Abstract
Hypertrabeculation/noncompaction of the myocardium is a rare disorder that involves most commonly the left ventricle of the heart and it has been recognized as a distinct cardiomyopathy by the World Health Organization. However, it is extremely rare for this condition to involve exclusively the right ventricle. We report the cases of three patients who presented with ventricular tachyarrhythmia and sudden cardiac death. They were found to have isolated right ventricular hypertrabeculation/noncompaction on echocardiography. This supports the hypothesis that this condition is highly arrhythmogenic and is associated with high mortality similarly to the left ventricular hypertrabeculation/noncompaction cardiomyopathy.
Keywords: hypertrabecultion, implantable cardioverter defibrillator, noncompaction cardiomyopathy, sudden cardiac death, ventricular arrhythmia
1. INTRODUCTION
Hypertrabeculation/noncompaction (HT/NC) of the ventricular myocardium is a rare congenital disorder characterized by specific morphological abnormalities, which include ventricular wall thickening, deep trabecular meshwork and deep intertrabecular recesses in the ventricular wall (Jenni, Oechslin, Schneider, Jost, & Kaufmann, 2001). The most common site of involvement is the left ventricle (LV) alone or rarely combined with right ventricle (RV) in very few reported cases (Jenni et al., 2001; Said, Cooper, Quevedo, Rodriguez, & Hernandez, 2013; Sato et al., 2007). However, HT/NC involving the RV alone is extremely rare and has only been described as single case reports (Chiribiri et al., 2009; Song, 2011; Ying, Xu, Chen, Ma, & You, 2008). Myocardial HT/NC has a wide spectrum of presentation that can range from an asymptomatic state to a progressive deterioration of cardiac function, systemic thromboembolism, different types of dysrhythmias and even sudden cardiac death (SCD) (Ichida et al., 1999; Jenni, Oechslin, & van der Loo, 2007). In this report, we describe the cases of three adult patients with isolated RV HT/NC who presented with ventricular tachyarrhythmia and sudden cardiac death.
2. CASE PRESENTATION
2.1. Case 1
A 52‐year‐old female patient was brought to our hospital postcardiac arrest. The patient has a remote history of atrial and ventricular septum defect correction, pulmonic valve repair at age of five, followed by tricuspid valve annuloplasty, bi‐atrial maze procedure for atrial fibrillation and an implantation of a dual chamber pacemaker (EnRhythm; Medtronic) at the age of 45. Initially, cardiopulmonary resuscitation was started by her husband when he found her unresponsive and pulseless at home, then continued for another fifteen minutes by paramedics resulting in return of spontaneous circulation. Therapeutic hypothermia was performed at the hospital for 2 days after which she fully recovered. Interrogation of the pacemaker showed a single premature ventricular contraction followed by ventricular fibrillation (Figure 1a). Echocardiographic examination revealed hypertrabeculation and dilatation of the RV (Figure 1b). Consequently, her pacemaker was upgraded to an implantable cardioverter defibrillator (ICD).
Figure 1.
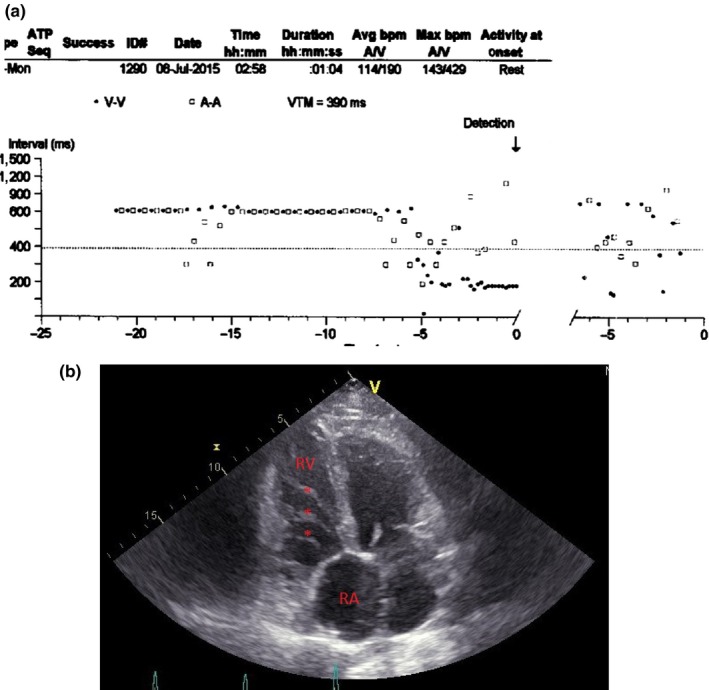
(a) Pacemaker interrogation revealing ventricular fibrillation. (b) Echocardiogram showing isolated hypertrabeculation of the right ventricle. RV, right ventricle; RA, right atrium; *Trabeculations
2.2. Case 2
A 55‐year‐old female patient presented to the emergency department because of weakness and palpitations. Patient has a history of tetralogy of Fallot that was corrected surgically at the age of 3 months. She is also known to have right bundle branch block and paroxysmal atrial fibrillation. Upon admission, electrocardiogram showed wide complex tachycardia at a rate of 193/min with left bundle branch block morphology (Figure 2a). All her laboratory tests were normal and cardiac ischemia was ruled out. Echocardiography showed normal LV, elevated systolic pulmonary artery pressure, dilatation and hypertrabeculation of the RV (Figure 2b). Subsequently, patient underwent an ICD implantation then discharged home. Interrogation of the device during a follow‐up visit 9 months later showed that the patient had one treated ventricular fibrillation, eleven episodes of nonsustained ventricular tachycardia, and several runs of paroxysmal atrial fibrillation.
