Abstract
Background: The distinction between ST elevation and nonST elevation infarcts is widely accepted and is employed as a guide to management.
Aim: This is review of the world literature to assess the basis for this distinction, since the two studies on which it is based are seriously flawed in method and conclusions.
Method: Pathologic and clinical studies were reviewed from the world literature.
Finding: The pathology of the two subsets is identical as are the morbidity, mortality and clinical course. Non‐ST elevation infarcts are likely to be subsequent, to occur in older patients and to involve the circumflex artery: this subset therefore includes a high‐risk group. ST deviation in any part of the electric field of the heart will predictably be accompanied by reciprocal deviation if the entire field of the heart is mapped. Further, ST deviation of infarction is often transient, resolving in minutes so that infarcts will be predictably misclassified. ST deviation per se is therefore not a rational basis for classification of infarcts. In fact, invasive therapy is indicated in both subsets with identical results.
Conclusion: The distinction between ST elevation and non‐ST elevation infarcts is baseless. The high risk subgroup included in the non‐ST elevation infarct set should not be denied the benefit of early invasive therapy.
Ann Noninvasive Electrocardiol 2010;15(3):191–199
Keywords: electrocardiography
The distinction between a myocardial infarction (MI) accompanied by ST elevation (STEMI) and MI without ST elevation (non‐STEMI) has been accepted universally, albeit uncritically, by the discipline of cardiology. Almost every current or recent publication regarding myocardial infarction employs this classification. 1 , 2 , 3 , 4 , 5 Profound pragmatic considerations hinge on this set of classifications and it is therefore surprising to find that the entire basis for the STE/non‐STE distinction arises from only two clinical studies—GISSI 6 and ISIS. 7 In these studies it was found that myocardial infarcts accompanied only by ST depression were not benefited by thrombolysis with streptokinase, in contrast to the group with ST elevation in which significant numbers showed clear cut benefit. These findings seem to have a slender basis for such a profound and universally accepted classification, a classification, moreover, that connotes a high order of practical significance in terms of pathology, therapy, and prognosis. Several questions must therefore be posed.
-
1
Is there in fact any difference in the pathology of the two subsets?
-
2
Is there any difference in clinical outcome—that is, in long or short‐term prognosis?
-
3
Should treatment differ in the two subsets?
-
4
Do the GISSI and ISIS studies in fact provide a valid basis for this distinction?
-
5
Is the distinction between ST elevation and depression valid in terms of electrocardiographic field theory?
Pathology of NSTEMI and STEMI
Raunio et al. 8 studied postmortem pathology in 80 patients who died of acute myocardial infarction. ST depression was recorded in 38 cases: ST depression was the only abnormality in 16 of these cases, (of which 33% were subendocardial infarcts and 17% transmural). In other words, half of the validated infarcts on postmortem examination were accompanied by ST depression while 20% manifested ST segment depression only. The pathology of the infarcts accompanied by ST elevation was compared critically with those accompanied only by ST depression.
There was no pathologic difference between the infarcts accompanied by ST elevation and those accompanied only by ST depression. The two processes were in fact identical. This study by Raunio and associates appears to present the only documentation to date of the pathology of the two subsets.
Clinical Correlates of Non‐STEMII
Montalescot et al. 9 studied 2151 consecutive MIs. STEMI patients were more likely to undergo invasive therapy or fibrinolysis, and follow‐up treatment was more intensive in this group, but despite these differences, early and late (1‐year) mortality were the same in STEMI and non‐STEMI. There was no difference in any measurable clinical index between the two groups. (The title of this study is illuminating and very much to the point. “STEMI and NONSTEMI—Are They So Different?”).
Lee et al. 10 addressed the specificity of ST depression in a study of 136 patients admitted with suspected MI with ST depression only. Seventy‐four (54%) were confirmed as infarcts: 43 (58%) of that group had previous infarcts. A 4 mm ST depression in a single lead was 20% sensitive and 97% specific for diagnosis of MI, while the finding of a total of 7 leads with ST depression was 21% sensitive and 95% specific for the same diagnosis. The mean age of those with confirmed non‐STEMI was 68 years. The authors comment that … . . “more severe ST depression is highly specific for the subsequent diagnosis of myocardial infarction”.
