24.2% vs. 2.2%), and one‐year all‐cause mortality (23.1% vs. 2.5%). And also these adverse cardiac events occur especially in the first month.
After an adjustment for potential confounders, it was found that the presence of the fQRS on the ECG was one of the independent predictors of one‐year all‐cause mortality (OR: 5.24; 95% CI: 1.43–19.2).
A 12‐lead ECG, which is easily available (and the cheapest modality), still remains the first option in the immediate triage, diagnosis, and recognition of high‐risk patients with acute coronary syndrome (ACS).17 A current electrocardiographic diagnostic criterion for MIs requires the development of pathologic Q waves or marked repolarization changes. The Q‐wave, which is the only depolarization abnormality and established sign of acute MI, is less common in NSTEMI and usually appears late. On the other hand, repolarization abnormalities frequently appear in the early stages of ACS.18 However, with the new treatment options of acute MI, the incidence of Q‐wave MIs have been associated with a significant decline, on the other hand, the NSTEMI was increased.19 Therefore, the predictive value of these electrocardiographic findings is questionable in patients with acute MI. Because of the difference in cardiac sarcolemmal ATP‐sensitive K channels and the new treatment methods (early PCI or thrombolytic), some ECG findings of acute MI (Q wave, ST elevation) may not be seen on the ECG.19, 20 In these patients, the fQRS may be often the only sign of electrocardiographic change for a myocardial ischemia or scar. On the other hand, Das et al.6 showed that fQRS has a higher sensitivity, but lower specificity, than the Q wave in demonstrating myocardial damage. In our study, we showed that fQRS has a sensitivity of 74.2% and specificity of 82.2%, and this result was correlated with others previous studies. Korhonen et al.21 reported that the increased fQRS in post‐MI patients predicts cardiac deaths and heart failure progression and also they founded that the fQRS is a stronger predictor than QRS duration.
The QRS complex occurs as a result of ventricular depolarization. Because of myocardial ischemia or scarring, heterogen‐echo ventricular activation manifests itself as a fQRS on the ECG.22, 23, 24 Depolarization (Q wave, duration of QRS) and repolarization (ST, T wave) changes are monitored on ECGs in patients with acute MI. Increased QRS duration with a new R1 wave or a QRS vector shift occurs because of the myocardial ischemia or scar.25 These changes are observed in different derivations of the ECG due to the localization of the acute MI.26 fQRS morphologies (notching on the upslope or downslope of the R and S waves) may also change because of the localization of ischemia or scar in the ventricles.
Many studies have demonstrated that the rates of the fQRS widely range between percentages (28%–54%).6, 10, 27 This wide range can be explained by the differences in the patients’ groups (such as STEMI, non‐STEMI, or USAP), different treatment methods, fQRS evaluation time interval, and variability in the ranges of filters adopted in the ECG imaging of these studies. In this present study, the frequency of fQRS was 22% in patients with acute STEMI undergoing primary PCI.
Many studies showed that, the presence of myocardial ischemia or the associated scar is related to adverse cardiac outcomes.6, 9, 10, 11, 28 These results could explain the reasons for the higher occurrence of adverse cardiac events in the group of patients with presence of fQRS on ECG. Depolarization (Q waves, new bundle branch blocks) and repolarization (ST‐T, associated changes) can be seen on ECG, which may be a transient marker, or may persist for a long time in patients with acute MI. Therefore, fQRS evaluation may not give precise results in patients with a previous MI. For this reason, in our study, we excluded patients who had a prior history of MI, to increase reliability, and to reduce the speculation of this prognostic marker of the Acute STEMI of the ECG.
Some recent studies have demonstrated a significant correlation between the presence of fQRS on ECGs and the presence of a scar on the MPS.6, 29, 30 In addition, a wide band recording of the electrocardiogram in patients with CAD and myocardial necrosis documented an increased number of notches in the R wave, and a slur in the S wave.31
Myocardial necrosis, or ischemia, is related with a poor prognosis due to the risk of fatal arrhythmias and advanced heart failure.6, 21, 29, 30 A fQRS signifies heterogeneous activation of the ventricles because of the myocardial scarring and/or ischemia in CAD. Endocardial and epicardial mapping in patients with CAD or those with dilated cardiomyopathy (with ventricular arrhythmias) was monitored with the fractionated QRS on an ECG, over a broad region surrounding the myocardial scar.20, 32 The fQRS is related to a higher adverse cardiac event and decreased life span in patients with known atherosclerotic heart disease.10 In our study, we demonstrated that the presence of the fQRS was significantly associated in high risk patients with acute STEMI undergoing primary PCI and who have a poor prognosis. On the other hand, we found that fQRS was not related with the location of the MI, value of the peak CK‐MB, acute thrombosis, in‐hospital reinfarction, post‐TIMI III flow, stent usage, and tirofiban usage. From these results, we assume that the presence of the fQRS on the ECG was a reliable and easily applicable prognostic indicator for the follow‐up of patients after acute MI.
fQRS is also a diagnostic marker of arrhythmogenic right ventricular dysplasia, which is associated with ventricular scarring and higher mortality because of ventricular arrhythmia and heart failure.33 Similarly, the incidence of fQRS is significantly higher in patients with Brugada syndrome, which is associated with a higher rate of ventricular fibrillation (85%). We also found that the presence of the fQRS was related with a higher rate of VT/VF in acute MI patients after primary PCI. For this reason, we think that fQRS represents myocardial scars, which may lay the groundwork for reentry and fatal ventricular arrhythmias. New studies need this utility in risk stratification of sudden death.
