Takotsubo syndrome (TTS) is a primary acquired cardiomyopathy,1, 2 mostly affecting postmenopausal women after a physical or psychological stressor often mimicking an acute coronary syndrome.3, 4 Its typical form is characterized by transient left ventricular dysfunction due to apical dyskinesia and hyperkinesia of basal segments, without significant epicardial coronary lesions (Figs. 1, 2, 3). The electrocardiogram (ECG) findings can often resemble those found during an anterior ST‐segment elevation myocardial infarction (STEMI). Elevation of biomarkers of myocardial injury is moderate and not proportional to the severity of left ventricular dysfunction. Despite the wide spectrum of clinical severity, in most cases the natural history of TTS is often benign with spontaneous and complete resolution of wall motion abnormalities in a few weeks. The pathophysiological mechanisms involved in TTS are not completely known. It has been associated with coronary spasm,5 perfusion defects secondary to impaired microcirculation,6, 7, 8, 9 or as currently most accepted, with the effects of catecholamines at toxic levels on myocardial β‐2 receptors.10, 11, 12, 13
Figure 1.
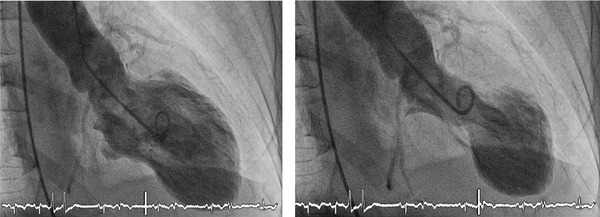
Example of Takotsubo syndrome ventriculography. Left picture shows left ventricle in diastole. Right picture shows the left ventricle in systole, with the typical shape due to apical dyskinesia and hypercontractility of the basal segments. See electrocardiogram monitoring.
Figure 2.
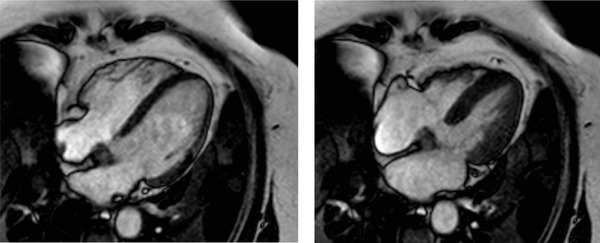
Images of cardiac magnetic resonance obtained 3 months after admission in a patient with the diagnostic of Takotsubo syndrome. Left picture shows a four‐chamber view in diastole. Right picture shows the same four‐chamber view in systole, demonstrating the complete recovery of the systolic function.
Figure 3.
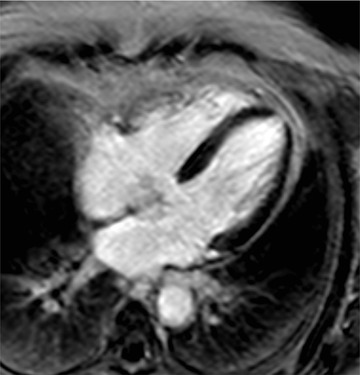
Images obtained by cardiac magnetic resonance at 3 months after admission in a patient with the diagnostic of Takotsubo syndrome, demonstrating the absence of late gadolinium enhancement in the left ventricle.
Of note, up to 1–2% of cases initially diagnosed as STEMI, and referred for primary percutaneous coronary intervention, are finally reclassified as TTS.14 The differential ECG diagnosis between these two entities can be challenging since no specific electrocardiographic criteria are available.
In this review we provide a systematic review of the ECG changes observed in patients with TTS.
ADMISSION ECG CHARACTERISTICS
The most common ECG abnormalities observed on admission are: ST‐segment elevation (49–90%), T‐wave inversion (44–83%), and Q waves (27–32%).4, 14, 15
ST‐segment elevation and negative T waves, were the two ECG findings proposed in the diagnostic criteria of the Mayo Clinic in 2004, later modified in 2008.16 It is also well known that these repolarization abnormalities follow a distinctive time sequence.17, 18
Time Course of the ECG Changes
Several authors have described a specific time course evolution of these ECG abnormalities. Mitsuma et al. followed a large series of TTS patients and analyzed serial ECGs obtained every 24 hours during hospital admission and subsequently every month up to ECG normalization.18 These authors described four phases in ECG evolution: (1) immediate ST‐segment elevation; (2) appearance of first peak of negative T waves from day 1 to 3; (3) subsequent transient reversion of negative T waves from day 2 to 6; (4) development of giant inverted T waves with prolongation of the QT interval, persisting up to 2 months until recovery (phase 4). See Table 1 and Figure 4.
