Abstract
Background: The controversial effects promoted by cardiac resynchronization therapy (CRT) on the ventricular repolarization (VR) have motivated VR evaluation by body surface potential mapping (BSPM) in CRT patients.
Methods: Fifty‐two CRT patients, mean age 58.8 ± 12.3 years, 31 male, LVEF 27.5 ± 9.2, NYHA III‐IV heart failure with QRS181.5 ± 14.2 ms, underwent 87‐lead BSPM in sinus rhythm (BASELINE) and biventricular pacing (BIV). Measurements of mean and corrected QT intervals and dispersion, mean and corrected T peak end intervals and their dispersion, and JT intervals characterized global and regional (RV, Intermediate, and LV regions) ventricular repolarization response.
Results: Global QTm (P < 0.001) and QTcm (P < 0.05) were decreased in BIV; QTm was similar across regions in both modes (P = ns); QTcm values were lower in RV/LV than in Intermediate region in BASELINE and BIV (P < 0.001); only RV/Septum showed a significant difference (P < 0.01) in the BIV mode. QTD values both of BASELINE (P < 0.01) and BIV (P < 0.001) were greater in the Intermediate than in the LV region. CRT effect significantly reduced global/regional QTm and QTcm values. QTD was globally decreased in RV/LV (Intermediate: P = ns). BIV mode significantly reduced global T peak end mean and corrected intervals and their dispersion. JT values were not significant.
Conclusions: Ventricular repolarization parameters QTm, QTcm, and QTD global/regional values, as assessed by BSPM, were reduced in patients under CRT with severe HF and LBBB. Greater recovery impairment in the Intermediate region was detected by the smaller variation of its dispersion.
Keywords: ventricular repolarization; electrocardiography, body surface potential mapping; cardiac resynchronization therapy; ventricular dyssynchrony
INTRODUCTION
The natural progression of congestive heart failure (CHF) may determine remarkable deterioration in patients, with alterations of the cardiac electrical activity, which promote conduction system disorders and abnormal repolarization, 1 and reflect on the different depolarization times which occur across different regions of the myocardium. This results in cardiac interventricular and/or intraventricular dyssynchrony. It can be speculated that there may be dyssynchrony when the electrocardiogram (ECG) shows a widened QRS (>120 ms), particularly with a left bundle‐branch block (LBBB) morphology. The finding of a widened QRS in this setting clearly relates to a worsening of the function, increased cavity diameter, and higher mortality rates. 2 , 3 Bakker (1994) has reported favorable results with biventricular pacing in cases with remarkable dyssynchrony, thereby giving birth to the method known as cardiac resynchronization therapy (CRT). 4 This therapeutic modality has already been incorporated worldwide into the guidelines for treatment of severe HF, and is indicated for treating heart failure in functional classes III and IV of the New York Heart Association (NYHA), in sinus rhythm and LBBB as shown by a QRS duration > 120 ms on the ECG. 5 , 6 The electromechanical reverse remodeling induced by CRT reduces HF symptoms and hospitalizations, promotes enhanced tolerance to exercise and improves quality of life, decreasing mortality as well. 7 , 8 However, around one‐third of the patients do not respond to this therapy. To elucidate this fact investigators have been studying factors such as baseline QRS duration, 9 positioning of LV epicardial lead, 10 presence of areas of scarring at the location of electrode implantation, 11 and influence of the right ventricular (RV) function. 12 However, no consensus has yet to be reached.
