Abstract
Atrial fibrillation (AF) is currently considered a risk factor for stroke. Depending on the severity of clinical factors (risk scores) a recommendation for full anticoagulation is made. Although AF is most certainly a risk factor for ischemic stroke, it is not necessarily the direct cause of it. The causality of association between AF and ischemic stroke is questioned by the reported lack of temporal relation between stroke events and AF paroxysms (or atrial high‐rate episodes detected by devices). In different studies, only 2% of patients had subclinical AF > 6 minutes in duration at the time of stroke or systemic embolism. Is it time to consider AF only one more factor of endothelial disarray rather than the main contributor to stroke? In this “opinion paper” we propose to consider not only clinical variables predicting AF/stroke but also electrocardiographic markers of atrial fibrosis, as we postulate this as a strong indicator of risk of AF/stroke. We ask if it is time to change the paradigm and to consider, in some special situations, to protect patients (preventing stroke) who have no evidence of AF.
1. Atrial Fibrillation and Stroke. The Role of Anticoagulation Therapy
Atrial fibrillation (AF) is frequently a progressive disease that starts as paroxysmal and later evolves into persistent and permanent forms (Jahangir et al., 2007). Its prevalence increases with age and the presence of associated risk factors. The Framingham study (Kannel, Abbott, Savage, & McNamara, 1982) showed that patients with permanent AF present higher mortality, six fold excess of strokes and three fold risk of congestive heart failure. Initially, treatment was directed to preventing the occurrence of AF by modifying risk factors such as diabetes, hypertension, and heart failure whenever possible (Benjamin et al., 1994). However, in the late 80s and early 90s, different studies consistently demonstrated that oral anticoagulation therapy decreased the risk of stroke in patients with AF by approximately 70%, at the expense of a small increase in the frequency of major bleeding (Atrial Fibrillation Investigators, 1994). Oral anticoagulation therapy was especially indicated in older patients with valvular heart disease, heart failure or ischemic heart disease. These AF risk factors are now part of the scores endorsed by scientific societies worldwide, including the most universally accepted, the CHA2DS2‐VASc (Kirchhof et al., 2016). Due to the associated risk of bleeding and unproven benefit, anticoagulation therapy is not indicated in young people with isolated AF, and should be used with caution in patients at high risk of bleeding (HAS‐BLED score ≥3).
2. Epidemiology of Atrial Fibrillation. Association with Embolic Stroke and Cognitive Impairment
The public health burden of AF is enormous, and expected to continue increasing in the future (Martínez‐Sellés, Massó‐van Roessel, et al., 2016). Currently, the prevalence of AF in the developed world is of 2% in the general population, with a clear age‐related increase, affecting about 5 million people in the United States, and a similar number in Europe (Svennberg et al., 2015; Kirchhof et al., 2016; Martínez‐Sellés, Massó‐van Roessel, et al., 2016). About 30% of strokes have an embolic origin (Atrial Fibrillation Investigators, 1994), and this rate also increases with age. The incidence of AF‐related ischemic stroke is about 0.2% per year in a population‐based cohort older than 65 years (Yiin et al., 2014). Around 5%–10% of patients that already presents AF have an embolic stroke in 2–3 years, 2% during the first year, and this rate that may even be >4% in patients with advanced age and structural heart disease (Atrial Fibrillation Investigators, 1994). Ischemic stroke associated to AF is nearly twice as likely to be fatal as non‐AF stroke and stroke may be the first manifestation of AF (Potpara & Lane, 2014). Therefore, diagnosing AF before the first stroke occurs is critical for reducing disability and mortality. However AF may be asymptomatic in up to 30%–40% of the patients (Healey et al., 2012; Potpara & Lane, 2014). Finally, AF has been also associated to cognitive impairment (Horstmann et al., 2014; Hui et al., 2015).
