The location of the injured zone during acute myocardial infarction (AMI) is identified by evaluating ECG changes in different leads especially ST elevation and the appareance of Q waves. The value of ECG is based on pathological correlations performed more than 50 years ago by Myers in patients who died from AMI. 1 During the last decades these correlations, especially the number of leads with Q wave, were used to estimate the size of MI (myocardial infarction) and the prognosis of the patient. The ECG changes were and still are considered as a primary reflection of the injured myocardial zone. Although ECG changes might also give some information about the location of the obstruction in the culprit artery, the ability of ECG to precisely locate it was underappreciated. In the majority of textbooks on electrocardiography, there is no mention on how the alteration of ST in the acute phase, “ups and downs,” may help to diagnose the place of occlusion and the anatomic characteristics of an occluded artery. 2 , 3 , 4 Only in the last few years the possibility to perform a coronary angiography in the very early phase of an acute coronary syndrome (ACS) with ST elevation, has given the opportunity to know much better, through analysis of ST elevations and depressions in different leads, which coronary artery and at what level is occluded. 5 , 6 Furthermore, with modern imaging techniques we may not only detect perfusion defects with nuclear studies (SPECT), 7 but also the injured and necrotic zones with magnetic resonance (MR) with gadolinium injection. 8 We wish to stress that information about the culprit artery and the location of the occlusion is not only of academic interest to improve diagnosis, but it also helps to take decisions regarding the need for urgent PTCA.
However, in spite of the lack of information during decades about the importance of ST elevations and depressions to identify the culprit artery and the location of coronary obstruction, already in the forties, Sir Thomas Lewis made some comments about the importance of this correlation. In his last book on ECG 9 published in 1949 he stated: “In the common type of coronary thrombosis (Fig. 1) and this is due to thrombosis of the descending branch of the left coronary artery and infarction of anterior and lower part of the ventricles the broad deflection is upwardly directed in lead I and downwardly directed in lead III. In the less common type and this is due to occlusion of the end of right coronary artery (RCA) and leads to infarction of posterior and upper parts of the ventricles, the deflection is downwardly directed in lead I and upwardly directed in lead III.” It is fascinating that with only three leads it was possible, more than 50 years ago, not only to make the diagnosis of anterolateral and inferoposterior MI but also to correlate it with the occluded artery. The aim of this article is to serve as guidelines for clinicians to help them to precisely identify culprit artery and the place of occlusion in evolving AMI with ST elevation.
Figure 1.
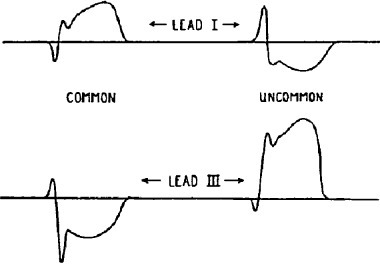
Predicting artery occlusion from ECG changes (taken from Lewis 9 ).
ECG—ANATOMIC CORRELATIONS IN AN ACUTE MI WITH ST ELEVATION
We will now describe how, thanks to the data obtained from the changes of ST, elevations, and depressions, we may not only recognize which walls are affected in course of AMI, but also and especially where is the place of occusion and what are the anatomical characteristics of the occluded culprit coronary artery responsible for AMI. It is important to remember that ST elevation is found in the leads that face the head of the injury vector, and that in the leads opposite ST depression may be recorded as a mirror image because these leads face the tail of this vector. 10
Various electrocardiographical criteria have been already described, based on these ST changes, to determine precisely the place of occlusion in a culprit artery. 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 20 In general all these criteria have high specificity (ranging from 70 to 100%) and the majority of them have also high sensitivity (up to 96%). Having in mind the most important criterion published 5 , 6 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 and considering also the most important data obtained from one of our unpublished preliminary study of 100 patients with an acute MI with ST elevation, we consider that to predict the culprit artery and the place of occlusion we should follow a systematic and sequential approach. This approach depends on the location of the most evident ST elevation—in precordial or inferior leads. We will now comment on the diagnostic approach in these two situations.