Little is known about electrical heterogeneity of ventricular repolarization (VR) during CRT. Moreover, overall VR behavior and its behavior in certain regions of the heart are more likely to be important for a deeper understanding of their action upon the clinical evolution of these patients. However, this has not yet been clearly described. Thus, the analysis of intervals QT, JT, and T peak end on the electrocardiogram and respective dispersions, may be of great value. 13
These modifications which occur during ventricular repolarization of hearts undergoing CRT remain a controversial matter. According to some authors, cardiac repolarization deteriorates after CRT, leading to severe ventricular arrhythmias. 14 , 15 On the other hand, other authors have reported evidence of improved QT interval and QT dispersion values, in addition to a decrease in the incidence of arrhythmias. 16 , 17 , 18 Failure to characterize the ventricular repolarization process during CRT still causes much uncertainty. In this setting, the aim of our study was to evaluate the global and regional ventricular repolarization process in patients undergoing CRT, using a noninvasive method: the 87‐lead body surface potential mapping, in patients with severe heart failure in NYHA classes III/IV, sinus rhythm, and LBBB.
METHODS
Fifty‐two patients from the Clinic of Artificial Pacing of InCor‐HCFMUSP, mean age 58.8±12.3 years, 31 male (59.6%), with severe heart failure (functional classes III–88.5%, and IV–11.5%), all undergoing CRT with implantation of the left ventricle (LV) lead through the coronary sinus, participated in the study. Patients who had right bundle‐branch block, atrial fibrillation, NYHA functional classes I/II, previously implanted pacemakers or ICD, with hypertrophic cardiomyopathy, in use of amiodarone or with the LV lead implanted by thoracotomy were excluded. Etiologies of cardiomyopathy were: 25 dilated (48%), 11 ischemic (21.1%), 8 chagasic (15.4%), other (15.4%). ECG study was performed using an 87‐lead body surface potential mapping model 7100 Fukuda Denshi equipment (Fukuda Denshi Inc., Tokyo, Japan), with multiple‐electrode adhesive strips attached to the anterior chest (9 strips, 59 electrodes), and on the back (4 strips, 28 electrodes) (see Fig. 1). Electrode strips were placed on the thoracic surface longitudinally and in parallel, starting at the right mid‐axillary line (strip A), and proceeding in a sequence until the left midaxillary line (strip I); strips J to M were placed in a sequence on the back. All patients provided a written informed consent to take part in the study, which was approved by an Institutional Review Board.
Figure 1.
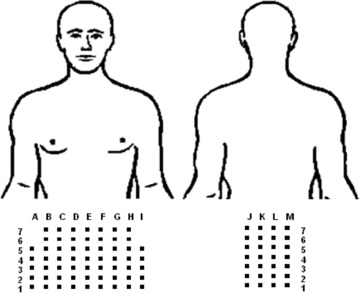
Distribution of the 87 BSPM leads on the anterior and posterior thoracic surface.
The study patients underwent BSPM examination in sinus rhythm with LBBB (BASELINE mode), and in biventricular pacing (BIV mode). Mean time from implantation of the resynchronization device and BSPM examination was 79 days (17–161) (this time span may have allowed for a reverse remodeling of the heart in some of the study patients). Recordings from the 87 BSPM electrodes were obtained both in BASELINE and BIV, with semiautomatic measurement of QRS duration, mean QT interval, measured from the onset of the QRS complex to the end of the T wave, QT correction for the heart rate using Bazett's formula (QTcm), and QT dispersion (QTD = QT max–QT min), as well as mean T peak–T end (Tp‐em) interval, measured from the peak of the T wave to its end, that is to the point where the T wave returned to the isoelectric line, and its correction by the heart rate (Tp‐ec), Tp‐e dispersion (Tp‐eD), and JT interval–this interval derived by subtracting the QRS duration from the QT interval. (see Fig. 2). 19 The latter two parameters, which are less dependent on ventricular depolarization, have been suggested to be useful in that they may better reflect the electrical heterogeneities of ventricular repolarization in this type of patient.
Figure 2.

Measurement of QRS. QT. Tpf and JT intervals on the BSPM.
It was possible to discriminate three different subsets of electrodes among the 87 BSPM leads, which corresponded to three specific regions. 20 Strips A to D related predominantly to the right ventricle (RV) region; strips E to H referred to the Intermediate region; and strips I to L, to the left ventricle (LV) region. Accordingly, the repolarization process was compared globally, and among the three delimited regions as well.