3. Atrial Fibrillation is not the Final Cause of Stroke. It is Just Another Risk Factor
The documentation of AF and the evaluation of its impact on prognosis relies on the methodology of AF screening. Implantable loop recorders allow for extended monitoring up to 3 years, increasing the detection of silent AF (Gladstone et al., 2014; Reiffel et al., 2014; Sanna et al., 2014). Detection of atrial high rate episodes by analyzing the information stored in pacemakers or implantable cardioverter defibrillators, allows more extended monitoring and further improve AF screening even though atrial high‐rate episodes represent only indirect indicators of AF (Gladstone et al., 2014; Sanna et al., 2014). However, although AF is most certainly a risk factor for ischemic stroke, it is not necessarily the direct cause of it. The causality of association between AF and ischemic stroke is questioned by the reported lack of temporal relation between stroke events and AF paroxysms or atrial high‐rate episodes detected by implantable loop recorders or devices (Hohnoloser et al., 2006; Glotzer et al., 2009; Benezet‐Mazuecos, Rubio, & Farré, 2014; Gladstone et al., 2014; Reiffel et al., 2014; Sanna et al., 2014). In different studies, only 2% of patients had subclinical AF >6 min in duration at the time of stroke or systemic embolism (Martin et al., 2015). Among the plausible explanations for this change of paradigm is the recently proposed concept of fibrotic atrial cardiomyopathy (Kottkamp, 2013; Hirsh, Copeland‐Halperin, & Halperin, 2015), according to which AF may result from an underlying progressive disease affecting atrial myocardium and resulting in replacement of myocardium with fibrosis and fat (Daccarett et al., 2011; Platonov, Mitrofanova, Orshanskaya, & Ho, 2011; Akoum et al., 2013; Kottkamp, 2013; Marrouche et al., 2014; Hirsh et al., 2015).
4. Advanced Interatrial Block as a Risk Marker of AF and Stroke
The idea that the easily available surface ECG could help to predict AF risk is attractive. The rationale for this emerges from the notion that the surface ECG is a good reflection of the anatomical substrate of AF that is atrial fibrosis (Kottkamp, 2013; Hirsh et al., 2015). The ECG is a simple and reliable technique to detect the presence of conduction delay in the atria (Bayés de Luna et al., 1985; Bayés de Luna, 2012; Conde, Baranchuk, & Bayés de Luna, 2015). Few years ago, a consensus document (Bayés de Luna et al., 2012) standardized the classification of interatrial blocks (IAB), facilitating its rapid identification as partial (P‐IAB) (P wave ≥120 ms) or advanced (A‐IAB) (P wave ≥120 ms plus biphasic (±) morphology in leads II, III, aVF) (Figure 1). The diagnosis of A‐IAB can be done by a quick look at ECG tracings, and provides us information regarding the possible risk of AF/stroke in the future. The presence of A‐IAB indicates a chain of events summarized in Figure 2 that include: (1) Delayed and abnormal left atrium activation with consequently abnormal contraction against a closed (closing) mitral valve (Goyal & Spodick, 2001), (2) Increased left atrium pressure, wall stress and dilation, (3) Damage to the endocardium and progressive atrial fibrosis (Kottkamp, 2013; Hirsh et al., 2015).
Figure 1.
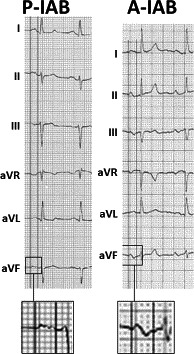
Examples of partial interatrial block (P‐IAB) (P wave duration ≥120 ms, positive in leads II, III, and aVF), and of advanced interatrial block (A‐IAB) (P wave duration ≥120 ms with plus/minus morphology in leads II, III, and aVF)
Figure 2.
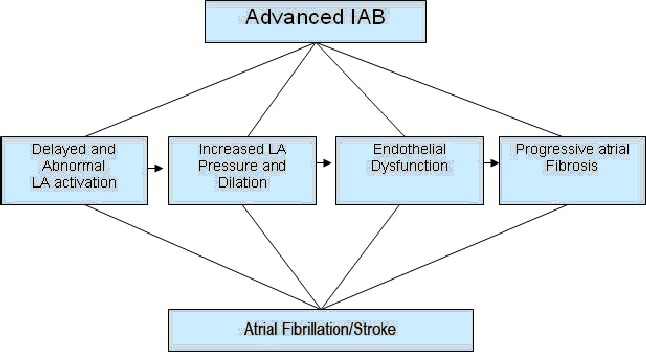
Physiopathological relation between advanced interatrial block (IAB) and atrial fibrillation
The association between the presence of interatrial block and the extent of atrial fibrosis has been confirmed in a detailed post mortem histology study. (Platonov et al., 2011) In clinical settings, the exact quantification of atrial fibrosis by imaging is more problematic, although pioneering studies that have used magnetic resonance imaging with gadolinium enhancement have shown promising results (Daccarett et al., 2011; Akoum et al., 2013). The presence of fibrotic atrial cardiomyopathy (Kottkamp, 2013; Hirsh et al., 2015) implies a stagnant and sluggish left atrium favouring the appearance of stasis‐induced thrombosis especially in the left atrial appendage. This may be, at least in part, the physiological rationale for the previously described association between IAB, AF and stroke.
