Abstract
Transcatheter aortic valve implantation (TAVI) is indicated in severe symptomatic aortic stenosis, when there is intermediate‐high surgical risk, or a condition considered inoperable, as in the case of “porcelain aorta” that could turn clamping or cannulation of the ascending aorta hazardous in open‐heart surgery. Among the complications of this less invasive procedure, intraventricular conduction disorders subsequent to the procedure stand out. TAVI causes worsening of intraventricular dromotropic disorders in more than 75% of the cases, with the presence of preexisting right bundle branch block and first‐degree atrioventricular block, deep prosthesis implant, male gender, size of the aortic annulus smaller than the prosthesis, and porcelain aorta being predictive of requirement for permanent pacemaker implant.
Keywords: left anterior fascicular block, left bifascicular block, left septal fascicular block, percutaneous transcatheter aortic valve implantation
1. CASE REPORT
The patient is an 81‐year old man from Brazil, who complained of oppression in the chest, dizziness, and shortness of breath.
The precordial oppressive pain did not radiate, it improved with burping and had no precipitating factors. He was in good general physical state with normal heart rhythm, a heart rate of 60 bpm, split, normal rhythmic heart sounds, pulsus parvus et tardus, intense mesosystolic ejection murmur of late peak in the aortic area, of crescendo‐decrescendo type radiating to the carotid arteries. In addition, a diastolic decrescendo murmur was auscultated. Blood pressure 150/60 mmHg and pulmonary auscultation was normal.
At admission, an ECG was recorded (Figure 1). Cardiac catheterization confirmed severe aortic stenosis with coronary arteries free from atherosclerotic disease.
Figure 1.
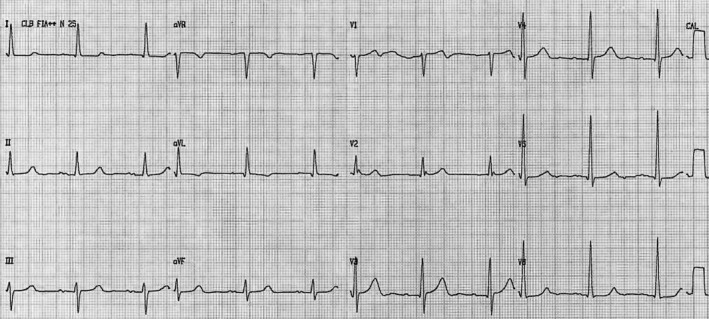
ECG before the procedure. P duration = 120 ms, bimodal aspect, PR interval = 220 ms, QRS axis +10°, QRS duration 110 ms, early transition in precordial leads (V1 or V2), embryonic initial q wave from V2 through V6. Conclusion: left atrial enlargement, doubtful first‐degree AV block (elderly), embryonic q wave from V2 through V6
Surgical risk was considered high (porcelain aorta), and transapical transcatheter aortic valve implantation (TAVI) was the procedure‐of‐choice (Figure 2). Another ECG was performed after procedure (Figure 3).
Figure 2.
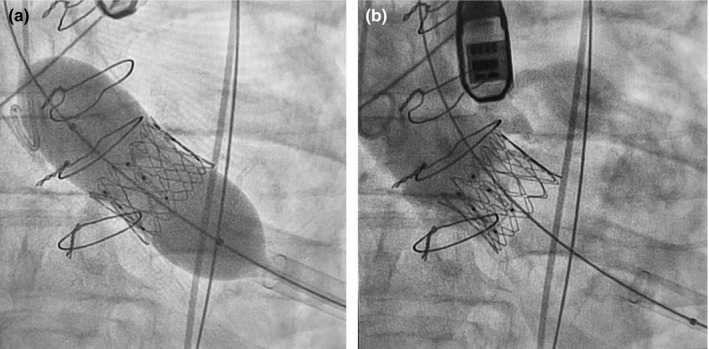
Transapical implant of aortic valve. (a) Catheter‐balloon inflation and prosthesis opening; (b) control aortography showing that the coronary ostia are intact, and absence of significant aortic insufficiency
Figure 3.
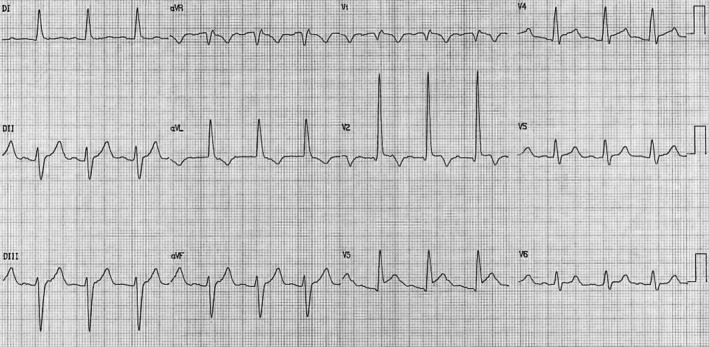
ECG performed immediately after the procedure. P duration = 120 ms, bimodal aspect, QRS axis −50°, QRS duration 130 ms, early transition in precordial leads, initial embryonic q wave from V2 to V6, R wave of large amplitude in V2: prominent anterior QRS forces (PAF), prolonged R‐wave peak time in V1–V2 (≥35 ms), R wave in crescendo from V1 to V2 and decreasing from V3 through V6, absence of initial q wave in the left leads (I, aVL, V5–V6) by absence of first septal vector of the middle third of the left septal surface. ST segment elevation followed by negative T wave in the right precordial leads Conclusion: left atrial enlargement + LAFB + LSFB + ischemic changes in anteroseptal wall
2. DISCUSSION
Intraventricular conduction disorders are frequent complications of TAVI. Moini et al. (2016) described the following intraventricular dromotropic disorders before and after the procedure: complete left bundle branch block (CLBBB), complete right bundle branch block (CRBBB), left anterior fascicular block (LAFB), and rarely left posterior fascicular block.