Evolving MI with the Most Evident ST Elevation in Precordial Leads
Dominant ST elevation in precordial leads indicates evolving MI of the anteroseptal wall with possible extension to the lateral and also inferior wall due to an occlusion in the LAD. 5 , 6 , 11 , 12 , 13 , 14 , 15 The analysis of ST in other leads will permit identifying the location of the occlusion. In a previous article (16) we discussed the anatomy of coronary arteries. Let me remind you now that the occlusion may be proximal to the first septal artery (S1) and first diagonal (D1) (20–45%), between S1 and D1 (30%), distal to S1 and D1 (10–30%), and if S1 originates after D1 may be distal to D1 but proximal to S1 (that happens in less than 10% of cases). The most important ECG changes allowing us to predict proximal or distal occlusion of LAD can be found looking first at the changes of ST in inferior leads, followed by detection of possible changes of ST in VR, V1, and V6. Once we have diagnosed that the occlusion is in LAD due to the presence of ST elevation in precordial leads we should look first at II, III, and aVF leads and also to VR, V1, and V6.
(a) ST depression in leads II, III, and VF indicates LAD occlusion proximal to D1 11 , 12 , 13 , 14 (Fig. 2A). The explanation for that is the following. If the occlusion is proximal to D1 the affected myocardium is very large and takes almost the entire anterolateral wall of the heart. If LAD wraps the apex, that happens most frequently, the injured zone extends to the apical part of inferoposterior wall of the heart. In these circumstances, the injury vector points not only to the front but also upward because the area of injured myocardium of anterolateral zone is much higher than the injured myocardium of the inferoposterior zone and consequently is recorded as ST elevation in precordial leads and ST depression in inferior leads (Fig. 2A). In our experience the sensitivity of this criterion is 73% while the specificity is 90%.
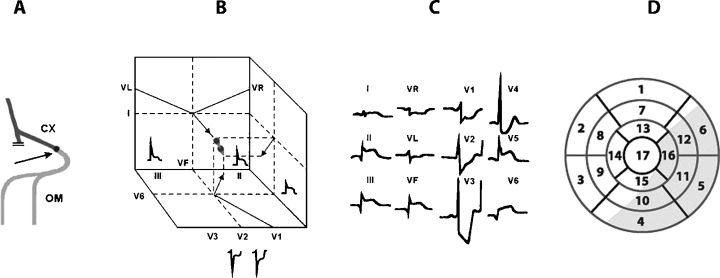
Figure 2.
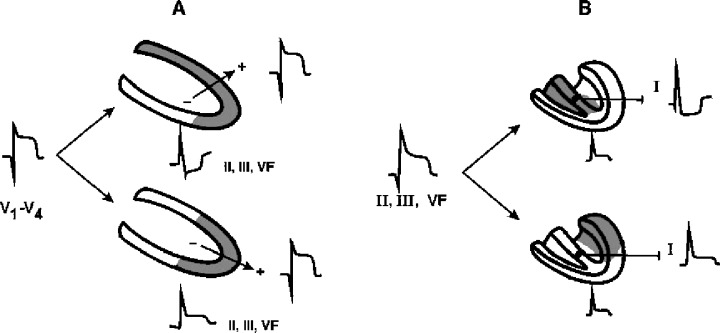
(A) Shows how in the case of ST elevation in precordial leads as a consequence of occlusion in LAD, the ST changes in reciprocal leads (II, III, VF) allow to identify whether the occlusion is in proximal (above) or distal LAD (below), and (B) shows how in the case of ST elevation in II, III, and VF the changes of ST in other leads (lead I) give us information on if the inferoposterior wall infarct is due to RCA (above) or LCX (below) occlusion.
