Abstract
Background
There are limited data regarding racial differences in response to cardiac resynchronization therapy with defibrillator (CRT‐D).
Methods
We assessed the effectiveness of CRT‐D, as compared to implantable cardioverter defibrillator (ICD) therapy alone, in reducing the risk of heart failure (HF) or death and changes in cardiac volumes among 1638 (90%) white patients and 143 (8%) black patients enrolled in the Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT‐CRT).
Results
Enrolled black patients displayed a higher frequency of diabetes mellitus, treated hypertension, higher creatinine levels, and a lower distance walked in the baseline 6‐minute walk test. Kaplan‐Meier survival analysis showed that at 3 years of follow‐up the cumulative probability of HF or death was higher among blacks (29%) as compared with whites (22%; P = 0.05). Both black and white patients experienced similar and pronounced reductions in cardiac volumes with CRT‐D therapy (all P values for comparison between the two groups >0.10). Risk reduction conferred by CRT‐D therapy as not significantly different between blacks and whites (hazard ratio = 0.78 and 0.60, respectively; P for the difference = 0.44). However, possibly due to sample size limitations the CRT‐D versus ICD only adjusted risk for HF/death in blacks was not statistically significant.
Conclusions
Black patients in MADIT‐CRT experienced increased risk of HF or death as compared with whites, but displayed a similar magnitude echocardiographic response to CRT‐D. These findings suggest that cardiac resynchronization therapy may be an effective therapeutic modality in black patients. However, further studies are needed to assess the clinical response to CRT‐D in this high‐risk population.
Keywords: cardiac resynchronization therapy, heart failure, race
Black patients were shown to have increased risk for heart failure (HF), sudden cardiac death, and all‐cause mortality,1 − 4 and demonstrate attenuated response to treatment with angiotensin converting enzyme (ACE) inhibitors.5, 6 Thus, device therapy, employing cardiac resynchronization therapy with a defibrillator (CRT‐D), may improve outcomes in this high‐risk population. Currently, however, data regarding the possible racial differences in response to CRT‐D are limited. The Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy (MADIT‐CRT) assessed the ability of CRT‐D to reduce the risk of the primary end point (death or HF, whichever came first) in asymptomatic or mildly symptomatic HF patients with a left ventricular ejection fraction (LVEF) ≤ 0.30 and QRS duration ≥ 130 ms.7 The study showed that CRT‐D was associated with a 34% reduction in HF or death compared to implantable cardioverter defibrillator (ICD) therapy alone after a mean follow‐up period of 2.4 years.7 The aim of the present MADIT‐CRT substudy was to compare the clinical and echocardiographic response to CRT‐D therapy between black and white patients enrolled in the trial.
METHODS
MADIT‐CRT
The design and primary results of MADIT‐CRT were recently published.7, 8 Briefly, between December 22, 2004, and April 23, 2008, a total of 1820 patients were enrolled in the study at 110 hospital centers. Enrolled patients were of either sex, 21 years of age or older, and had a low LVEF (30% or less), a prolonged QRS interval (130 ms or greater), sinus rhythm, and ischemic cardiomyopathy (NYHA Class I or Class II) or nonischemic cardiomyopathy (NYHA class II only). Patients were randomly assigned in a 3:2 ratio to receive either CRT‐D or ICD therapy. The institutional review board approved the MADIT‐CRT protocol at each participating center, and all patients gave written informed consent prior to enrollment.
Among the 1820 enrolled patients, 1638 (90%) were white; 143 (8%) patients were black; and 39 (2%) were Hispanic or other racial/ethnic groups. Racial grouping was defined according to self‐reported racial and ethnic populations. Because of the small number and diversity of Hispanic and other racial groups, we focused our analysis on the comparison between black and white patients enrolled in the trial (total n = 1781, comprising 98% of the study population).
Echocardiographic Studies
Echocardiograms were obtained according to a study‐specific protocol at baseline, which was prior to device implantation (n = 1809) and at 1 year. Paired echocardiograms from baseline and at 12 months with device turned on were available in 1354 black and white patients enrolled in the study (76%).
