Abstract
A 65‐year‐old woman was admitted to the hospital because of a syncopal episode with documented transient complete atrioventricular block. A DDD pacemaker was implanted. Post implantation, the patient was diagnosed with bidirectional ventricular tachycardia. Analysis of the arrhythmia and differential diagnosis is performed.
Keywords: bidirectional ventricular tachycardia, differential diagnosis
A 65‐year‐old woman with hypertension, type 2 diabetes, and Chagasic cardiomyopathy was admitted to the hospital because of a syncopal episode with documented transient complete atrioventricular block. At the time of admission, the patient presented with sinus rhythm with recovered A‐V conduction, complete right bundle branch block (CRBBB), and left anterior fascicular block (LAFB) by electrocardiogram (EKG) (Cardisuny C110, Fukuda M‐E, Kogyo Co Ltd., Tokyo, Japan). A DDD pacemaker (St. Jude, St. Paul, MN, USA) was implanted.
Postimplantation, the following situations developed, as shown by the EKG images in Figures 1 and 2. Initially, the patient was diagnosed with bidirectional ventricular tachycardia, alternating with ventricular bigeminy and what was interpreted as ventricular triplets. The patient was asymptomatic. During the isolated ventricular bigeminy, atrial activity was due primarily to atrial pacing, attributed to underlying sinus bradycardia. As seen in Figure 1, QRS “R1” and “R2” alternated with cycle lengths of 400 and 480 milliseconds. “R1” had an image of CRBBB and a frontal axis, directed to the left superior quadrant; “R2” was an atypical image of CRBBB with a frontal axis that was directed inferiorly (+90 degrees). This rhythm appeared to be bidirectional ventricular tachycardia. Ventricular pacing was not observed. As shown in Figure 2, we observed atrial and ventricular pacing, followed by a ventricular premature beat (VPB) that was identical to “R2” in Figure 1, and then a ventricular triplet, initiated with the same VPB (“R2”) that was followed by the same “R1” of Figure 1 and “R2” again. Reviewing the EKG from before implantation of the pacemaker, “R1” was identical to the QRS with CRBB and LAFB that was observed in sinus rhythm.
Figure 1.
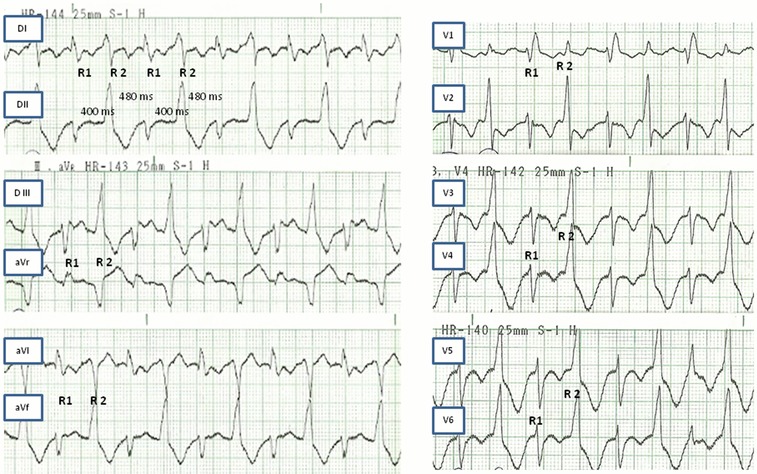
See explanation in text.
Figure 2.
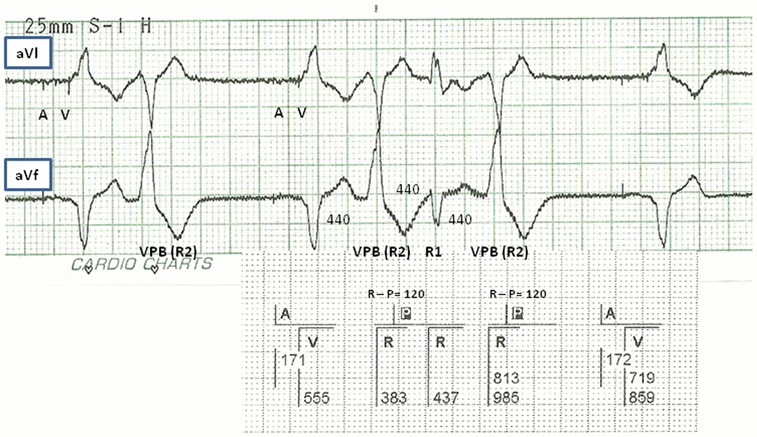
A = auricular pacing stimulation; P = atrial sensed event (during the postventricular atrial refractory period); R = ventricular sensed event; R1 and R2 = see explanation in text; V = ventricular pacing stimulation; VPB = ventricular premature beat.