Table 1.
Phases of the Time Course of ECG Changes
| Phase | Timing | ECG Changes |
|---|---|---|
| 1 | Immediate after | ST‐segment |
| onset of symptoms | elevation | |
| 2 | Days 1–3 | Negative T waves |
| 3 | Days 2–6 | Reversion of negative T waves |
| 4 | Up to 60 days | Giant negative T waves |
Figure 4.

Twelve‐lead ECG example of the time course ECG changes in a patient with Takotsubo syndrome. Day 0: day of admission.
ST‐Segment Changes
ST‐segment elevation is more frequently identified when ECG is performed in the very early phase of the syndrome, typically within a few hours from the onset of symptoms. The prevalence of this sign decreases when the ECG is obtained at a later stage. Accordingly Tsuchihashi et al. reported a prevalence of ST elevation of 90%, with ECGs obtained at 6 ± 9 hours from the onset of symptoms.15 In another study by Guerra et al. the median time for the admission ECG was 14 hours (interquartile range 4–27 hours) resulting in a much lower prevalence of ST‐segment elevation (31%).19 Also in a large series by Sharkey et al., the mean time from symptom onset to initial ECG was 8.4 ± 17 hours for patients with ST‐segment elevation, compared with 13.0 ± 18 hours for those without, although this difference was not statistically significant.5
ST‐segment elevation is usually more apparent in precordial leads V3–V6.20 The magnitude of ST‐segment elevation and the number of leads showing this pattern is usually lower in patients with TTS than in cases of STEMI.19, 21
Abnormal Q‐waves are also present in up to 42% of patients with TTS, more commonly in leads V3 and V4.15 The disappearance of Q‐waves with the reappearance of R‐waves, has been described in up to 75% of patients, most likely reflecting the electrophysiologic manifestation of an underlying stunned myocardium and/or edema as evaluated with cardiac magnetic resonance imaging (CMR).22
T‐Wave Inversion and QT‐Interval Prolongation
T‐wave inversion usually occurs within the first 24–72 hours from the onset of symptoms and is present in a large number of leads18, 19 mostly affecting V2–V6 but also I, II, aVL, and negative aVR (−aVR). The magnitude of the negative T waves and the number of leads affected is usually higher in TTS than in STEMI.5, 17, 18
QT‐interval prolongation is associated with the onset of negative T waves. Prolongation of the QT‐interval tends to be more pronounced in TTS than in STEMI and maintained throughout time. Moreover, the number of leads with T‐wave inversion is initially higher in TTS patients than in STEMI, but this difference is no longer significant beyond the third day.17, 19 There are some case reports of polymorphic ventricular tachycardia (VT) related to long QT‐interval.23, 24 The incidence of sustained VT is reported around 1.2% in a literature review.25
Kurisu et al. reported complete normalization of ECG in all patients at 6 months follow‐up.17
Interestingly, these ECG changes persist well beyond alterations in myocardial dysfunction.17 Mitsuma et al. observed that left ventricular wall motion abnormalities, evaluated by echocardiography, started to improve after phase 3 in all patients, coinciding with the appearance of giant inverted T waves.18 CMR imaging studies have shown that these ECG changes coincided and correlated with the apicobasal gradient of myocardial edema.26, 27
Other ECG Changes
QRS‐complex voltage attenuation has recently been reported and is probably related to myocardial edema, due to the lower resistance offered to the passage of electricity than normal tissue.28 In this line of research, Madias reviewed the 368 ECGs from 614 TTS articles published in the international literature from 2000 to 2013.29 Low voltage on admission ECG or voltage attenuation during in‐hospital stay were observed in 91% and 93% of patients, respectively.
J wave (Osborn) has also been described—it may represent the earliest ECG phase in TTS.30
Differential Diagnosis of TTS and Anterior Wall STEMI
Several studies have compared TTS and anterior STEMI ECG findings mainly focusing on ST‐segment elevation.
Ogura et al. compared the admission ECG in STEMI and TTS patients. ST‐segment elevation was more frequently seen in leads V4–V6 in TTS and in leads V1–V3 in STEMI. The magnitude of ST‐elevation in leads V1–V3 was higher in STEMI than TTS, resulting in a higher V4–V6/V1–V3 voltage ratio in TTS.20 This criterion yielded the greater specificity (100%) and overall accuracy (91%) in this study.