If ST depression in II, III, and aVF is accompanied by ST elevation in VR and V1 and/or by ST depression in V6, occlusion of LAD is proximal not only to D1 but also to S1 (Fig. 3) because the head of the injury vector also faces the leads VR and V1 and the tail of the injury vector faces V6. ST depression in V6, independently of the presence of ST elevation in VR and/or V1, in patients already diagnosed with LAD occlusion proximal to D1 has in our experience a sensitivity of 91% and specificity of 61% for the diagnosis of LAD occlusion proximal not only to D1 but also to S1. When ST depression in II, III, and VF is not accompanied by ST depression in V6 and/or elevation of ST in VR or V1 it indicates that the occlusion is proximal to D1 but distal to S1 (Fig. 4).
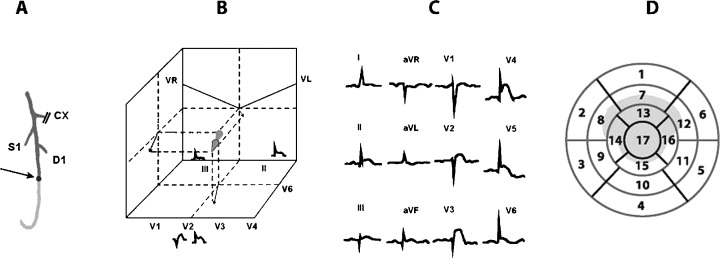
Figure 3.
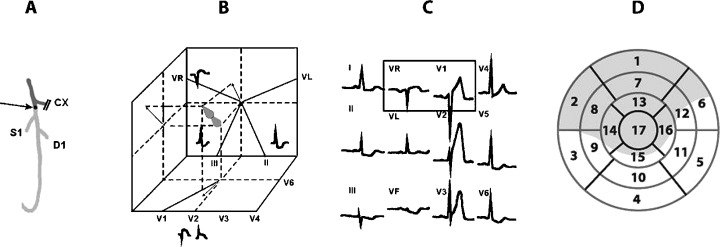
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D), in case of occlusion of LAD proximal to D1 and S1.
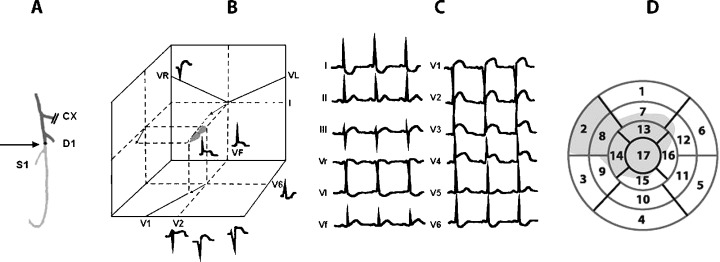
Figure 4.
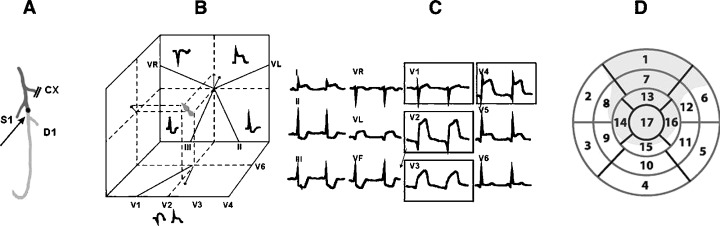
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D) in case of occlusion LAD proximal to D1 but distal to S1.
(b) ST elevated in II, III, and VF predicts LAD occlusion distal to D1 and S1 15 (Fig. 5). This is due to a fact that in these cases the affected anterolateral wall is not very large and if LAD wraps the apex, the injured part of inferior wall affected may be equal or even more important that the injured anterolateral wall. In these circumstances the injury vector points to the front (elevation of ST in precordial leads) but often a little below, that explains the usually small elevation of ST in II, III, and aVF (Fig. 2A). If LAD is not long and the occlusion is in the distal LAD the MI will be small and there will be not evident ST changes in inferior leads.
