Abstract
Brugada syndrome (BrS) is an inherited channelopathy that predisposes individuals to malignant arrhythmias and can lead to sudden cardiac death. The condition is characterized by two electrocardiography (ECG) patterns: the type‐1 or “coved” ECG and the type‐2 or “saddleback” ECG. Although the type‐1 Brugada ECG pattern is diagnostic for the condition, the type‐2 Brugada ECG pattern requires differential diagnosis from conditions that produce a similar morphology. In this article, we present a case that is suspicious but not diagnostic for BrS and discuss the application of ECG methodologies for increasing or decreasing suspicion for a diagnosis of BrS.
Keywords: Brugada ECG pattern, electrocardiography, ECG criteria
Brugada syndrome (BrS) is an inherited channelopathy that displays autosomal dominant inheritance of variable penetrance.1 The condition has been linked to over 70 mutations, most of which are related to cardiac sodium channels, with the SCN5A gene being implicated in about 25% of cases.2 Patients with BrS may be asymptomatic until the point of sudden death because of polymorphic ventricular tachycardia/fibrillation as the first clinical manifestation of the condition. The hallmark of BrS lies in the electrocardiogram (ECG) in which one of two patterns may be observed: (i) type‐1, or coved pattern, depicting ST‐segment elevation, followed by a symmetric negative T wave in the right precordial leads and; (ii) type‐2 or Saddle‐back pattern, depicting an r’ wave in lead V1 followed by ST‐segment elevation, which is convex respect to the isoelectric line and by a T wave that is positive in lead V2 and variable in V1.3 Although the type‐1 Brugada ECG pattern is diagnostic for BrS, the type‐2 Brugada ECG pattern requires differential diagnosis from conditions that produce a similar morphology.3 These include normal variant because of inadvertent placement of leads in the second and third intercostal space, incomplete right bundle branch block (IRBBB), healthy athletes, pectus excavatum, arrhythmogenic right ventricular dysplasia (ARVD), electrolyte abnormalities, and early repolarization.4, 5, 6, 7, 8 The ECG is an important tool in the evaluation of cardiac disease and although it appears to be relatively archaic, it continues to prove itself as a valuable instrument in the diagnosis of complex arrhythmic disease. A number of recent studies have validated specific ECG criteria as tools to rule in or out disease such as ARVD,9, 10 or differentiate between Brugada ECGs and IRBBB11 or healthy athletes.12 The purpose of this manuscript is to review recently published electrocardiographic techniques that allow for the differentiation of a Brugada ECG pattern from other mimicking patterns and to apply them to a real case.
CASE PRESENTATION
A 31‐year‐old man with no cardiovascular history presented to the emergency department with possible heat stroke. His family history was significant for a second cousin who died at 20 years old, however the patient had no personal history of syncope, arrhythmias, or aborted sudden cardiac death. Physical exam was unremarkable. A 12‐lead ECG revealed an r’ in leads V1 and V2; raising suspicion for a diagnosis of BrS with a possible type‐2 Brugada ECG pattern (Fig.1). He was referred to the arrhythmia clinic for diagnostic evaluation of BrS where he received a provocative test with a sodium channel‐blocking agent (procainamide), the results of which were negative. How can we reliably distinguish the Brugada ECG pattern from conditions that present with similar morphologies?
Figure 1.
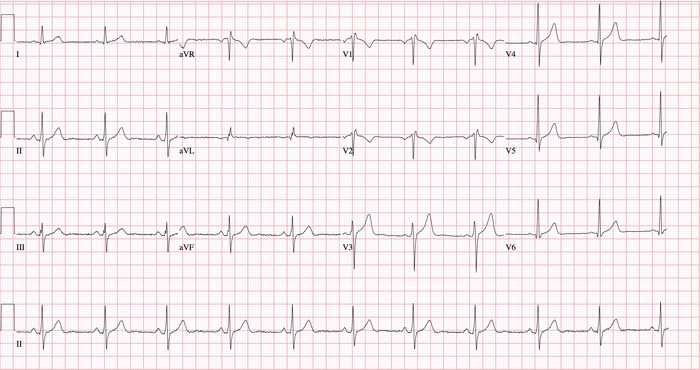
Presenting ECG displaying an r′ wave in leads V1 and V2.