Continual variables are presented as mean±SD and 95% Confidence Interval (CI). Comparison of global values between the two pacing modes was made by paired Student t‐test; ANOVA compared values among the three regions. Values of P<0.05 were considered significant.
RESULTS
Table 1 summarizes the values obtained in the study. There was a global QRS reduction of 11% under BIV mode. Global QTm (P < 0.001), QTcm (P < 0.05), and QTD (P < 0.05) values were significantly reduced under BIV pacing as compared with BASELINE. The same occurred with regional values found in the three study regions: the RV region showing decreased values of QTm (P = 0.0014), QTcm (P = 0.016), and QTD (P = 0.04); there was also a significant decrease in values of QTm (P = 0.0001) and QTcm (P = 0.004) at the Intermediate region, while the QTm (P = 0.0018) and QTD (P = 0.023) values were significantly reduced at the LV region. Interestingly, these study regions display a characteristic ventricular repolarization behavior, with the Intermediate region showing a significantly delayed recovery time in BASELINE (QTcm: P < 0.0001 and QTD: P = 0.012), and in BIV mode as well (QTcm: P < 0.011 and QTD: P < 0.0009). Figure 3 shows the comparisons between BASELINE and BIV modes of global and regional mean QT intervals (QTm) and corrected QT values (QTcm), while Figure 4 compares the respective global and regional QT dispersion results.
Table 1.
Comparison of CRT Effect in Relation to BASELINE Mode (mean ± SD) on Global and Regional QTm, QTc m, and QTD
| BASELINE versus BIV | Δms | P | Δ% | ||
|---|---|---|---|---|---|
| HR(b/min) | 69.1 ± 10.8 | 71.2 ± 9.0 | ns | 2.9 | |
| QRS | 181.5 ± 24.2 | 161.7 ± 20.3 | 19.8 | <0.001 | −10.9 |
| QTm global | 455.8 ± 46.5 | 424.4 ± 38.7 | 31.4 | <0.001 | −6.9 |
| QTD global | 74.9 ± 28.7 | 61.2 ± 26.2 | 13.7 | <0.05 | −18.3 |
| QTc m global | 483.8 ± 41.4 | 460.7 ± 42.3 | 23.1 | <0.05 | −4.8 |
| QTm–RV | 451.2 ± 47.3 | 412.2 ± 70.4 | 39.0 | 0.0014 | −8.60 |
| QTc m–RV | 480.4 ± 42.1 | 441.1 ± 98.7 | 39.3 | 0.016 | −8.20 |
| QTD–RV | 48.6 ± 25.4 | 38.6 ± 24.8 | 10.0 | 0.04 | −20.60 |
| QT m– lnterm. | 466.7 ± 48.4 | 431.2 ± 38.5 | 35.5 | 0.0001 | −7.60 |
| QTc m–lnterm. | 497.2 ± 44.8 | 468.9 ± 42.8 | 28.3 | 0.004 | −5.70 |
| QTD–Interm. | 55.7 ± 28.7 | 47.1 ± 20.2 | 8.6 | ns | −15.50 |
| QTm–LV | 449.3 ± 48.0 | 422.9 ± 34.4 | 26.4 | 0.0018 | −5.80 |
| QTc m–LV | 478.5 ± 43.0 | 460.7 ± 41.7 | 17.8 | ns | −3.80 |
| QTD–LV | 40.5 ± 23.0 | 30.6 ± 20.4 | 9.9 | 0.023 | −24.30 |
Δms = variation in milliseconds; Δ% = percent variation of BIV effect; ns = not significant
Figure 3.
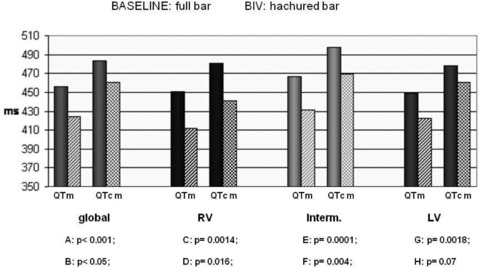
Global and regional QT interval – BASELINE versus BIV.
