Clinical exercise tests are used primarily for diagnosis of coronary insufficiency or appraisal of working capacity. Occasionally hemodynamic responses are observed during diagnostic catherization of the heart. Since interpretation of findings depends upon quantitative differences from normal values, variations due to age, sex, physical status and circumstances of the test need to be appreciated. To be effective, exercise stresses must involve large muscle masses, and the patient or subject must be ambulatory, cooperative and properly motivated. Some of the approaches to testing will be reviewed, and preliminary observations on a new technique will be presented.
The simplest test of exercise tolerance is for a physician to accompany a cardiac patient over one or more flights of stairs and to observe the symptoms. If this is not rewarding, increasing the work load by accelerating the pace or taking two steps at a time is more likely to be informative. But under these conditions the work loads are not well standardized, physiological responses are not usually monitored, and the physician is not necessarily of the same sex and comparable age.
Master's two step test is familiar to most internists; its value for diagnosis and prognosis of coronary insufficiency has been established. 1 , 2 An abnormal resting electro‐cardiogram is considered a contraindication for performance of this test. Although interpretation of results depends upon electrocardiographic changes, these have not been monitored routinely during exertion, even though a suitable technique was described 10 years ago. 3 The exercise stress varies with age, sex and body weight, but in terms of energy expenditure per unit of weight the underweight individual is stressed much more than the overweight person.
Wahlund appraised physical work capacity in physical units by determining the work load on a bicycle ergometer which was needed to increase the heart rate to 170 per minute. 4 Since oxygen consumption in cardiacs increased more slowly to the same or slightly higher levels as observed in normals at submaximal work loads, pulse rates were considered more appropriate indices of working capacity. Kjellberg et al. found a linear relationship with a high degree of correlation between this measurement of working capacity and total hemoglobin in men, women, and children. 5 Working capacity of normals in varying degrees of physical training, individuals with vasoregulatory asthenia, and cardiac patients were differentiated by this method. 6 Yet exercise studies of working men over 50 years of age revealed the maximal heart rate averaged only 160/minute when they were tested in a similar manner. 7 Furthermore, not all cardiacs can accelerate heart rate to 170/minute. Since many patients, in our experience, are not accustomed to bicycling, this form of exercise may be awkward, inefficient and quickly lead to fatigue of the muscles in the legs.
“Physical fitness” of air force personnel was tested by Balke and Ware who used progressively increased work loads (1% increment in grade every minute) while the subjects walked on a treadmill at 3.3 mph until heart rate reached 180/minute. 8 Since oxygen consumption could be predicted, its measurement was considered impractical. Only 18% of 500 men achieved “good” fitness, which was defined as 18 or more minutes of exercise, or maximal oxygen intake of at least 40 ml/Kg/minute. All others were nearly equally divided between “poor” and “fair” categories. Within this sample, fitness varied more with living habits than with age. As for clinical application, not all cardiacs are able to walk this fast, and it is doubtful that oxygen intake can be predicted under these circumstances when the rate of change is more delayed than in normal subjects.
Earlier studies by Bruce et al. described a work load of walking slowly at 1.7 mph and 10% grade on a treadmill to appraise exercise tolerance of cardiacs. 9 Although this stress was only moderate for normals and cardiacs with minimal impairment, it was indeed maximal for the severely impaired patients who could not continue exertion for as long as 10 minutes. Performance was expressed in terms of a “physical fitness index,” or ratio of the product of duration of exertion and average rate of oxygen removal to the sum of 3 recovery heart rates. This ratio represented a modification of the index previously described for evaluation of athletes by Johnson et al. 10 This index varied inversely with the alveolar arterial oxygen gradient during exercise and roughly correlated with clinical assessment of functional capacity in the majority of cardiac patients. 11 Patients in Class I or II functional capacity were not adequately differentiated from normal controls by this technique. Unpredictable results occurred in a minority of the tests where the apparent severity of symptoms and limitations for “ordinary” activities were either unknown, underestimated or exaggerated. With serial tests the optimal time for elective mitral commissurotomy was defined. 12 Experience over a period of years demonstrated an inverse relationship between the duration of exercise preoperatively and operative risk. When tolerance for this exertion fell below 4 minutes, operative mortality increased from nil to 26% as the more severely impaired cardiac patients were more vulnerable to any complication of the surgery or postoperative course.
The hazard of testing ambulatory cardiacs under these conditions and with the supervision of a physician has been quite minimal. Well over a thousand patients have been tested in the last ten years without evidence of serious consequences except in the following instances:
One young man with tight mitral stenosis and atrial fibrillation was retested during intensive treatment with quinidine for conversion to regular rhythm. He developed intractable pulmonary edema and died 2 days later.
Another patient with angina pectoris, who showed ST changes on exercise, developed ventricular fibrillation the following day when he was catheterized for angiographic studies. No contrast material was injected, and he responded to defibrillation once, but succumbed with a recurrence of the arrhythmia several hours later.
In the first fatality, quinidine therapy was an important contributory factor, since no pulmonary congestion occurred with previous testing of the same patient. The second patient survived the exercise test, but not the subsequent diagnostic studies.
This single stage test aided clinical evaluation of cardiac patients by providing an opportunity to observe symptoms and signs under physiologic conditions of moderate exertion in the upright posture. This extends the physical examination which is limited to observation of patients only at rest.