DISCUSSION
Differentiating between the type‐2 Brugada ECG pattern and other patterns presenting with an r’ wave may be difficult, yet this distinction is of the utmost importance as management differs from one condition to the next, with misdiagnoses having potentially fatal consequences. In 2011, Chevalier et al.11 successfully distinguished between type‐2 Brugada ECG patterns and IRBBB ECG patterns through employment of newly developed ECG criteria. Two ECG parameters were measured in their study: (i) the α‐angle, defined as the angle between a vertical line and the downslope of the r’ wave; and (ii) the β‐angle, defined as the angle between the upslope of the S wave and the downslope of the r’ wave (Fig. 2A).11 The authors determined that the β‐angle had a higher sensitivity and specificity than the α‐angle. Using a cutoff value of ≥58°, Chevalier et al. concluded that the β‐angle had a sensitivity of 79% and specificity of 83% for the diagnosis of a Brugada ECG pattern. Subsequently, in a study performed by Serra et al.,12 the β‐angle was further validated along with three new criteria in the distinction of a type‐2 Brugada ECG pattern from the ECG pattern of healthy athletes. These included: (i) the duration of the base of the triangle between the upslope of the S wave and the downslope of the r’ wave at 0.5 mV from the high takeoff; (ii) the duration of the base of the triangle at the isoelectric line; and (iii) the ratio of base/height of the triangle formed by the upslope of the S wave and the downslope of the r’ wave at the isoelectric line (Fig. 2B).12 The authors determined that the base of the triangle at 5 mm from the high takeoff was the easiest parameter to measure. Using a cutoff value of ≥4 mm (160 milliseconds), the base of the triangle had a sensitivity of 95.6% and specificity of 85% for the detection of a Brugada ECG pattern. These criteria have only been validated for the patterns of healthy athletes or IRBBB. Brugada phenocopies (BrP) are the leading differential diagnosis for a BrS. These criteria are currently being tested in the differentiation of the two conditions. In the evaluation of Brugada ECG patterns, current recommendations for differentiation between BrS and BrP focus on the systematic diagnostic criteria including a provocative test, which is of the utmost importance.13, 14
Figure 2.
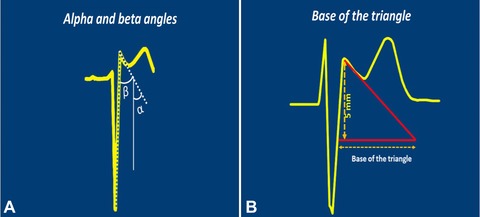
(A) The α and β angles as described by Chevalier et al.7 (B) The base of the triangle measured at 5 mm from the high takeoff as described by Serra et al.8
APPLYING THE NEW CRITERIA TO THE PRESENTED CASE
The presented ECG shows sinus rhythm with a rate of approximately 60 beats per minute with a normal axis. Precordial leads V1 and V2 display an RSR’ pattern with T wave inversion in leads V1 and V2. Immediately, one notices the inverted T wave in V2, which is atypical of the type‐2 Brugada ECG pattern that usually presents with a T wave that is positive in lead V2 and variable in V1. The β‐angle, between the upslope of the S wave and the downslope of the r’ wave, was measured at 29° and 28° in leads V1 and V2, respectively (Fig. 3A). The duration of the base of the triangle between the upslope of the S wave and the downslope of the r’ wave at 0.5 mV from the high takeoff was measured at 2.4 and 2.3 mm, respectively (Fig. 3B). These measurements, both falling well below their respective cutoff values suggest a low probability for the Brugada ECG pattern.
Figure 3.