Echocardiograms were sent on videotape or digital storage to the echocardiographic core laboratory at Brigham and Women's Hospital where they were screened for quality, and left ventricular, right ventricular, and left atrial measurements were made. Echocardiographic parameters were measured according to established American Society of Echocardiography protocols.9 Left ventricular and atrial volumes were measured by Simpson's method of disks in the apical four‐chamber and two‐chamber views and averaged. LVEFs were calculated according to standard methods. Reproducibility of the primary volumetric measures was assessed by having the primary observer re‐analyze 101 random studies. The coefficient of variation for end‐diastolic volume, end‐systolic volume, and ejection fraction were 5.2%, 6.2%, and 5.5%, respectively.
Study Design and End Points
After the publication of the primary report of MADIT‐CRT,7 analyses were done comparing left bundle branch block (LBBB) patients, comprising 70% of the study patients, with non‐LBBB patients, revealing evidence that the CRT‐D benefit of reducing risk of the primary end point appeared to be largely, or even entirely, in the LBBB subgroup.10 Consistent with this finding, the assessment of CRT‐D efficacy in black and white patients was allowed for possible differential effects by QRS morphology, specifically, LBBB or non‐LBBB at baseline.
Clinical Response
We assessed the effect of CRT‐D versus ICD‐only therapy on the clinical end points of (1) the first occurrence of a nonfatal HF event or death, whichever came first, during follow‐up; and (2) the first occurrence HF alone.
Remodeling Effects
An echocardiographic response was defined as percent improvement in ejection fraction and reduction in cardiac volumes (including left ventricular end diastolic volume [LVEDV]), left ventricular end systolic volume [LVESV], and left atrial volume [LAV]) between enrollment and 1 year (calculated as the difference between 1‐year cardiac volumes and baseline cardiac volumes, divided by baseline cardiac volumes).
Statistical Analysis
The clinical characteristics of study patients were compared by race using the chi‐square test for categorical variables, and the t‐test for continuous variables. Kaplan‐Meier estimates for HF or all‐cause mortality and of HF alone by treatment allocation in black and white patients were determined and statistically evaluated with the log‐rank test. The Cox proportional hazards regression model was used to evaluate the independent contribution of baseline clinical factors to the development of the end points. All models included the following prespecified covariates: race, treatment arm, age ≥ 65, ischemic status, LBBB, diabetes mellitus, LAV index (mL/body surface area [BSA]), enrollment LVEF, and creatinine ≥1.4 mg/dL. The effect of treatment allocation on outcomes in black and white patients was assessed by including a treatment‐by‐race interaction term in the multivariate models.
Interaction term analysis was also used to assess the benefit of CRT‐D in black and white patients separately by gender, the etiology of cardiomyopathy (categorized as ischemic vs nonischemic), QRS duration (dichotomized at ≥150 ms), and QRS morphology (categorized by the presence or absence of LBBB). Echocardiographic changes in ejection fraction and cardiac volumes at 1 year with CRT‐D therapy were compared between black and white patient groups with Student's t‐test or chi‐square test, as appropriate. All P values were two‐sided, and a P value < 0.05 was considered significant. Analyses were performed with the use of SAS software (version 9.20; SAS Institute, Cary, NC).
RESULTS
The baseline clinical characteristics of study patients by race are presented in Table 1. Black patients enrolled in this trial displayed a higher frequency of diabetes mellitus, treated hypertension, higher creatinine levels, and a lower distance walked in the baseline 6‐minute walk test, whereas whites had a higher frequency of patients with an older age, an ischemic etiology of cardiomyopathy, and atrial tachyarrhythmias prior to enrollment. The two groups did not display statistically significant differences in baseline echocardiographic parameters. Similarly, cardiac medications were prescribed to a similar frequency of black and white patients, with the exception of digitalis and diuretic, which were prescribed more frequently in blacks.
Table 1.