Study Limitations
This study was a single‐center study. It was nonrandomized, and thus, subject to selection bias. However, we were careful to include consecutive patients. A fQRS was not defined in the presence of complete or incomplete bundle branch blocks or paced rhythms, and therefore in this present study these patients were excluded from the analyses. We also did not look to other specific cardiomyopathies in the emergency department and catheter laboratory. And also despite adjusting for multiple risk factors, it is possible that residual confounding conditions and medications may have been present. Also, we did not use other quantitative modalities (myocardial perfusion scanning, echocardiography, or magnetic resonance imaging) to show the myocardial ischemia or scarring. Essentially, in this study, we demonstrated the efficiency and usefulness of the fQRS on ECG, which is the indirect method for measuring myocardial necrosis or scarring.
CONCLUSION
Our study showed that patients with a history of fQRS (on ECG) had poorer clinical outcomes and higher mortality than patients with an absence of fQRS on ECG. However, they were both studied while in the hospital, and during the subsequent one‐year follow‐up period. In summary, the presence of fQRS revealed by ECG is a valuable prognostic factor in patients undergoing primary PCI for STEMI. In light of the present study, we suggest that the fQRS on ECG is a simple and easily measurable method that can be used in risk stratification in patients with STEMI, and to determine in‐hospital adverse outcomes and long‐term prognosis. Since the presence of fQRS on the ECG is related to myocardial scarring or necrosis, and the size of the myocardial infarct, patients with STEMI, and the presence of fQRS on an ECG should be monitored closely.
REFERENCES
- 1. Fox KA, Cokkinos DV, Deckers J, et al. The ENACT study: A pan‐European survey of acute coronary syndromes. Eur Heart J 2000;21:1440–1449. [DOI] [PubMed] [Google Scholar]
- 2. Fox KA, Goodman SG, Anderson FA Jr, et al. From guidelines to clinical practice: The impact of hospital and geographical characteristics on temporal trends in the management of acute coronary syndromes. The Global Registry of Acute Coronary Events (GRACE). Eur Heart J 2003;24:1414–1424. [DOI] [PubMed] [Google Scholar]
- 3. Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. Am J Manag Care 2009;15: 36–41. [PubMed] [Google Scholar]
- 4. Nakamura N, Gohda M, Satani O, et al. Myocardial salvage for ST‐elevation myocardial infarction with terminal QRS distortion and restoration of brisk epicardial coronary flow. Heart Vessels 2009;24:96–102. [DOI] [PubMed] [Google Scholar]
- 5. Michael MA, El Masry H, Khan BR, et al. Electrocardiographic signs of remote myocardial infarction. Prog Cardiovasc Dis 2008; 50:198–208. [DOI] [PubMed] [Google Scholar]
- 6. Das MK, Khan B, Jacob S, et al. Significance of a fragmented QRS complex versus a Q wave in patients with coronary artery disease. Circulation 2006;113:2495–2501. [DOI] [PubMed] [Google Scholar]
- 7. Castle CH, Keane WM. Electrocardiographic “peri‐infarction block.” A clinical and pathologic correlation. Circulation 1965;31:403–408. [DOI] [PubMed] [Google Scholar]
- 8. Shadaksharappa KS, Kalbfleisch JM, Conrad LL, et al. Recognition and significance of intraventricular block due to myocardial infarction (peri‐infarction block). Circulation 1968;37:20–26. [DOI] [PubMed] [Google Scholar]
- 9. Pietrasik G, Goldenberg I, Zdzienicka J, et al. Prognostic significance of fragmented QRS complex for predicting the risk of recurrent cardiac events in patients with Q‐wave myocardial infarction. Am J Cardiol 2007;100:583–586. [DOI] [PubMed] [Google Scholar]
- 10. Das MK, Saha C, El Masry H, et al. Fragmented QRS on a 12‐lead ECG: A predictor of mortality and cardiac events in patients with coronary artery disease. Heart Rhythm 2007;4:1385–1392. [DOI] [PubMed] [Google Scholar]
- 11. Chatterjee S, Changawala N. Fraqmented QRS complex: A novel marker of cardiovascular disease. Clin Cardiol 2010;33:68–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two‐ Dimensional Echocardiograms. J Am Soc Echocardiogr 1989;2:358–367. [DOI] [PubMed] [Google Scholar]
