Abstract
Background
Takotsubo cardiomyopathy (TC) can resemble acute anterior ST‐elevation myocardial infarction. Most studies have examined TC in Asians and Caucasians (non‐African Americans [AA]), while very few cases have been reported in AA. We aimed to assess the electrocardiographic features of TC in AA patients and compare them to non‐AA TC patients.
Methods
We retrospectively compared electrocardiograms of 52 AA and 47 non‐AA patients diagnosed with TC. All patients met the modified Mayo Clinic criteria for the diagnosis of TC. Information collected included PR interval, QRS duration and amplitude, QT interval in milliseconds (msec) adjusted for heart rate (QTc), ST‐segment deviation at the J point in limb and precordial leads (≥1 mm), ST elevation (≥1 mm), and T‐wave inversion (≥0.5 mm).
Results
T‐wave inversion was more prevalent on presentation among AA patients (82% vs 48% in non‐AA; P < 0.01), whereas ST depression was more common among non‐AA (21% vs 7% in AA; P = 0.05). T‐wave inversions in AA patients were frequent in both limb and precordial leads, whereas T‐wave inversions in non‐AA were limited to precordial leads. The average QTc upon presentation in AA was longer than non‐AA (491 msec in AA vs 456 msec in non‐AA; P < 0.01) as was the maximum average QTc during index hospitalization (527 msec in AA vs 497 msec in non‐AA, P = 0.03).
Conclusion
In patients presenting with TC, AA patients more frequently present with diffuse T‐wave inversions and a more prolonged QTc, whereas non‐AA patients more often present with ST depressions. AA patients also more frequently present with T‐wave inversions diffusely, whereas non‐AA patients present with T‐wave inversions more limited to the precordial leads.
Keywords: takotsubo, African American, electrocardiography, cardiomyopathy, apical ballooning
Takotsubo cardiomyopathy (TC), also known as stress‐induced cardiomyopathy, is reported to frequently resemble acute anterior ST‐elevation myocardial infarction (STEMI) on electrocardiogram (ECG). TC is characterized by apical or midventricular wall motion abnormalities, despite nonobstructive coronary artery disease. TC commonly affects postmenopausal women after a stressful event and usually presents with chest pain and dyspnea.
The most common reported electrocardiographic abnormality in the acute phase of TC is mild ST‐segment elevation beyond the distribution of a single coronary artery, followed by T‐wave inversions, and QT interval prolongation in the subacute phase.1, 2, 3 Several attempts have been made to differentiate STEMI from TC in order to select the appropriate treatment strategy, especially in the acute phase, with several ECG criteria proposed in the literature.4
However, the reported prevalence of ST elevation upon admission for TC is variable in the literature.5, 6, 7 Further, most of the literature has reported TC in Asians and Caucasians (non‐African Americans [AA]), who are the most commonly affected ethnic populations, with very few cases reported in AA.8 We aimed to assess the electrocardiographic features of TC in AA patients and compare them to non‐AA TC patients.
METHODS
We conducted a retrospective, descriptive study reviewing patients with the discharge diagnosis of stress‐induced cardiomyopathy or TC between 2003 and 2013 at Einstein Medical Center, Philadelphia, PA.
Inclusion criteria were as per modified Mayo Clinic criteria:9 (1) akinesia or dyskinesia of the apical and/or midventricular segments of the left ventricle with regional wall motion abnormalities that extended beyond the distribution of a single epicardial vessel, (2) absence of obstructive coronary artery disease, (3) new electrocardiographic abnormalities, and (4) absence of pheochromocytoma or myocarditis. A total of 99 patients from different racial and ethnic backgrounds (Hispanics, Whites, and AA) met the Mayo Clinic Criteria and were included in the study.
We retrospectively evaluated ECGs collected upon admission, at 24 and 48 hours, at discharge, and prior to the index event when available. All patients developed symptoms within 12 hours of recording initial ECGs. The ECGs during the index event were compared to prior ECGs and new changes were collected. All ECG measurements were analyzed by two investigators blinded to the demographic information.
Information collected included PR interval, QRS duration and amplitude, QT interval in milliseconds (msec) adjusted for heart rate (QTc) using the Bazett's formula, ST‐segment deviation at the J point in limb and precordial leads (≥1 mm), ST elevation (≥1 mm), and T‐wave inversion (≥0.5 mm).
