Abstract
Background: Hospital referral regions (HRRs) are often used to characterize inpatient referral patterns, but it is unknown how well these geographic regions are aligned with variation in Medicare-financed hospice care, which is largely provided at home.
Objective: Our objective was to characterize the variability in hospice use rates among elderly Medicare decedents by HRR and county.
Methods: Using 2014 Master Beneficiary File for decedents 65 and older from North and South Carolina, we applied Bayesian mixed models to quantify variation in hospice use rates explained by HRR fixed effects, county random effects, and residual error among Medicare decedents.
Results: We found HRRs and county indicators are significant predictors of hospice use in NC and SC; however, the relative variation within HRRs and associated residual variation is substantial. On average, HRR fixed effects explained more variation in hospice use rates than county indicators with a standard deviation (SD) of 10.0 versus 5.1 percentage points. The SD of the residual error is 5.7 percentage points. On average, variation within HRRs is about half the variation between regions (52%).
Conclusions: The magnitude of unexplained residual variation in hospice use for NC and SC suggests that novel, end-of-life-specific service areas should be developed and tested to better capture geographic differences and inform research, health systems, and policy.
Keywords: Bayesian statistics, health care cost, hospice, Medicare, practice variation
Introduction
Delivery of end-of-life (EOL) health care services through the Medicare hospice benefit has increased substantially in the United States, with Medicare hospice expenditures increased from ∼$3 billion in 2000 to nearly $16 billion in 2015.1 Palliative care services, including use of the Medicare hospice benefit, have the potential to improve the quality of EOL care at reduced cost.2–7 Researchers and policy makers need relevant geographic markets to measure competition and to characterize capacity for these services.1 The Dartmouth Atlas Hospital Referral Regions (HRRs) often are the best available approximation for health care markets, and are frequently used to provide denominators in the evaluation of all types of health services' cost and use. However, HRRs were developed for health system planning of specialized inpatient services and may not accurately reflect EOL care markets.
The patient population and care setting data used to define the HRR unit differs from the patient population and care settings that typically characterize EOL care. Approximately 20 years ago, the Dartmouth Atlas of Health Care used referral patterns for acute care services to develop HRRs, with each unit containing at least one provider of major cardiovascular and neurosurgeries.8 Conversely, 97.2% of all Medicare-financed hospice care is provided in patients' homes.1 Additionally, older or more severely ill individuals are less likely than other patients to travel for medical treatment to remain close to caregivers and other familiar resources.9,10 HRRs are frequently used to demonstrate geographic variation in health care services such as inpatient admissions, post-acute, and EOL care.11–14 However, there is little evidence quantifying the amount of geographic variation in hospice death service ratio (DSR) captured by HRRs.
Many important research questions, for example understanding determinants of EOL disparities, require a geographic unit to define and compare availability of local health resources and other health system characteristics.15,16 Evidence to help researchers and policy makers determine their relative usefulness in the context of end-of-life care is lacking. The goal of this study is to characterize the geographic variation of hospice use among Medicare decedents between and within HRRs in North and South Carolina. We hypothesize that there is substantial variation in county hospice use rates after controlling for HRR. In other words, HRRs are too large to capture local market variation in hospice use.
Methods
This study used Medicare data from the 2014 Hospice Public Use File published by the Centers for Medicare and Medicaid Services (CMS) and the 100% Limited Dataset (i.e., the Master Beneficiary File) for North and South Carolina. County characteristics were obtained from the 2014 American Community Survey.17 HRRs were defined using the Dartmouth Atlas.8 The study cohort included Medicare beneficiaries age 65 and older who died in 2014.
Key measures
The primary outcome was county hospice use rate among decedents. Hospice use rate, also known as DSR, is calculated as the ratio of the number of Medicare beneficiaries who died in 2014 who used at least one day of hospice in 2014 to the total number of Medicare beneficiaries who died in 2014. Secondary measures of hospice use included expenditures among hospice users (Supplementary Appendix S1).
Patient demographic variables included age, race (black vs. Other), gender, and state of residence. Hospice-qualifying diagnoses were categorized into cancer, circulatory illness, respiratory illness, dementia, or other diagnosis. Patient data were aggregated by county and converted to percentages of all Medicare decedents. County characteristics included hospice supply as measured by the number of hospices and socioeconomic status as measured by percentage of population below the poverty line. Additional county covariates included the percentage of population over the age of 65 and a size indicator (more than 250 vs. 250 or fewer decedents in 2014) to account for larger sampling variability in small counties.