Figure 4.
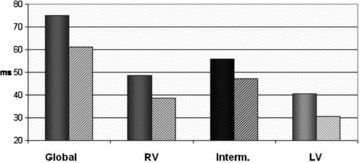
Global and regional QTD–BASELINE versus BIV.
Table 2 presents results of T peak end mean (Tp‐em), corrected (Tp‐ec m) and dispersion (Tp‐e D) values. BIV pacing significantly reduced all the values (Tp‐e m: P<0.001; Tp‐ec m: P<0.001, and Tp‐e D, P<0.01). JT intervals are also shown in Table 2 (JTm), with very modest and non‐significant reductions.
Table 2.
Comparison of CRT Effect in Relation to the BASELINE Mode (m ± SD) on Global Tp‐e m , Tp‐e c m, and Tp‐e D, and on Global and Regional JT m
| ms | BASAL × BIV | P | ↓Δ % | ↓Δ ms |
|---|---|---|---|---|
| Tp‐em | 107.4 ± 14.8 × 96.9 ± 139 | <0.001 | 9.8 | 10.5 |
| Tp‐ec m | 114.2 ± 15.9 × 105.6 ± 17.3 | <0.001 | 7.6 | 8.6 |
| Tp‐eD | 51.9 ± 16.6 × 45.2 ± 14.0 | <0.01 | 13.0 | 6.7 |
| Global JTm | 274.3 ± 46.9 × 262.7 ± 35.7 | ns | 4.3 | 11.6 |
| JTm RV | 269.6 ± 48.4 × 258.4 ± 36.2 | ns | 4.2 | 11.2 |
| JTm lnterm. | 285.2 ± 48.1 × 269.5 ± 35.7 | ns | 5.5 | 15.7 |
| JTm LV | 267.7 ± 47.2 × 261.2 ± 32.2 | ns | 2.5 | 6.7 |
↓Δms = variation in millisseconds; ↓Δ% = percent variation of BIV effect; ns = not significant
DISCUSSION
Cardiac resynchronization therapy has been used as an effective alternative approach to control symptoms of advanced heart failure, while at the same time decreasing mortality rates. When properly indicated, CRT would be expected to obtain good clinical responses for most patients. However, about 30% do not respond to the therapy. Ventricular repolarization, under this therapeutic modality, has shown controversial behavior, and no reports could be found in the literature showing its effect on mortality rates. In our methodology, acquisition of recordings was obtained using the body surface potential mapping (BSPM), given that its 87 electrodes capture the data comprising a broader thoracic surface, thus providing a richer data body for analysis. The system also enables the performance of global and regional evaluations, by defining regions of the heart and thereby characterizing the specific electrical activation and repolarization behavior in those regions. Local heterogeneities of the ventricular recovery process, related to a multipolar pattern, can better reflect a cardiac state vulnerable to arrhythmias. This type of pattern can only be detected on maps, not on standard ECG 21 .
From a global viewpoint, QTm fell within the range of normal values. On the other hand, QTc m values were abnormally high, which could be the result of these patient's hearts presenting severe cardiomyopathy associated with intraventricular conduction disorder (LBBB). Analysis of the regional QT intervals showed that the RV and LV regions had similar values (451.1 ± 47.3 ms and 449.3 ± 48.0 ms, respectively), while the Intermediate region had a value 3.7% greater (466.7 ± 48.4 ms) than the other regions. Statistically, this difference was not significant; however, analysis of the corrected values (QTc m) resulted in quite significant differences (480.4 ± 42.1 ms; 497.2 ± 44.8 ms, and 478.5 ± 43.0 ms–RV, Intermediate and LV regions, respectively, P < 0.0001), particularly at the Intermediate region. This could suggest that this region had an anomalous recovery in relation to that of the RV and LV. In the presence of LBBB, there is an impaired conduction of two‐thirds of the interventricular septum that correspond to the LV, so this portion of the Intermediate region suffers the greatest changes in its electrical activation. 22 In this electrical state, activation of the left ventricle is delayed due to the impaired transmission of impulses from one cell to another. However, it is at the Intermediate region that the greatest delays occur, as our results showed.