Figure 2.
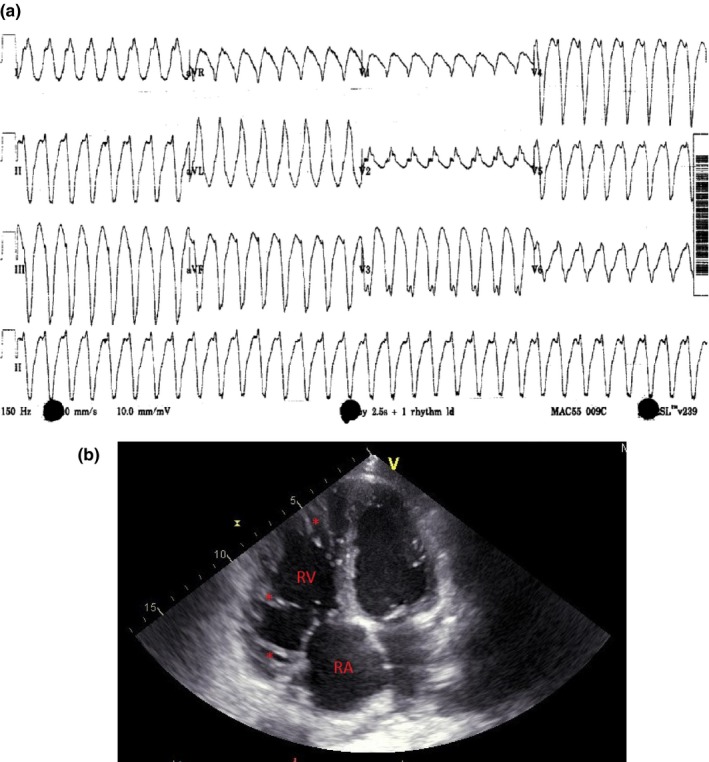
(a) Electrocardiogram upon presentation showing sustained ventricular tachycardia at a rate of 190 bpm. (b) Echocardiogram showing right ventricular hypertrabeculation and dilatation. RV, right ventricle; RA, right atrium; *Trabeculations
2.3. Case 3
A 39‐year‐old male patient with a medical history of ostium primum atrial septal defect surgically corrected at the age of three and heart failure with preserved ejection fraction, was admitted to our institution because of congestive heart failure decompensation and atrial flutter. Blood work results were unremarkable. Cardiac ischemia work‐up was negative. Patient was cardioverted after exclusion of intracardiac clots, treated for heart failure and was discharged home. One week after discharge, he was found dead, two hours after he went to bed. Review of his previous echocardiographic images showed hypertrabeculation and dilatation of the RV (Figure 3).
Figure 3.