Because HRRs can cross county and state borders, we used a cross-walk between HRR and census block, and also census block and counties to assign counties to HRRs based on the proportion of the population within each county that falls within each HRR.18 In addition, the proportion of each county's population that falls within each HRR was determined through Census data by taking population counts by Census block and summing the total population in the overlap area of each county and HRR.
Statistical analysis
We used Bayesian mixed models to quantify the variation in county DSR explained by HRR fixed effects (between-HRR variation), county random effects (within-HRR variation), and residual error.19,20 We used a Bayesian model to reflect the uncertainty in estimates of variance rather than presenting a single estimate. In a Bayesian model, data are combined with uninformative priors and a likelihood function to generate a distribution of plausible estimates, which is called a posterior distribution. The Bayesian model naturally provides a distribution of likely values for the key parameter (in this case the county variation in DSR) that reflects the uncertainty in the data. The ratio of within-HRR variation to the between-HRR variation is presented to describe the relative variation in DSR not explained by HRRs. For each posterior draw, we calculated within variation as the weighted standard deviation (SD) of the estimated county effects within each HRR, and between variation as the SD of the HRR fixed effects.
We used a Bayesian estimation with Hamiltonian Markov chain Monte Carlo process to generate values from the posterior distribution.19,20 Uninformative independent normal priors and the intercept prior reflected a weak prior belief that the average DSR by county will be around 50%, approximating the national average, which was 48% in 2016.21 Parameter values that are frequently drawn indicate that those specific values come from a high probability area of the posterior distribution. All regression coefficients other than the intercept were assigned uninformative independent normal priors. As continuous covariates were mean centered, the intercept was instead assigned a normal prior with mean 50 and SD 20 to reflect a weak prior belief that the average DSR by county will be around 50%. The noise error SD σs for both large and small counties was assigned a uniform prior on the range (0–25).
To test for sensitivity to the choice of prior in estimating the county random effects, two different priors were used: (1) exponential distribution with mean 2, which places a higher probability on small values for the county effect variation, and (2) a uniform distribution on (0–10). Results were not significantly different in the sensitivity analysis, indicating the conclusions are not sensitive to the choice of priors (see Supplementary Table S2). The more conservative (estimation of the county effects will be closer to zero) exponential distribution is presented. Full regression parameters, sensitivity analyses, and model fit assessments are available in the Statistical Appendix in Supplementary Data. Results were consistent in a sensitivity analyses using Gamma generalized linear models with a log link. Analyses were performed using ArcGIS, STATA v14, and R.
Results
Among Medicare decedents in North and South Carolina, 42.9% utilized hospice for at least one day, with an average 77.9 days of use at a cost of 12,080 dollars per hospice user (Table 1). Within the study population, 43,737 decedents across 146 counties utilized hospice for at least one day before death. Decedents living in South Carolina had greater use of hospice than decedents living in North Carolina. Percentage of decedents with any hospice use was 2.5 percentage points higher in South Carolina than North Carolina (44.6 vs. 42.1, respectively). Hospice beneficiaries in South Carolina spent an average of 92.8 days in hospice as compared with 68.4 days in North Carolina. On average, South Carolina also has twice as many hospice providers per county as North Carolina (2.1 vs. 0.8), although many counties in South Carolina have no hospice provider.
Table 1.