Several studies have looked into the ability of IAB to predict AF. Bayés de Luna et al. (1988, 1999) published a few decades ago that 80% of patients with A‐IAB advanced heart disease and ambient arrhythmias, presented AF or atrial flutter after 3 years of follow‐up. CHA2DS2‐VASc score (≥3) and the P wave duration ≥160 ms were also presented in 80% of these patients. The association of A‐IAB with AF has been recently named Bayés Syndrome (Conde & Baranchuk, 2014a,b; Bacharova & Wagner, 2015).
It has also been reported that A‐IAB may predict AF in different clinical scenarios. P wave prolongation has shown strong association with incident AF in epidemiological studies such as Aric cohort (O'Neal, Zhang, Loehr, Chen, Alonso, & Soliman, 2016), Copenhagen cohort (Nielsen et al., 2015) and in patients with a CHA2DS2 (Wu et al., 2016b). ECG signs of abnormal atrial conduction were predictive of new onset AF in patients with advanced heart disease (Caldwell et al., 2014; Wu et al., 2016a). A‐IAB also predicts AF recurrence after pulmonary vein isolation (Agarwal, Aronow, Levy, & Spodick, 2003; Holmqvist et al., 2009; Holmqvist et al., 2010), and after atrial flutter ablation (Enriquez et al., 2015). In patients with atrial flutter ablation, recognizing A‐IAB could be a reason to consider extending the anticoagulation treatment to cover for possible AF episodes after the ablation of the cavotricuspid isthmus. A‐IAB has also identified patients at risk of developing AF after pharmacological cardioversion (Enriquez, Conde, Hopman, et al., 2014), and it remains to be investigated whether these patients should be considered for pulmonary vein isolation earlier. A‐IAB was found a predictor of new onset AF in a series of patients with severe heart failure receiving cardiac resynchronization (Sadiq Ali et al., 2015). In patients with advanced Chagas' disease A‐IAB was also able to predict new onset AF (Enriquez, Conde, Femenia, et al., 2014). Finally, a study performed in centenarians also concluded that IAB, particularly A‐IAB, is a pre‐AF condition associated with premature atrial beats (Martínez‐Sellés, Massó‐van Roessel, et al., 2016).
Interatrial blocks is also an independent risk factor for stroke and also cognitive impairment. Spodick's group was the first to publish this association in patients hospitalized (Ariyarajah, Puri, Apiyasawat, & Spodick, 2007). In a cohort of global population O'Neal, Kamel, Zhang, Chen, Alonso, & Soliman, (2016) recently confirmed the association of A‐IAB with incident ischemic stroke. Wu et al. (2016c) also found this association between IAB and stroke in patients with high CHA2DS2‐V score. Finally, Martínez‐Sellés, Massó‐van Roessel, et al., 2016 found that centenarians with IAB presented a higher prevalence of cognitive impairment and previous stroke than centenarians with normal P wave.
5. The Main Aim should be to reduce the Risk of Stroke
The present strategy to reduce the incidence of ischemic stroke is focused on the documentation of AF in those with high risk of stroke, especially in after ischemic stroke and no known AF. This approach demands development of cost‐efficient and minimally invasive ECG monitoring techniques as likelihood of AF detection is related to the duration of ECG monitoring, being the highest using implantable loop recorders, or availability of the on‐demand AF screening options such as thumb‐ECG recorded using hand‐held devices. The drawbacks of this approach are the associated costs and uncertainty in regard to the causal relationship between ischemic cerebral events and ultra‐short AF episodes, which appear to be common in patients with cardiovascular comorbidities (Gaita et al., 2013). A recent randomized study found no temporal relation between atrial tachyarrhythmias and stroke; and the strategy of early initiation and interruption of anticoagulation based on remotely detected atrial tachyarrhythmias did not prevent thromboembolic events (Martin et al., 2015).