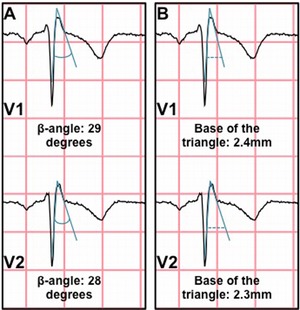
The measurements of three criteria applied to the case. (A) The base of the triangle. (B) The β‐angle. All measurements fell well below the cutoff values required for a type‐2 Brugada ECG pattern.
In this case, a remote family history of early death coupled with the patient's presenting symptoms of heat stroke and an ECG pattern showing a morphology suggestive of a Brugada ECG pattern was suspicious enough for BrS to prompt further investigation with a sodium channel blocking agent, the results of which were negative. We demonstrated how the use of the β‐angle and the base of the triangle were able to effectively rule out the diagnosis of a Brugada ECG pattern thereby reducing suspicion for BrS, which was definitively ruled out through a negative provocative test.
Conflict of Interest Disclosure: None.
REFERENCES
- 1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome: a multicenter report. J Am Coll Cardiol 1992;20:1391–1396. [DOI] [PubMed] [Google Scholar]
- 2. Probst V, Wilde AA, Barc J, et al. SCN5A mutations and the role of genetic background in the pathophysiology of Brugada syndrome. Circ Cardiovasc Genet 2009;2:552–557 [DOI] [PubMed] [Google Scholar]
- 3. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol 2012;45:433–442. [DOI] [PubMed] [Google Scholar]
- 4. Bayés de Luna A, García‐Niebla J, Baranchuk A. New electrocardiographic features in Brugada syndrome. Curr Cardiol Rev 2014;10:175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baranchuk A, Enriquez A, García‐Niebla J, et al. Differential diagnosis of rSr’ pattern in leads V1‐V2. Comprehensive review and proposed algorithm. Ann Noninvasive Electrocardiol 2015; 20:7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koppikar S, Barbosa‐Barros R, Baranchuk A. A practical approach to the investigation of an rSr’ pattern in leads V1‐V2. Can J Cardiol 2015. Apr 18 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 7. Awad SF, Barbosa‐Barros R, Belem Lde S, et al. Brugada phenocopy in a patient with pectus excavatum: systematic review of the ECG manifestations associated with pectus excavatum. Ann Noninvasive Electrocardiol 2013;18(5):415–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Genaro NR, Anselm DD, Cervino N, et al. Brugada phenocopy clinical reproducibility demonstrated by recurrent hypokalemia. Ann Noninvasive Electrocardiol 2014;19(4):387–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gottschalk B, Gysel M, Barbosa‐Barros R, et al. The use of fontaine leads in the diagnosis of arrhythmogenic right ventricular dysplasia. Ann Noninvasive Electrocardiol 2014;19:279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hoffmayer KS, Bhave PD, Marcus GM, et al. An electrocardiographic scoring system for distinguishing right ventricular outflow tract arrhythmias in patients with arrhythmogenic right ventricular cardiomyopathy from idiopathic ventricular tachycardia. Heart Rhythm 2013;10(4):477–482. [DOI] [PubMed] [Google Scholar]
- 11. Chevallier S, Forclaz A, Tenkorang J, et al. New electrocardiographic criteria for discriminating between Brugada types 2 and 3 patterns and incomplete right bundle branch block. J Am Coll Cardiol 2011;58:2290–2298. [DOI] [PubMed] [Google Scholar]
- 12. Serra G, Baranchuk A, Bayes‐De‐Luna A, et al. New electrocardiographic criteria to differentiate the type‐2 Brugada pattern from electrocardiogram of healthy athletes with r′‐wave in leads V1/V2. Europace 2014;16:1639–1645. [DOI] [PubMed] [Google Scholar]
- 13. Baranchuk A, Nguyen T, Ryu MH, et al. Brugada phenocopy: new terminology and proposed classification. Ann Noninvasive Electrocardiol 2012;17(4):299–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gottschalk B, Anselm DD, Baranchuk A. Brugada phenocopy: morphological classification and importance of provocative testing. Ann Noninvasive Electrocardiol 2014;19(6):604–605. [DOI] [PMC free article] [PubMed] [Google Scholar]