Global BASELINE DQT values were Somewhat low (74.9 ± 28.7 ms). Regionally, a significant difference was detected in the comparison of QTD values among the three regions (P = 0.012), with a greater difference between the Intermediate and LV regions, and practically normal values in the LV region (40.5 ± 23 ms). The highest QTD value was shown in the Intermediate region (55.7 ± 28.7 ms), which may indicate that this region exhibits the greatest repolarization heterogeneity.
Hina et al. 23 showed that when we find the highest QTDc values before implantation of the resynchronization device (mean 102 ± 26 ms), patients are more likely to have a good response to CRT compared to nonresponders (mean 40 ± 12 ms), over a 3‐month follow‐up period. This type of analysis was not done in our study; however, we believe that this is a very elegant approach, considering that with simple data such as QTD values obtained by a reliable recording method, Hina et al. were able to amass valuable information which can be used for prognosis and for further refining the indication for CRT.
Regional analysis showed that in this pacing mode QTc m values stayed within the normal range in all three regions, with the highest values found in the Intermediate and LV regions, suggesting that these regions may have more difficulty in recovery in relation to the RV region. Further, it must also be taken into account that the pacing of the Intermediate region by the ventricular electrodes is less pronounced. Additionally, QTD values approached the normal range, both globally and regionally, particularly in the LV region.
The variation promoted by CRT effect in BIV pacing mode, in relation to BASELINE (Δ%), determined a global reduction of QTm by 7% (P < 0.001), QTcm by 4.8% (P < 0.05), and DQT by 18.3% (P < 0.05). Yet, our findings of global Tp‐e m detected a similar behavior to that of the QT interval, i.e., CRT effect reduced all the values, whilst at the same time showing that the JT interval did not show any strong expression in this type of analysis. These findings are in agreement with those reported by Berger et al., who performed their analyses by similar methodology. 24 Regionally, QTm had significant reduction in the three regions (8.6%, P = 0.0014; 7.6%, P = 0.0001; and 5.8%, P = 0.0018, in the RV, Intermediate, and LV regions, respectively). QTcm was also reduced in the three regions (8.2%, P = 0.016; 5.7%, P = 0.004; and 3.8%, P = 0.07, in the RV, Intermediate, and LV regions, respectively). Such decreases were not significant in the LV region, although it showed the same trend. CRT promoted significant global, as well as RV and LV regional percent reductions of the cardiac ventricular repolarization dispersion. The Intermediate region again showed greater resistance to becoming more electrically homogeneous. Thus, we may infer that CRT promoted a more homogeneous ventricular repolarization from a global viewpoint, which was also higher in the ventricles than in the Intermediate region. In our study, CRT promoted greater uniformity of ventricular recovery in this selected study population, and these mechanisms are likely to act by attenuating any possible arrhythmias. Chalil et al. 26 clearly showed that greater QTcm reductions (median 5.0 ms) in patients after 48 days from CRT were not associated with major arrhythmic events. In the present study the mean reduction of this interval was even greater (23.1 ms), thus corroborating the findings of that study. There was also greater DQT values found in sinus rhythm (median 40 ms) not associated with arrhythmias either in the Chalil et al. study. Our study detected DQT values of 75 ms in sinus rhythm, with a 13.7 ms reduction (ΔDQT) under BIV effect. This strengthens our hypothesis that CRT is capable of reducing the arrhythmic risk.