However, we think our aim has to be to prevent embolic stroke. We propose a different strategy based on the findings of the strong association between the high CHA2DS2‐VASc score, the presence of ambient arrhythmias, and the risk of AF, which was repeatedly documented in the cohorts of ischemic stroke survivors, and in selected cohorts of patients evaluated for palpitations (Henriksson et al., 2011; Suzuki et al., 2013; Zuo et al., 2013; Acharya et al., 2015). It is therefore plausible to suggest that patients with high CHA2DS2‐VASc score may benefit from anticoagulation without need for documentation of AF. This approach is based on the earlier discussed value of IAB as an ECG‐based AF‐marker, and the well‐known association of the CHA2DS2‐VASc score association with both AF and ischemic stroke events. It is necessary to emphasize that the vast majority of patients with A‐IAB have at the same time a CHA2DS2‐VASc score ≥2 and therefore, if AF is documented, the patients would fulfil conventional indications for oral anticoagulation. Consequently, one could argue that given the association of A‐IAB with AF, there is a possibility that many strokes would be avoided if patients with high CHA2DS2‐VASc score and A‐IAB, were treated with anticoagulation regardless of the documented evidence of AF (Chhabra & Gowdar, 2016; Hughes & Worrall, 2016; Martínez‐Sellés, Fernández Lozano, Baranchuk, Bayes‐Genis, & Bayés de Luna, 2016). Of course, the possible benefits derived from this hypothesis; need to be counter balanced with the possible side effects of anticoagulation. Fortunately the incidence of cerebral haemorrhage as a consequence of treatment is low. The results of five randomized trials (Atrial Fibrillation Investigators, 1994) showed that it was 1% in the placebo arm, and 1.3% in patients under warfarin. The new oral anticoagulants are even associated with less risk of bleeding (Heidbuchel et al., 2016) and their benefits could be expanded to some patients with A‐IAB, even if they had no documented AF. Whether any of these approaches is superior to others is not known and can only be tested in a clinical trial. In order to advance knowledge in this topic, and International Registry (BAYES Registry) was launched on October 1, 2016 with a follow‐up estimated in 3 years (Martinez‐Selles, Baranchuk, Elousa, & Bayes de Luna, 2016). The beneficial efficacy and safety profile of the new oral anticoagulants together with insufficient efficacy of the current primary stroke prevention strategies indicate that the paradigm of having to document AF in order to start anticoagulation may need to be broken.
6. Conclusions
We suggest a new step in the prevention of ischemic stroke: to use anticoagulation therapy in sinus rhythm patients if they are at high risk of AF and stroke, even without documentation of AF. The subgroup of patients suitable for this approach may be represented by those with A‐IAB, structural heart disease, CHA2DS2‐VASc score ≥3, and frequent premature atrial contractions. Prospective validation of this approach in a controlled interventional study is ultimately needed; however, the expected benefits would be further reducing embolic stroke and/or cognitive impairment in high risk patients not fulfilling conventional indications for anticoagulation today. It remains to be seen whether this benefit may compensate for the well‐established side effects of anticoagulation, which should be tested in prospective studies.
Bayés de Luna A, Baranchuk A, Martinez‐Sellés M, and Platonov PG. Anticoagulation in patients at high risk of stroke without documented atrial fibrillation. Time for a paradigm shift?. Ann Noninvasive Electrocardiol. 2017;22:e12417. doi: 10.1111/anec.12417.
References
- Acharya, T. , Tringali, S. , Bhullar, M. , Nalbandyan, M. , Ilineni, V. K. , Carbajal, E. , & Deedwania, P. (2015). Frequent atrial premature complexes and their association with risk of atrial fibrillation. American Journal of Cardiology, 116, 1852–1857. [DOI] [PubMed] [Google Scholar]