Kuch et al. 11 reported findings in 6748 consecutive patients diagnosed with MI: 45.8% presented with ST elevation, 14% with ST depression only, 32.4% with no ST deviation, and 7.8% with bundle‐branch block. The 28‐day case fatality in the group with ST depression was slightly higher than in the group with ST elevation (12.4%, vs 8.8%, P = 0.03).
Pitta et al. 12 studied 255,256 patients enrolled in the National Registry of Myocardial Infarction who had an acute MI with initial ST depression. The in‐hospital mortality rate for those with ST depression only was 15.8%—almost exactly the same as for those presenting with ST elevation (15.5%). The authors comment that the current common classifications of “S‐T segment elevation myocardial infarction and non S‐T elevation myocardial infarction has led to serious undertreatment of the high‐risk group associated with S‐T depression, as documented in this and other studies.”
Menown et al. 13 studied 1041 consecutive patients presenting with chest pain (335 with myocardial infarction) and 149 controls without chest pain. The authors point out that “ST elevation has poor sensitivity for acute MI with up to 50% of patients reported as exhibiting ‘atypical’ changes at presentation including isolated ST depression, T inversion or even a normal ECG.” In their series, primary ST depression (ST depression without coexistent elevation) occurred in 130 patients, (45 with acute MI, 85 without). As in the study by Lee and Rawls 10 cited above, they found that the presence of depression in five or six or more leads was associated with high specificity for acute myocardial infarction.
Angiographic Correlations
Abbas et al. 14 reported angiographic findings in 61 patients with non‐ST elevation MI. They found that the circumflex artery was threefold more likely to be the site of MI without ST segment elevation than either of the other major vessels. Patients with previous coronary bypass surgery were four times as likely to present with non‐ST elevation MI. The authors comment that limiting diagnosis to ST elevation therefore excludes a high‐risk group. They additionally note that “Despite the delay in revascularization and the absence of ST elevation, patients who had non‐ST elevation MI and underwent emergency revascularization had similar procedural outcomes, in‐hospital events and 6‐month outcomes in this analysis.” (as compared with the ST elevation group.)
Choice of therapy: The notion that the non‐ST elevation MI differed in some essential quality from the ST‐elevation variety raised the question of appropriate therapy for the former group.
A large series of well‐controlled studies comparing conservative with invasive therapy in the setting of non‐STEMI has by now settled the question of appropriate treatment. A study of 1635 consecutive patients by Scull et al., 15 the FRISC study, 16 the RITA trial, 17 the VINO study 18 a multicenter Holland/UK/U.S. study, 19 and a large‐scale multicenter U.S. study 20 all recorded significant benefit from early percutaneous intervention as compared with conservative management in patients with non‐STEMI. The term “early” used in all these studies, had varying significance. In the RITA trial, 17 patients were included within 72 hours of the onset of symptoms. In the FRISC I I study, 16 48 hours was the acceptable interval between onset of symptoms and intervention, while in the VINO project 18 “first day angiography” was defined as the time limit for intervention. In the study cited in reference 19 by Ronner et al. the time of maximum benefit with intervention was defined as one day, while in the study by Bach and coworkers 20 patients were assigned to invasive therapy 4 to 48 hours after randomization. In brief, invasive study and treatment has been established as appropriate and indicated therapy for non‐STEMI Timing of intervention in all these studies exceeded the “golden 90 minute” rule which raises an important question. Does this particular rule apply to the non‐STEMI set? The question remains moot for the very good reason that to date no study has addressed this problem. Thus the terms “urgent” or “emergency” may be applied with equal justification to intervention in the non‐STEMI set at this time. Further elucidation is needed.