Figure 5.
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D) in case of occlusion LAD distal to S1 and D1.
When the ST elevation in II, III, and VF is accompanied by ST elevation in VR and often in V1 and/or by ST depression in V6 the occlusion is distal to D1 (ST elevation in II, III, and VF) but proximal to S1 (ST elevation in VR and/or V1 and/or ST depression in V5–V6) (Fig. 6).
Figure 6.
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D) in case of occlusion LAD distal to D1 but proximal to S1.
Evolving MI with the Most Evident ST Elevation in Inferior Leads
Dominant ST elevation in inferior leads indicates evolving MI of the inferoposterior zone with possible extension to lateral wall, due to occlusion in theRCA (70–80% of cases) or left circumflex artery (LCX) (30% of cases). 17 , 18 , 19 , 20 To know more details about which is the affected artery and its characteristics we have to do the following:
-
(a)
To check if right precordial leads have been recorded. These leads will be helpful to distinguish between a proximal RCA with right ventricle involvement (elevation of ST), RCA distal (positive T wave), or LCX (negative T wave). 6 , 11
-
(b)
In 12‐lead surface ECG we have to first check the ST segment in lead I. An ST depression in lead I indicates that RCA is much probably the culprit artery (the injury vector is directed not only downward (ST elevation in II, III, and VF), but also to the right and originates a ST depression in lead I) (Figs. 2B, 7, and 8). An ST elevation in lead I probably indicates that LCX is the affected artery because the lesion vector is directed leftward (Figs. 2B and 9). Only in cases of extremely dominant RCA or LCX we have found that this rule may fail.
-
(c)
In case of isoelectric ST in lead I we must check if ST elevation in lead II is equal or greater than ST elevation in lead III. In this case the affected artery is usually LCX (the injured vector is directed leftward) (Figs. 7 and 8) and if it is the contrary (ST elevation is greater in lead III than in lead II), although the most probably RCA is the culprit artery, there may exist some doubts. 19 (Fig. 9). To be sure we have to proceed to another step.
-
(d)
We need to check if ST depression in V1 divided by ST elevation in lead III is greater than 1 or lower than 1. 20 In the first case the most probable is that the affected artery is LCX (Fig. 9) with a great specificity (posterior forces are more important than inferior forces) because LCX irrigates more the posterior part of inferoposterior wall (segment 4 especially) that the inferior part (segments 10 and 15) that normally corresponds more to the RCA. 20 In the other cases (ratio of ST depression in V1 to ST elevation in III is equal or lower than 1) RCA is the culprit artery.
-
(e)
When we have ECG criteria of evident MI due to right coronary occlusion defined by depression of ST in I and ST elevation in III > II, the lack of ST depression in leads V1–V3 favours right ventricular involvement because the injury vector goes less backward (Fig. 7). Lack of ST depression in V1–V2 may also be seen in cases of small inferior MI in the absence of right ventricular involvement, but in these cases there is no evident ECG sign of major MI (the ascent of ST in inferior leads is small).
Figure 7.
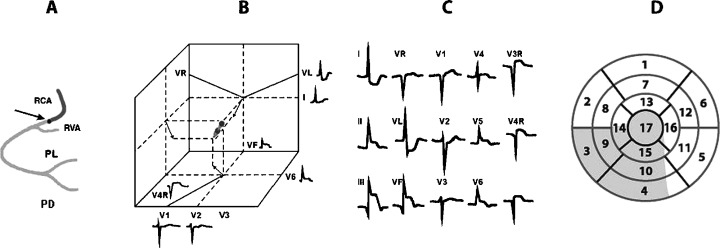
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D) in case of proximal occlusion of RCA, before the artery of the right ventricle.
Figure 8.