- Agarwal, Y. K. , Aronow, W. S. , Levy, J. A. , & Spodick, D. H. (2003). Association of interatrial block with development of atrial fibrillation. American Journal of Cardiology, 9, 882. [DOI] [PubMed] [Google Scholar]
- Akoum, N. , Fernandez, G. , Wilson, B. , Mcgann, C. , Kholmovski, E. , & Marrouche, N. (2013). Association of atrial fibrosis quantified using LGE‐MRI with atrial appendage thrombus and spontaneous contrast on transesophageal echocardiography in patients with atrial fibrillation. Journal of Cardiovascular Electrophysiology, 24, 1104–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariyarajah, V. , Puri, P. , Apiyasawat, S. , & Spodick, D. H. (2007). Interatrial block: A novel risk factor for embolic stroke? Annals of Noninvasive Electrocardiology, 12, 15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atrial Fibrillation Investigators (1994). Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Archives of Internal Medicine, 154, 1449–1457. [PubMed] [Google Scholar]
- Bacharova, L. , & Wagner, G. S. (2015). The time for naming the interatrial block Syndrome: Bayes Syndrome. Journal of Electrocardiology, 48, 133–134. [DOI] [PubMed] [Google Scholar]
- Bayés de Luna, A. , Cladellas, M. , Oter, R. , Torner, P. , Guindo, J. , Martí, V. , … Iturralde, P. (1988). Interatrial conduction block and retrograde activation of the Left Atrium and paroxysmal supraventricular tachyarrhythmia. European Heart Journal, 9, 1112–1118. [DOI] [PubMed] [Google Scholar]
- Bayés de Luna, A. , Fort de Ribot, R. , Trilla, E. , Julia, J. , Garcia, J. , Sadurni, J. , … Sagues, F. (1985). Electrocardiographic and vectorcardiographic study of interatrial conduction disturbances with left atrial retrograde activation. Journal of Electrocardiology, 18, 1–13. [DOI] [PubMed] [Google Scholar]
- Bayés de Luna, A. , Guindo, J. , Viñolas, X. , Martinez‐Rubio, A. , Oter, R. , & Bayés‐Genís, A. (1999). Third‐degree inter‐atrial block and supraventricular tachyaarhythmias. Europace, 1, 43–46. [DOI] [PubMed] [Google Scholar]
- Bayés de Luna, A. , Platonov, P. , Cosio, F. G. , Cygankiewicz, I. , Pastore, C. , Baranowski, R. , … Spodick, D. (2012). Interatrial blocks. A separate entity from Left atrial enlargement: A consensus report. Journal of Electrocardiology, 45, 445–451. [DOI] [PubMed] [Google Scholar]
- Bayés deLuna, A. (2012). Clinical electrocardiography, 4th edn, Vol. 103. West Sussex, UK: Wiley‐Blackwell. [Google Scholar]
- Benezet‐Mazuecos, J. , Rubio, J. M. , & Farré, J. (2014). Atrial high rate episodes in patients with dual‐chamber cardiac implantable electronic devices: Unmasking silent atrial fibrillation. Pacing and Clinical Electrophysiology, 37, 1080–1086. [DOI] [PubMed] [Google Scholar]
- Benjamin, E. J. , Levy, D. , Vaziri, S. M. , D'Agostino, R. B. , Belanger, A. J. , & Wolf, P. A. (1994). Independent risk factors for atrial fibrillation in a population‐based cohort. Journal of the American Medical Association, 271, 840–844. [PubMed] [Google Scholar]
- Caldwell, J. , Koppikar, S. , Barake, W. , Redfearn, D. , Michael, K. , Simpson, C. , … Baranchuk, A. (2014). Prolonged P wave duration is associated with atrial fibrillation recurrence after successful pulmonary vein isolation for paroxysmal atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 39, 131–138. [DOI] [PubMed] [Google Scholar]
- Chhabra, L. , & Gowdar, S. (2016). Interatrial block to guide the thromboembolic prevention strategy: Should it be the next step? American Journal of Cardiology, pii, S0002–S9149 (16)30883‐9. doi: 10.1016/j.amjcard.2016.05.029 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Conde, D. , & Baranchuk, A. (2014a). Interatrial block as anatomical‐electrical substrate for supraventricular arrhythmias: Bayés syndrome. Archivos de Cardiología de México, 84, 32–40. [DOI] [PubMed] [Google Scholar]
- Conde, D. , & Baranchuk, A. (2014b). What a cardiologist must know about Bayés' Syndrome. Revista Argentina de Cardiología, 82, 220–222. [Google Scholar]
- Conde, D. , Baranchuk, A. & Bayés de Luna, A. (2015). Advanced interatrial block as a substrate of supraventricular tachyarrhythmias: A well recognized syndrome. Journal of Electrocardiology, 48, 135–140. [DOI] [PubMed] [Google Scholar]