Chi‐square and the Student's t‐tests were used to assess statistical differences in categorical and continuous variables, respectively. A 2‐tailed P < 0.05 was considered statistically significant. All analyses were performed employing Excel 2010 and IBM SPSS Statistics 22 (IBM Corp., Armonk, NY).
This study was approved by the hospital's Institutional Review Board.
RESULTS
A total of 99 patients met the modified Mayo criteria for the diagnosis of TC. Fifty‐two patients were AA and 47 were non‐AA. Non‐AA patients included 7 Hispanics, 2 Asians, and 38 Caucasians. Seventeen were males and 82 females. See basic clinical characteristics of our population in Table1.
Table 1.
Baseline Characteristics by Race in Patients Diagnosed with Takotsubo Cardiomyopathy
| African American | Non‐African American | ||
|---|---|---|---|
| (n = 52) | (n = 47) | P Value | |
| Mean age ± SD | 67.3 ± 14.3 | 63.9 ± 16.3 | 0.4 |
| Male | 8 (15%) | 9 (19%) | 0.6 |
| Hypertension | 39 (75%) | 31 (66%) | 0.5 |
| Diabetes mellitus type 2 | 15 (29%) | 7 (15%) | 0.1 |
| Hyperlipidemia | 24 (46%) | 17 (36%) | 0.3 |
| Smoking history | 21 (40%) | 19 (40%) | 0.9 |
| Heart failure during index event | 18 (34.6%) | 12 (25.5%) | 0.7 |
| LV thrombus | 2 (3.8%) | 1 (2.1%) | 0.6 |
| In‐hospital death | 5 (9.6%) | 6 (12.7%) | 0.6 |
| LVEF upon admission | 31% | 35% | 0.1 |
| LVEF follow‐up | 52% | 57% | 0.7 |
SD = standard deviation; LV = left ventricle; LVEF = left ventricular ejection fraction.
T‐wave inversion was more prevalent upon presentation in AA patients (n = 45; 82% vs n = 23; 48% in non‐AA; P < 0.01), whereas ST depression was more common in non‐AA patients (n = 10; 21% vs n = 4; 7% in AA; P = 0.05). At 48 hours after admission, the frequency of T‐wave inversions was similar in both groups. See typical ECG examples in an AA and a non‐AA patient in Figures 1 and 2, respectively.
Figure 1.
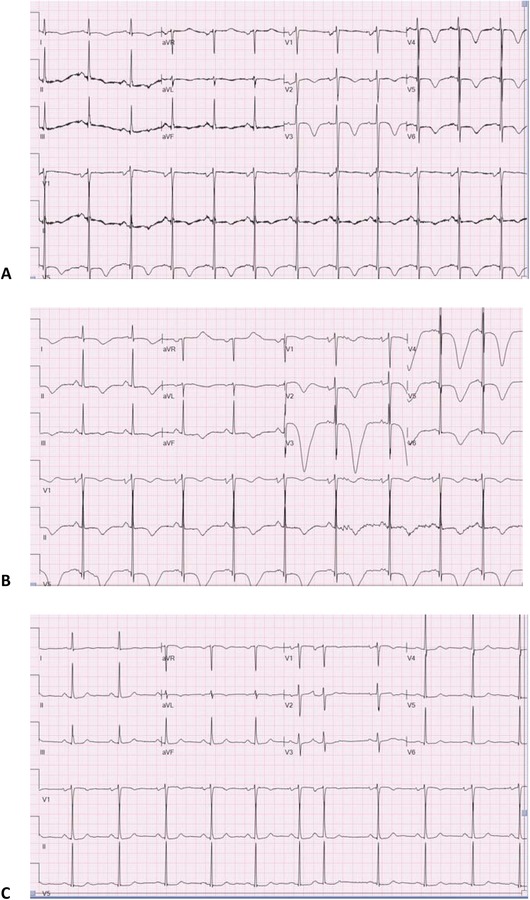
Representative ECG in an AA patient: (A) ECG on admission showing sinus rhythm with diffuse T‐wave inversions, (B) ECG at 48 hours with deeper T‐wave inversions, and (C) ECG at follow‐up with resolution of T‐wave inversions.
Figure 2.