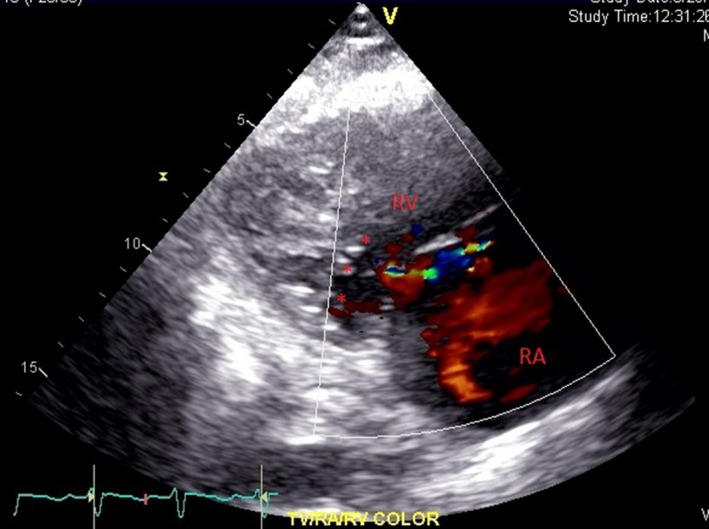
Echocardiogram showing hypertrophy of the right ventricle, with hypertrabeculation and perfused recesses. RV, right ventricle; RA, right atrium; *Trabeculations and recesses
2.4. Echocardiographic features
For these three cases, we applied the same diagnostic echocardiographic criteria of LV HT/NC to the RV (Ulusoy, Kucukarslan, Kirilmaz, & Demiralp, 2006): 2D‐echocardiography showed marked hypertrabeculation and hypertrophy of the RV, involving the apex, free lateral wall and the base at the level of tricuspid valve. All three patients showed hypokinetic noncompacted segments with a two‐layer structure and perfused recesses. To note that hypertrabeculation was mostly pronounced at the middle of the cavity and at the base of the RV adjacent to the tricuspid valve. All patients had normal LV wall thickness, dimensions and function. Echocardiographic findings are summarized in Table 1.
Table 1.
Echocardiographic findings and measures
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| RV TD | 5.66 cm | 5.16 cm | 4.47 cm |
| RV LD | 9.25 cm | 9.84 cm | 8.43 cm |
| No. NC segments | 7 | 6 | 5 |
| NC/C ratio | 3.65 | 5.23 | 5.43 |
| PA pressure | 57 mm Hg | 63 mm Hg | 90 mm Hg |
| RV volume overload | Present | Present | Present |
| LV ejection fraction | >55% | >55% | >55% |
PA, pulmonary artery; RV, right ventricle; LV, left ventricle; RV TD, right ventricle transverse diameter; RV LG, right ventricle longitudinal diameter; NC, noncompaction; NC/C, noncompaction/compaction.
3. DISCUSSION
Congenital noncompaction of the ventricular myocardium is a rare genetic disorder with a prevalence of 0.01% in adults and 0.14% in pediatric population and varies between 0.06% and 0.24% in the general population (Said et al., 2013). HT/NC has been attributed to postnatal persistence of the embryonic pattern of the myo‐architecture and arrest of compaction of the fetal loose meshwork (Ritter et al., 1997; Weiford, Subbarao, & Mulhern, 2004). Isolated LV HT/NC is now recognized as a distinct cardiomyopathy according to the WHO classification under the unclassified cardiomyopathies (Richardson et al., 1996), and its gene has been identified on the human chromosome 11p15 (Sasse‐Klaassen et al., 2004). Nowadays, myocardial HT/NC is more and more diagnosed because of the rising awareness of this entity and the frequent use of diagnostic modalities such as echocardiography and cardiac magnetic resonance imaging. Myocardial HT/NC has been described as an isolated congenital disorder or in association with other congenital diseases such as neuro‐muscular disorders, Barth syndrome, Ebstein anomaly, and tetralogy of Fallot (Stähli et al., 2013). On the other hand, some authors believe that it can be an acquired disease. For instance, in a retrospective review of HT/NC, the average detection time from a previously normal echocardiogram was 3.8 years (Finsterer, Stöllberger, & Schubert, 2008). The pathogenesis of acquired HT/NC remains uncertain but it has been suggested that hypertrabeculation is an adaptive and compensatory mechanism in attempt to enlarge the endocardial surface to increase stroke volume/cardiac output in chambers with reduced contractility or in chambers subjected to increased pressure/volume overload (Finsterer et al., 2008). Another proposed mechanism for hypertrabeculation is the transformation of the myocardium to a meshform of trabeculae caused by reduced adhesion of cardiac myocytes and malfunction of Gap junction (Song, 2011). These mechanisms are extrapolated from the spongy icefish heart which is characterized by myocardial pseudo‐hypertrophy and its ability to pump a larger stroke volume at a lower pressure (Agnisola & Tota, 1994). In this report, the patients had all the echocardiographic criteria for congenital HT/NC involving the RV as described by Frischknecht and his colleagues (Frischknecht et al., 2005). At the same time, they had significant pulmonary hypertension and pressure volume overload of the RV making an acquired HT/NC also probable. However, the presence of all four echocardiographic features for noncompaction as shown in previous validation study, together with involvement of the apex, the free lateral wall and the basal segment distinguish our patients as having congenital isolated RV HT/NC associated with congenital heart disease (Frischknecht et al., 2005). Besides, it is important to consider other differentials for RV cardiomyopathies such as RV dysplasia or dilated cardiomyopathy. However, none of the patients' echocardiographic features meet the revised Task Force Criteria for Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia (ARVC/D). There was no evidence of RV aneurysms or segments of reduced thickness, no Epsilon wave on electrocardiogram, and no familial history suggestive of this condition. Only one major criterion was present and consisted of a sustained ventricular tachycardia of left bundle‐branch morphology with superior axis in one patient, insufficient to consider the diagnosis (Marcus et al., 2010). Then again, all of the three patients showed highly specific echocardiographic criteria for myocardial HT/NC namely the presence of noncompacted segments with a two‐layered structure, perfused recesses, wall thickening, along with a noncompaction/compaction ratio of more than 3.0. These findings are considerably less obvious in other causes of dilated cardiomyopathy such as ARVC/D, and if present, the ratio of NC/C would be less than 2.0 (Frischknecht et al., 2005).
