Abstract
Patent foramen ovale (PFO) is thought to be a risk factor for decompression illness (DCI). Catheter‐based closure procedure reduces the risk of DCI in selected scuba divers with PFO. Major complication of invasive approach are rare, minor, especially heart rhythm disturbances are reported relatively often. We describe a case of 41‐year‐old diver, who underwent PFO closure due to recurrent DCI events. Afterward, he experienced no DCI symptoms; however, he complained about feeling of the heart beating during a submersion. Arrhythmia should be considered as a life‐threatening for scuba diver, thus we performed underwater ECG monitoring and exclude the arrhythmia.
Keywords: electrocardiography, Holter
1. Introduction
The prevalence of patent foramen ovale (PFO) among divers is not known, but the number of scuba divers with patent foramen ovale worldwide is estimated to be in millions. It was postulated that a cardiac right‐to‐left shunt (RLS) through a PFO allows paradoxical gas embolism and could be a substrate for the skin and the neurological form of decompression illness (DCI) (Billinger et al., 2011). There are limited data about management and clinical setting of divers with PFO. The efficacy of PFO closure in the prevention of DCI is not defined. Furthermore, peri‐ and postprocedural complications might occur. High prevalence of postprocedural arrhythmias was observed in same nonrandomized comparative studies, however, research results are inconclusive (Gaspardone et al., 2013; Spies, Khandelwal, Timmermanns, & Schräder, 2008). Cardiac arrhythmias may be more frequent in scuba divers because of the submersion reflex. We present a case of a technical scuba diver (scuba diver that exceeds the limits of recreational diving) who underwent percutaneous PFO closure due to recurrent DCI episodes, and afterward complained about uncomfortable feeling of the heart beating during a submersion.
2. Case Report
A fit, 41‐year‐old male was admitted to the Department of Cardiology for percutaneous PFO closure. The patient, technical scuba diver, complained of recurrent DCI events. He reported several incidences of skin DCS (itchy rash on the belly), one episode of vertigo and nausea with short latency after surfacing and one short incidence of clouding of consciousness, which occurred during the ascent. All episodes were associated with decompression dives, and occurred even if desaturation time was extended. The patient denied preexisting medical conditions. The physical examination of the patient was normal, same as ECG, Holter ECG, chest x‐ray and routine laboratory tests’ results. There were no abnormalities in transthoracic echocardiography (TTE). Transesophageal echocardiography (TEE) revealed phasic excursion of interatrial septum into the left atrium in cardiorespiratory cycle and temporary blood flow through PFO (Figure 1). For the detection of right‐to‐left (RLS) shunting across the PFO, contrast medium was injected into antecubital vain. More than 20 contrast bubbles crossed over into the left atrium (Figure 2). RLS contrast shunting was revealed without the Valsalva maneuver. The percutaneous PFO closure was successfully performed with the 26 mm Nit‐Occlud‐PFO occluder system (Figure 3). Before device implantation, the patient received 1 g of cefazolin intravenously and loading dose of aspirin (300 mg) and clopidogrel (300 mg). The procedure was guided by fluoroscopy and TEE. After the procedure, dual antiplatelet therapy was prescribed for 3 months and then aspirin alone for the next 3 months (75 mg/daily). Infective endocarditis prophylaxis and break from diving were recommended for a time of 6 months. The patient was discharged a day later in a stable condition and 12 weeks later control TEE was performed showing no residual leak. He returned to unrestricted diving 6 months after PFO closure. No episode of DCI occurred, but he complained about uncomfortable feeling of the heart beating that appeared repeatedly during the submersion. He denied having fast heart palpitations, chest pain, shortness of breath, or any other symptoms. The 24‐hours ECG Holter was recorded and it revealed a few single supraventricular (n = 6) and ventricular (n = 10) premature beats not induced by physical activity. The ECG exercise test was negative and the results of blood tests were normal. To exclude arrhythmias mediated by cold‐water submersion, we performed Holter ECG monitoring during diving. The freshwater dive was done using air as breathing gas and technical diving gear in the standard configuration. A Holter was set up under a dry suit. The patient, while diving, was assisted by rescue diver. A depth of 30 m was slowly reached by descent along the slope and then the ascent was conducted using Minimum Deco strategy. During the ascent, some underwater exercises were done to provoke arrhythmias. The dive lasted 1 hr 14 min, the visibility varied from 2 to 3.5 m, the water temperature ranged from 8° to 11°C (Figure 4). Holter ECG revealed no rhythm abnormalities. Interestingly, submersion‐inducted heart rate drop was not found (Figure 4). The patient was reassured and no specific action was required. Afterward, the patient performed 55 dives (about 30 with decompression) without negative symptoms.