- Daccarett, M. , Badger, T. J. , Akoum, N. , Burgon, N. S. , Mahnkopf, C. , Vergara, G. , … Marrouche, N. F. (2011). Association of left atrial fibrosis detected by delayed‐enhancement magnetic resonance imaging and the risk of stroke in patients with atrial fibrillation. Journal of the American College of Cardiology, 57(83), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enriquez, A. , Conde, D. , Femenia, F. , de Luna, A. B. , Ribeiro, A. , Muratore, C. , … Baranchuk, A. (2014). Relation of interatrial block to new‐onset atrial fibrillation in patients with Chagas cardiomyopathy and implantable cardioverter defibrillators. American Journal of Cardiology, 113, 1740–1743. [DOI] [PubMed] [Google Scholar]
- Enriquez, A. , Conde, D. , Hopman, W. , Mondragon, I. , Chiale, P. A. , de Luna, A. B. , & Baranchuk, A. (2014). Advanced interatrial block is associated with recurrence of atrial fibrillation post pharmacological cardioversion. Cardiovascular Therapeutics, 32, 52–56. [DOI] [PubMed] [Google Scholar]
- Enriquez, A. , Sarrias, A. , Villuendas, R. , Ali, F. S. , Conde, D. , Hopman, W. M. , … Baranchuk, A. (2015). New‐onset atrial fibrillation after cavotricuspid isthmus ablation: Identification of advanced interatrial block is key. Europace, 17, 1289–1293. [DOI] [PubMed] [Google Scholar]
- Gaita, F. , Corsinovi, L. , Anselmino, M. , Raimondo, C. , Pianelli, M. , Toso, E. , … Scaglione, M. (2013). Prevalence of silent cerebral ischemia in paroxysmal and persistent atrial fibrillation and correlation with cognitive function. Journal of the American College of Cardiology, 62, 1990–1997. [DOI] [PubMed] [Google Scholar]
- Gladstone, D. , Spring, M. , Dorian, P. , Panzov, V. , Thorpe, K. E. , Hall, J. , … EMBRACE Investigators and Coordinators . (2014). Atrial fibrillation in patients with cryptogenic stroke. New England Journal of Medicine, 370, 2467–2477. [DOI] [PubMed] [Google Scholar]
- Glotzer, T. V. , Daoud, E. G. , Wyse, D. G. , Singer, D. E. , Ezekowitz, M. D. , Hilker, C. , … Ziegler, P. D. (2009). The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: The TRENDS study. Circulation. Arrhythmia and Electrophysiology, 2, 474–480. [DOI] [PubMed] [Google Scholar]
- Goyal, S. , & Spodick, D. (2001). Electromechanical dysfunction of the left atrium associated with interatrial block. American Heart Journal, 142, 823–827. [DOI] [PubMed] [Google Scholar]
- Healey, J. S. , Connolly, S. J. , Gold, M. R. , Israel, C. W. , Van Gelder, I. C. , Capucci, A. , … ASSERT Investigators . (2012). Subclinical atrial fibrillation and the risk of stroke. New England Journal of Medicine, 366, 120–129. [DOI] [PubMed] [Google Scholar]
- Heidbuchel, H. , Verhamme, P. , Alings, M. , Antz, M. , Diener, H. C. , Hacke, W. , … Kirchhof, P. (2016). Updated European Heart Rhythm Association practical guide on the use of non‐vitamin‐K antagonist anticoagulants in patients with non‐valvular atrial fibrillation: Executive summary. European Heart Journal, pii, ehw058. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Henriksson, K. M. , Farahmand, B. , Asberg, S. , Terént, A. , & Edvardsson, N. (2011). First‐ever atrial fibrillation documented after hemorrahagic or ischemic stroke: The role of the CHADS(2) score at the time of stroke. Clinical Cardiology, 34, 309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh, B. J. , Copeland‐Halperin, R. S. , & Halperin, J. L. (2015). Fibrotic Atrial Cardiomyopathy, Atrial Fibrillation, and thromboembolism: Mechanistic Links and Clinical Inferences. Journal of the American College of Cardiology, 65, 2239–2251. [DOI] [PubMed] [Google Scholar]
- Hohnoloser, S. H. , Capucci, A. , Fain, E. , Gold, M. R. , van Gelder, I. C. , Healey, J. , … ASSERT Investigators and Committees . (2006). Asymptomatic atrial fibrillation and stroke evaluation in pacemaker patients and the atrial fibrillation reduction atrial pacing Trial (ASSERT). American Heart Journal, 152, 442–447. [DOI] [PubMed] [Google Scholar]