Patient, County, and Hospice Use Characteristics among Medicare Decedents by State
| Total | North Carolina | South Carolina | |
|---|---|---|---|
| Hospice beneficiaries | 43,737 | 27,117 | 16,620 |
| Counties, N | 146 | 100 | 46 |
| HRRs, N | 14 | 9 | 5 |
| % or Mean (SD) | % or Mean (SD) | % or Mean (SD) | |
| Patient characteristics | |||
| Female | 59.3 | 59.3 | 59.4 |
| Black | 15.3 | 13.6 | 17.9 |
| Primary diagnosisa | |||
| Cancer | 27.3 | 29.5 | 23.8 |
| Circulatory disease | 32.4 | 31.6 | 33.6 |
| Mental disorder | 4.9 | 4.3 | 5.9 |
| Respiratory illness | 18.4 | 18.3 | 18.5 |
| Other | 25.5 | 24.6 | 26.8 |
| County characteristicsb | |||
| Poverty rate | 18.3 | 18.1 | 18.7 |
| Four-year college degree | 25.4 | 25.8 | 24.8 |
| Uninsured | 18.5 | 18.5 | 18.6 |
| Hospice providers | 1.2 (1.8) | 0.8 (0.7) | 2.1 (2.9) |
| Hospice use | |||
| Death service ratioc | 42.9 | 42.1 | 44.6 |
| Hospice paymenta (thousands, $) | 12.1 (14.5) | 10.9 (13.6) | 13.9 (15.6) |
| Hospice daysa | 77.9 (102.0) | 68.4 (95.2) | 92.8 (110.3) |
Values displayed are per beneficiary averages for patients who used at least one day of hospice in calendar year 2014.
Percentages displayed are beneficiary-weighted averages of county-level percentages.
Death Service Ratio is defined as the ratio of the number of decedents in 2014 who used at least one day of hospice to the total number of decedents in 2014.
HRRs, hospital referral regions; SD, standard deviation.
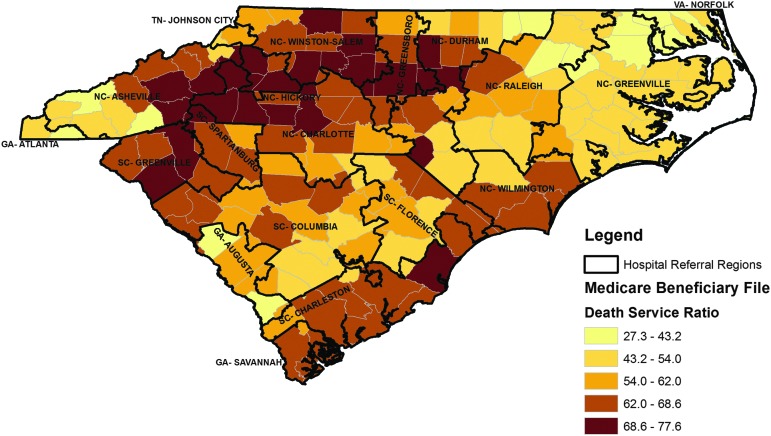
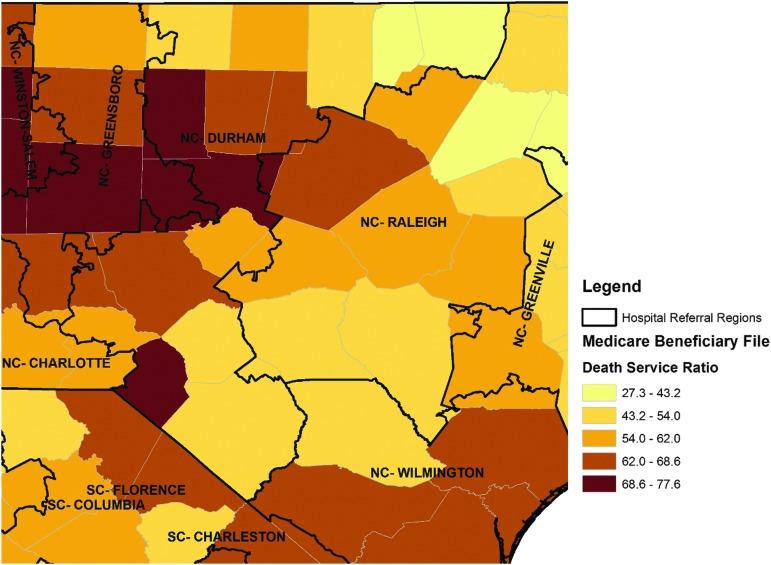
Location and size of the 14 HRRs are overlaid on counties in the map presented in Figure 1. North Carolina and South Carolina are divided into nine and five HRRs respectively. The shading represents the county level variation in the hospice DSR. Light yellow indicates the counties with the lowest rates of hospice use (i.e., <43.2), and the darkest orange indicates the counties with the highest rates of use (i.e., >68.6). Many HRRs have extreme variation in hospice use across counties. For example, counties within the Durham NC HRR have rates ranging from <43.2 near the Virginia border to >68.6 near the South Carolina border (Fig. 2).
