Abstract
Combined anterior and inferior ST elevation due to occlusion of wrapped left anterior descending artery (LAD) is well reported in the literature. However, there is rare literature mentioned about inferolateral ST elevation in this patient group. Herein, we report a case of acute proximal wrapped LAD occlusion with initial electrocardiographic sign of inferolateral ST elevation. The most likely mechanism of this electrocardiographic finding might be related to old anteroseptal myocardial infarction, combination with other coronary abnormality, such as chronic total occlusion of left circumflex artery that caused larger injury current in inferolateral than anteroseptal myocardium, and made anteroseptal leads reveal isoelectric pattern.
Ann Noninvasive Electrocardiol 2010;15(1):90–93
Keywords: inferolateral ST elevation, acute myocardial infarction, wrapped left anterior descending artery
The 12‐lead electrocardiogram (ECG) is essential for diagnosing ST elevation myocardial infarction (STEMI) and localizing the infarct‐related artery. However, it is sometimes difficult for physicians to correlate infarct‐related artery and electrocardiographic findings. We report a case of acute myocardial infarction (MI) with inferolateral ST elevation, but further ECG follow‐up and coronary angiography survey revealed left anterior descending artery (LAD) was the infarct‐related artery during this episode.
CASE REPORT
A 56‐year‐old male suffering from acute substernal chest pain for 2 hours had come to our Emergency Department for help. He is a Chinese herbal doctor and has a history of smoking, but denied any systemic disease such as hypertension, diabetes, and dyslipidemia before. Initial vital signs were pulse 81 beats/min and blood pressure 91/68 mmHg. ECG showed ST elevation over lead V4–V6 and lead II, III, aVF (Fig. 1A). Laboratory workup revealed: creatinine kinase MB(CK‐MB): 10 IU/L, troponin I: 0.25 ng/mL. Emergent percutaneous coronary intervention (PCI) was suggested under the impression of STEMI, however, the patient refused PCI due to personal reasons, therefore, we gave thrombolytic therapy as the alternative choice of reperfusion therapy. Interestingly, follow‐up ECG after thrombolytic therapy 2 hours later revealed all precordial leads with pathologic Q wave and serial ST‐T change despite resolution of inferolateral ST elevation, which highly suggested LAD was the culprit vessel (Fig. 1B). Further cardiac enzymes follow‐up also demonstrated early peak (CKMB: 501.2 IU/L, TnI: 469.89 ng/mL). The patient later agreed to coronary angiography survey under our detailed explanation. Coronary angiography showed LAD was a relatively long vessel that extended to the inferoapical wall (Fig. 2A) and proximal LAD (distal to diagonal 1 branch) had subtotal occlusion with thrombus formation (Fig. 2B). Distal left circumflex artery (LCX) with total occlusion was identified (Fig. 2A), which received Rentrop grade 3 collateral from dominant right coronary artery (Fig. 2C). Because LAD was favored as the infarct‐related artery, we performed angioplasty with stenting over LAD first and thrombolysis in myocardial infarction 3 flow was restored subsequently (Fig. 2D). Then we tried to perform PCI over total occlusion lesion of LCX. However, we had difficulty in penetrating it. After PCI and medication optimization, the patient was discharged under stable condition.
Figure 1.
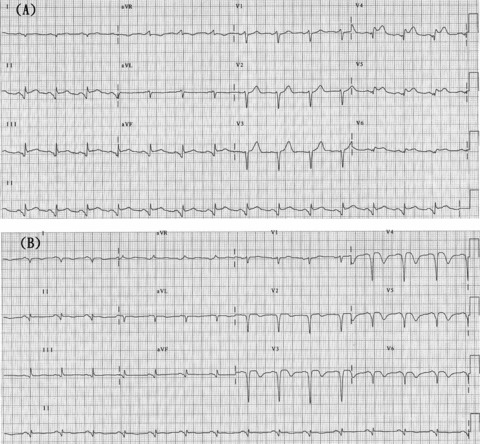
(A) Electrocardiogram revealed ST elevation over lead V4‐V6, lead II, III, and aVF. (B) Follow‐up electrocardiogram revealed resolution of inferolateral ST elevation, but all precordial leads had pathologic Q wave and serial ST‐T change.
Figure 2.
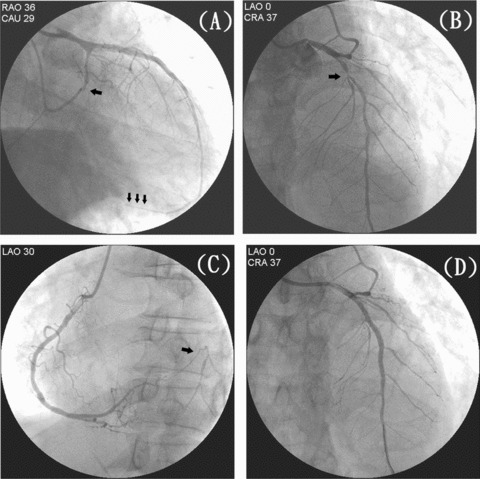
(A) Coronary angiography revealed left anterior descending artery (LAD) was a relatively long vessel, which extended to the inferoapical wall (small arrows), and distal left circumflex artery (LCX) with total occlusion (large arrow). (B) Proximal LAD subtotal occlusion with thrombus formation (arrow). (C) Right coronary artery gave Rentrop grade 3 collateral to distal total occlusion lesion of LCX (arrow). (D) Successful angioplasty with stenting over LAD and thrombolysis in myocardial infarction (TIMI) 3 flow was restored.