Ortak et al. presented experiences with the LOTUS prosthesis. They found new LBBB after TAVI in over 30% of the patients, both before and after the introduction of a specific clinical protocol to limit the postprocedural permanent pacemaker implantation rate. The rate of new complete atrioventricular block and CRBBB was lower (Ortak et al., 2018).
According to Kessler et al. patients with need for permanent pacemaker implantation compared with patients without need for implantation had more often preprocedural CRBBB (16.3% vs 0, p < .001), and this conduction disorder was an independent risk factors for need of permanent pacemaker by multiple regression analysis. On the other hand, CLBBB in the preprocedural ECG was seen in 7.5% of the patients, who needed a permanent pacemaker and in 10.7%, in those without need for pacemaker implantation (p = .49). The corresponding numbers for LAFB were 20% and 14.6% (p = .33). Left septal fascicular block (LSFB) has never been described in the setting of TAVI (Kessler, Gonska, Seeger, Rottbauer, & Wohrle, 2017).
The presence of LSFB has been described predominantly in scenarios of acute coronary syndrome by critical obstruction of the left anterior descending (LAD) coronary artery before its first septal perforating branch (Perez‐Riera, Nadeau‐Routhier, Barbosa‐Barros, & Baranchuk, 2016), in a transient fashion during stress test (Uchida, Moffa, Riera, & Ferreira, 2006), and in Wellens' syndrome (Riera et al., 2008). In all these cases, LSFB has been a response to severe proximal obstruction in the LAD. In Latin America, LSFB has been observed in Chagas disease (Moffa et al., 1982).
3. CONCLUSION
We present a case of transient LSFB associated with LAFB in the scenario of a TAVI procedure. The transitoriness of the dromotropic disorder reinforces the fact that the prominent anterior QRS forces (PAF) are not due to other causes that may cause PAF.
CONFLICTS OF INTEREST
None.
Pérez‐Riera AR, Barbosa‐Barros R, Cabral de Oliveira MF, Daminello‐Raimundo R, de Abreu LC, Nikus K. Transient left anterior and septal fascicular blocks after self‐expandable percutaneous transcatheter aortic valve implantation. Ann Noninvasive Electrocardiol. 2019;24:e12553 10.1111/anec.12553
REFERENCES
- Kessler, M. , Gonska, B. , Seeger, J. , Rottbauer, W. , & Wohrle, J. (2017). Predictors of permanent pacemaker implantation after transfemoral aortic valve implantation with the Lotus valve. American Heart Journal, 192, 57–63. 10.1016/j.ahj.2017.07.011 [DOI] [PubMed] [Google Scholar]
- Moffa, P. J. , Del Nero, E. , Tobias, N. M. , Serro Azul, L. G. , Pileggi, F. , & Decourt, L. V. (1982). The left anterior septal block in Chagas' disease. Japanese Heart Journal, 23, 163–165. [Google Scholar]
- Moini, C. , Sidia, B. , Poindron, D. , Fiorina, L. , Farge, A. , Amara, W. , & El Issa, M. (2016). Cardiac permanent pacemaker after transcatheter aortic valve implantation: A predictive and scientific review. Annales de cardiologie et d'angéiologie, 65(5), 346–351. [DOI] [PubMed] [Google Scholar]
- Ortak, J. , D'Ancona, G. , Ince, H. , Agma, H. U. , Safak, E. , Oner, A. , & Kische, S. (2018). Transcatheter aortic valve implantation with a mechanically expandable prosthesis: A learning experience for permanent pacemaker implantation rate reduction. European Journal of Medical Research, 23(1), 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Riera, A. R. , Nadeau‐Routhier, C. , Barbosa‐Barros, R. , & Baranchuk, A. (2016). Transient left septal fascicular block: An electrocardiographic expression of proximal obstruction of left anterior descending artery? Annals of Noninvasive Electrocardiology, 21(2), 206–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riera, A. R. , Ferreira, C. , Ferreira Filho, C. , Dubner, S. , Schapachnik, E. , Uchida, A. H. , … de Luna, A. B. (2008). Wellens syndrome associated with prominent anterior QRS forces: An expression of left septal fascicular block? Journal of Electrocardiology, 41(6), 671–674. [DOI] [PubMed] [Google Scholar]
- Uchida, A. H. , Moffa, P. J. , Riera, A. R. , & Ferreira, B. M. (2006). Exercise‐induced left septal fascicular block: An expression of severe myocardial ischemia. Indian Pacing and Electrophysiology Journal, 6(2), 135–138. [PMC free article] [PubMed] [Google Scholar]