Critique of the GISSI and ISIS2 Conclusions Relative to ST Depression Infarcts
Lee and colleagues 10 point out several obvious sources of error in both studies. Their comments are well worth quoting. “First the number of patients with ST depression who received therapy was relatively small in both trials (224 patients in GISSI and 571 in ISIS‐2). The confidence intervals for mortality reduction would therefore be expected to be wide in these patients. Indeed this was the case in the ISIS‐2 trial with an odds ratio for mortality reduction of 1.01 (95% confidence interval 0.75–1.36). Second, in patients with ST depression, the criterion for the administration of thrombolytic therapy was based on clinical suspicion only and not on ECG changes. This would almost certainly mean that a large number of patients who received thrombolytic therapy in these trials did not in fact suffer an infarction.”
In the ISIS‐2 study, patients were included who entered the hospital up to 24 hours after onset of symptoms with a median time to admission of 5 hours. ECG abnormality was not a requirement for inclusion. Given the frequently transient nature of ST deviation (1, 2, and 3) it is certain that many of the patients in the ISIS2 study must have manifested ST elevation at some earlier time in the course of the disease and were hence misclassified. (This is a major and obvious source of error: it is surprising that it has not been previously remarked.)
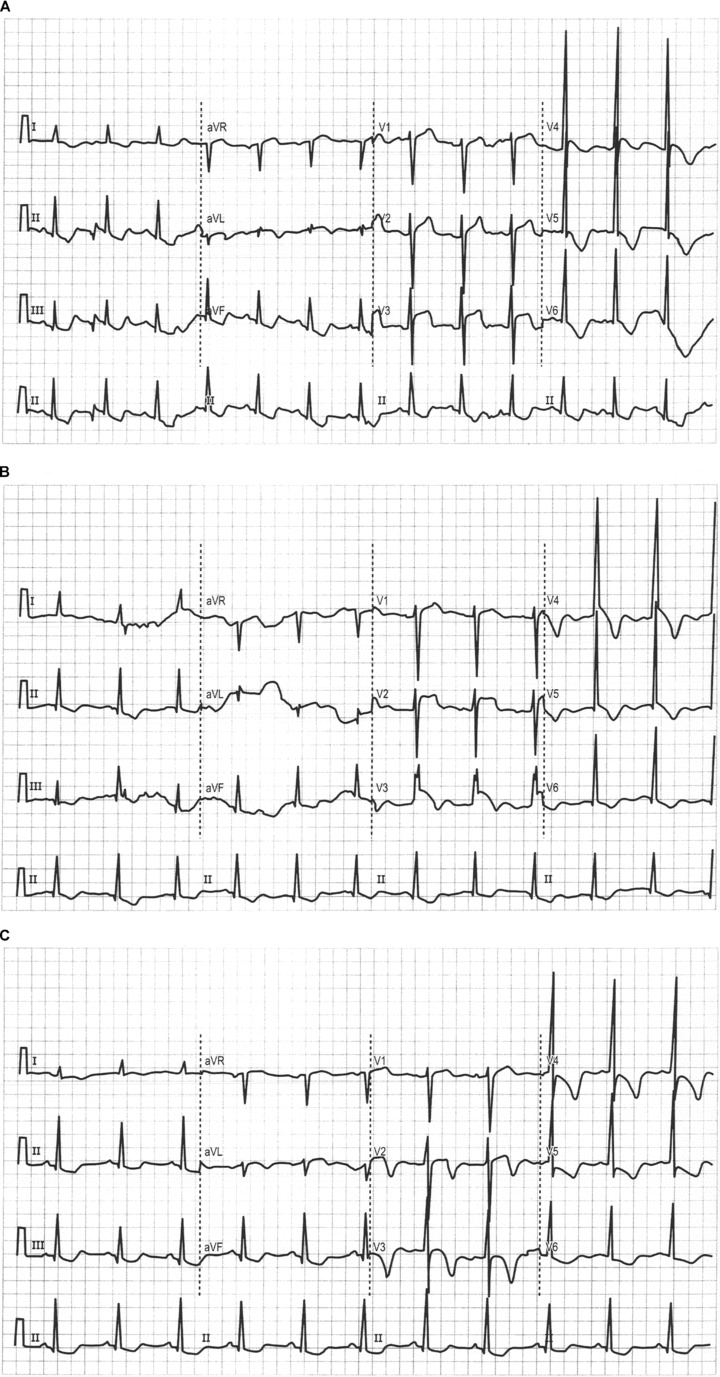
Figure 1.