It has also been suggested that reciprocal changes may also help to differentiate between these two entities. Bybee et al. observed a higher prevalence of reciprocal ST‐segment changes in the inferior wall in STEMI when compared to TTS.21 Inoue et al. suggested that reciprocal changes in inferior leads may help differentiate TSS from STEMI due to proximal lesions in left descending coronary artery, but not those with distal lesions. Reciprocal ST‐segment depression in the inferior leads was observed less frequently in patients with TTS than in anterior STEMI due to occlusion of the proximal left anterior descending artery. On the other hand ST‐segment elevation in the inferior leads was observed more frequently in TTS. ECG findings did not differ between TTS and STEMI patients with distal culprit lesions.31 ST‐segment elevation of ≥1.0 mm in lead II was found to be the most sensitive (62.5%) and specific (92.6%) criterion for TTS.32
Finally, Kosuge et al. concluded that ST‐segment shift in leads aVR and V1 may help differentiating TTS from anterior STEMI in patients who are admitted within 6 hours of symptom onset. The combination of ST‐segment depression in lead aVR and the absence of ST‐segment elevation in lead V1 identified TTS with 91% sensitivity, 96% specificity, and 95% predictive accuracy, which was superior to any other electrocardiographic findings.33 Other authors have not been able to reproduce these findings.34 Carrillo et al. noted that the location of culprit lesions in left anterior descending artery had not been taken into account and furthermore, did not reach such diagnostic accuracy in their series.35
Several studies have attempted to establish the best ECG criteria capable of distinguishing between TTS and STEMI (see Table 1). Johnson et al. analyzed the performance of six different ECG criteria in a cohort of TTS and STEMI patients demonstrating in all cases a limited diagnostic accuracy and concluded that ECG should not be used in clinical practice as the only diagnostic criterion.36 See Table 2.
Table 2.
Accuracy of the ECG Findings for the Diagnosis of Takotsubo Syndrome
| ECG Sign | n | Sens | Spe | Accuracy | Ref |
|---|---|---|---|---|---|
| Absence of reciprocal changes | 13 TTS | 100% | 69% | 84% | 23 |
| Absence of Q waves | 13 a. AMI | 83% | 69% | 76% | |
| ΣSTeV4–V6 volt/ΣSTeV1–V3 volt ≥ 1 | 80% | 77% | 76% | ||
| 36% | 80% | 75% | 36 | ||
| STe II > 1 mm | 8 TTS | 62% | 93% | 86% | |
| Ste < 1 mm in ≥ 2 inferior leads | 27 a. AMI | 50% | 93% | 83% | |
| STe V2 volt < 1.75 mV and STe V3 volt < 2.5 mV | 18 TTS | 67% | 94% | – | 24 |
| (3xSTe V2 volt + STe V3 volt + 2xSTe V5 volt) < 11.5 mm | 36 a. AMI | 94% | 72% | – | |
| STe ‐aVR volt ≥ 0.5 mm | 33 TTS | 91% | 96% | – | 37 |
| and STeV1 volt ≤ 1 mm | 342 a. AMI | ||||
| 51 TTS | 6% | 99% | 74% | 38 | |
| 135 a.AMI | |||||
| nTw in ‐aVR | 100% | 87% | 89% | ||
| Absence of nTw in V1 | 34 TTS | 94% | 68% | 72% | 40 |
| nTw in ‐aVR and absence of nTw in V1 | 237 a. AMI | 94% | 95% | 94% |
n = number of patients; Sens = sensitivity; Spe = specificity; STe = ST‐segment elevation; volt = voltage; nTw = negative T wave; TTS = Takotsubo; a. AMI = anterior acute myocardial infarction; Ref = reference number.
CONCLUSIONS
Repolarization abnormalities in TTS go well beyond the classic ST‐segment changes and may aid in the differential diagnosis with STEMI. Unfortunately in the acute clinical setting all electrocardiographic criteria have limited diagnostic accuracy in differentiating between TTS and STEMI. Patients presenting with ST‐segment elevation should undergo emergent coronary angiography in order to rule out STEMI even at the cost of false positive, alas inevitable, activation of STEMI networks.