Various types of arrhythmias are associated with LV HT/NC, with the most frequent being sustained or nonsustained ventricular tachycardia (Stollberger & Finsterer, 2010). Several mechanisms for genesis of ventricular arrhythmia have been implicated in patients with LV HT/NC (Oechslin, Jost, Rojas, Kaufmann, & Jenni, 2000). Re‐entry either of the macro or micro type is the main proposed mechanism with its substrate being a localized necrosis and fibrosis caused by subendocardial ischemia and/or coronary microcirculatory dysfunction (Oechslin et al., 2000). Other suggested mechanism is the presence of a conduction abnormality at the level of the Purkinje fibers, components of the false tendon that is frequently seen in HT/NC (Lotkowski, Grzybiak, Kozłowski, Budzyn, & Kuta, 1996). Back to our patients, ventricular fibrillation was documented in one of them by his permanent pacemaker, and rapid sustained monomorphic right ventricular tachycardia at a rate of 193/min was seen on presentation of the second one. To note that all of our patients had normal LV function and dimensions. These facts show that isolated myocardial HT/NC of the RV is highly arrhythmogenic and necessitates prompt intervention such as the implantation of an ICD to prevent future arrhythmias and SCD.
4. CONCLUSION
The prevalence of isolated RV HT/NC remains underestimated and although echocardiography can help identifying specific characteristics of HT/NC, the morphological assessment of RV continues to be difficult and challenging. The swift recognition of RV HT/NC is extremely important because of its association with high mortality and morbidity, and ICD implantation is highly indicated to prevent catastrophic outcomes in this population.
CONFLICTS OF INTEREST
None of the authors has any conflict of interest to disclose.
Bekheit S, Karam B, Daneshvar F, et al. Sudden cardiac death in isolated right ventricular hypertrabeculation/noncompaction cardiomyopathy. Ann Noninvasive Electrocardiol. 2018;23:e12487 10.1111/anec.12487
REFERENCES
- Agnisola, C. , & Tota, B. (1994). Structure and function of the fish cardiac ventricle: Flexibility and limitations. Cardioscience, 5(3), 145–153. [PubMed] [Google Scholar]
- Chiribiri, A. , Leuzzi, S. , Salvetti, I. , Patané, S. , Bonamini, R. , Trevi, G. P. , … Cesarani, F. (2009). Isolated noncompaction of the right ventricular myocardium in the adulthood? International Journal of Cardiology, 134(1), e17–e19. [DOI] [PubMed] [Google Scholar]
- Finsterer, J. , Stöllberger, C. , & Schubert, B. (2008). Acquired left ventricular noncompaction as a cardiac manifestation of neuromuscular disorders. Scandinavian Cardiovascular Journal, 42(1), 25–30. [DOI] [PubMed] [Google Scholar]
- Frischknecht, B. S. , Jost, C. H. A. , Oechslin, E. N. , Seifert, B. , Hoigné, P. , Roos, M. , & Jenni, R. (2005). Validation of noncompaction criteria in dilated cardiomyopathy, and valvular and hypertensive heart disease. Journal of the American Society of Echocardiography, 18(8), 865–872. [DOI] [PubMed] [Google Scholar]
- Ichida, F. , Hamamichi, Y. , Miyawaki, T. , Ono, Y. , Kamiya, T. , Akagi, T. , … Tomimatsu, H. (1999). Clinical features of isolated noncompaction of the ventricular myocardium: Long‐term clinical course, hemodynamic properties, and genetic background. Journal of the American College of Cardiology, 34(1), 233–240. [DOI] [PubMed] [Google Scholar]
- Jenni, R. , Oechslin, E. N. , Schneider, J. , Jost, C. A. , & Kaufmann, P. (2001). Echocardiographic and pathoanatomical characteristics of isolated left ventricular non‐compaction: A step towards classification as a distinct cardiomyopathy. Heart, 86(6), 666–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenni, R. , Oechslin, E. N. , & van der Loo, B. (2007). Isolated ventricular non‐compaction of the myocardium in adults. Heart, 93(1), 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotkowski, D. , Grzybiak, M. , Kozłowski, D. , Budzyn, K. , & Kuta, W. (1996). A microscopic view of false tendons in the left ventricle of the human heart. Folia morphologica, 56(1), 31–39. [PubMed] [Google Scholar]