Baseline Characteristics by Race
| Whites | Blacks | ||
|---|---|---|---|
| (n = 1638) | (n = 143) | P Value | |
| Age at enrollment (years) | 65 ± 11 | 61 ± 11 | <0.001 |
| Male gender | 76% | 61% | <0.001 |
| Cardiac history | |||
| Ischemic heart disease | 57% | 34% | <0.001 |
| Nonischemic heart disease | 43% | 66% | <0.001 |
| NYHA class II | 85% | 94% | <0.01 |
| BNP level (pg/mL) | 122 ± 152 | 152 ± 233 | 0.79 |
| NYHA Class III or IV >3 months before enrollment | 10% | 12% | 0.58 |
| Hypertension | 62% | 80% | <0.001 |
| Atrial arrhythmia >1 month before enrollment | 12% | 5% | <0.01 |
| Diabetes mellitus | 29% | 39% | 0.01 |
| Cigarette smoking | 12% | 12 | 0.97 |
| Body mass index ≥30 kg/m2 | 35% | 42% | 0.11 |
| Prior coronary artery bypass graft | 30% | 12% | <0.001 |
| Cardiac findings at enrollment | |||
| Systolic blood pressure (mmHg) | 123 ± 17 | 122 ± 18 | 0.68 |
| Diastolic blood pressure (mmHg) | 72 ± 10 | 72 ± 10 | 0.99 |
| Blood urea nitrogen >25 mg/dL | 24% | 20% | 0.28 |
| Creatinine ≥ 1.4 mg/dL | 21% | 28% | 0.04 |
| Left bundle branch block (LBBB) | 71% | 65% | 0.11 |
| Right bundle branch block (RBBB) | 12% | 15% | 0.24 |
| QRS duration (ms) | 158 ± 20 | 156 ± 19 | 0.14 |
| QRS duration ≥ 150 ms | 65% | 62% | 0.44 |
| Enrollment left ventricular ejection fraction | 29 ± 3 | 29 ± 3 | 0.65 |
| 6‐Minute walk distance (m) | 363 ± 106 | 332 ± 110 | <0.001 |
| Echocardiogram/Doppler (baseline) | |||
| LVEDV index (mL/m2) | 124 ± 29 | 120 ± 26 | 0.10 |
| LVESV index (mL/m2) | 88 ± 23 | 85 ± 20 | 0.19 |
| LAV index (mL/BSA) | 47 ± 10 | 45 ± 10 | 0.09 |
| Medications at baseline | |||
| Aldosterone antagonist | 31% | 37% | 0.16 |
| Amiodarone | 7% | 4% | 0.15 |
| Angiotension‐converting‐enzyme inhibitors | 77% | 79% | 0.57 |
| Angiotensin receptor blockers | 21% | 22% | 0.77 |
| Beta‐blockers excluding Sotalol | 93% | 95% | 0.36 |
| Digitalis | 24% | 43% | <0.001 |
| Diuretic | 67% | 76% | 0.02 |
| Lipid‐lowering statin drugs | 68% | 58% | 0.01 |
Plus‐minus values are means ± SD; other values are percent.
BSA = body surface area; LAV = left atrial volume; LVEDV = LV end diastolic volume; LVEF = left ventricular ejection fraction; LVESV = LV end systolic volume; NYHA = New York Heart Association.
During follow‐up, 328 white patients (20%) and 39 black patients (27%) experienced the primary end point of HF or death. Kaplan‐Meier survival analysis showed that at 3 years of follow‐up the cumulative probabilities of HF or death and of HF alone were higher among blacks as compared with whites (Figs. 1A and B, respectively).
Figure 1.
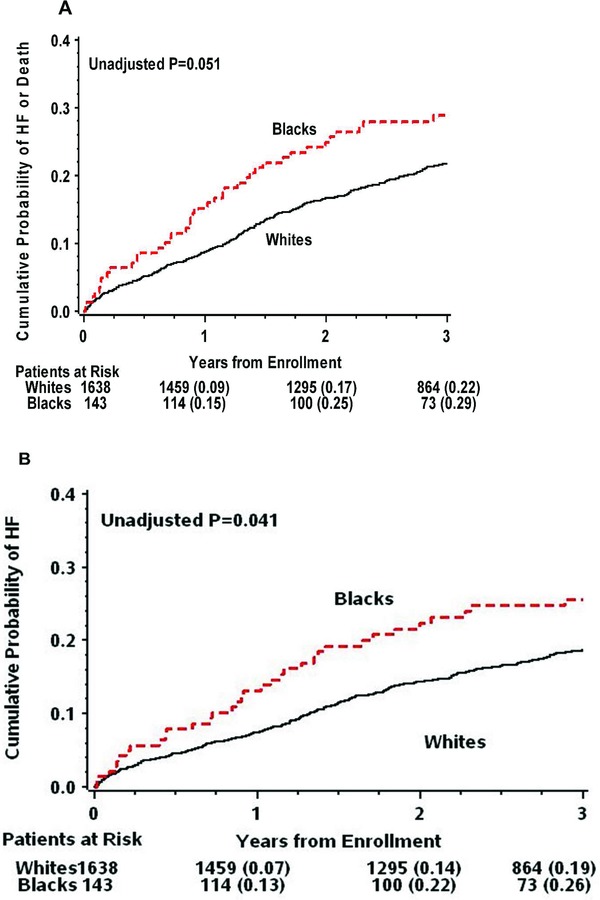
Kaplan‐Meier estimates of the cumulative probability of (A) HF or death; and (B) HF alone, by race.