In conclusion, during CRT, the ventricular repolarization parameters, which were evaluated herein using the body surface potential mapping method, showed significant global reduction of QTm and QTcm intervals, in addition to a QT dispersion decrease. Our results strongly suggest that regionally, under CRT, this population clearly had greater recovery impairment at the Intermediate region, which can be noted by a smaller variation of its dispersion.
CLINICAL IMPLICATIONS
This study aimed to analyze the particular aspect of ventricular repolarization behavior during CRT in a selected study population, and to thus create a more specific evaluation parameter which could refine the indication for a resynchronization device implantation. However, despite the employment of the BSPM, a specific, computerized tool, analysis of the ventricular repolarization is always subject to criticism, as well as many possible biases, given that no gold standard has yet to be established for such analysis.
The characteristics of our study results describe the cardiac electrical activity behavior, for which reason they should not be applied to clinical correlations. Nevertheless, based on the present data, it may be possible to extend them clinically, where they could be useful for a better selection of candidates for CRT, and even to establish better prognostic criteria associated with therapy response.
REFERENCES
- 1. Armoundas AA, Tomaselli GF. Electrical and structural remodeling of the ventricular myocardium in disease In Gussak I. et al (eds.): Contemporary Cardiology: Cardiac Repolarization: Bridging Basic and Clinical Science., Totowa NJ , Humana Press Inc, 2003, pp. 127–152. [Google Scholar]
- 2. Grines CL, Bashore TM, Boudoulas H, et al Functional abnormalities in isolated left bundle branch block. The effect of interventricular asynchrony. Circulation 1989;79:845–853. [DOI] [PubMed] [Google Scholar]
- 3. Baldasseroni S, Opasich C, Gorini M, et al Italian Network oncongestive heart failure investigators. Left bundle‐branch block is associated with increased 1‐year sudden and total mortality rate in 5517 outpatients with congestive heart failure: A report from the Italian network on congestive heart failure. Am Heart J 2002;143:398–405. [DOI] [PubMed] [Google Scholar]
- 4. Bakker PF, Meijburg H, Devries JW, et al Beneficial effects of biventricular pacing in congestive heart failure. PACE 1994;17:820 (abstract). [Google Scholar]
- 5. Bocchi EA, Marcondes‐Braga FG, Ayub‐Ferreira SM, et al III Diretriz Brasileira de Insuficiência Cardíaca Crônica. Arq Bras Cardiol 2009;93 :1–71. [PubMed] [Google Scholar]
- 6. Vardas PE, Auricchio A, Blanc JJ et al, European Society of Cardiology. European Heart Rhythm Association. Guidelines for cardiac pacing and cardiac resynchronization therapy. The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Europace 2007;9:959–998. [DOI] [PubMed] [Google Scholar]
- 7. Stellbrink C, Breithardt OA, Franke A, et al PATH‐CHF (PAcing THeraphies in Congestive Heart Failure) Investigators, CPI Guidant Congestive Heart Failure Research Group: Impact of cardiac resynchronization therapy using hemodynamically optimized pacing on left ventricular remodeling in patients with congestive heart failure and ventricular conduction disturbances. J Am Coll Cardiol 2001;38:1957–1965. [DOI] [PubMed] [Google Scholar]
- 8. Cleland JGF, Daubert J‐C, Erdmann E, et al For the Cardiac Resynchronization–Heart Failure (CARE‐HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352:1539–1549. [DOI] [PubMed] [Google Scholar]
- 9. Adelstein EC, Saba S. Usefulness of baseline electrocardiographic QRS complex pattern to predict response to cardiac resynchronization. Am J Cardiol 2009;103:238–242. [DOI] [PubMed] [Google Scholar]
