Abstract
Background: Although atrial fibrillation (AF) is commonly encountered in patients with constrictive pericarditis (CP), little has been done to clarify its associated predisposing factors. Our aim was to evaluate the association of age, gender, disease duration, and pericardial calcification with AF in these patients.
Methods: The medical records of 44 patients with CP were reviewed. There were 13 (29.5%) with AF and 31 (70.5%) with sinus rhythm. The two groups were compared for demographic variables, disease duration, and the presence of pericardial calcification.
Results: The male‐to‐female ratio was 3.4:1. Calcification was seen in 11 (25%) of the entire group. AF was much more common in those with calcification than those with sinus rhythm (odds ratio, 7.87 [95% CI, 1.73–35.78], P = 0.008). There was no association between the presence of AF and the age (P = 0.156) or gender (P ≈ 1.00). Logistic regression, however, showed that the chance of developing AF increased by 27% by each year of increase in disease duration (P = 0.025).
Conclusion: It seems that in patients with CP, the presence of pericardial calcification and the increasing disease duration are associated with a higher chance of developing AF.
Keywords: constrictive pericarditis, atrial fibrillation, calcification
Atrial arrhythmias including atrial fibrillation (AF) are usually a part of the natural history of constrictive pericarditis (CP). In their recent series of 143 patients with surgically proven CP, Talreja et al. 1 detected AF in 22% of their subjects. These arrhythmias have been attributed to the underlying myocardial abnormalities, atrial dilation, epicardial inflammation, and calcification. 2
Ling and his coworkers 3 have reported calcific pericaditis in 36 (27%) of their 135 patients. A calcified pericardium, however, not necessarily ends up with constriction and that constriction may occur in the absence of pericardial calcification. Since the association between the presence of pericardial calcification and AF is not well defined, this study was done to clarify this issue.
METHODS
The medical records of all patients with hemodynamically and surgically proven CP, who were admitted to our main university hospitals in Shiraz and Isfahan during the years 1970–2005, were reviewed. Demographic data, disease duration, etiologic diagnosis, and the presence of pericardial calcification on histopathological grounds were recorded. In addition, the electrocardiograms (ECGs) of all patients were analyzed for the presence or absence of AF. Subsequently, the patients were divided in those with sinus rhythm or AF and the two groups were compared for all aforementioned variables.
Statistical Methods
Continuous variables, expressed as mean ± SD or median values, were compared by Mann‐Whitney test. Fisher exact test was used for comparison of the sex, and the presence of calcification between the two groups. In addition, logistic regression was used to assess the association of calcification and AF with age and disease duration. All data were analyzed with SPSS‐15 (SPSS Inc., Chicago, IL). A P value <0.05 was considered significant.
RESULTS
There were a total of 44 patients with constrictive pericarditis of whom 13 (29.5%) had AF and the remaining 31 (70.5%) subjects had sinus rhythm. The male‐to‐female ratio was 3.4:1. Tables 1 and 2 show the demographic characteristics, specific causes of constriction, disease duration, and the presence of calcification in those with and without AF. Calcification was seen in 11 (25%) of the 44 patients. This included 7(30%) of 23 patients with idiopathic and 3 (23%) of 13 subjects with tuberculous CP. The underlying cause, however, did not have any association with the presence of calcification (odds ratio 1.46 [95% CI 0.30–6.98] P = 0.716]. The same was also true for age (odds ratio 0.99, P = 0.546) and disease duration (odds ratio 1.007, P = 0.287).
Table 1.
The Age Distribution and Disease Duration in 44 Constrictive Pericarditis Patients with Normal Sinus Rhythm or Atrial Fibrillation
| Constrictive Pericarditsis | P Value | ||
|---|---|---|---|
| Normal Sinus Rhythm n = 31 | Atrial Fibrillation n = 13 | ||
| Age (years) | 0.156 | ||
| Range | 7–74 | 30–63 | |
| Mean ± SD | 36.1 ± 20.46 | 44.8 ± 10.8 | |
| Median | 33 | 45 | |
| Disease duration (months) | 0.078 | ||
| Range | 2–120 | 2–180 | |
| Mean ± SD | 28.9 ± 26.3 | 71.5 ± 69.4 | |
| Median | 24 | 36 | |
Table 2.