HF = heart failure.
Clinical Response to CRT‐D in Black and White Patients
Hazard ratios comparing CRT‐D and ICD therapy in blacks and whites for the end points of death or HF (whichever came first) and HF only, in the total study population and in the subgroups of LBBB and non‐LBBB patients, are shown in Table 2. In the total study population and the subgroup of patients with LBBB, CRT‐D conferred a similar magnitude of reduction in the risk of HF or death and of HF alone compared to ICD in both races, with no statistically significant difference in the effect by race (interaction P‐values > 0.10; Table 2). In both black and white patients with LBBB, CRT‐D was associated with >60% reduction in the risk of HF or death, with no significant difference between the races (interaction P value = 0.39). However, possibly due to sample size limitations the effect of CRT‐D therapy on the end points was statistically significant only in white patients (Table 2 and Fig. 2).
Table 2.
Multivariate Analysis: Risk of End Points by Treatment in Blacks and Whites
| CRT‐D:ICD Hazard Ratioa (95% Confidence Interval) | Interaction | ||
|---|---|---|---|
| End Points | Whites | Blacks | P Value |
| Total population (143, 1638)b | |||
| Death or heart failure | 0.60 | 0.78 | 0.44 |
| (0.49–0.73) | (0.42–1.46) | ||
| Heart failure | 0.53 | 0.62 | 0.67 |
| (0.43–0.66) | (0.32–1.20) | ||
| Conduction disturbance | |||
| LBBB (93, 1167)b | |||
| Death or heart failure | 0.47 | 0.67 | 0.39 |
| (0.37–0.60) | (0.31–1.43) | ||
| Heart failure | 0.40 | 0.55 | 0.43 |
| (0.30–0.52) | (0.25–1.22) | ||
| Non‐LBBB (50, 469)b | |||
| Death or heart failure | 1.00 | 1.06 | 0.91 |
| (0.69–1.44) | (0.37–3.05) | ||
| Heart failure | 0.94 | 0.77 | 0.75 |
| (0.64–1.40) | (0.23–2.53) | ||
Adjusted for treatment arm, LBBB, age ≥ 65, left ventricular ejection fraction, creatinine ≥1.4 mg/dL, diabetes mellitus, left atrial volume index (mL/BSA); bNumbers in parentheses represent patient counts (B, W).
Figure 2.
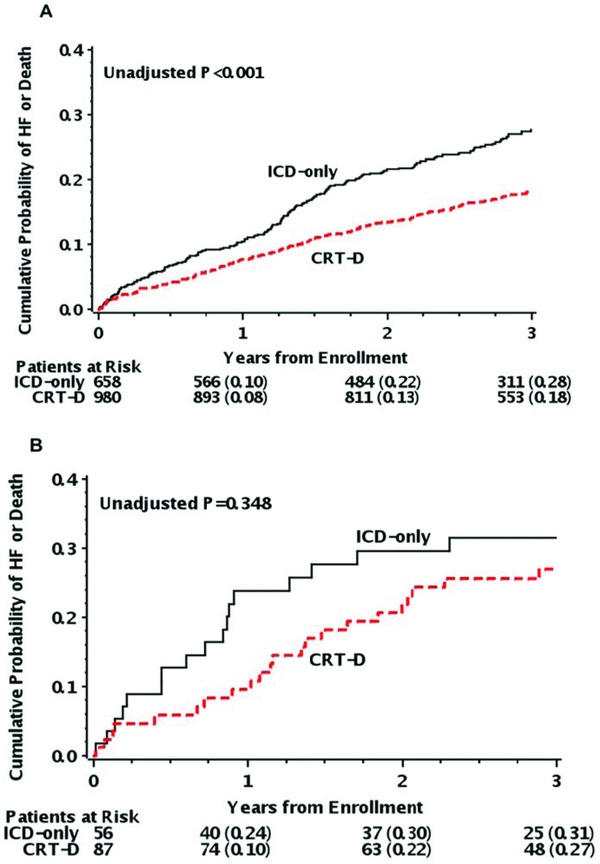
Kaplan‐Meier estimates of the cumulative probability of HF or death by treatment arm in (A) white patients; and (B) black patients.