Controlling the pacemaker with a programmer, the markers allowed us to understand what was occurring. In Figure 2, atrial and ventricular pacing (“A” and “V,” respectively, in the figures) was followed by sensed QRS (“R” in the figures). Some of the QRS was followed 120 milliseconds later by atrial activity (“P” in the figures) included in the post ventricular atrial refractory period of the pacemaker. These QRS (first and third “R” of the triplets—“R2” in the EKG) were VPBs with retrograde ventriculoatrial conduction. The “R” in the middle (“R1” in the EKG) of the triplet was a result of anterograde conduction from the previous retrograde P wave. The “ventricular triplets” were the result of the inability of the second retrograde P wave to conduct anterogradely, and episodes of pseudo “bidirectional ventricular tachycardia” were initiated when anterograde conduction of this retrograde P waves was present (Figure 3). In Figure 3, variation in the cycle length was observed in the EKG between “R1” and “R2” (400 and 480 milliseconds), in contrast to the alternation in the pacemaker markers. This apparent incongruity is explained by disparate times at which the observations were made: in the EKG, the beginning of the QRS— i.e., “global” ventricular activation—and the markers in the pacemaker strip measure the moment of activation in the ventricular area, where the lead dipole is attached.
Figure 3.
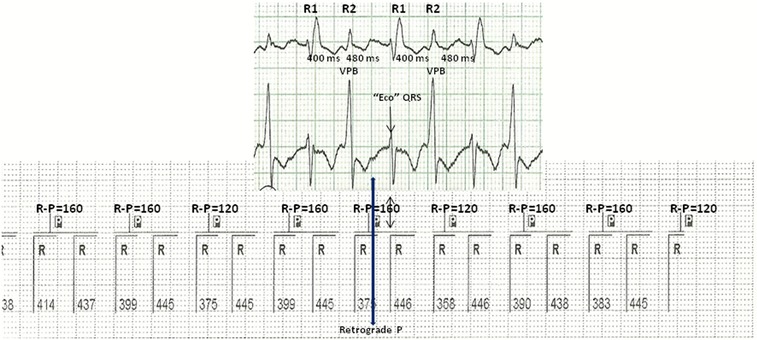
Same as Figure 2.
The addition of a beta‐blocker prevented the retrograde ventriculoatrial conduction from the VPBs and its effects: the triplets and episodes of pseudo ventricular tachycardia.
Bidirectional ventricular tachycardia is characterized by an alternating beat‐to‐beat electrocardiographic QRS axis. Triggered activity and reentry mechanism are postulated as possible mechanisms. The etiology is most commonly digitalis toxicity and rarely herbal aconitine poisoning, hypokalemic periodic paralysis, cathecolaminergic VT, myocarditis, and Anderson‐Tawil syndrome.1, 2, 3, 4, 5, 6
In this case, the ventricular bigeminy with retrograde ventriculoatrial conduction and consequent A‐V conduction causes this pseudo “bidirectional ventricular tachycardia.” In a search trough Pub Med, we did not find published in the literature other case like this. In the differential diagnosis of this ventricular tachycardia, we have to consider this possibility.
Financial support: Clinical fees and Fellowship.
REFERENCES
- 1. Cohen SI, Voukydis P. Supraventricular origin of bidirectional tachycardia. Report of a case. Circulation 1974;50(3):634–638. [DOI] [PubMed] [Google Scholar]
- 2. Klein GJ, Wallace AG, Gallagher JJ. Transfer of coupling of premature ventricular contractions to an ectopic ventricular tachycardia: A mechanism for atypical bidirectional tachycardia. J Electrocardiol 1979;12(1):65–68. [DOI] [PubMed] [Google Scholar]
- 3. Levy S, Hilaire J, Clementy J, Bartolin R, et al. Bidirectional tachycardia. Mechanism derived from intracardiac recordings and programmed electrical stimulation. Pacing Clin Electrophysiol 1982;5(5):633–638. [DOI] [PubMed] [Google Scholar]
- 4. Al‐Khafaji A, Corwin HL, Adhar GC, et al. Bidirectional tachycardia: Two cases and a review. Anesth Analg 2002;95(2):310–315. [DOI] [PubMed] [Google Scholar]
- 5. Siegal D, Quinlan C, Parfrey B, et al. Type II bidirectional ventricular tachycardia as a mechanism of termination of sustained ventricular tachycardia. J Cardiovasc Electrophysiol 2009;20(3):345–346. [DOI] [PubMed] [Google Scholar]
- 6. Baher AA, Uy M, Xie F, et al. Bidirectional ventricular tachycardia: Ping pong in the His‐Purkinje system. Heart Rhythm 2011;8(4):599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]