Tracing recorded early in the course of a myocardial infarct. ST segment changed from depression to elevation in 18 heartbeats: ST elevation then resolved in six beats. (Continuous tracing.)
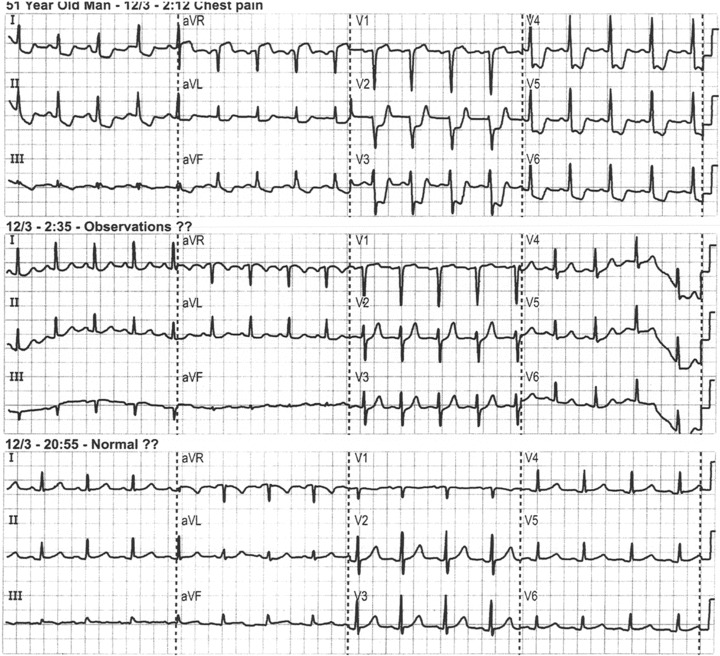
Figure 2.
(A) ECG recorded at 14:45 in a suspected MI. (B) Second tracing 15 minutes later recording further striking ST elevation of ST segments with typical convex pattern of infarction. (C) Third tracing recorded 6 minutes later with complete resolution of ST elevation. This would now be classed as a “non‐STEMI.”
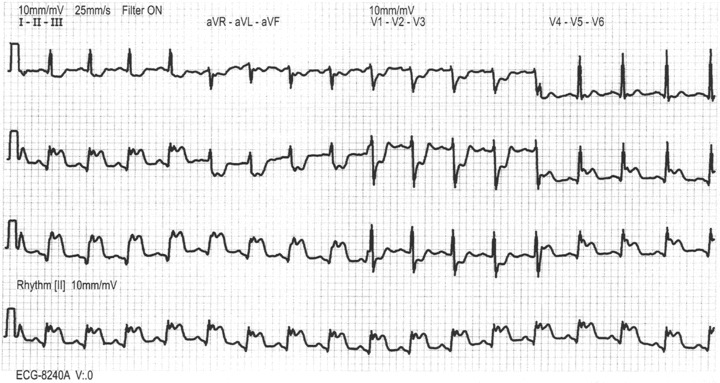
Figure 3.
Series of three tracings recorded at 2:12, 2:35, and 2:55 with complete resolution of profound ST depression and emergence of a normal ECG. An MI was in progress.
It is also striking that in the GISSI trial there was no benefit from thrombolytic therapy in inferior or lateral myocardial infarcts or in patients with previous infarcts! The significance figures for all these categories were the same as for those in the “ST depression” category. To imagine that this entire subset of myocardial infarcts differed in some essential character from anterior infarcts would defy logic.