- 13. Stevens LA, Coresh J, Greene T, et al. Assessing kidney function measured and estimated glomerular filtration rate. N Engl J Med 2006;354:2473–2483. [DOI] [PubMed] [Google Scholar]
- 14. Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: A comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation 1987;76:142–154. [DOI] [PubMed] [Google Scholar]
- 15. Killip T, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol 1967;20:457–464. [DOI] [PubMed] [Google Scholar]
- 16. Kristian T, Alpert JS, Jaffe AS, et al. The writing Group on behalf of the Joint ESC/ACCF/AHA/WHF. Task Force for the Universal Definition of Myocardial Infarction. Eur Heart J 2012;33:2551–2567. [DOI] [PubMed] [Google Scholar]
- 17. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non‐ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 2000;284:835–842. [DOI] [PubMed] [Google Scholar]
- 18. Boden WE, Gibson RS, Schechtman KB, et al. ST segment shifts are poor predictors of subsequent Q wave evolution in acute myocardial infarction. A natural history study of early non‐Q wave infarction. Circulation 1989;79:537–548. [DOI] [PubMed] [Google Scholar]
- 19. Furman MI, Dauerman HL, Goldberg RJ, et al. Twenty‐two year (1975 to 1997) trends in the incidence, in‐hospital and long‐term case fatality rates from initial Q‐wave and non‐Q‐wave myocardial infarction: A multi‐hospital, community‐wide perspective. J Am Coll Cardiol 2001;37:1571–1580. [DOI] [PubMed] [Google Scholar]
- 20. de Winter RJ, Verouden NJW, Wellens HJJ, et al. A new ECG sign of proximal LAD occlusion. N Engl J Med 2008;359:2071–2073. [DOI] [PubMed] [Google Scholar]
- 21. Korhonen P, Husa T, Konttila T, et al. Fragmented QRS in prediction of cardiac deaths and heart failure hospitalizations after myocardial infarction. Ann Noninvasive Electrocardiol 2010;15(2):130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Flowers NC, Horan LG, Thomas JR, et al. The anatomic basis for high‐frequency components in the electrocardiogram. Circulation 1969;39:531–539. [DOI] [PubMed] [Google Scholar]
- 23. Lesh MD, Spear JF, Simson MB. A computer model of the electrogram: What causes fractionation? J Electrocardiol 1988;21:S69–S73. [DOI] [PubMed] [Google Scholar]
- 24. Gardner PI, Ursell PC, Fenoglio JJ Jr, et al. Electrophysiologic and anatomic basis for fractionated electrograms recorded from healed myocardial infarcts. Circulation 1985;72:596–611. [DOI] [PubMed] [Google Scholar]
- 25. Friedman BM, Dunn MI. Postinfarction ventricular aneurysms. Clin Cardiol 1995;18:505–511. [DOI] [PubMed] [Google Scholar]
- 26. Wiener I, Mindich B, Pitchon R. Fragmented endocardial electrical activity in patients with ventricular tachycardia: A new guide to surgical therapy. Am Heart J 1984;107:86–90. [DOI] [PubMed] [Google Scholar]
- 27. Das MK, El Masry H. Fragmented QRS and other depolarization abnormalities as a predictor of mortality and sudden cardiac death. Curr Opin Cardiol 2010;25:59–64. [DOI] [PubMed] [Google Scholar]
- 28. Michael MA, Das MK. Fragmented QRS on 12‐lead EKG is a sign of acute or recent myocardial infarction. Circulation 2006;114:512–519. [Google Scholar]
- 29. Mahenthiran J, Khan BR, Sawada SG, et al. Fragmented QRS complexes not typical of a bundle branch block: A marker of greater myocardial perfusion tomography abnormalities in coronary artery disease. J Nucl Cardiol 2007;14:347–353. [DOI] [PubMed] [Google Scholar]
- 30. Varriale P, Chryssos BE. The RSR' complex not related to right bundle branch block: Diagnostic value as a sign of myocardial infarction scar. Am Heart J 1992;123:369–376. [DOI] [PubMed] [Google Scholar]
- 31. Langner PH Jr, Geselowitz DB, Briller SA. Wide band recording of the electrocardiogram and coronary heart disease. Am Heart J 1973;86:308–317. [DOI] [PubMed] [Google Scholar]
- 32. Stevenson WG, Soejima K. Catheter ablation for ventricular tachycardia. Circulation 2007;115:2750–2760. [DOI] [PubMed] [Google Scholar]
- 33. Peters S, Trummel M, Koehler B. QRS fragmentation in standard ECG as a diagnostic marker of arrhythmogenic right ventricular dysplasiacardiomyopathy. Heart Rhythm 2008;5:1417–1421. [DOI] [PubMed] [Google Scholar]