HF = heart failure.
Subgroup analyses for the primary end point in prespecified race‐related risk subsets showed no significant differences in the effect of CRT‐D therapy between black and white patients in subgroups stratified by the etiology of cardiomyopathy, gender, QRS duration, and QRS morphology (all values for treatment‐by‐race interaction within subgroups >0.10; Fig. 3).
Figure 3.
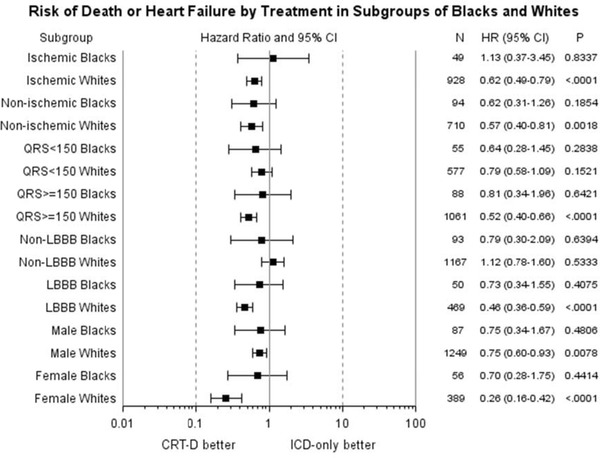
Risk of HF or death in black and while patients in prespecified subgroups (stratified by the etiology of cardiomyopathy, gender, QRS duration, and QRS morphology).
Findings were obtained from multivariate models further adjusted for age ≥ 65, etiology of cardiomyopathy, left ventricular ejection fraction, creatinine ≥1.4 mg/dL, diabetes mellitus, left atrial volume index (mL/BSA); analyses were carried out separately in blacks and whites and the effect in subgroups was assessed using interaction term analysis.
Echocardiographic Response to CRT‐D in Blacks and Whites
At baseline, LVEF, LAV, LVEDV, and LVESV were not significantly different between black and white patients (Table 1). At 1‐year follow‐up, CRT‐D therapy was associated with a pronounced and similar increase in the LVEF among blacks and whites and with significant reductions in cardiac volumes among both black and white patients (all P values for comparison between the two groups >0.10; Figs. 4A and B, respectively).
Figure 4.
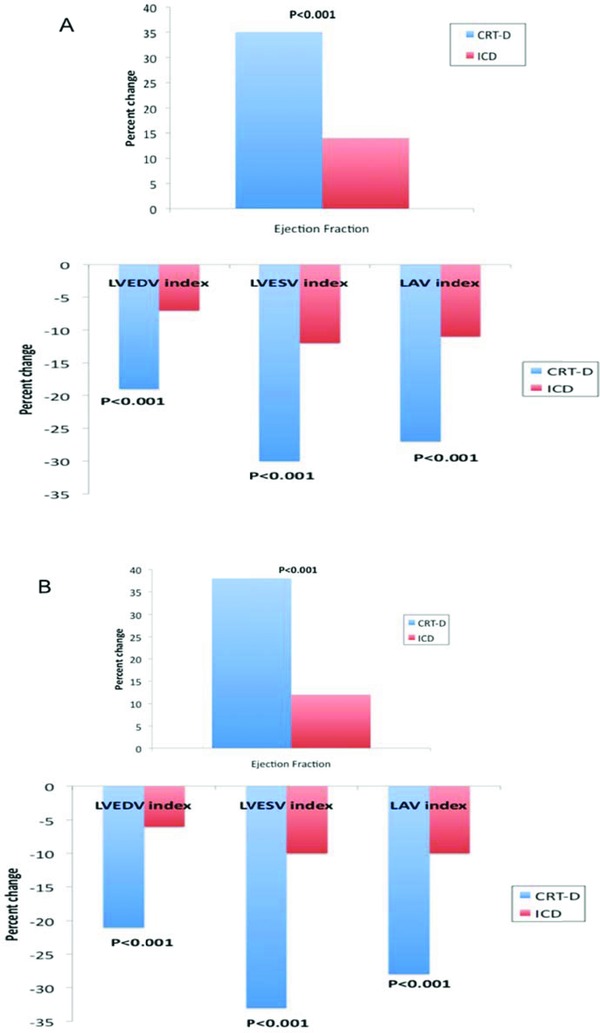
Percent change at 1 year in ejection fraction and cardiac volumes in (A) black patients; and (B) white patients.