The Gender, Etiologic Diagnosis, and the Presence of Calcification in 44 Constrictive Pericarditis Patients with Normal Sinus Rhythm or Atrial Fibrillation
| Constrictive Pericarditis | P Value | ||||
|---|---|---|---|---|---|
| Normal Sinus Rhythm | Atrial Fibrillation | ||||
| Number | Percent | Number | Percent | ||
| Sex | ≈1.00 | ||||
| Males | 24 | 77.4% | 10 | 76.9% | |
| Females | 7 | 22.6% | 3 | 23.1% | |
| Etiologic diagnosis | |||||
| Idiopathic | 15 | 48.4% | 8 | 61.5% | 0.64 |
| Tuberculosis | 10 | 32.3% | 3 | 23.1% | 0.805 |
| Chronic renal failure | 2 | 6.5% | 0 | 0.0% | – |
| Postsurgical (valve replacement) | 2 | 6.5% | 2 | 15.4% | – |
| Traumatic | 2 | 6.5% | 0 | 0.0% | – |
| Calcification | 0.008 | ||||
| Yes | 4 | 12.9% | 7 | 53.8% | |
| No | 27 | 87.1% | 6 | 46.2% | |
AF was much more common in those with calcification than those with sinus rhythm (odds ratio, 7.87 [95% CI, 1.73–35.78], P = 0.008). There was no association between the presence of atrial fibrillation and the age (odds ratio 1.027, P = 0.156) or gender (P ≈ 1.00). Logistic regression, however, showed that the chance of developing AF increased by 27% by each year of increase in disease duration (odds ratio 1.020, P = 0.025) (Fig 1).
Figure 1.
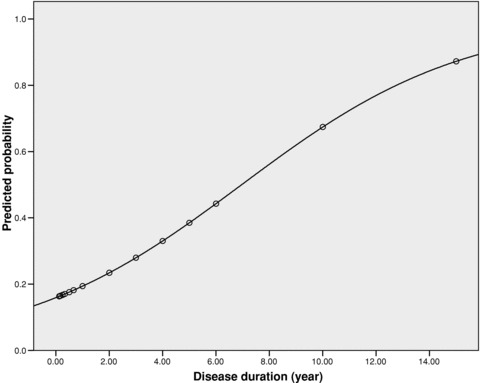
The predicted probability of developing atrial fibrillation with the increasing disease duration.
DISCUSSION
In this series of patients with CP, we found that:
-
1
AF was more frequent in those with pericardial calcification;
-
2
The chance of developing AF increased by 27% by each year of increase in disease duration; and
-
3
Calcification was almost equally common in patients with idiopathic as well as tuberculous CP.
Pericardial calcification was found in 25% of our series, which is very much similar to the 27% reported by Ling et al. However, it was less than the 53% prevalence reported by Rienmüller and colleagues 4 and more than the 5% prevalence reported by Cameron et al. in their series of 106 patients with CP. 5
Thirteen (29%) of our 44 patients had tuberculosis of whom 3 (23%) had calcification. This is in contrast with the 76% when tuberculosis was common in the developed countries too. 6 The presence of calcification was significantly more in those with AF than in patients with sinus rhythm. The 27% prevalence of AF in our series is similar to the 22% reported by Talreja and colleagues in their series of 143 patients with surgically proven constriction. In a series of 135 patients with calcificCP, Ling et al. 3 reported AF to be present in 16 (12%) patients too.
Although AF is a part of the natural history of CP, little has been done to clarify its associated predisposing factors. In this study, the presence of calcification and the increasing disease duration were associated with a higher chance of having AF. We could not detect any age or sex differences between the two groups.
AF is closely associated with some electrophysiological abnormalities of the atria, namely, a reduction in the refractory period and conduction velocity and an increase in the dispersion of the refractory period of the atrial muscle. 7 , 8
Our study is limited by the lack of a systematic study on these electrophysiological parameters and by its small number of patients. Larger series of patients and more detailed studies including electrophysiological studies might illuminate these issues.
REFERENCES
- 1. Talreja DR, Edwards WD, Danielson GK, et al Constrictive pericarditis in 26 patients with histologically normal pericardial thickness. Circulation 2003;108:1852–1857. [DOI] [PubMed] [Google Scholar]
- 2. Goldstein JA. Cardiac tamponade, constrictive pericarditis and restrictive cardiomyopathy. Curr Probl Cardiol 2004;29:503–567. [DOI] [PubMed] [Google Scholar]
- 3. Ling LH, Oh JK, Breen JF, et al Calcific constrictive pericarditis: Is it still with us? Ann Intern Med 2000;132:444–450. [DOI] [PubMed] [Google Scholar]
- 4. Rienmüller R, Gurgan M, Erdmann E, et al CT and MR evaluation of pericardial constriction: A new diagnostic and therapeutic concept. J Thorac Imaging 1993;8:108–121. [DOI] [PubMed] [Google Scholar]
- 5. Cameron J, Oesterle SN, Baldwin JC, et al The etiologic spectrum of constrictive pericarditis. Am Heart J 1987;113:354–360. [DOI] [PubMed] [Google Scholar]
- 6. Aagaard MT, Haraldsted VY. Chronic constrictive pericarditis treated with pericardiectomy. Thorac Cardiovasc Surg 1984;32:311–314. [DOI] [PubMed] [Google Scholar]
- 7. Shimizu A, Centurion OA. Electrophysiological properties of the human atrium in atrial fibrillation. Cardiovasc Res 2002;54:302–314. [DOI] [PubMed] [Google Scholar]
- 8. Lau CP, Tse HF. Electrical remodeling of chronic atrial fibrillation. Clin Exp Pharmacol Physiol 1997;24:982–983. [DOI] [PubMed] [Google Scholar]