Hemodynamic studies in conjunction with diagnostic catheterization of the heart showed that 16 cardiac patients with little impairment of function increased cardiac output and stroke volume when observed during exercise with this single stage test. Ten others, who were similarly observed showed “exertional hypotension,” or a fall in arterial pressure from the resting level recorded in the upright posture. 13 Cardiac output at rest tended to be lower in these latter cases, and it showed smaller increments with exertion. Heart rate accelerated more, while stroke volume remained at the relatively low amount observed when these individuals were sitting at rest. Peripheral resistance diminished in both groups as vasodilatation occurred in the exercising muscles. Under these conditions mean systemic arterial pressure fell in the second group as cardiac output, and particularly stroke output, were insufficient. Depending upon the magnitude of the fall, such patients experienced marked fatigue, lightheadeness, or chest pain. Exertional hypotension was more commonly observed in patients with valvular stenosis, but it was also observed with other types of heart disease or just simply ventricular bigeminy during exercise.
Harris critically reviewed many tests of exercise tolerance and concluded that there was no suitable test of proven reliability. 14 Those which depend upon ventilatory measurements may be distorted by the anxious individual who, in the performance of an unfamiliar test, may alter his ventilatory response. Motivation for optimal or maximal performance may be suspect in cases where compensation is dependent upon results of the tests. Heart rates after exertion are not closely related to capacity, and maximal values during exertion diminish with age. Maximal heart rates and oxygen intakes cannot be predicted from submaximal responses. 7 , 15 The maximal oxygen intake, as noted earlier by Hill, Long and Lupton, 16 provides the ultimate measurement of the oxygen transport system. With increasing data on maximal oxygen intake in normals provided by Taylor et al. 17 the Åstrands 18 , 19 and Mitchell et al., 20 the need to determine this in cardiacs became increasingly obvious, yet traditionally tests involving maximal effort have been considered inappropriate for clinical purposes. Reconsideration of experience with the single stage exercise test clearly indicated the most reliable results were obtained in the most impaired cardiacs for whom this particular work load was maximal. Since they were tested with safety, the principle of stressing more strenuously the mildly impaired cardiacs who presented the greatest difficulty in appraising working capacity became justifiable. To do this effectively required appropriate studies on normals who have been tested in a similar manner.
On the basis of these considerations, a multistage treadmill test which required each individual, whether normal or cardiac, to attain a self‐determined point of maximal exertion has been investigated. Material for this study was obtained from normal subjects and patients from the Cardiology Clinic of the University Hospital and the Seattle Cardiac Work Evaluation Clinic, as well as students from the Department of Physical Education for Men.
MULTISTAGE EXERCISE CAPACITY TEST
The primary defect in the single stage treadmill test has been corrected by adding progressively greater work loads until each individual tested is exhausted by fatigue. If properly motivated, maximal performance then achieves the definition of capacity for exercise. The conditions and approximate rates of aerobic energy expenditure for young men are as follows:
| Stage | Speed mph | Grade % | Duration min | Oxygen Intake L/min |
|---|---|---|---|---|
| 1 | 1.7 | 10 | 3 | 1.1 |
| 2 | 3.4 | 14 | 3 | 2.2 |
| 3 | 5.0 | 18 | 3 | 3.0 |
| 4 | 6.0 | 22 | to exhaustion | 3.5 |
Although patients are not able to perform all stages, the same principle of at least one submaximal work load prior to maximal exertion applies to all but the most severly impaired. Subjects are asked to give a signal when they feel they cannot continue exertion for more than 1/2 minute at maximal exercise. Heart rate, rhythm and ST forces are monitored from a precordial lead electrocardiogram. A high velocity face mask and valve system and open circuit methods are used to collect expired air during the last minute, or 1/2 minute, of each exercise period. Ventilation and oxygen intakes are determined with a spirometer and Beckman Analyzer.
Circulatory transport of oxygen may be displayed graphically for analysis in 3 dimensional diagrams where the ordinate represents the oxygen pulse/Kg, and the right and left abscissa represent the heart rate and duration for each work load (Fig. 1). Since by substitution in the Fick equation, oxygen pulse represents the product of stroke volume and AV oxygen difference, and since stroke volume usually exhibits little change with short periods of exercise, this primarily reflects changes in AV oxygen difference. Combinations of such diagrams may be employed for each work load to display the sequential changes in these variables (Fig. 2). The volume of each block then represents the total oxygen intake for that work load; these may be summated to indicate the total aerobic energy expenditure for the entire test.
Figure 1.
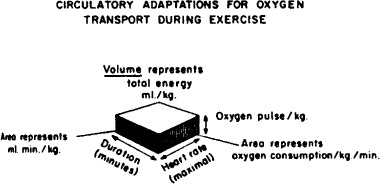
Diagrammatic representation of oxygen transport for any given work load of multistage exercise test. The product of oxygen pulse, heart rate and duration of exercise (in minutes) equals the estimated total oxygen intake for that period; this is represented by the volume of the block diagram.
Figure 2.