Transient Nature of STT Deformity
Figure 1 is a continuous ECG recorded in the early stage of a myocardial infarct. The striking ST elevation persisted for five beats and resolved with progressive inversion of the T wave: an infarct was amply confirmed subsequently. Figures. 2(A–C) illustrates much the same phenomenon with appearance of typical ST elevation within 15 minutes and complete disappearance within another 6 minutes. In Figure 3 ST depression of as much as 6 millimeters resolved completely in 23 minutes leaving a completely normal ECG in the presence of a documented MI. It is absolutely predictable that in studies like ISIS 1 and 2 and GISSI, many of the infarcts studied within 24 hours—the only time‐criterion for entry—did in fact manifest ST deviation at some time previously, that is, elevation or depression that had resolved by the time the subject was studied.
Basic Conceptual Error
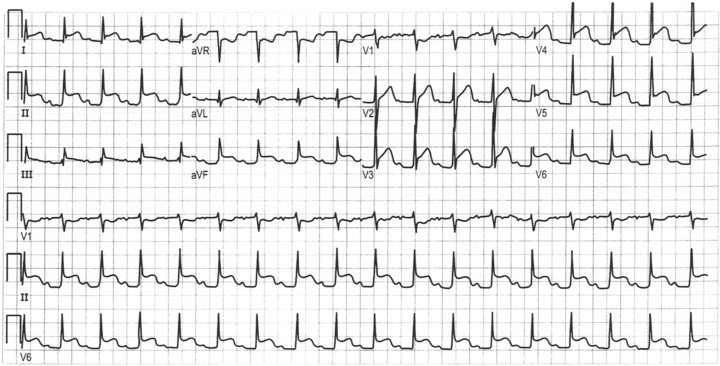
Finally, and more fundamentally, the STEMI and non‐STEMI differentiation ignores one of the basic tents of electrocardiography, that is, that any deflection will produce a reciprocal image 180 degrees removed, on the opposite aspect of the field. (Contemplation of V1 and V6 in the setting of bundle branch block or of ventricular hypertrophy should make this concept abundantly clear.) In simple terms, during myocardial infarction, ST elevation or depression are in fact identical entities, that is, a result of an injury current viewed from opposite aspects of the electric field of the heart (Fig. 4). As an extreme example, even the epicardial injury current produces a negative ST deviation in aVR (Fig. 5) and would certainly produce the same negative deflection in any other leads recorded in the superior and rightward aspects of the electrocardiographic field.
Figure 4.
Acute inferior myocardial infarct with posterior‐wall involvement. The reciprocal ST deviations are obviously equivalent reflections of the same event.
Figure 5.
Tracing recorded in the setting of well‐documented pericarditis. Note reciprocal ST depression in aVR.
This is not a new observation. Prystowsky in Topol 21 states that “Reciprocal ST depression is observed in most patients with inferior infarcts and in approximately 70% of patients with anterior infacts.” Surawicz 22 makes the point even clearer when he comments “Moreover it appears that new ST segment depression may be present in some patients with a diagnosis of non‐STEMI which requires the presence of ST elevation in some leads on the opposite side of the electrical field.”
In the simplest terms ST depression and ST elevation during MI are equal and opposite manifestations of an injury current with identical significance. One or the other may appear in the relatively limited field of the 12‐lead ECG, but if the entire cardiac field were recorded the reciprocal image of each would inevitably appear.
Comment: The STE/non‐STE dichotomy is so widely accepted that it may seem surprising to find that it has no basis in pathology, clinical correlates, or therapeutic implications. To put all this in perspective, however, one need only recall the imaginary distinction between Q and non‐Q infarcts that filled medical texts and journals for some 30 years before it was shown to be baseless. Non‐Q wave infarcts were alleged on all hands to be “subendocardial” and, when that misconception had been corrected, they were described as “unstable.” Both notions have been dispelled, 23 , 24 , 25 , 26 but the example is very much to the point here.
What may be termed “electrocardiographic naivete” and a tendency to rush to publication on the basis of a relatively simple comparison seem to have formed the basis of the torrent of observations in the field. In concrete terms, the alleged distinction has almost certainly done real harm as many cardiologists must have been led into treating non‐STEMI's as something other than what they really are, infarcts that do not happen to project a positive injury current on some part of the limited electric field recorded by standard ECG leads.