REFERENCES
- 1. Maron BJ, Towbin JA, Thiene G, et al. Contemporary definitions and classifications of the cardiomyopathies: An American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 2006;113:1807–1816. [DOI] [PubMed] [Google Scholar]
- 2. Sato H, Tateishi H, Uchida T, et al. Takotsubo‐like left ventricular dysfunction due to multivessel coronary spasm. Kagakuhyouronsha 1990;56–64. [Google Scholar]
- 3. Akashi YJ, Goldstein DS, Barbaro G, et al. Takotsubo cardiomyopathy: A new form of acute, reversible heart failure. Circulation 2008;1182754–1182762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (tako‐tsubo) cardiomyopathy. J Am Coll Cardiol 2010;55:333–341. [DOI] [PubMed] [Google Scholar]
- 5. Kurisu S, Sato H, Kawagoe T, et al. Tako‐tsubo‐like left ventricular dysfunction with ST‐segment elevation: A novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J 2002;143:448–455. [DOI] [PubMed] [Google Scholar]
- 6. Kume T, Akasaka T, Kawamoto T, et al. Assessment of coronary microcirculation in patients with takotsubo‐like left ventricular dysfunction. Circ J 2005;69934–69939. [DOI] [PubMed] [Google Scholar]
- 7. Elesber A, Lerman A, Bybee KA, et al. Myocardial perfusion in apical ballooning syndrome correlate of myocardial injury. Am Heart J 2006;152:469;e9–13. [DOI] [PubMed] [Google Scholar]
- 8. Yoshida T, Hibino T, Kako N, et al. A pathophysiologic study of tako‐tsubo cardiomyopathy with F‐18 fluorodeoxyglucose positron emission tomography. Eur Heart J 2007;28:2598–2604. [DOI] [PubMed] [Google Scholar]
- 9. Shah DP, Sugeng L, Goonewardena SN, et al. Images in cardiovascular medicine. Takotsubo cardiomyopathy. Circulation 2006;113:e762. [DOI] [PubMed] [Google Scholar]
- 10. Ueyama T, Kasamatsu K, Hano T, et al. Emotional stress induces transient left ventricular hypocontraction in the rat via activation of cardiac adrenoceptors: A possible animal model of ‘tako‐tsubo’ cardiomyopathy. Circ J 2002;66:712–713. [DOI] [PubMed] [Google Scholar]
- 11. Wittstein IS, Thiemann DR, Lima JA, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352:539–548. [DOI] [PubMed] [Google Scholar]
- 12. Lyon AR, Rees PS, Prasad S, et al. Stress (Takotsubo) cardiomyopathy–A novel pathophysiological hypothesis to explain catecholamine‐induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med 2008;5:22–29. [DOI] [PubMed] [Google Scholar]
- 13. Paur H, Wright PT, Sikkel MB, et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2‐adrenergic receptor/Gi‐dependent manner: A new model of Takotsubo cardiomyopathy. Circulation 2012;126:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: A systematic review. Eur Heart J 2006;27(13):1523–1529. [DOI] [PubMed] [Google Scholar]
- 15. Tsuchihashi K, Ueshima K, Uchida T, et al. Transient left ventricular apical ballooning without coronary artery stenosis: A novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris‐Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 2001;38:11–18. [DOI] [PubMed] [Google Scholar]
- 16. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako‐Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am Heart J 2008;155:408–417. [DOI] [PubMed] [Google Scholar]
- 17. Kurisu S, Inoue I, Kawagoe T, et al. Time course of electrocardiographic changes in patients with Tako‐Tsubo syndrome: Comparison with acute myocardial infarction with minimal enzymatic release. Circ J 2004;68:77–81. [DOI] [PubMed] [Google Scholar]
- 18. Mitsuma W, Kodama M, Ito M. Serial electrocardiographic findings in women with Takotsubo cardiomyopathy. Am J Cardiol 2007;100:106–109. [DOI] [PubMed] [Google Scholar]
- 19. Guerra F, Rapaj E, Pongetti G, et al. Differences and similarities of repolarization patterns during hospitalization for Takotsubo cardiomyopathy and acute coronary syndrome. Am J Cardiol 2013;112:1720–1724. [DOI] [PubMed] [Google Scholar]