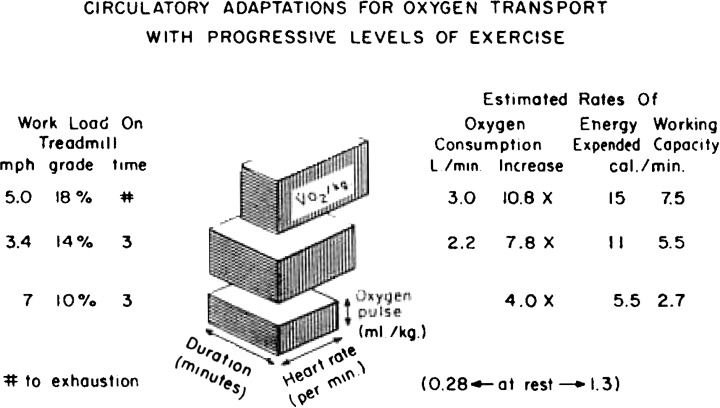
Representative changes in average heart rate, oxygen pulse/Kg and oxygen intake/Kg for the first 3 stages of the multistage test. Speed and grade of incline for the treadmill are shown on the left. To the right are the representative values of oxygen intake for young men, the corresponding energy expediture in calories and the predicted capacity for prolonged work in individuals capable of performing these work loads for testing of acute maximal effort. This is based upon Åstrand's concept that capacity for sustained work approaches 50% of the rate of energy expenditure for acute maximal exercise. 18
EXERCISE RESPONSES OF “NORMAL” SUBJECTS
Normal subjects have been selected on the basis of willingness to be tested and absence of symptoms or signs of cardiovascular disease. The question of “steady state” measurements at submaximal loads was examined by continuing exertion for 6 minutes and repeating the measurements in 10 subjects. The following results indicate no significant differences:
| Stage | 3rd Minute | 6th Minute | |
|---|---|---|---|
| Oxygen intake, ml/Kg | 1 | 11.6 ± 1.6 | 11.9 ± 2.0 |
| Oxygen intake, ml/Kg | 2 | 20.3 ± 2.2 | 20.7 ± 2.3 |
| Oxygen pulse, ml/Kg | 1 | .09 ± .02 | .10 ± .02 |
| Oxygen pulse, ml/Kg | 2 | .14 ± .02 | .14 ± .02 |
Reproducibility of measurements when retested several days later was evaluated in 17 subjects. Mean heart rates and oxygen intakes were virtually identical. Although duration of maximal effort increased about 20%, the change was not significant. Representative responses for normals for the first 3 stages of the multistage test are shown in Figure 2. None were studied in the basal state.
Data obtained from graduate students conducting a similar test on physically inactive boys indicates variations with age that suggest the possibility of deterioration in fitness during late adolescence (Fig. 3). 21 Differences in selection may be important also. Certainly, the effects of selection and vigorous physical training are conspicuous in young men.
Figure 3.
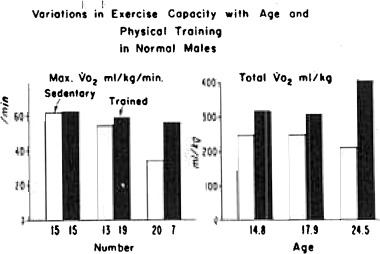
Comparison of maximal and total oxygen intakes/Kg in junior and senior high school boys and young men. Number of subjects tested is shown under the bars on the left, the average age of these groups is displayed under the bars on the right. (By permission of M. S. Huckle, Jr. and R. J. Staudacher.)
Changes in exercise capacity before and after a training course in swimming that was limited to only 2 periods of 25 minutes each week for 10 weeks were observed by Anderson (Fig. 4). 22 Not only did swimming skills and endurance improve, but 12 instead of 5 out of 24 were able to attain the 4th stage of exercise as a result of this training. Oxygen intake for the 3rd stage increased from 53 to 56 ml/Kg/min. Mean duration of total exercise increased 10% as total oxygen intake increased 14% from 296 to 339 ml/Kg (P < ·01).
Figure 4.
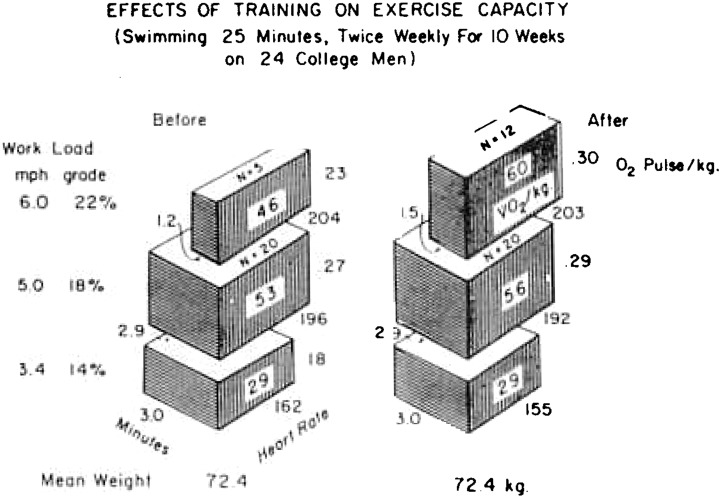
Analysis of changes in heart rate, oxygen transport and duration of exercise for each stage of multistage test in 24 college men who were studied before and after a training class in swimming. (By permission of T. D. Anderson.)
With respect to clinical testing of “normals,” 2 out of 85 were not motivated to continue even moderate exertion. Twenty per cent of the men, and none of the women reached the 4th stage, while one 16 year old girl, when highly motivated and retested, achieved the 4th stage. Sixty‐four per cent of the men and 46 per cent of the women reached the 3rd stage. One‐half of the men and one‐quarter of the women exhibited heart rates over 180/minute. Since in 15% heart rate did not exceed 150/minute, their motivation was suspect. Men and women under 36 years of age had twice the total oxygen intake of subjects who averaged 20 years older.
EXERCISE RESPONSES OF CARDIAC PATIENTS
There are two important prerequisites to the clinical application of this multistage exercise test to patients:
-
1
The patients tested should be ambulatory. Even normal subjects, when confined to bed for 3 weeks, exhibit cardiovascular deconditioning. Patients who are confined to bed and chair because of recent myocardial infarction, pulmonary embolism, uncontrolled ventricular tachycardia, marked congestive heart failure or acute myocarditis are not tested. A normal resting electrocardiogram, is not required. Many patients with angina pectoris, chest pain syndromes, ventricular “strain” patterns in the electrocardiogram, mild to moderate degrees of congestive heart failure, or arrhythmias such as atrial fibrillation, ventricular premature beats or complete heart block have been tested. Treatment with digitalis is not a contraindication, but it commonly causes abnormalities of ventricular repolarization. Quinidine or pronestyl in large doses may render testing hazardous because of exertional hypotension.