Finally, the division of myocardial infarcts into “ST elevation” and “non‐ST elevation” subsets fails the ultimate pragmatic test. There is now universal agreement that both entities should be subjected to invasive intervention although the optimal time limits for benefit in the latter group have not been studied and hence have not been defined. The distinction between the two electrocardiographic categories, in addition to being invalid, does not serve any useful purpose, and in the setting of older patients, patients with circumflex lesions and patients with recurrent infarcts, it may be dangerous.
CONCLUSIONS
All available data reveal that there is no pathologic difference between STEMI and non‐STEMI infarcts. Since the pathology is essentially identical in the two subsets, there is no reason to suppose that treatment or prognosis should differ.
In fact, the clinical implications of the two subsets are similar in terms of acute and long‐term prognosis. Invasive intervention is indicated in both categories although the precise time/benefit relation in the non‐STEMI has not yet been definitively studied. The ST elevation of documented infarcts is frequently so transient it disappears in minutes, making this an irrational basis for classification and comparison.
Finally, the direction of ST deviation is not a valid means for differentiation since any deviation represents nothing more than a reciprocal change in electrically opposed leads. Both ST elevation and depression will appear in every case if the entire cardiac field is recorded.
The non‐STEMI subset includes many older patients, patients with previous MIs and patients with circumflex lesions, a high‐risk group that should not be denied the benefits of maximal therapy, including acute intervention. The entire concept of STEMI/non‐STEMI differentiation is baseless and has probably caused harm: it should be discarded.
REFERENCES
- 1. Blumentahl R, Kleinschmidt K, Ashen M, et al Focus on the management of acute coronary syndrome: What's new and what's to come. Advanced Studies Med, Johns Hopkins Univ 2006;6:5475–5500. [Google Scholar]
- 2. Herrman H, Henry T. Optimizing reperfusion outcomes in STEMI. Am Heart J 2006;151(Supp1. 6):54–539. [Google Scholar]
- 3. Alexander KP, Newby LK, Cannon CP, et al Acute coronary care in the elderly, Part 1: Non‐S‐segment elevation acute coronary syndromes: A scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: In collaboration with the section of geriatric cardiology. Circulation 2007;115:2549–3569. [DOI] [PubMed] [Google Scholar]
- 4. Kelbak H, Terkelsen C, Hekquist S, et al Randomized comparison of distal protection versus conventional treatment in primary percutaneous coronary intervention: The ST‐elevation myocardial infarction trial. J Am Coll Cardiol 2008;51:899–905. [DOI] [PubMed] [Google Scholar]
- 5. Antman EM, Aube DT, Anbe D, et al ACC/AHA guidelines for the management of patients with ST elevation myocardial infarction. Circulation 2004;44:671–719. [DOI] [PubMed] [Google Scholar]
- 6. Gruppo Italiano per lo studio della streptokinase nell’infarcto miocardio (GISSI) . Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet 1986;397–402. [PubMed] [Google Scholar]
- 7. ISIS‐2:second collaborative study of infarct survival, collaborative group randomised trial of intravenous sreptokinase, oral aspirin, both, or neither, among 17187 cases of suspected acute myocardial infarction. Lancet 1988;13:349–360. [PubMed] [Google Scholar]
- 8. Raunio H, Rissanen V, Rompannen T, et al Changes in the QRS complex and ST segment in transmural and subendocardial infarctions: A clinicopathologic study. Am Heart J 1998;2:176–184. [DOI] [PubMed] [Google Scholar]
- 9. Montalescot G, Dallongeville J, Von Belle E, et al STEMI and NSTEMI: Are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (The Opera Registry). Eur Heart J 2007;28:1409–1417. [DOI] [PubMed] [Google Scholar]