Figure 1.
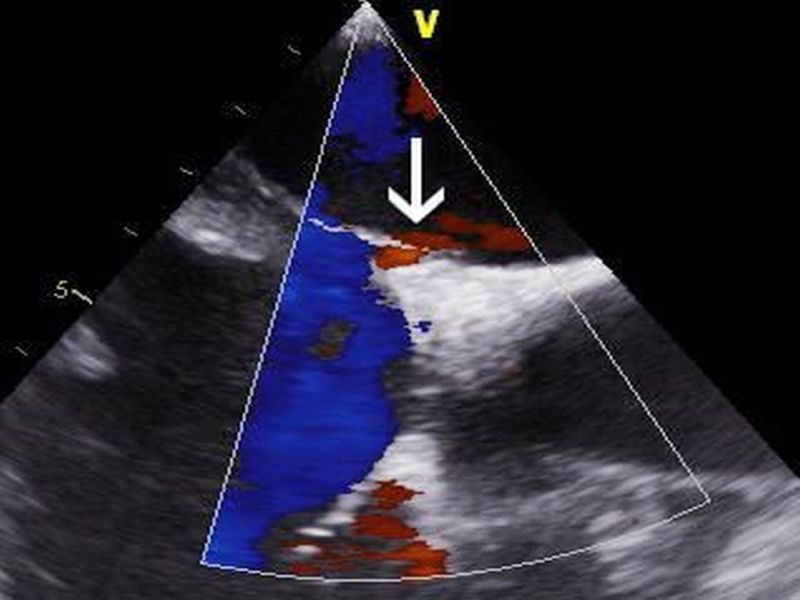
Transesophageal echocardiography. Temporary right‐to‐left shunt through the patent foramen ovale (arrow)
Figure 2.
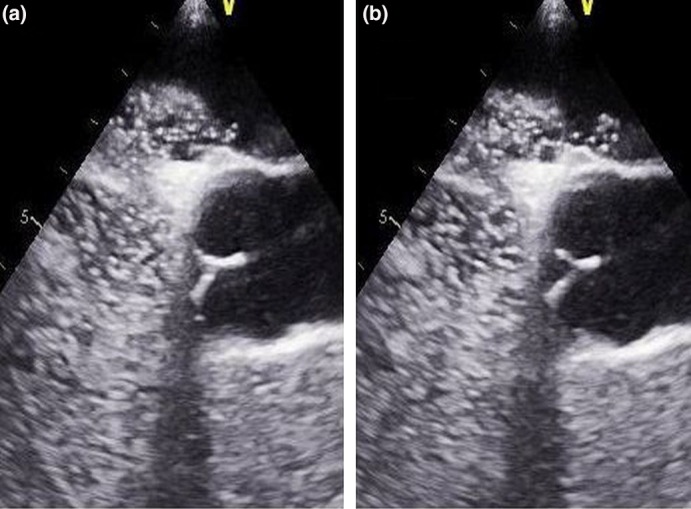
Transesophageal echocardiography (a‐b). Crossover of contrast bubbles from right‐to‐left atrium
Figure 3.
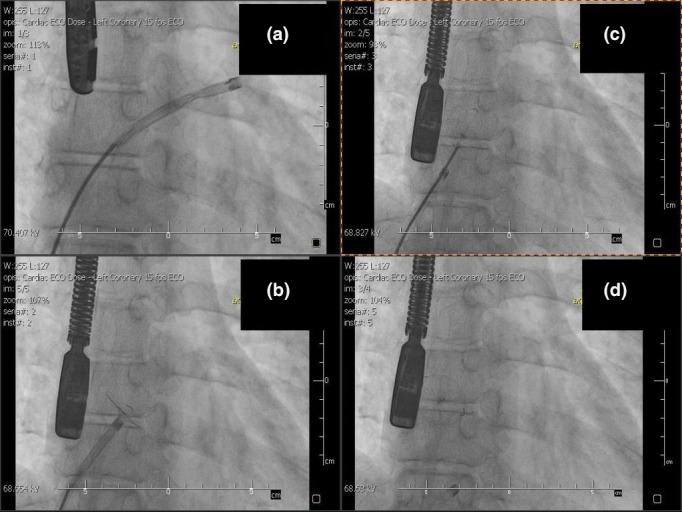
The catheter‐based patent foramen ovale (PFO) closure: (a) Cannula in the right atrium. (b, c) Release of PFO closure device. (d) Final result
Figure 4.