-
2
A properly informed physician should be in attendance to observe the patient for significant signs of hypoxic distress and to monitor the electrocardiogram. Indications for terminating the test are severe chest pain or dyspnea, faltering gait, or onset of paroxysmal ventricular tachycardia. A substantial fall in blood pressure is another hazardous sign. ST depression alone has not been a routine indication for stopping exertion. One hand is permitted to rest on the hand bar as a safety measure, but “leaning” on this support to diminish the load on the legs, is not permitted.
Following the test, each patient should be interviewed regarding symptoms and their intensity. A brief examination is made for cyanosis, jugular venous hypertension, basilar rales, or gallop rhythm as evidence of circulatory insufficiency. The ECG is monitored for at least 3 minutes. Nitroglycerine is permitted for relief of anginal pain.
Average responses in the first 45 male patients are shown in Figure 5. They had a variety of lesions, including healed myocardial infarction and valvular diseases, but they were grouped for the purposes of this study according to clinical estimates of functional capacity and compared with 14 apparently normal men. From 43% of the normals to 15, 8 and 0% of Class I, II, and III patients reached the 3rd stage. Indeed, some individuals in all 4 of these groups were unable to complete the second stage of exercise. Accordingly, the average duration of time for this work load fell from 2.9 minutes in the controls and Class I cardiacs to 2.2 and 1.2 minutes in patients in Classes II and III. Despite rather obvious differences in performance between these groups, it was not possible to demonstrate statistically significant intergroup differences with respect to either heart rate or oxygen intake. Yet the products of oxygen intake/Kg and duration of time, when summated for all work loads to represent the total oxygen intake for the entire test readily differentiated each group from the others (Fig. 6). Actually there was a ninefold difference in energy expenditure between younger men who were trained athletes and Class III cardiac patients.
Figure 5.
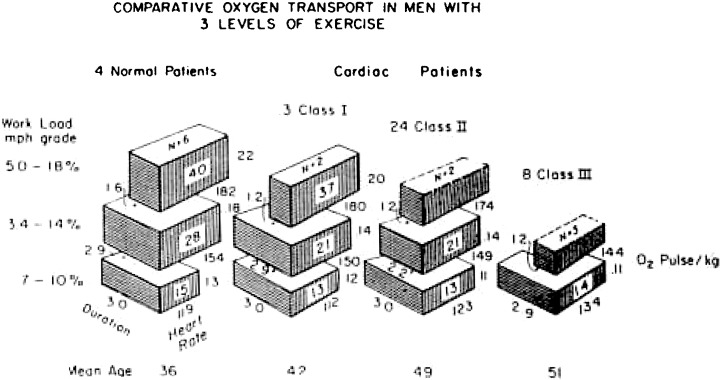
Analysis of average responses observed in patients with cardiovascular diseases grouped according to clinical appraisals of functional capacity and compared with ambulatory hospital patients with no evidence of cardio‐respiratory diseases. The number who were able to exercise at the highest work load is indicated for each group; duration of exertion is the average time for these patients.
Figure 6.
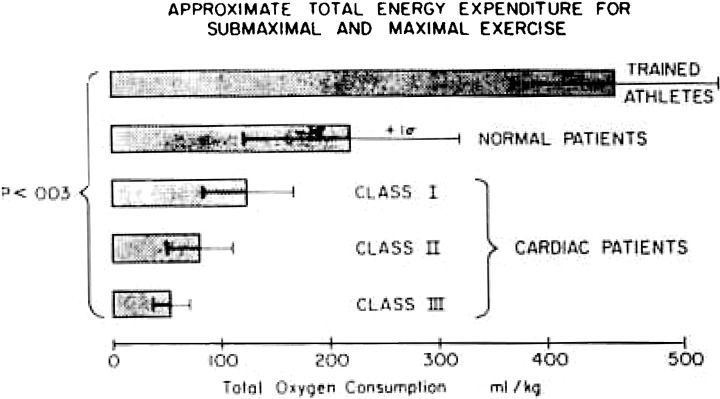
Comparison of approximate total energy expenditure in terms of total oxygen intake/Kg in athletes, normals and cardiac patients. (Same cases as shown in Figure 5.)
To date 269 clinical tests of exercise capacity have been performed on allegedly normal subjects and patients with cardiovascular diseases. About 4% have been unsatisfactory because of obviously inappropriate motivation to attain maximal exertion. In a few instances the test was repeated either to determine the reproducibility or to ascertain the effects of therapy. The distribution of 83 normals and 136 patients according to the highest stage of exercise attained is shown in Figure 7. None of the normals who ranged in age from 15 to 62 years of age was limited to the first stage, which happened to be the maximal work load for 18% of the patients. The majority of patients were unable to go beyond the 2nd stage, while the majority of normals attained the 3rd stage. Only 1 patient, a 15‐year‐old male with uncomplicated ventricular septal defect reached the 4th stage of this test.
Figure 7.
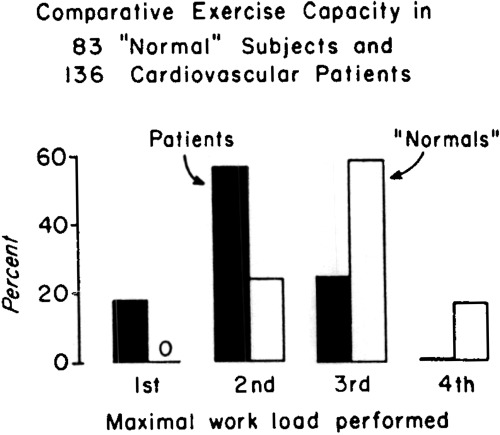
Comparative distribution of normal subjects and cardiac patients according to highest stage of exercise test attained (not necessarily completed).