- Marcus, F. , McKenna, W. , Sherrill, D. , Basso, C. , Bauce, B. , Bluemke, D. , … Zareba, W. (2010). Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasi: Proposed modification of the task force criteria. Circulation, 121, 1533–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oechslin, E. N. , Jost, C. H. A. , Rojas, J. R. , Kaufmann, P. A. , & Jenni, R. (2000). Long‐term follow‐up of 34 adults with isolated left ventricular noncompaction: A distinct cardiomyopathy with poor prognosis. Journal of the American College of Cardiology, 36(2), 493–500. [DOI] [PubMed] [Google Scholar]
- Richardson, P. , McKenna, R. , Bristow, M. , Maisch, B. , Mautner, B. , O'connell, J. , … Nordet, P. (1996). Report of the 1995 world health organization/international society and federation of cardiology task force on the definition and classification of cardiomyopathies. Circulation, 93(5), 841–842. [DOI] [PubMed] [Google Scholar]
- Ritter, M. , Oechslin, E. , Sütsch, G. , Attenhofer, C. , Schneider, J. , & Jenni, R. (1997). Isolated noncompaction of the myocardium in adults. Mayo Clinic Proceedings, 72(1), 26–31. [DOI] [PubMed] [Google Scholar]
- Said, S. , Cooper, C. J. , Quevedo, K. , Rodriguez, E. , & Hernandez, G. T. (2013). Biventricular non‐compaction with predominant right ventricular involvement, reduced left ventricular systolic and diastolic function, and pulmonary hypertension in a hispanic male. The American Journal of Case Reports, 14, 539–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasse‐Klaassen, S. , Probst, S. , Gerull, B. , Oechslin, E. , Nürnberg, P. , Heuser, A. , … Thierfelder, L. (2004). Novel gene locus for autosomal dominant left ventricular noncompaction maps to chromosome 11p15. Circulation, 109(22), 2720–2723. [DOI] [PubMed] [Google Scholar]
- Sato, Y. , Matsumoto, N. , Matsuo, S. , Sakai, Y. , Kunimasa, T. , Imai, S. , … Saito, S. (2007). Right ventricular involvement in a patient with isolated noncompaction of the ventricular myocardium. Cardiovascular Revascularization Medicine, 8(4), 275–277. [DOI] [PubMed] [Google Scholar]
- Song, Z.‐Z. (2011). An isolated right ventricular hypertrabeculation and dyskinesia in an elderly man: A possible diagnosis of isolated right ventricular noncompaction? International Journal of Cardiology, 148(1), e3–e6. [DOI] [PubMed] [Google Scholar]
- Stähli, B. E. , Gebhard, C. , Biaggi, P. , Klaassen, S. , Buechel, E. V. , Jost, C. H. A. , … Greutmann, M. (2013). Left ventricular non‐compaction: Prevalence in congenital heart disease. International Journal of Cardiology, 167(6), 2477–2481. [DOI] [PubMed] [Google Scholar]
- Stollberger, C. , & Finsterer, J. (2010). Arrhythmias and left ventricular hypertrabeculation/noncompaction. Current Pharmaceutical Design, 16(26), 2880–2894. 10.2174/138161210793176518 [DOI] [PubMed] [Google Scholar]
- Ulusoy, R. E. , Kucukarslan, N. , Kirilmaz, A. , & Demiralp, E. (2006). Noncompaction of ventricular myocardium involving both ventricles. European Journal of Echocardiography, 7(6), 457–460. [DOI] [PubMed] [Google Scholar]
- Weiford, B. C. , Subbarao, V. D. , & Mulhern, K. M. (2004). Noncompaction of the ventricular myocardium. Circulation, 109(24), 2965–2971. [DOI] [PubMed] [Google Scholar]
- Ying, Z.‐Q. , Xu, G. , Chen, S. , Ma, J. , & You, X.‐D. (2008). Cerebral infarction in an adult patient with right ventricular hypertrabeculation/noncompaction. International Journal of Cardiology, 127(3), e150–e151. [DOI] [PubMed] [Google Scholar]