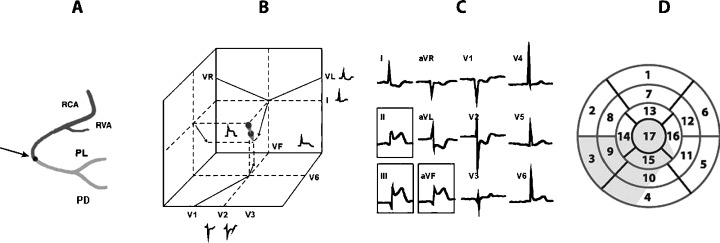
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D) in case of occlusion of RCA distal to the artery of right ventricle.
Figure 9.
The location of the occlusion (A), vectors of injury (B), ECG changes (C), and segments affected in eye bull view (D) in case of occlusion of Cx.
In Figures 10 and 11 we may see how to proceed to diagnose the culprit artery (RCA vs. LCX) in case of inferior MI with ST ascent in II, III, and VF, as well as how to predict the place of occlusion in LAD in case of MI with ST elevation in precordial leads. The algorithms presented in Figures 10 and 11 allow us to identify the culprit artery and/or the place of occlusion wit the accuracy of over 90%. 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20
Figure 10.
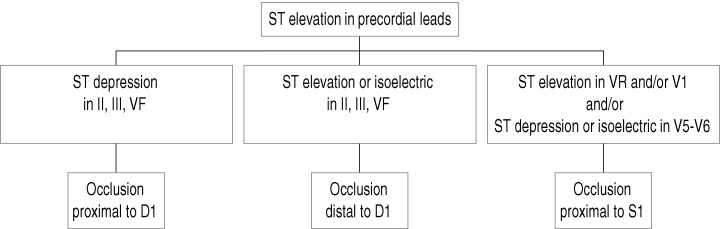
The algorithm to follow for prediction of the place of occlusion in LAD artery in case of evolving MI with ST elevation in precordial leads (see text).
Figure 11.
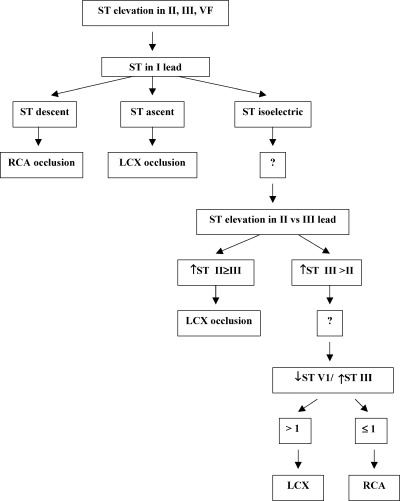
The algorithm to follow for prediction of the culprit artery (RCA vs. LCX) in case of evolving MI with ST elevation in inferior leads (see text).
CONCLUSIONS
-
1
There is a good correlation between ECG changes in the acute phase of a first MI with ST elevation and the affected myocardial zone and the location of the occluded artery.
-
2
Looking at the ECG leads that present the most prominent ST elevation and checking the reciprocal changes in other leads (ST elevations and depressions) we can predict with relatively high sensitivity and specificity which is the culprit artery, and the location of the coronary occlusion.
-
3
These careful ECG analyses are not only interesting to perform better diagnosis, but also to help in taking a decision to reccomend an urgent PTCA.