Averages of maximal heart rate, oxygen intake, duration of exercise and total oxygen intake were appreciably less in older than in younger normal subjects (Table 1). Similarly, these variables varied with the predominant cardiovascular lesion. Duration and total oxygen intake were highest in patients with hypertensive disease and lowest in patients with angina pectoris. Intermediate values were observed in patients with healed myocardial infarction or valvular lesions.
Table 1.
Average Responses to Maximal Exercise (Males and Females Combined)
| Groups | N | Age years | Maximal* | Total# | ||
|---|---|---|---|---|---|---|
| HR/min. | V̇o2 ml/Kg/min. | Duration Seconds | V̇o2 ml/Kg | |||
| Normals < 36 years of age | 41 | 24.8 | 184 | 32.5 | 506 | 201 |
| Congenital Cardiacs | 21 | 25.5 | 164 | 18.7 | 315 | 113 |
| Normals > 35 years of age | 42 | 44.6 | 171 | 23.2 | 387 | 114 |
| Hypertensive Disease | 7 | 44.1 | 153 | 18.0 | 329 | 102 |
| Myocardial Infarction | 29 | 51.1 | 145 | 15.9 | 303 | 73 |
| Aortic Regurgitation | 11 | 38.3 | 159 | 16.4 | 317 | 74 |
| Aortic Stenosis | 12 | 46.8 | 151 | 18.0 | 301 | 81 |
| Mitral Regurgitation | 16 | 43.4 | 161 | 16.5 | 278 | 71 |
| Mitral Stenosis | 25 | 40.7 | 157 | 14.5 | 266 | 59 |
| Angina Pectoris | 9 | 55.3 | 135 | 14.1 | 233 | 40 |
HR = heart rate
*Maximal refers to maximal rates per minute
V̇o2= oxygen intake
# Total represents summation for entire duration of exercise
Determination of maximal exercise capacity is an effective way to assess either therapy or recovery from illness. Two examples will be cited.
Preoperative study of K.K., a 29‐year‐old woman with tight mitral stenosis and minimal aortic regurgitation indicated she was able to walk only 15 seconds in the 2nd stage because of severe dyspnea and fatigue. Although not digitalized, the ECG revealed 2 mm of ST depression when heart rate accelerated to 175; this persisted for 2 minutes in recovery. Systolic blood pressure fell from 150 to 140 mm Hg indicating exertional hypotension. Four months after a successful mitral commissurotomy, she was able to walk for 2% minutes in the 2nd stage with only moderate dyspnea. Again the heart rate accelerated to 175/minute, but there was less than 0.5 mm ST depression. On this occasion systolic pressure rose from 138 to 190 mm Hg. Total oxygen intake increased from 50 to 72 ml/Kg. Clinically, her functional capacity had improved from Class III to Class II.
Satisfactory recovery from acute myocardial infarction was documented in L.A.H., a 47‐year‐old male with a functional capacity of Class I. He was able to walk for 3 minutes in the 2nd stage and 25 seconds in the 3rd stage at 5 mph and 18% grade. Heart rate increased from 65 at rest to 130/minute with this exertion, and blood pressure rose from 110/80 to 170/80 mm Hg. The ECG showed neither premature beats nor ST depression. Total oxygen intake was 87 mm/Kg.
So far there have been no serious consequences from testing ambulatory cardiac patients in this manner. Actually, since many impaired cardiacs are unable to perform as much work as normals, they usually show clinical recovery from this maximal stress as quickly as the normal subjects who expend much more energy.
ELECTROCARDIOGRAPHIC RESPONSES TO MAXIMAL‐EXERTION
Two and 3 stage exercise tests with progressive work loads until exhaustion in over 150 normal college men1 have failed to show any ST depression indicative of myocardial ischemia. Yet junctional changes varying with respiration from elevation to depression are commonly seen with strenuous exertion. An example is illustrated in Figure 8. This first became apparent during the 3rd minute of the first stage of walking slowly. The magnitude of this respiratory variation increased with the faster heart and respiratory rates during the second and third stages, and then faded away during the first 2 minutes of recovery. There was also some respiratory variation of the baseline, and amplitudes of the QRS and T forces.
Figure 8.
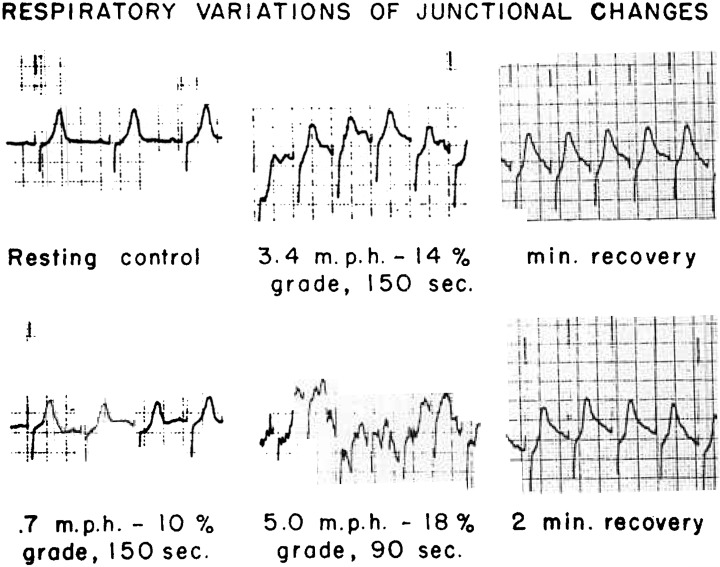
Example of respiratory variation of the ST junction in the precordial lead electro‐cardiogram.