FIG. 1.
Hospice death service ratio by county in North Carolina and South Carolina.
FIG. 2.
Hospice death service ratio by county in the Raleigh-Durham area.
To quantify the relative variation in DSR explained by HRR, we compared the mean SDs for the distributions of estimates for HRR, county, and residual error. The estimates of variation between HRR had a SD of 10 percentage points with a generally normal distribution (Supplementary Appendix S1). The estimates of county variation within HRR had a SD of 5.1 percentage points, about half that of the between variation. Finally, estimates of residual variation had a SD of 5.7, indicating that substantial residual variation is not explained by HRR or county indicators.
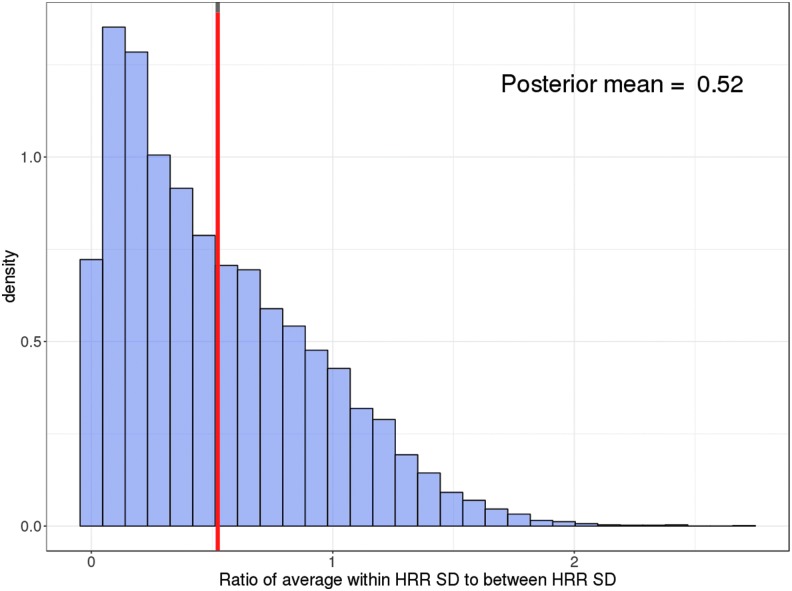
The relative variation is the ratio of within-HRR variation to the between-HRR variation. On average, the relative variation is 0.52, which means that the variation in hospice use within HRR is about 52% of the variation between HRR (Fig. 3). In other words, HRRs account for about twice as much variation in hospice use as do counties. Since the distribution of county SD does not follow a normal distribution (i.e., it is skewed), the measure of relative variation was also skewed (Supplementary Appendix S1). Across both States, HRRs consistently explained more variation than county (relative variation <1); however, the relative variation ranges from a high of 70% in Greenville, NC to a low of 26% in Hickory, NC (Table 2). The Durham, NC HRR shows substantial variation across included counties (Fig. 2), which is reflected in a relative variation of 63.4%. The relative variation within HRRs is reduced in regions with fewer counties, such as Hickory, and the relative variation was more substantial for HRRs that comprised a large number of counties, such as Durham, NC.
FIG. 3.
Histogram for the relative variation of hospice use within HRRs. For each posterior draw, we calculated within variation as the weighted SD of the estimated county effects within each HRR, and between variation as the SD of the HRR fixed effects. The relative variation is the ratio of within-HRR variation to the between-HRR variation. HRR, hospital referral region; SD, standard deviation.
Table 2.