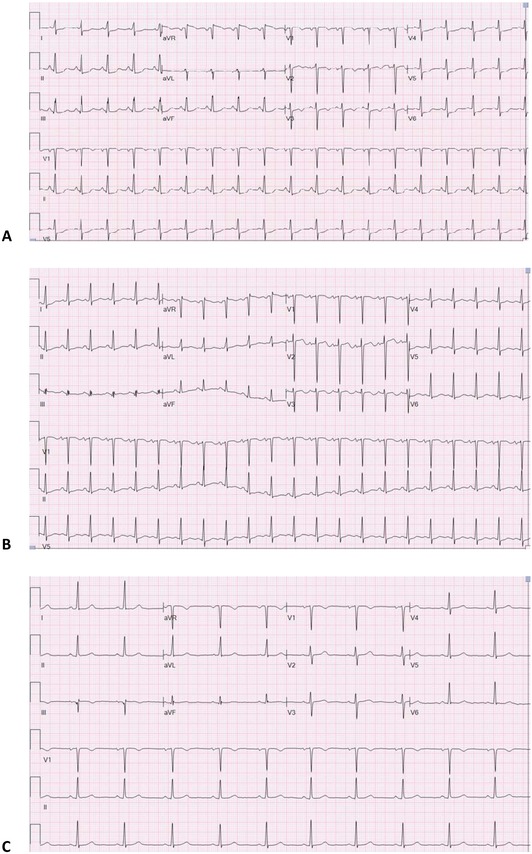
Representative ECG in a non‐AA patient: (A) ECG on admission showing sinus tachycardia with diffuse ST depressions and T‐wave inversions in V1–V3, (B) ECG at 48 hours with persistent T‐wave inversions in V1–V3 and mild improvement of diffuse ST depressions, and (C) ECG at follow‐up with resolution of ST‐depressions and T‐wave inversions.
Upon presentation, T‐wave inversions among AA patients were more frequent in both limb and precordial leads (31% and 54%, respectively) when compared with T‐wave inversions in non‐AA patients which were more limited to the precordial leads (11% and 24%, respectively). Frequency of T‐wave inversions in individual limb leads in AA versus non‐AA included lead I (n = 22; 42% vs n = 9; 19%; P = 0.01), II (n = 16; 31% vs n = 5; 11%; P = 0.01), III (n = 13; 25% vs n = 5; 11%; P = 0.06), aVR (n = 17; 33% vs n = 7; 15%; P = 0.03), aVL (n = 23; 44% vs n = 10; 21%; P = 0.01), and aVF (n = 17; 33% vs n = 4; 9%; P = 0.03). See Table 2.
Table 2.
Electrocardiographic Features by Race in Patients Diagnosed with Takotsubo Cardiomyopathy
| African American | Non‐African American | ||
|---|---|---|---|
| ECG Features at Presentation | (n = 52) | (n = 47) | P Value |
| PR interval | 149 msec | 153 msec | NS |
| QRS duration | 91 msec | 90 msec | NS |
| Prolonged QTca | 36 (70%) | 27 (59%) | |
| Mean QTc interval | 491 msec | 456 msec | <0.01 |
| ST depression | 4 (7)% | 10 (21%) | 0.05 |
| ST elevation | 11 (21%) | 12 (26%) | 0.6 |
| T‐wave inversion | 45 (82%) | 23 (48%) | <0.01 |
| Lead I | 22 (42%) | 9 (19%) | 0.01 |
| Lead II | 16 (31%) | 5 (11%) | 0.01 |
| Lead III | 13 (25%) | 5 (11%) | 0.06 |
| Lead aVR | 17 (33%) | 7 (15%) | 0.03 |
| Lead aVL | 23 (44%) | 10 (21%) | 0.01 |
| Lead aVF | 17 (33%) | 4 (9%) | 0.03 |
| Lead V1 | 13 (25%) | 9 (19%) | 0.4 |
| Lead V2 | 21 (40%) | 13 (28%) | 0.1 |
| Lead V3 | 23 (44%) | 11 (23%) | 0.05 |
| Lead V4 | 26 (50%) | 11 (23%) | 0.01 |
| Lead V5 | 27 (52%) | 11 (23%) | <0.01 |
| Lead V6 | 26 (50%) | 10 (21%) | <0.01 |
aProlonged QTC (QTc ≥ 450 for both genders).
ECG = electrocardiogram; NS = nonstatistically significant.