Minor degrees of ST depression with maximal exertion are observed in otherwise normal individuals. The exact frequency has not yet been determined, but the incidence increases with each decade of age. A positive ECG response suggestive of ischemia does not necessarily indicate demonstrable coronary arterial disease. 2
For example, J.L., a 36 year old male was able to attain the 3rd stage of exertion despite ST depression, and showed atrial premature beats in recovery. Yet 3 separate injections of contrast material revealed normal coronary arteries by angiographic examination. Longitudinal studies will be necessary to evaluate the potential diagnostic and prognostic significance of ST depression in individuals who have a good exercise capacity.
A classical example of ST depression due to myocardial ischemia is shown in Figure 9.
Figure 9.
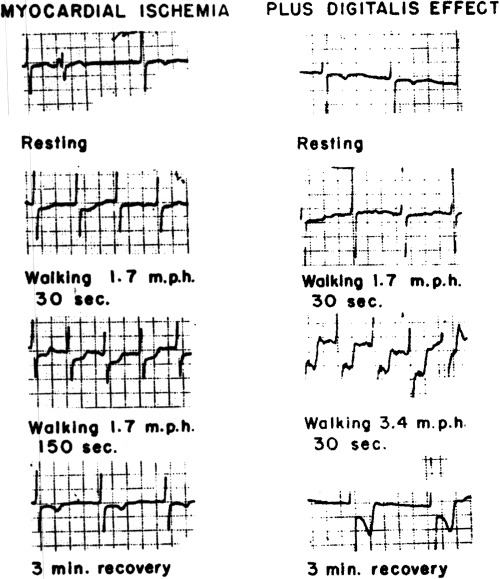
Demonstration of progressive ST depression due to myocardial ischemia in a patient with angina pectoris and slight evidence of congestive failure is displayed on the left. (These tracings were recorded with 0.5 mv. standardization.) Additional effects of digitalis therapy, which increased exercise capacity and delayed onset of typical chest pain until after exertion, are shown on the right.
L.H., a 69 year old male, had angina pectoris for some time and used nitroglycerine as necessary. He developed pain with the 1st stage of this test. Slight ST depression was apparent within the first minute, and this amounted to 4 to 6 mm displacement by the end of the 3rd minute of exertion, and slowly diminished during the first 5 minutes of recovery. He exhibited occasional ventricular premature beats during exercise and recovery. The T wave inverted during the recovery period.
An example of ST depression representative of the combined effects of myocardial ischemia and digitalis effect is also shown in Figure 9.
The same patient, L.H., was digitalized and retested 2 weeks later. Exercise capacity improved and he was able to walk for one minute, until limited by dyspnea, during the second stage of the test. ST depression increased to 6 to 8 mm while the QT interval shortened from 0.40 to 0.32 seconds. Yet typical chest pain was not noticed until the recovery period.
Altogether nearly one‐half of the patients with angina pectoris and/or healed myocardial infarction have exhibited ST depression with maximal exertion. Possibly adequate collateral circulation prevents the others from exhibiting this effect. One‐quarter of the patients with valvular heart disease or hypertension and only 8% of the congenitals have shown this change.
Some “normals” have shown ST depression with this maximal exertion when this response was absent on Master's test. The frequency of such occurrences is currently under study. 24
Patients with a ventricular aneurysm may develop ST elevation during exertion (Fig. 10).
Figure 10.
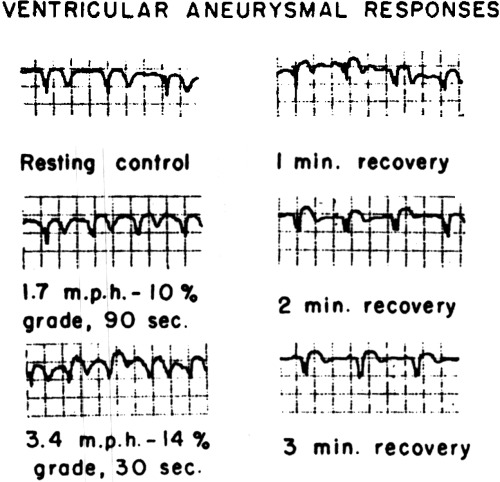
Demonstration of elevation of ST segment in an ambulatory executive with a ventricular ancurysm. llc continues to work full time despite mild fitigue
T.R., a 55 year old male with previous anterior wall infarction showed 1‐2 mm elevation; yet he was able to continue exertion for 80 seconds to the 2nd stage of the test. Another 54 year old patient, W.B., with 2 previous myocardial infarcts and a large ventricular aneurysm posterolaterally showed no ST deviation, but rather widening of the QRS interval from 0.10 to .15 seconds with some junctional changes (Fig. 11). Although he developed chest pain, he continued walking for 3 minutes in the second stage. During the second minute of recovery, he had a paroxysmal of ventricular tachycardia with a rate of 200 for a few seconds.
Figure 11.
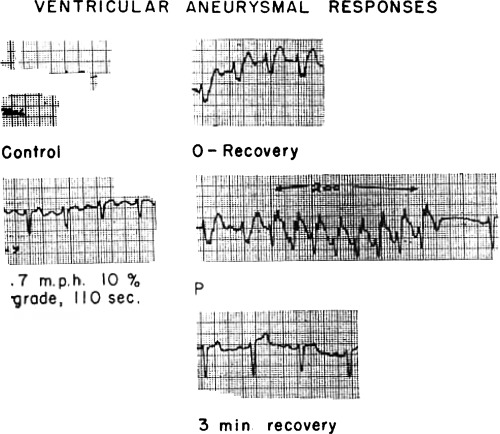
A rarely observed prolongation of QRS conduction followed by a short paroxysm of ventricular tachycardia in recovery in another patient with a large ventricular aneurysm. He continues to do moderate physical work.