- Holmqvist, F. , Platonov, P. G. , Carlson, J. , Zareba, W. , Moss, J. ; MADIT II Investigators . (2009). Altered interatrial conduction detected in MADIT II patients bound to develop atrial fibrillation. Annals of Noninvasive Electrocardiology, 14, 268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmqvist, F. , Platonov, P. G. , McNitt, S. , Polonsky, S. , Carlson, J. , Zareba, W. , & Moss, A. J. ; MADIT II Investigators . (2010). Abnormal P‐wave morphology is a predictor of atrial fibrillation development and cardiac death in MADIT II patients. Annals of Noninvasive Electrocardiology, 15, 63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horstmann, S. , Rizos, T. , Rauch, G. , Fuchs, M. , Arden, C. , & Veltkamp, R. (2014). Atrial fibrillation and prestroke cognitive impairment in stroke. Journal of Neurology, 261, 546–553. [DOI] [PubMed] [Google Scholar]
- Hughes, T. M. , & Worrall, B. B. (2016). Acute interatrial block is a distinct risk factor for ischemic stroke. Neurology, 87, 344–345. [DOI] [PubMed] [Google Scholar]
- Hui, D. S. , Morley, J. , Mikolajczak, P. , Lee, R. (2015). Atrial fibrillation: A major risk factor for cognitive decline. American Heart Journal, 169, 448–456. [DOI] [PubMed] [Google Scholar]
- Jahangir, A. , Lee, V. , Friedman, P. A. , Trusty, J. M. , Hodge, D. O. , Kopecky, S. L. , … Gersh, B. J. (2007). Long‐term progression and outcomes with aging in patients with lone atrial fibrillation: A 30‐year follow‐up study. Circulation, 115, 3050–3056. [DOI] [PubMed] [Google Scholar]
- Kannel, W. B. , Abbott, R. D. , Savage, D. D. , & McNamara, P. M. (1982). Epidemiologic features of chronic atrial fibrillation. New England Journal of Medicine, 306, 1018–1022. [DOI] [PubMed] [Google Scholar]
- Kirchhof, P. , Benussi, S. , Kotecha, D. , Ahlsson, A. , Atar, D. , Casadei, B. , … Vardas, P. (2016). 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC)Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC Endorsed by the European Stroke Organisation (ESO). European Heart Journal, pii, ehw210. [Google Scholar]
- Kottkamp, H. (2013). Human atrial fibrillation substrate: Towards a specific fibrotic atrial cardiomyopathy. European Heart Journal, 34, 2731–2738. [DOI] [PubMed] [Google Scholar]
- Marrouche, N. F. , Wilber, D. , Hindricks, G. , Jais, P. , Akoum, N. , Marchlinski, F. , … Brachmann, J. (2014). Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation. The DECAAF study. Journal of the American Medical Association, 311, 498–506. [DOI] [PubMed] [Google Scholar]
- Martin, D. T. , Bershohn, M. M. , Waldo, A. L. , Wathen, M. S. , Choucair, W. K. , Lip, G. Y. , … IMPACT Investigators . (2015). Randomized trial of atrial arrhythmia monitoring to guide anticoagulation in patients with implanted defibrillator and cardiac resynchronization devices. European Heart Journal, 36, 1660–1668. [DOI] [PubMed] [Google Scholar]
- Martinez‐Selles, M. , Baranchuk, A. , Elousa, R. , & Bayes de Luna, A. (2016). Rationale and design of the BAYES (interatrial Block And Yearly EventS) Registry. Clinical Cardiology Nov 24 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez‐Sellés, M. , Fernández Lozano, I. , Baranchuk, A. , Bayes‐Genis, A. , & Bayés de Luna, A. (2016). Should we anticoagulate patients at high risk of atrial fibrillation? Revista Espanola de Cardiologia, 69, 374–376. [DOI] [PubMed] [Google Scholar]
- Martínez‐Sellés, M. , Massó‐van Roessel, A. , Álvarez‐García, J. , de García la Villa, B. , Cruz‐Jentoft, A. J. , Vidán, M. T. , … Investigators of the Cardiac and Clinical Characterization of Centenarians . (2016). Interatrial block and atrial arrhythmias in centenarians: Prevalence, associations, and clinical implications. Heart Rhythm: the Official Journal of the Heart Rhythm Society, 13, 645–651. [DOI] [PubMed] [Google Scholar]
- Nielsen, J. B. , Kühl, J. T. , Pietersen, A. , Graff, C. , Lind, B. , Struijk, J. J. , … Holst, A. G. (2015). P‐wave duration and the risk of atrial fibrillation: Results from the Copenhagen ECG Study. Heart Rhythm: the Official Journal of the Heart Rhythm Society, 12, 1887–1895. [DOI] [PubMed] [Google Scholar]