When we evaluated T‐wave inversions in the precordial leads we found that there was no statistically significant (NS) difference in leads V1 and V2 between groups, but V3 through V6 in AA versus non‐AA patients were significant as follows: V3 (n = 23; 44% vs n = 11; 23%; P = 0.05), V4 (n = 26; 50% vs n = 11; 23%; P = 0.01), V5 (n = 27; 52% vs n = 11; 23%; P < 0.01), and V6 (n = 26; 50% vs n = 10; 21%; P < 0.01).
The average QTc upon presentation in AA was higher than in non‐AA (491 msec vs 456 msec; P < 0.01), as well as the maximum achieved average QTc during index hospitalization (527 msec vs 497 msec; P = 0.03). Based on standard criteria (≥450 msec in both genders), we found QTc prolongation in 70% (n = 36) of AA and 59% (n = 27) of non‐AA.
ST elevation was present in 26% of non‐AA patients and 21% of AA (P = 0.6) patients. Only two patients (non‐AA) had reciprocal ST depression in the inferior leads. ST elevations were more frequent in the precordial versus limb leads in both groups.
The mean QRS duration was similar in both groups at 90 msec. The mean PR interval was also similar in both groups (149 msec in AA and 153 msec in non‐AA; P: NS).
None of the patients diagnosed with TC had other comorbidities, such as hemorrhagic stroke, during the index event that could potentially be associated with the development of deep T‐wave inversions.
DISCUSSION
The findings of this study examining ECG changes with TC in AA versus non‐AA patients include:
-
1.
AA patients more frequently present with global T‐wave inversion and QTc prolongation.
-
2.
AA patients have less ST depression on presentation when compared with non‐AA patients; however, ST depressions are present in a minority of both groups.
-
3.
AA patients more frequently present with T‐wave inversions diffusely, whereas non‐AA patients present with T‐wave inversions more limited to the precordial leads.
The classic evolutionary ECG changes described in TC include acute ST elevation which resolves within 1 to 2 days, followed by the development of diffuse T‐wave inversion involving most leads, as well as prolongation of the corrected QT interval.10
Our study found that AA more commonly present with diffuse T‐wave inversions and QTc prolongation, which is more consistent with a non‐STEMI picture. Our findings support a prior report of four AA patients with TC.8 Patel et al. reported rapid development of deep, broad, diffuse T‐wave inversions with a prolonged QT interval within 2 to 48 hours of presentation in five AA patients.11 Thus, TC may be underdiagnosed in AA if we rely on ST elevation to make the diagnosis.
In our study, non‐AA patients presented less frequently with T‐wave inversions, and when present, they were more limited to the precordial leads.
We found ST elevation in approximately 25% of TC cases upon presentation, and this was mostly limited to non‐AA. In the literature, there is a significant variability in the reported frequency of ST elevation upon presentation, ranging from 34% to 100%.5, 6, 7 Reasons that may account for this variability in the reported frequency of ST‐segment elevation include: first, most of these findings have been documented in non‐AA; and second, the elevation is transient, and therefore, the time from symptom onset to presentation may influence whether it is detected.10
Two studies reported that a lack of ST elevation in V1 and ST‐depression in aVR distinguished TC from STEMI.4, 12 In contrast, in our study, seven patients presented with ST elevation in V1 (two AA and five non‐AA). Only two patients presented with reciprocal changes when they presented with acute ST elevations which is similar to other reports.13, 14
Nascimento et al.15 reported that the most common ECG abnormalities in Hispanics consisted of T‐wave inversions, followed by ST elevations and ST depressions. In our study, four out of seven Hispanic patients presented with initial T‐wave inversions.
The reason for these electrocardiographic differences between AA and non‐AA patients diagnosed with TC remains to be elucidated, but may involve complex interactions between genetic predisposition, response to stress, and potential physiological differences.
CONCLUSIONS
Among patients presenting with TC, AA patients more frequently present with diffuse T‐wave inversions and a more prolonged QTc, whereas non‐AA patients more often present with ST depression.
Further studies with large populations are needed to better characterize the variability in incidence, prevalence, and presentation of patients diagnosed with TC and different ethnic backgrounds.
CLINICAL PERSPECTIVE
In clinical practice, it would be helpful to identify electrocardiographic features that suggest a diagnosis of TC in a patient presenting with an acute coronary syndrome. It would be of further benefit to know that TC presentation on ECG varies based on race. Currently, AA constitute the second largest racial and ethnic minority in the United States. However, most of the literature describes ECG features of Caucasian and Asian patients with TC. Little is known to date about TC ECG features in AA patients. In the present study we found that AA patients diagnosed with TC present differently than non‐AA patients on index ECG. Recognizing typical ECG patterns of TC by race may lead to earlier diagnosis and appropriate treatment.