These findings, although not commonly observed, are not predictable. Therefore, they indicate the value and need for ECG monitoring.
One “normal” control exhibited 2 premature ventricular beats during the 2nd minute of the 2nd stage. He suddenly felt fatigued and wanted to stop. Within the first few seconds of recovery he showed multifocal ventricular beats and one short paroxysm of ventricular tachycardia with a rate over 200/minute (Fig. 12).
Figure 12.
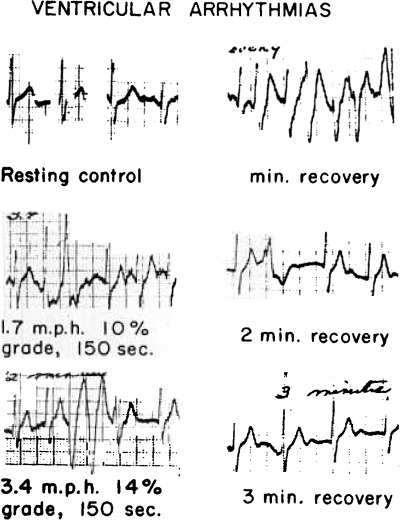
Occasional ventricular premature beats during exercise and a short paroxysm of ventricular techycardia immediately after exertion in an otherwise normal control subject.
Even a patient with an implanted pacemaker and fixed heart rate can exhibit interesting changes. During initial recovery after exercise for 3 minutes, J.C. showed 3 beats initiated by the AV node (Fig. 13).
Figure 13.
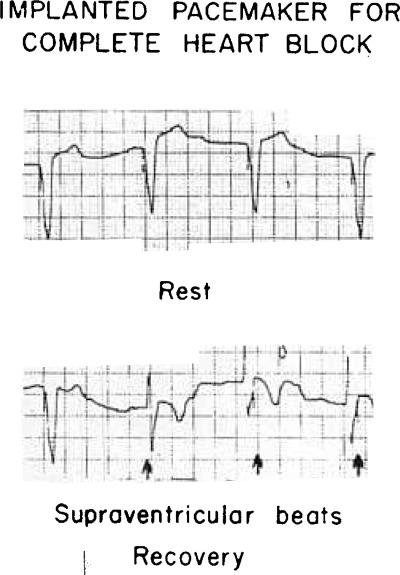
Transient restoration of supraventricular conduction after exertion in a patient with complete heart block and implanted pacemaker with a fixed rate. Note that stimulus artefact follows, rather than precedes QRS responses momentarily.
By observing heart rate, ST displacement and duration of the exercise test, it is generally possible to differentiate patients with ischemic heart disease from those with chest pain of non‐cardiac origin.
COMMENTS
Several approaches to assessment of physical working capacity have shown the complexities of the problems and the limitations of the methods. From this experience certain principles begin to emerge. The only satisfactory appraisal of capacity for exercise is maximal exertion. A treadmill ergometer effectively regulates the rate of energy expenditure for a common from of exertion. Since virtually the entire body weight is supported by the exercising legs, higher work loads are more readily attained than with a subject seated on a bicycle ergometer. Preliminary submaximal work loads should be permitted before very high work loads are imposed. Three minute periods of submaximal exertion provide the optimal compromise between requirements for physiological adaptations and minimal time for expeditious testing. Although assessment of anaerobic responses would provide a biochemical appraisal of circulatory inadequacy of oxygen transport, it may be roughly estimated as one‐fifth to one‐third of the metabolic response when maximal work is achieved. 25 This is usually identified subjectively as exhaustive fatigue; sometimes it is accompanied by severe dyspnea, chest pain, claudication, weakness or nausea. The validity of such symptoms is suspect in rare instances when physiological responses to stress are much less than expected and duration of effort is markedly shortened. Aerobic capacity for exertion should be considered in relation to body weight. When analyzed in relation to heart rate, oxygen pulse and apparent oxygen deficit per kilogram of body weight, the interface between circulatory adjustments and metabolic requirements for oxygen transport can be assessed for the body as a whole. Under the conditions of the multistage‐test presented here, preliminary observations of rates of energy expenditure failed to differentiate cardiac patients from normal subjects at work loads both groups could perform. Maximal oxygen intake could not be measured when individuals were unable to continue exertion for as long as one minute at the highest work load. (Under these conditions it was assumed to be as much as observed in the preceding submaximal work load.) Therefore statistical evaluation of maximal rates of oxygen intake for many groups of patients failed to show as much significance as anticipated. Estimates for total oxygen intake, representing the summation of available data for all work loads differentiated each functional class of cardiacs from normals however. Total duration of time was not as satisfactory.
While exercise capacity is being determined, it is essential to monitor myocardial and circulatory responses for any significant changes due to arrhythmias, ischemia and/or hypotension. The supervising physician must be prepared to terminate the test abruptly whenever hazardous changes develop. He should also accept the patient's desires to stop the exertion, even though the objective evidence of distress may not be impressive. If indicated after further discussion with the patient, the test may be repeated at once.
With further refinements in selection of normal controls and cardiac patients, improvements in technical measurements of metabolic and circulatory responses, and possibly the use of other intermediary work loads, a more precise appraisal of physical working capacity may become available in the future. But the results will still be affected by variations in conditioning, motivation and apprehension which occur in both normals and cardiacs whenever a test of performance is utilized. Furthermore, responses in some patients will be altered somewhat by the presence of other diseases or physiologic states, which affect the circulatory transport of oxygen during the stress of exercise.