Diving profile and Holter monitor strips: (a) submersion (b) the depth of 30 m (c) emersion
3. Discussion
The recommendations for divers with PFO and unprovoked decompression events include discontinuation of diving, conservative approach to diving, or PFO closure (Honěk et al., 2014). The role of catheter‐based PFO closure in prevention of DCI incidences is not established. Nevertheless, Honěk et al. (2014) reported that invasive management might eliminate the arterializations of venous bubbles. Billinger et al. (2011) found that PFO closure reduced the risk of symptomatic and asymptomatic neurological incidences associated with scuba diving. Also, Pearman, Bugeja, Nelson, Szantho, & Turner (2015) retrospectively assessed that after PFO closure, the majority of scuba divers are able to return to unrestrictive diving. Our patient wished to continue technical diving, so invasive approach was advocated in this case.
The patient was informed about limited data on efficacy of PFO closure and about potential peri‐ and postprocedural complications. Serious complications, however, are rare and occur in <1% of cases (Meier, 2005). Unfortunately, in the early period after catheter‐based PFO closure, palpitations are reported by about 10% of the patients. Heart rhythm disturbances should be considered as potentially life‐threatening for a technical diver; thus, we decided to perform underwater Holter (ECG) monitoring. No abnormalities in the heart rhythm were recorded. What was interesting was that we did not observe reduction in heart rate. We hypothesize that the submersion reflex was compensated by physical exertion during diving. We are aware that even good quality ECG tracing obtained from one dive does not exclude arrhythmias as cause of the symptoms. However, the patient was reassured and performed 55 dives without negative symptoms. To the best of our knowledge, there is only one preliminary investigation demonstrating the utility of underwater Holter (ECG) monitoring (Bosco et al., 2014). Authors reported that underwater Holter monitoring could produce good quality tracings (Bosco et al., 2014).
In conclusion, the underwater Holter monitoring should be considered as a diagnostic option for scuba divers suspected of having arrhythmias.
Conflicts of Interest
No conflicts of interest.
Olędzki S, Wojtarowicz A, Płońska‐Gościniak E, Lewandowski M, Gorący J. Scuba diving, patent foramen ovale and heart rhythm disturbances: The role of underwater Holter monitoring—Case report. Ann Noninvasive Electrocardiol. 2017;22:e12450 10.1111/anec.12450
References
- Billinger, M. , Zbinden, R. , Mordasini, R. , Windecker, S. , Schwerzmann, M. , Meier, B. , … Seiler, C. (2011). Patent foramen ovale closure in recreational divers: Effect on decompression illness and ischaemic brain lesions during long‐term follow‐up. Heart, 97(23), 1932–1937. [DOI] [PubMed] [Google Scholar]
- Bosco, G. , De Marzi, E. , Michieli, P. , Omar, H. R. , Camporesi, E. M. , Padulo, J. , … Schiavon, M. (2014). 12‐lead Holter monitoring in diving and water sports: A preliminary investigation. Diving and Hyperbaric Medicine, 44(4), 202–207. [PubMed] [Google Scholar]
- Gaspardone, A. , Giardina, A. , Iamele, M. , Gioffrè, G. , Polzoni, M. , Lamberti, F. , … Lani, C . (2013). Effect of percutaneous closure of patent foramen ovale on post‐procedural arrhythmias. Journal of the American College of Cardiology, 62(25), 2449–2450. [DOI] [PubMed] [Google Scholar]
- Honěk, J. , Srámek, M. , Sefc, L. , Januška, J. , Fiedler, J. , Horváth, M. , … Veselka, J. (2014). Effect of catheter‐based patent foramen ovale closure on the occurrence of arterial bubbles in scuba divers. JACC: Cardiovascular Interventions, 7(4), 403–408. [DOI] [PubMed] [Google Scholar]
- Meier, B. (2005). Closure of patent foramen ovale: Technique, pitfalls, complications, and follow up. Heart, 91(4), 444–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearman, A. , Bugeja, L. , Nelson, M. , Szantho, G. V. , & Turner, M. (2015). An audit of persistent foramen ovale closure in 105 divers. Diving and Hyperbaric Medicine, 45(2), 94–97. [PubMed] [Google Scholar]
- Spies, C. , Khandelwal, A. , Timmermanns, I. , & Schräder, R. (2008). Incidence of atrial fibrillation following transcatheter closure of atrial septal defects in adults. American Journal of Cardiology, 102(7), 902–906. [DOI] [PubMed] [Google Scholar]