- 10. Kronborg MB, Albertsen AE, Nielsen JC, et al Long‐term clinical outcome and left ventricular lead position in cardiac resynchronization therapy. Europace 2009; 11:1177–1182. [DOI] [PubMed] [Google Scholar]
- 11. Ypenburg C, Schalij MJ, Bleeker GB, et al Impact of viability and scar tissue on response to cardiac resynchronization therapy in ischaemic heart failure patients. Eur Heart J 2007;28:33–41. [DOI] [PubMed] [Google Scholar]
- 12. Burri H, Domenichini G, Sunthorn H, et al Right ventricular systolic function and cardiac resynchronization therapy. Europace. 2010;12:389–394. [DOI] [PubMed] [Google Scholar]
- 13. Santangelo L, Ammendola E, Russo V, et al Influence of biventricular pacing on myocardial dispersion of repolarization in dilated cardiomyopathy patients. Europace. 2006;8:502–505. [DOI] [PubMed] [Google Scholar]
- 14. Medina‐Ravell VA, Lankipalli RS, Yan GX, et al Effect of epicardial or biventricular pacing to prolong QT interval and increase transmural dispersion of repolarization. Does resynchronization theraphy pose a risk for patients predisposed to long QT or Torsade de Pointes? Circulation 2003;107:740–746. [DOI] [PubMed] [Google Scholar]
- 15. Fish JM, Brugada J, Antzelevitch C. Potential proarrhythmic effects of biventricular pacing. J Am Coll Cardiol 2005;46:2340–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Walker S, Levy T, Rex S, et al Usefulness of suppression of ventricular arrhythmia by biventricular pacing in severe congestive cardiac failure Am J Cardiol 2000;86:231–233. [DOI] [PubMed] [Google Scholar]
- 17. Zagrodzky JD, Ramaswamy K, Page RL, et al Biventricular pacing decreases inducibility of ventricular tachycardia in patients with ischemic cardiomyopathy. Am J Cardiol 2001;87:1208–1210. [DOI] [PubMed] [Google Scholar]
- 18. Harada M, Osaka T, Yokoyama E, et al Biventricular pacing has an advantage over left ventricular epicardial, pacing alone to minimize proarrhythmic perturbation of repolarization. J Cardiovasc Electrophysiol 2006;17:151–156. [DOI] [PubMed] [Google Scholar]
- 19. Pastore CA, Arcencio SR, Tobias NMMO, et al QT interval dispersion analysis in patients undergoing left partial ventriculectomy (Batista Operation). Annals Noninv Electrocardiol 2004;9:375–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pastore CA, Tobias NMMO, Samesima N, et al Body surface potential mapping investigating the ventricular activation patterns in the cardiac resynchronization of patients with left bundle‐branch block and heart failure J Electrocardiology, 2006;39:93–102. [DOI] [PubMed] [Google Scholar]
- 21. De Ambroggi L, Corlan AD. Clinical Use of BSPM in Cardiac Arrhythmias. Anadolu Kardiyol Derg 2007;7:8–10. [PubMed] [Google Scholar]
- 22. Sanches PCR, Moffa PJ. Distúrbios da condução intraventricular [Intraventricular conduction disorders] In Moffa PJ e, Sanches PCR. (eds.): Eletrocardiograma normal e patológico. [Normal and Pathological ECG] . São Paulo , Brasil , Roca, 2001, pp. 381–394. [Google Scholar]
- 23. Hina K, Kawamura H, Murakami T,et al Association of corrected QT dispersion with symptoms improvement in patients receiving cardiac resynchronization therapy. Heart Vessels 2008;23:325–333. [DOI] [PubMed] [Google Scholar]
- 24. Berger T, Hanser F, Hintringer F, et al Effect of cardiac resynchronization therapy on ventricular repolarization in patients with congestive heart failure. J Cardiovasc Electrophysiol 2005; 16:611–617. [DOI] [PubMed] [Google Scholar]
- 25. Chalil S, Yousef ZR, Muyhaldeen SA, et al Pacing‐induced increase in QT dispersion predicts sudden cardiac death following cardiac resynchronization therapy J Am Coll Cardiol 2006;47:2486–2492. [DOI] [PubMed] [Google Scholar]