Relative Variation Within-Hospital Referral Region versus Between-Hospital Referral Region
| HRR | Mean | 2.5% | Median | 97.5% |
|---|---|---|---|---|
| Atlanta, GAa | 0.156 | 0.004 | 0.109 | 0.558 |
| Augusta, GAa | 0.291 | 0.008 | 0.211 | 1.024 |
| Savannah, GAa | 0.190 | 0.005 | 0.135 | 0.656 |
| Asheville, NC | 0.643 | 0.015 | 0.427 | 2.466 |
| Charlotte, NC | 0.635 | 0.015 | 0.404 | 2.627 |
| Durham, NC | 0.634 | 0.015 | 0.417 | 2.528 |
| Greensboro, NC | 0.288 | 0.008 | 0.216 | 0.988 |
| Greenville, NC | 0.705 | 0.017 | 0.441 | 2.865 |
| Hickory, NC | 0.261 | 0.008 | 0.194 | 0.902 |
| Raleigh, NC | 0.562 | 0.013 | 0.367 | 2.258 |
| Wilmington, NC | 0.354 | 0.010 | 0.251 | 1.301 |
| Winston-Salem, NC | 0.537 | 0.013 | 0.359 | 2.157 |
| Charleston, SC | 0.428 | 0.011 | 0.288 | 1.653 |
| Columbia, SC | 0.687 | 0.016 | 0.430 | 2.785 |
| Florence, SC | 0.407 | 0.011 | 0.276 | 1.571 |
| Greenville, SC | 0.361 | 0.010 | 0.251 | 1.399 |
| Spartanburg, SC | 0.307 | 0.008 | 0.219 | 1.121 |
| Johnson City, TNa | 0.122 | 0.003 | 0.084 | 0.453 |
| Norfolk, VAa | 0.401 | 0.011 | 0.276 | 1.514 |
For each posterior draw, we calculated the weighted SD of the estimated county effects within each HRR, where the weights are the proportion of the county population within the HRR. The relative variation is the ratio of within-HRR variation to the between-HRR variation, and higher values indicate that county explains a greater amount of variation than lower values.
Data for HRRs extending into Georgia (3), Tennesee (1), and Virginia (1) are truncated at the borders of North and South Carolina.
HRR, hospital referral region.
Discussion
This study characterized the variation in hospice use, measured by the DSR, among Medicare decedents in North and South Carolina by HRR and county to better understand the value and limitations of commonly used market definitions in the context of end-of-life care. Both HRR and county indicators contribute significant explanatory power as predictors of DSR, and HRR generally explained more variation than county; however, substantial relative variation by counties within HRRs persists after controlling for observable patient and county characteristics. The magnitude of unexplained residual variation suggests that neither counties nor HRRs adequately capture geographic differences in DSR needed to inform research, health systems, and policy.
The variation in DSR we found between and within HRRs is consistent with existing evidence of substantial geographic variation in EOL care and costs across commonly used market areas, including HRRs, hospital service areas, core-based statistical areas, and physician practices.22,23 HRRs were created more than 20 years ago and there have been important changes in health care markets since then, chief among them, consolidation of hospital systems. Even the smaller components of HRRs, such as hospital service areas, do not account for differences between disease conditions and types of medical care, and more than half of primary care and specialist markets are smaller than these service areas.9,24 Our study confirms prior evidence that market areas vary across the types of health services, and specifically that hospice markets may be distinct from existing markets for nonhospice health services.
The county variation in DSR within HRRs suggests that markets for EOL care, including hospice, may be more local than other forms of care for which patients may be willing to travel greater distances. For specialty surgeries and certain conditions (e.g., cancer treatment), patients consider care options across the state or even country. Conversely, patients near the end of life may seek out and prioritize providers closer to home—including skilled nursing and other residential communities. These patients may prefer to be proximal to other resources, such as family, friends, and religious institutions. The majority of Americans live within 30 minutes of at least two in-home or stand-alone hospice facilities, and there is little evidence to suggest patients seek care beyond a one hour radius of home.25 Prior studies have reported the median distance between decedent's residence and hospice location was 9.8 miles.26 To provide home-based hospice services, hospice providers must limit their service area based on driving distance.27 In this context, our findings support the conclusion that HRR may be too large to capture local heterogeneity for end-of-life services.
The substantial residual variation we found in hospice use reflects the fact that HRRs and counties were developed with a focus on center-based networks of health care service providers, and not more distributed health care services such as hospice. HRRs are centered around hospitals that offer highly specialized cardiovascular and neurosurgery services that may not be needed by or recommended for patients at the end of life. Rather, care in the last six months of life is marked by multiple care transitions to and from the home, hospital, skilled nursing facilities, and home health or hospice agencies.14 Recognizing the limitations of the available geographic markers as applied to end-of-life care, prior studies have crafted study-specific hospice provider service areas. For example weighted average of the counties from which a hospice drew its patients or any county or counties where at least 20% of the hospice's patients resided.27–29 However, no geographic market area for measuring hospice outcomes has been validated or shown to be generalizable for defining denominators in EOL markets. Future research should develop and compare novel geographic methodologies and their application to health services at the end of life to inform local and national policy.