DISCUSSION
Our substudy of the MADIT‐CRT trial is the first to compare CRT‐D to ICD therapy in blacks and whites. We have shown that: (1) blacks exhibited higher risk clinical characteristics and consistently experienced a higher rate of HF events during follow‐up; (2) the echocardiographic response to CRT‐D was not significantly different between blacks and whites; and (3) no significant difference in the clinical response to CRT‐D was observed between black and white patients. However, possibly due to sample size limitations, the CRT‐D versus ICD risk of HF or death in blacks was not statistically significant.
Our finding that blacks are at greater risk than whites for several cardiac end points, including HF, is consistent with the Multi‐Ethnic Study of Atherosclerosis,1 as well as other heart studies.2, 3 Although blacks and whites in our study were equally medicated with ACE inhibitors, several previous studies have found that ACE inhibitors are less effective in lowering blood pressure in blacks than whites,5, 6 possibly contributing to black participants being in more advanced stages of HF than white participants from the beginning of the study. Our finding that blacks in MADIT‐CRT were more likely to be on HF medications, particularly digitalis and diuretics, lends support to this claim.
Despite blacks being at greater risk of HF than whites, it is interesting that blacks and whites may derive a similar benefit from CRT‐D therapy. Of the possible reasons for this equal benefit, we believe that the disordered electromechanical physiology of HF is basically the same in different races; thus, the beneficial effects of CRT‐D should be similar in blacks and whites after adjustment for relevant clinical imbalances. While no previous study has explored the responses of blacks and whites to CRT‐D therapy, several studies have shown that the two races have similar clinical responses to some HF medications and device therapies. The Digitalis Investigation Group study, which followed 897 black patients and 6660 white patients for an average of 37 months, found no differences in the ability of the drug digoxin to reduce mortality or CHF‐related hospitalizations in blacks and whites.11 In the Sudden Cardiac Death in Heart Failure trial (SCD‐HeFT), which followed 425 African Americans and 1932 whites for an average of 45.5 months, ICD therapy was associated with equal reductions in all‐cause mortality in blacks and whites, despite black participants being at 27% greater risk of mortality.12 In contrast, our prior MADIT‐II race study showed that ICD therapy was associated with a significantly greater reduction in the risk of sudden cardiac death in white patients as compared with blacks.13
Our findings also suggest that both black and white patients with LBBB benefit more from CRT‐D therapy than any other subgroup. Several prior studies have shown that patients with intraventricular conduction delays, particularly LBBB, have significantly better outcomes with CRT‐D therapy than ICD therapy,10, 14 and this was true in our MADIT‐CRT racial substudy as well.