DISCUSSION
Twelve‐lead ECG is an important part of the diagnosis and initial evaluation of patients with chest pain. Based on the patterns of ST segment elevation, we could simply classify this as anterior, inferior (inferior‐posterior), or lateral MI. However, there are still some different electrocardiographic signs of ST‐segment elevation such as simultaneous anterior and inferior ST elevation. 1 , 2 , 3 This makes it difficult for physicians to evaluate which vessel is the true infarct‐related artery without angiography. Despite the present era of PCI, coronary angiography still sometimes cannot easily identify the true infarct‐related artery if more than one lesion is noted over different coronary arteries.
According to the previous literature, some researches have studied the cause and clinical significance of simultaneous anterior and inferior ST elevation in the cases of anterior MI. 1 , 2 , 3 Despite simultaneous anterior and inferior ST elevation, patients with this ECG finding often prove to have a relatively distal LAD lesion with limited infarction size and preserved left ventricular function. 1 There is a special term “Wrapped LAD,” which is defined as an LAD from a postreperfusion coronary angiogram that perfuses at least one‐fourth of the inferior wall of the left ventricle in the right anterior oblique projection. 4 However, this is still the normal anatomic pattern in most individuals.
Sasaki et al. reported that there are four ECG‐related conditions in cases with LAD occlusion according to the existence of a wrapped LAD. 4 If the patient has a wrapped LAD and the location of the occlusion is distal to the diagonal 1 branch, the ST segment is elevated in anterior and inferior leads simultaneously. In the other three conditions, ST segment in inferior leads is either isoelectric or depressive. Our case is more similar to the first condition because the patient had a wrapped LAD and a culprit lesion distal to diagonal 1 branch, which might be total occlusion before thrombolytic therapy. However, initial ST elevation was simultaneous over the inferior and lateral leads rather than the anterior and inferior leads. This electrocardiographic phenomenon was rarely reported in the literature in the cases with wrapped LAD occlusion. Duzenli et al. once described an isolated inferolateral STEMI due to acute occlusion of the distal LAD. 5 In their case, the occlusion site was over distal LAD and the explanation for inferolateral ST elevation is probably occlusion of the LAD just after supplying the anterolateral wall and that the LAD also supplies the inferoposterior region as an anatomical variation. However, in our case, the occlusion site was over relative proximal LAD. The most possible mechanism of inferolateral ST elevation might be as follows: First, old anteroseptal silent MI was suspected according to the initial electrocardiographic finding of poor R‐wave progression over V1–V3, which could lead to scar formation and shift the ST‐segment vector during this episode. Second, according to Bayés de Luna's research about the new electrocardiographic classification of Q‐wave MI based on correlations with magnetic resonance imaging, 6 old lateral infarction should be considered if Q (qr or r) waves in lead I, aVL, V5–V6 are found, which electrocardiographic findings were also noted in our case. In combination with the coronary angiographic findings of well collateral development to the total occlusion of LCX and serial ECG follow‐up showing pathologic Q waves in all precordial leads, LAD was favored as the acute culprit lesion during this episode. However, chronic total occlusion of LCX was also an important factor influencing the myocardial injury current and correlating with the electrocardiographic findings. Serial ST‐T changes were found in lead I, aVL, and V5–V6. In addition, initial small r wave in lead aVL also progressed to low voltage QS pattern under ECG follow‐up (Fig. 1). These electrocardiographic findings suggested that new lateral infarction also occurred during this episode, which was possibly related to the invisible collaterals from the occluded LAD and decreased coronary flow during acute MI. In this situation, inferolateral myocardium might suffer from more serious myocardial damage than anteroseptal myocardium if acute thrombosis of wrapped LAD occurs. This is why there was no obvious ST elevation over anteroseptal leads and it caused the electrocardiographic finding of simultaneous inferior and lateral ST elevation.
Acknowledgments
Acknowledgments: Financial support: None.
REFERENCES
- 1. Sadanandan S, Hochman JS, Kolodziej A, et al Clinical and angiographic characteristics of patients with combined anterior and inferior ST‐segment elevation on the initial electrocardiogram during acute myocardial infarction. Am Heart J 2003;146:653–661. [DOI] [PubMed] [Google Scholar]
- 2. Tamura A, Kataoka H, Nagase K, et al Clinical significance of inferior ST elevation during acute anterior myocardial infarction. Br Heart J 1995;74:611–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sapin PM, Musselman DR, Dehmer GJ, et al Implications of inferior ST‐segment elevation accompanying anterior wall acute myocardial infarction for the angiographic morphology of the left anterior descending coronary artery morphology and site of occlusion. Am J Cardiol 1992;69:860–865. [DOI] [PubMed] [Google Scholar]
- 4. Sasaki K, Yotsukura M, Sakata K, et al Relation of ST‐segment changes in inferior leads during anterior wall acute myocardial infarction to length and occlusion site of the left anterior descending coronary artery. Am J Cardiol 2001;87:1340–1345. [DOI] [PubMed] [Google Scholar]
- 5. Duzenli MA, Aygul N, Aydin MU, et al An unusual electrocardiographic presentation of acute obstruction of the left anterior descending coronary artery. J Electrocardiol 2008;41:107–109. [DOI] [PubMed] [Google Scholar]
- 6. Bayés de Luna A. New heart wall terminology and new electrocardiographic classification of Q‐wave myocardial infarction based on correlations with magnetic resonance imaging. Rev Esp Cardiol 2007;60:683–689. [PubMed] [Google Scholar]