SUMMARY
-
1
Several approaches to assessment of physical work capacity in the upright posture in normal adults and cardiac patients have been reviewed critically.
-
2
Preliminary experience has been presented with a new multistage treadmill test of maximal exercise which permits appraisal of either a physically trained normal subject or an impaired but ambulatory cardiac patient.
-
3
The most effective means of differentiating cardiacs from normals has been an estimate of the total oxygen intake/Kg of body weight.
-
4
The need for monitoring the circulation with respect to arrhythmias, ischemia and/or hypotension has been emphasized.
The authors wish to acknowledge their appreciation of many physicians, particularly Dr. Robert M. Levenson of the Seattle Cardiac Work Evaluation Clinic, and medical and graduate students who have assisted in the testing of patients and normals. The assistance of Mrs. Gladys Pettet is gratefully acknowledged also.
These studies have been supported in part by Grant H908 from the National Heart Institute, National Institutes of Health, U.S. Public Health Service.
Footnotes
In 2 instances, however, transient 2:1 AV conduction was observed during the first 2 minutes of recovery.
REFERENCES
- 1. Master AM, Pordy L, Chesky K. Two step exercise electrocardiogram. Follow‐up investigation in patients with chest pain and normal resting electrocardiogram. JAMA 1953;151: 458. [PubMed] [Google Scholar]
- 2. Mattingly T. The postexercise electrocardiogram. Its value in the diagnosis and prognosis of coronary arterial disease. Am J Cardiol 1962;9: 395. [DOI] [PubMed] [Google Scholar]
- 3. Yu PNG, Soffer A. Studies of electrocardiographic changes during exercise (modified double two step test) Circ 1952;6: 183. [DOI] [PubMed] [Google Scholar]
- 4. Wahlund H. Determination of physical working capacity. A physiological and clinical study with special reference to standardization of cardio‐pulmonary tests. Acta Med Scand 1948;132(suppl):215. [Google Scholar]
- 5. Kjellberg SR, Rudhe U, Sjöstrand T. The amount of hemoglobin (blood volume) in relation to the pulse rate and heart volume during work. Acta Physiol. Scand 1949;19: 152. [Google Scholar]
- 6. Holmgren A, Ström G. Blood lactate concentrations in relation to absolute and relative work loads in normal men, and in mitral stenosis, atrial septal defect and vasoregulatory asthenia. Acta Med Scand 1959;163: 185. [DOI] [PubMed] [Google Scholar]
- 7. Åstrand I. The physical work capacity of workers 50–64 years old. Acta Physiol Scand 1958;42: 73. [DOI] [PubMed] [Google Scholar]
- 8. Balke B, Ware RW. An experimental study of “physical fitness” of Air Force personnel. US Armed Forces Med J 1959;10: 675. [PubMed] [Google Scholar]
- 9. Bruce RA, Lovejoy FW Jr, Yu PNG, McDowell ME. Evaluation and significance of physical fitness for moderate work. AMA Arch Ind Hyg Occupat Med 1951;4: 236. [PubMed] [Google Scholar]
- 10. Johnson RE, Brouha L, Darling RC. A test of physical fitness for strenuous exertion. Rev Canad Biol 1942;1: 491. [Google Scholar]
- 11. Bruce RA. Evaluation of functional capacity and exercise tolerance of cardiac patients. Mod Concepts Cardiovasc Dis 1956;25: 321. [PubMed] [Google Scholar]
- 12. Bruce RA, Merendino KA, Pampush JJ, Bergy GG. Functional evaluation of mitral valvulotomy. Superiority of the treadmill exercise tolerance test to clinical and resting hemodynamic evaluations in selecting patients. Am J Med 1956;20: 745. [DOI] [PubMed] [Google Scholar]
- 13. Bruce RA, Cobb LA, Katsura S, Morledge JII, Andrus WW, Fuller TJ. Exertional hypotension in cardiac patients. Circ 1959;19: 543. [DOI] [PubMed] [Google Scholar]
- 14. Harris EA. Exercise tolerance tests. The Lancet Aug 23 1958;409. [DOI] [PubMed] [Google Scholar]
- 15. Rowell LE. Personal communication. 1962.
- 16. Hill AV, Long CNH, Lupton H. Muscular exercise, lactic acid, and the supply and utilization of oxygen. Proc Royal Soc B 1924;97: 84. [Google Scholar]
- 17. Taylor HL, Buskirk E, Henschel A. Maximal oxygen intake as an objective measure of cardiorespiratory performance. J. Appl Physiol 1955;8: 73. [DOI] [PubMed] [Google Scholar]
- 18. Åstrand PO. Experimental studies of physical working capacity in relation to age and sex. Copenhagen , Ejnar Munksgaard, 1952. [Google Scholar]
- 19. Åstrand I. Aerobic work capacity in men and women with special reference to age. Acta Physiol Scand 1960;49(Suppl):169. [PubMed] [Google Scholar]
- 20. Mitchell JH, Sproule BJ, Chapman CB. The physiological meaning of the maximal oxygen intake test. J. Clin. Invest 1958;37: 538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huckle MS Jr, Staudacher RJ. Personal communication. 1962.
- 22. Anderson TD. Personal communication. 1962.
- 23. Taylor HL, Henschel A, Brozek, J , Keys A. Effects of bed rest on cardiovascular function and work performance. J. Appl Physiol 1949;2: 223. [DOI] [PubMed] [Google Scholar]
- 24. Doan A Unpublished studies. 1962.
- 25. Bruce RA, Jones JW, and Strait GB Anaerobic Metabolic Responses to Acute Maximal Exercise in Male Athletes. In preparation 1963. [DOI] [PubMed]