As alternative payment models proliferate, a methodology for defining home-based care markets, analogous to HRRs for acute care markets, may facilitate policies to improve access to palliative care and other home based services. In addition to identifying the economic drivers of variation in use and cost, defining markets is necessary to evaluate network adequacy within markets and compare quality of EOL care across markets. Alternative payment models aim to improve use of high-value services like hospice and palliative care among patients with advanced illness and set standards for high-quality care across the care continuum. Hospice and palliative care services are included in the package of services for which accountable care organizations are paid and held accountable. The adequacy of home health and palliative care provider networks available for patients with advanced illnesses may be a key facilitator for value-based programs to succeed in achieving the triple aim of improved outcomes and care at reduced cost.
Some data points were only available for the Carolinas, and this exploratory study in two states provides preliminary evidence that a national study may be warranted. Generalizability to other States is limited, particularly in regions where counties are much larger than in the Carolinas. Because our data were limited to North and South Carolina, information for HRRs that extend beyond these state borders was incomplete. Accordingly, our models may have underestimated the variation within HRRs extending outside of North and South Carolina due to fewer county observations, which would likely result in more conservative estimates of the relative variation. Hospice stays extending outside the calendar year are censored in these data, which may underestimate the length of hospice use; however, this censoring would only impact the estimates if correlated with county and HRR. We were unable to account for important individual-level characteristics associated with hospice use, including income, education, and occupation. Hospice use may also be impacted by the availability and characteristics of caregivers for beneficiaries, which we could not quantify.
Researchers and policymakers seeking to improve end-of-life care access, delivery, and payment models rely on existing market area definitions, including HRR and county, which have limited relevance in explaining variation in hospice use. While HRRs have significant explanatory power to predict rates of hospice enrollment, the relative variation within regions and residual variation is substantial. HRR and county markets fail to adequately capture the geographic variation in end-of-life care. Market areas developed for evaluation of acute health service use outcomes are likely not ideal for research and health systems planning related to end-of-life outcomes that include more distributed services such as hospice care. The development of health service areas specific to home-based hospice and palliative care may improve measurement of end-of-life outcomes and planning for regional end-of-life care systems.
Supplementary Material
Acknowledgments
Internally funded by the Duke-Margolis Center for Health Policy. N.A.B. was supported by the National Heart, Lung, and Blood Institute (NHLBI) grant K01HL140146. The contents of this publication are solely the responsibility of the authors and have not been approved by the Department of Health and Human Services or the CMS. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the National Institutes of Health.
Author Disclosure Statement
The authors have no conflicts of interest to disclose.
Supplementary Material
Supplementary Appendix Figure SA1
Supplementary Appendix Figure SA2
Supplementary Appendix Figure SA3
References
- 1. Medicare Payment Advisory Commission: March 2017 report to the Congress: Medicare payment policy. In: Chapter 12: Hospice Services, Vol. 2017 Washington, DC: Medicare Payment Advisory Commission, 2017;317–339 [Google Scholar]
- 2. Hogan C, Lunney J, Gabel J, Lynn J: Medicare beneficiaries' costs of care in the last year of life. Health Aff (Millwood) 2001;20:188–195 [DOI] [PubMed] [Google Scholar]
- 3. Shreyansh S, Moradiya Y, Murth S: Utilization of in-hospital palliative care for ischemic stroke deaths in United States (S45.005). Neurology 2014;82 [Google Scholar]
- 4. DiMartino LD, Weiner BJ, Hanson LC, et al. : Inpatient palliative care consultation and 30-day readmissions in oncology. J Palliat Med 2018;21:62–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Braun LT, Grady KL, Kutner JS, et al. : Palliative care and cardiovascular disease and stroke: A policy statement from the American Heart Association/American Stroke Association. Circulation 2016;11:e198–e225 [DOI] [PubMed] [Google Scholar]