- 20. Ogura R, Hiasa Y, Takahashi T, et al. Specific findings of the standard 12‐lead ECG in patients with takotsubo cardiomyopathy: Comparison with thefindings of acute anterior myocardial infarction. Circ J 2003;67:687–690. [DOI] [PubMed] [Google Scholar]
- 21. Bybee KA, Motiei A, Syed IS, et al. Electrocardiography cannot reliably differentiate transient left ventricular apical ballooning syndrome from anterior ST‐segment elevation myocardial infarction. J Electrocardiol 2007;40:38.e1–e6. [DOI] [PubMed] [Google Scholar]
- 22. Sharkey SW. Electrocardiogram mimics of acute ST‐segment elevation myocardial infarction: Insights from cardiac magnetic resonance imaging in patients with takotsubo (stress) cardiomyopathy. J Electrocardiol 2008;41:621–625. [DOI] [PubMed] [Google Scholar]
- 23. Çakici M, Cetin M, Polat M, et al. Long QT‐induced ventricular tachycardia associated with Takotsubo cardiomyopathy. Turk Kardiyol Dern Ars 2014;42:71–75 [DOI] [PubMed] [Google Scholar]
- 24. Sasaki O, Nishioka T, Akima T, et al. Association of takotsubo cardiomyopathy and long QT syndrome. Circ J 2006;70:1220–1222. [DOI] [PubMed] [Google Scholar]
- 25. Syed FF, Asirvatham SJ, Francis J. Arrhythmia occurrence with takotsubo cardiomyopathy: A literature review. Europace 2011;13:780–788. [DOI] [PubMed] [Google Scholar]
- 26. Perazzolo‐Marra M, Zorzi A, Corbetti F, et al. Apicobasal gradient of left ventricular myocardial edema underlies transient T wave inversion and QT interval prolongation (Wellens’ ECG pattern) in Tako‐Tsubo cardiomyopathy. Heart rhythm 2013;10:70–77. [DOI] [PubMed] [Google Scholar]
- 27. Migliore F, Zorzi A, Marra MP, et al. Myocardial edema underlies dynamic T‐wave inversion (Wellens’ ECG pattern) in patients with reversible left ventricular dysfunction. Heart Rhythm 2011;8:1629–1634. [DOI] [PubMed] [Google Scholar]
- 28. Madias JE, Bazaz R, Agarwal H, et al. Anasarca‐mediated attenuation of the amplitude of electrocardiogram complexes: A description of a heretofore unrecognized phenomenon. J Am Coll Cardiol 2001;3:756–764. [DOI] [PubMed] [Google Scholar]
- 29. Madias JE. Transient attenuation of the amplitude of the QRS complexes in the diagnosis of Takotsubo syndrome. Eur Heart J Acute Cardiovasc Care 2014;3:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zorzi A, Migliore F, Perazzolo Marra M, et al. Electrocardiographic J waves as a hyperacute sign of Takotsubo syndrome. J Electrocardiol 2012;45:353–356. [DOI] [PubMed] [Google Scholar]
- 31. Inoue M, Shimizu M, Ino H, et al. Differentiation between patients with Takotsubo cardiomyopathy and those with anterior acute myocardial infarction. Circ J 2005;69:89–94. [DOI] [PubMed] [Google Scholar]
- 32. Jim MH, Chan AO, Tsui PT, et al. A new ECG criterion to identify takotsubo cardiomyopathy from anterior myocardial infarction: Role of inferior leads. Heart Vessels 2009;24:124–130. [DOI] [PubMed] [Google Scholar]
- 33. Kosuge M, Ebina T, Hibi K, et al. Simple and accurate electrocardiographic criteria to differentiate Takotsubo cardiomyopathy from anterior acute myocardial infarction. J Am Coll Cardiol 2010;55:2514–2516. [DOI] [PubMed] [Google Scholar]
- 34. Núñez‐Gil IJ, Luaces M, Garcia‐Rubira JC, et al. Electrocardiographic criteria in Takotsubo cardiomyopathy and race differences: Asians versus Caucasians. J Am Coll Cardiol 2010;56:1433–1434. [DOI] [PubMed] [Google Scholar]
- 35. Carrillo A, Fiol M, García‐Niebla J, et al. Electrocardiographic differential diagnosis between Takotsubo syndrome and distal occlusion of LAD is not easy. J Am Coll Cardiol 2010. Nov 2;56:1610–1611. [DOI] [PubMed] [Google Scholar]
- 36. Johnson NP, Chavez JF, Mosley WJ 2nd, et al. Performance of electrocardiographic criteria to differentiate Takotsubo cardiomyopathy from acute anterior ST elevation myocardial infarction. Int J Cardiol 2013;164:345–348. [DOI] [PubMed] [Google Scholar]