Our study had several limitations, including the following: (1) Since our data are retrospective in nature, there may exist potential imbalances in important risk variables, such as the frequency of ischemic and nonischemic cardiomyopathy; however, these imbalances were adjusted for in the Cox regression model. (2) With a sample of only 143 black patients (8% of the total MADIT‐CRT study population), the study was underpowered to detect statistically significant treatment effects in blacks, particularly with regard to clinical response to CRT‐D. Despite these sample size limitations, the fact that the hazard ratios for the effect of CRT‐D therapy on the risk of HF or death were similar between the 2 groups is highly suggestive of a similar clinical effect of the device. In addition, the lack of a statistically significant treatment‐by‐race interaction effect for all clinical outcomes also suggests that there is no significant difference in the effect of CRT‐D therapy between black and white patients. (3) In MADIT‐CRT there was a large variability in the enrollment of black patients by center. Thus, the present population may not truly represent the general distribution of HF patients based on race. These effects may be assessed in large population studies. (4) Data about compliance to medications were not collected in MADIT‐CRT, therefore, the effect of on‐treatment medication usage was not assessed in this study. (5) Black patients enrolled in MADIT‐CRT had greater baseline rates of diabetes mellitus, treated hypertension, and creatinine levels than whites, it is possible that these initial comorbidities in blacks might have contributed to their greater risk of cardiac end points (including HF) compared to whites. As stated earlier, the higher frequency of comorbidities among black patients in this study may be due to a selection bias by the enrolling centers rather than a representation of the general population.
In conclusion, although blacks had a higher probability of cardiac events than whites, the results of this study suggest that black and white patients derive a similar echocardiographic response to CRT‐D therapy. The sample of black patients enrolled in MADIT‐CRT may have been underpowered to detect a statistically significant clinical effect. Thus, additional studies, focused primarily on black patients, are needed in order to better characterize the clinical benefit of CRT‐D in this population.
Disclosures: The authors have no conflicts to disclose.
REFERENCES
- 1. Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: The multi‐ethnic study of atherosclerosis. Arch Intern Med 2008;168:2138–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dries DL, Exner DV, Gersh BJ, et al. Racial differences in the outcome of left ventricular dysfunction. N Engl J Med 1999;340:609–616. [DOI] [PubMed] [Google Scholar]
- 3. Alexander M, Grumbach K, Selby J, et al. Hospitalization for congestive heart failure: Explaining racial differences. JAMA 1995;274:1037–1042. [PubMed] [Google Scholar]
- 4. Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: A summary of current research, 1999. Vital Health Stat 1999;2(128):1–13. [PubMed] [Google Scholar]
- 5. Weir MR, Gray JM, Paster R, et al. Differing mechanisms of action of angiotensin‐converting enzyme inhibition in black and white hypertensive patients. Hypertension 1995;25:124–130. [DOI] [PubMed] [Google Scholar]
- 6. Materson BJ, Reda DJ, Cushman WC, et al. Single‐drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. N Engl J Med 1993;328:914–921. [DOI] [PubMed] [Google Scholar]
- 7. Moss AJ, Hall WJ, Cannom DS, et al. Cardiac‐resynchronization therapy for the prevention of heart‐failure events. N Engl J Med 2009;361:1329–1338. [DOI] [PubMed] [Google Scholar]
- 8. Moss AJ, Brown MW, Cannom DS, et al. Multicenter automatic defibrillator implantation trial‐cardiac resynchronization therapy (MADIT‐CRT): Design and clinical protocol. Ann Noninvasive Electrocardiol 2005;10:34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiography 2005;18:1440–1463. [DOI] [PubMed] [Google Scholar]
- 10. Zareba W, Klein H, Cygankiewicz I, et al. for MADIT‐CRT Investigators. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial‐Cardiac Resynchronization Therapy (MADIT‐CRT). Circulation 2011;123:1061–1072. [DOI] [PubMed] [Google Scholar]
- 11. Mathew J, Wittes J, McSherry F, et al. Racial differences in outcome and treatment effect in congestive heart failure. Am Heart J 2005;150:968–976. [DOI] [PubMed] [Google Scholar]
- 12. Mitchell JE, Hellkamp AS, Mark DB, et al. Outcomes in African Americans and other minorities in the Sudden Cardiac Death in Heart Failure Trial (SCD‐HeFT). Am Heart J 2008;155:501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vorobiof G, Goldenberg I, Moss AJ, et al. Effectiveness of the implantable cardioverter defibrillator in blacks versus whites (from MADIT‐II). Am J Cardiol 2006;98:1383–1386. [DOI] [PubMed] [Google Scholar]
- 14. Bristow MR, Saxon LA, Boehmer J, et al. Cardiac‐resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004;350:2140–2150. [DOI] [PubMed] [Google Scholar]