REFERENCES
- 1. Myers GB, Klein HA, Stofer BE. Correlation of electrocardiographic findings in anteroseptal infarction. Am Heart J 1948;36: 535–575. [DOI] [PubMed] [Google Scholar]
- 2. Startt Selvester RH, Wagner GS, Ideker RE. Myocardial infarction In McFarlane PW, Veitch Lawrie TD. (eds.): Comprehensive Electrocardiology. New York , Pergamon Press, 1989. [Google Scholar]
- 3. Chou T. Electrocardiography in Clinical Practice. New York , Grune&Stratton, 1979. [Google Scholar]
- 4. Wagner G. Marriott's Practical Electrocardiography. Philadelphia , Lippincott Williams and Wilkins, 2001. [Google Scholar]
- 5. Sclarowsky S. Electrocardiography of Acute Myocardial Ischaemia. London , Martin Dunitz , 1999. [Google Scholar]
- 6. Wellens TH. The ECG in the Acute Myocardial Infarction. Boston , Kluwer Academic Publishers, 2003. [Google Scholar]
- 7. Candell‐Riera J, Ortega‐Alcalde D (eds.). Nuclear Cardiology in Everyday Practice. Dordrecht , Kluwer Academic Publisher, 1994. [DOI] [PubMed] [Google Scholar]
- 8. Pons G. Atlas of MRI in Cardiology. Dordrecht , Kluwer Academic Publishers, 1999. [Google Scholar]
- 9. Lewis T. Clinical Electrocardiography and Heart Beat Disorders. London , Shaw Sons Limited Medical Publishers, 1949. [Google Scholar]
- 10. Bayes de Luna A. Clinical Electrocardiography: A textbook, 2nd Updated Edition Armonk , NY , Futura Publishers, 1998. [Google Scholar]
- 11. Engelen DJ, Gorgels AP, Cheriex EC, et al Value of electrocardiogram in localizing the occlusion site in the left anterior descending artery in acute anterior myocardial infarction. J Am Coll Cardiol 1999;34: 389–395. [DOI] [PubMed] [Google Scholar]
- 12. Birnbaum Y, Solodky A, Herz I, et al Implications of inferior ST segment depression in anterior acute myocardial infarction: Electrocardiographic and angiographic correlation. Am Heart J 1994;127: 1467–1473. [DOI] [PubMed] [Google Scholar]
- 13. Tamura A, Kataoka H, Mikuriya Y, et al Inferior ST segment depression as a useful marker for identifying proximal left anterior descending artery occlusion during acute anterior myocardial infarction. Eur Heart J 1995;16: 1795–1799. [DOI] [PubMed] [Google Scholar]
- 14. Kim TY, Alturk N, Shaikh N, et al An electrocardiographic algorithm for the prediction of the culprit lesion site in acute anterior myocardial infarction. Clin Cardiol 1999;22: 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sapin PM, Musselman DR, Dehmer GJ, et al Implications of inferior ST segment elevation accompanying anterior wall acute myocardial infarction for the angiographic morphology of the left anterior descending coronary artery morphology and site of occlusion. Am J Cardiol 1992;69: 860–865. [DOI] [PubMed] [Google Scholar]
- 16. Bayes de Luna A, Carreras F, Cygankiewicz I, et al Evolving myocardial infarction with ST elevation: anatomic considerations regarding the correlation between the site of occlusion and injured segments of the heart. Ann Noninvasive Electrocardiol 2004;9: 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bairey CN, Shah PK, Lew AS, et al Electrocardiographic differentiation of occlusion of the left circumflex versus the right coronary artery as a cause of inferior acute myocardial infarction. Am J Cardiol 1987;60: 456–459. [DOI] [PubMed] [Google Scholar]
- 18. Herz I, Assali A, Adler Y, et al New electrocardiographic criteria for predicting either the right or left circumflex artery as a culprit coronary artery in inferior wall acute myocardial infarction. Am J Cardiol 1997;80: 1343–1345. [DOI] [PubMed] [Google Scholar]
- 19. Saw J, Davies C, Fung A, et al Value of ST elevation in lead III greater than lead II in inferior wall acute myocardial infarction for predicting in‐hospital mortality and diagnosing right ventricular infarction. Am J Cardiol 2001;87: 448–450. [DOI] [PubMed] [Google Scholar]
- 20. Kosuge M, Kimura K, Ishigawa T, et al New electrocardiographic criteria for predicting the site of coronary artery occlusion in inferior wall acute myocardial infarction. Am J Cardiol 1998;82: 1318–1322. [DOI] [PubMed] [Google Scholar]