- O'Neal, W. T. , Kamel, H. , Zhang, Z. M. , Chen, L. Y. , Alonso, A. , & Soliman, E. Z. (2016). Advanced interatrial block and ischemic stroke: The Atherosclerosis Risk in Communities Study. Neurology, 87, 352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neal, W. T. , Zhang, Z. M. , Loehr, L. R. , Chen, L. Y. , Alonso, A. , & Soliman, E. Z. (2016). Electrocardiographic Advanced interatrial block and atrial fibrillation risk in the general population. American Journal of Cardiology, 117, 1755–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platonov, P. G. , Mitrofanova, L. B. , Orshanskaya, V. , & Ho, S. Y. (2011). Structural abnormalities in atrial walls are associated with presence and persistency of atrial fibrillation but not with age. Journal of the American College of Cardiology, 58, 2225–2232. [DOI] [PubMed] [Google Scholar]
- Potpara, T. S. , & Lane, D. A. (2014). Diving to the foot of an iceberg: The SEARCH for undiagnosed atrial fibrillation. Thrombosis and Haemostasis, 112, 1–3. [DOI] [PubMed] [Google Scholar]
- Reiffel, J. , Verma, A. , Halperin, J. L. , Gersh, B. , Tombul, S. , Carrithers, J. , … Kowey, P. (2014). Rationale and design of REVEAL AF: A prospective study of previously undiagnosed atrial fibrillation as documented by an insertable cardiac monitor in high‐risk patients. American Heart Journal, 167, 22–27. [DOI] [PubMed] [Google Scholar]
- Sadiq Ali, F. , Enriquez, A. , Conde, D. , Redfearn, D. , Michael, K. , Simpson, C. , … Baranchuk, A. (2015). Advanced interatrial block is a predictor of new onset atrial fibrillation in patients with severe heart failure and cardiac resynchronization therapy. Annals of Noninvasive Electrophysiology, 20, 586–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanna, T. , Diener, H. C. , Passman, R. , Di Lazzaro, V. , Bernstein, R. A. , Morillo, C. A. , … CRYSTAL AF Investigators . (2014). Cryptogenic stroke and underlying atrial fibrillation. New England Journal of Medicine, 370, 2478–2486. [DOI] [PubMed] [Google Scholar]
- Suzuki, S. , Sagara, K. , Otsuka, T. , Kano, H. , Matsuno, S. , Takai, H. , … Yamashita, T. (2013). Usefulness of frequent supraventricular extrasystoles and a high CHADS2 score to predict first‐time appearance of atrial fibrillation. American Journal of Cardiology, 111, 1602–1607. [DOI] [PubMed] [Google Scholar]
- Svennberg, E. , Engdahl, J. , Al‐Khalili, F. , Friberg, L. , Frykman, V. , & Rosenqvis, M. (2015). Mass screening for untreated atrial fibrillation: The STROKESTOP study. Circulation, 131, 2176–2184. [DOI] [PubMed] [Google Scholar]
- Wu, J. T. , Long, D. Y. , Dong, J. Z. , Wang, S. L. , Fan, X. W. , Yang, H. T. , … Yang, C. K. (2016a). Advanced interatrial block predicts clinical recurrence of atrial fibrillation after catheter ablation. Journal of Cardiology, 68, 352–356. [DOI] [PubMed] [Google Scholar]
- Wu, J. T. , Wang, S. L. , Chu, Y. J. , Long, D. Y. , Dong, J. Z. , Fan, X. W. , … Yang, C. K. (2016b). Usefulness of a combination of interatrial block and a high chads2 score to predict new onset atrial fibrillation. International Heart Journal, 57, 580–585. [DOI] [PubMed] [Google Scholar]
- Wu, J. T. , Wang, S. L. , Chu, Y. J. , Long, D. Y. , Dong, J. Z. , Fan, X. W. , … Qian, P. (2016c). CHADS2 and CHA2DS2‐VASc scores predict the risk of ischemic stroke outcome in patients with interatrial block without atrial fibrillation. Journal of Atherosclerosis and Thrombosis Jun 15 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yiin, G. S. , Howard, D. P. , Paul, N. L. , Li, L. , Luengo‐Fernandez, R. , Bull, L. M. , … Oxford Vascular Study . (2014). Age‐specific incidence, outcome, cost, and projected future burden of atrial fibrillation‐related embolic vascular events. Circulation, 130, 1236–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo, M. L. , Liu, S. , Chan, K. H. , Lau, K. K. , Chong, B. H. , Lam, K. F. , … Siu, C. W. (2013). The CHADS2 and CHA 2DS 2‐VASc scores predict new occurrence of atrial fibrillation and ischemic stroke. Journal of Interventional Cardiac Electrophysiology, 37, 47–54. [DOI] [PubMed] [Google Scholar]