- 6. Holloway RG, Ladwig S, Robb J, et al. : Palliative care consultations in hospitalized stroke patients. J Palliat Med 2010;13:407–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Burton CR, Payne S, Addington-Hall J, Jones A: The palliative care needs of acute stroke patients: A prospective study of hospital admissions. Age Ageing 2010;39:554–559 [DOI] [PubMed] [Google Scholar]
- 8. Wennberg JE, Cooper MA: The Quality of Medical Care in the United States: A Report on the Medicare Program. Chicago, IL: American Hospital Association, 1999 [PubMed] [Google Scholar]
- 9. Kilaru AS, Wiebe DJ, Karp DN, et al. : Do hospital service areas and hospital referral regions define discrete health care populations? Med Care 2015;53:510–516 [DOI] [PubMed] [Google Scholar]
- 10. Buntin MB, Garten AD, Paddock S, et al. : How much is postacute care use affected by its availability? Health Serv Res 2005;40:413–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Barnato AE, Mohan D, Lane RK, et al. : Advance care planning norms may contribute to hospital variation in end-of-life ICU use: A simulation study. Med Decis Making 2014;34:473–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barnato AE, Herndon MB, Anthony DL, et al. : Are regional variations in end-of-life care intensity explained by patient preferences?: A study of the US Medicare population. Med Care 2007;45:386–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Keating NL, Huskamp HA, Kouri E, et al. : Factors contributing to geographic variation in end-of-life expenditures for cancer patients. Health Aff (Millwood) 2018;37:1136–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Teno JM, Gozalo PL, Bynum JP, et al. : Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 2013;309:470–477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson KS, Kuchibhatla M, Payne R, Tulsky JA: Race and residence: Intercounty variation in black-white differences in hospice use. J Pain Symptom Manage 2013;46:681–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stiefel M, Feigenbaum P, Fisher ES: The Dartmouth atlas applied to Kaiser Permanente: Analysis of variation in care at the end of life. Perm J 2008;12:4–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Klemish D: American Community Survey. US Census Bureau, Suitland, Maryland, 2014 [Google Scholar]
- 18. Dartmouth Atlas of Health Care: Crosswalk Files—Dartmouth Atlas of Health Care. The Trustees of Dartmouth College. www.dartmouthatlas.org/crosswalk-files 2014. (Last accessed April19, 2019)
- 19. Hoff PD: A First Course in Bayesian Statistical Methods, 1st ed. New York, NY: Springer-Verlag, 2009 [Google Scholar]
- 20. Gelman A, Stern HS, Carlin JB, et al. : Bayesian Data Analysis, 3rd ed. Chapman and Hall/CRC, New York, 2013 [Google Scholar]
- 21. National Hospice and Palliative Care Organization. Facts and Figures: Hospice Care in America. www.nhpco.org/sites/default/files/public/Statistics_Research/2017_Facts_Figures.pdf 2016. (Last accessed July20, 2019)
- 22. Committee on Approaching Death: Addressing Key End of Life Issues, Institute of Medicine: Financing Care at the End of Life and the Implications of Potential Reforms. Washington, DC: National Academies Press (US), 2015 [Google Scholar]
- 23. Zhang Y, Baik SH, Fendrick AM, Baicker K: Comparing local and regional variation in health care spending. N Engl J Med 2012;367:1724–1731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kleiner S, Lyons S, White WD: Provider Concentration in Markets for Physician Services for Patients with Traditional Medicare. Health Manage Policy Innov 2012;1:15 [Google Scholar]
- 25. Carlson MD, Bradley EH, Du Q, Morrison RS: Geographic access to hospice in the United States. J Palliat Med 2010;13:1331–1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chapman KL, Jenkins TM, Harshbarger DS, Townsend JS: Hospice use among cancer decedents in Alabama, 2002–2005. Prev Chronic Dis 2009;6:A119. [PMC free article] [PubMed] [Google Scholar]
- 27. Johnson KS, Payne R, Kuchibhatla MN, Tulsky JA: Are hospice admission practices associated with hospice enrollment for older African Americans and Whites? J Pain Symptom Manage 2016;51:697–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Iwashyna TJ, Chang VW, Zhang JX, Christakis NA: The lack of effect of market structure on hospice use. Health Serv Res 2002;37:1531–1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carlson MD, Herrin J, Du Q, et al. : Hospice characteristics and the disenrollment of patients with cancer. Health Serv Res 2009;44:2004–2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.