- 10. Lee HS, Cross S, Rawles J, et al Patients with suspected myocardial infarction who present with ST depression. Lancet 1993;342:1204–1212. [DOI] [PubMed] [Google Scholar]
- 11. Kuch B, Von Scheldt W, Kling B, et al Characteristics and outcome of patients with acute myocardial infarction according to presenting electrocardiogram (from the MONICA/KORA Augsburg myocardial infarction registry). Am J Cardiol 2007;100:1056–1060. [DOI] [PubMed] [Google Scholar]
- 12. Pitta S, Grzybowski M, Welch R, et al S‐T segment depression in the initial electrocardiogram in acute myocardial infarction‐ prognostic significance and its effect on short‐term mortality: A report from the National Registry of Myocardial Infarction (NRMI‐1,2,3). Am J Cardiol 2005;95:843–848. [DOI] [PubMed] [Google Scholar]
- 13. Menown IBA, MacKenzie G, Adgey AAJ. Optimizing the initial 12‐lead electrocardiographic diagnosis of acute myocardial infarction. Eur Heart J 2000;21:275–283. [DOI] [PubMed] [Google Scholar]
- 14. Abbas A, Boura J, Brewington S, et al Acute angiographic analysis of non‐ST segment elevation acute myocardial infarction. Am J Cardiol 2004;94:907–909. [DOI] [PubMed] [Google Scholar]
- 15. Scull G, Martin J, Weaver D, et al Early angiography versus conservative treatment in patients with non‐ST elevation acute myocardial infarction. J Am Coll Cardiol 2000;35:895–902. [DOI] [PubMed] [Google Scholar]
- 16. FRISC‐II investigators . Fragmin and fast revascularization during instability in coronary artery disease (FRISC II) investigators. Invasive compared with non‐invasive treatment in unstable coronary‐artery disease: FRISC II prospective randomized multicenter study. Lancet 1999;354:708–714. [PubMed] [Google Scholar]
- 17. K, Poole‐Wilson PA, Henderson RA, Clayton DA, et al Interventional versus conservative treatment for patients with unstable angina or non‐ST elevation myocardial infarction: The British Foundation RITA 3 randomized trial. Lancet 2002;360:743–751. [DOI] [PubMed] [Google Scholar]
- 18. Spacek R, Widimsky P, Straka E, et al Value of first day angiography/angioplasty in evolving non‐ST segment elevation myocardial infarction: An open multicenter randomized trial. Eur Heart J 2002;23:230–238. [DOI] [PubMed] [Google Scholar]
- 19. Ronner E, Boersma E, Akkerhuiis KM, et al Patients with acute coronary syndromes without persistent ST elevation undergoing percutaneous coronary intervention benefit most from early intervention with protection by a glycoprotein IIb/IIIa receptor. Eur Heart J 2002;23:239–246. [DOI] [PubMed] [Google Scholar]
- 20. Bach R, Cannon C, Weintraub W, et al The effect of routine, early invasive management on outcome for elderly patients with non‐ST elevation acute coronary syndromes. Ann Int Med 2004;141:186–195. [DOI] [PubMed] [Google Scholar]
- 21. Prystowski E. In Topol E, Textbook of cardiovascular medicine,1573–4 Lippincott‐Raven, Philadelphia‐New York, 2002.
- 22. Surawicz B. In Chou T‐C, Electrocardiography in clinical practice Elsevier‐Saunders, 2008, p. 206.
- 23. Phibbs B. “Transmural” versus “subendocardial” infarcts, an electrocardiographic myth. J Am Coll Cardiol 1983;1:561–564. [DOI] [PubMed] [Google Scholar]
- 24. Spodick D. Q wave infarction versus S‐T‐T infarction: Non‐specificity of electrocardiographic criteria for differentiating transmural and nontransmural lesions. Am J Cardiol 1983;51:914–917. [DOI] [PubMed] [Google Scholar]
- 25. Phibbs B, Marcus F, Moss A, et al Q wave versus non‐Q wave myocardial infarction: A meaningless distinction. J Am Coll Cardiol 2000;2:576–582. [DOI] [PubMed] [Google Scholar]
- 26. Phibbs B. The Q wave infarct: Phenomenon or chimera? Eur Heart J 2001;22:980–982. [DOI] [PubMed] [Google Scholar]