Ann Noninvasive Electrocardiol 2016;21(5):486–492
Conflict of Interest: The authors have no conflict of interest.
REFERENCES
- 1. Gianni M, Dentali F, Grandi AM, et al. Apical ballooning syndrome or takotsubo cardiomyopathy: A systematic review. Eur Heart J 2006;27:1523–1529. [DOI] [PubMed] [Google Scholar]
- 2. Perazzolo M, Zorzi A, Orbetti F, et al. Apicobasal gradient of left ventricular myocardial edema underlies transient T‐wave inversion and QT interval prolongation (Wellens' ECG pattern) in Tako‐Tsubo cardiomyopathy. Heart Rhythm 2013;10:70–77. [DOI] [PubMed] [Google Scholar]
- 3. Kurisu S, Inoue I, Kawagoe T, et al. Time course of electrocardiographic changes in patients with tako‐tsubo syndrome: Comparison with acute myocardial infarction with minimal enzymatic release. Circ J 2004;68:77–81. [DOI] [PubMed] [Google Scholar]
- 4. Parkkonen O, Allonen J, Vaara S, et al. Differences in ST‐elevation and T‐wave amplitudes do not reliably differentiate takotsubo cardiomyopathy from acute anterior myocardial infarction. J Electrocardiol 2014;47:692–699. [DOI] [PubMed] [Google Scholar]
- 5. Dib C, Asirvatham S, Elesber A, et al. Clinical correlates and prognostic significance of electrocardiographic abnormalities in apical ballooning syndrome (Takotsubo/stress‐induced cardiomyopathy). Am Heart J 2009;157(5):933–938. [DOI] [PubMed] [Google Scholar]
- 6. Sharkey SW, Lesser JR, Menon M, et al. Spectrum and significance of electrocardiographic patterns, troponin levels, and thrombolysis in myocardial infarction frame count in patients with stress (tako‐tsubo) cardiomyopathy and comparison to those in patients with ST‐elevation anterior wall myocardial infarction. Am J Cardiol 2008;101(12):1723–728. [DOI] [PubMed] [Google Scholar]
- 7. Bybee KA, Kara T, Prasad A, et al. Systematic review: Transient left ventricular apical ballooning: A syndrome that mimics ST‐segment elevation myocardial infarction. Ann Intern Med 2004;141:858–865. [DOI] [PubMed] [Google Scholar]
- 8. Qaqa A, Daoko J, Jallad N, et al. Takotsubo syndrome in African American vs. non‐African American women. West J Emerg Med 2011;12:218–223. [PMC free article] [PubMed] [Google Scholar]
- 9. Kawai S, Kitabatake A, Tomoike H, Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J 2007;71:990–992. [DOI] [PubMed] [Google Scholar]
- 10. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako‐Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am Heart J 2008;155:408–417. [DOI] [PubMed] [Google Scholar]
- 11. Patel HM, Kantharia BK, Morris DL, et al. Takotsubo syndrome in African‐American women with atypical presentations: A single‐center experience. Clin Cardiol 2007;30:14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kosuge M, Ebina T, Hibi K, et al. Simple and accurate electrocardiographic criteria to differentiate takotsubo cardiomyopathy from anterior acute myocardial infarction. J Am Coll Cardiol 2010;55:2514–2516. [DOI] [PubMed] [Google Scholar]
- 13. Ogura R, Hiasa Y, Takahashi T, et al. Specific findings of the standard 12‐lead ECG in patients with 'Takotsubo' cardiomyopathy: Comparison with the findings of acute anterior myocardial infarction. Circ J 2003;67:687–690. [DOI] [PubMed] [Google Scholar]
- 14. Inoue M, Shimizu M, Ino H, et al. Differentiation between patients with takotsubo cardiomyopathy and those with anterior acute myocardial infarction. Circ J 2005;69:89–94. [DOI] [PubMed] [Google Scholar]
- 15. Nascimento FO, Santana O, Perez‐Caminero M, et al. The characteristics of stress cardiomyopathy in an ethnically heterogeneous population. Clinics (Sao Paulo) 2011;66:1895–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]


