Abstract
Background: Interatrial block (IAB; P wave ≥ 110 ms) is highly prevalent and associated with atrial tachyarrhythmias, left atrial electromechanical dysfunction and is a potential risk for embolism. Investigators have often used different parameters for P‐wave duration to define IAB, and this causes confusion further adding to clinician ignorance of IAB. We therefore appraised the mode P‐wave duration in IAB and evaluated the sensitivity and specificity of using previously used durations.
Methods: We prospectively evaluated 225 electrocardiograms (ECGs) of patients at a tertiary care general hospital for P‐wave duration. Of these, 49 were excluded because of severe motion artifact, errors in lead placement, absence of adequate patient identification, and atrial flutter or fibrillation. Mean, standard error of mean (SEM), standard deviation (SD), mode P‐wave duration, specificity, and sensitivity were calculated of the remaining 176 ECGs.
Results: From the sample (N = 176; ages 15–95 years; mean ± SD = 69.15 ± 16.53 years, female 50.3%), measured P‐wave durations ranged from 50 ms to 230 ms (mean ± SD = 113.75 ± 30.56 ms, SEM 2.30 ms). 96 patients (54.55%) showed IAB (P wave ≥ 110 ms) with the mode P‐wave duration being 120 ms. Sensitivity and specificity of using P wave ≥ 110 ms is 100% and 88.9%, respectively (accuracy 94.31%), while P wave ≥130 ms yielded 64% and 100%, respectively (accuracy 82.38%).
Conclusions: Mode P‐wave duration in IAB is 120 ms, and thus, for all practical reasons, it may be used to clinically diagnose IAB using ECGs recorded at the bedside at 25 mm/s with 10 mm/mV standardization.
Keywords: interatrial block, P‐wave duration, electrocardiogram
BACKGROUND
Normal P‐wave duration has been defined by the World Health Organization (WHO) International Society and Federation of Cardiology Task Force 1 as <110 ms on the electrocardiogram (ECG) and denotes the normal transit time of electrical impulse generated in right atrium to conduct to left atrium (LA) resulting in atrial depolarization and its subsequent contraction. 2 Hence, P‐wave prolongation (P wave ≥ 110 ms) implies interatrial conduction delay and has been so described by Bayes de Luna as interatrial block (IAB). 3 , 4
IAB has been shown to be >40% prevalent among all patients in sinus rhythm in two separate general hospital populations. 5 , 6 It is also a strong predictor of atrial tachyarrhythmias, especially atrial fibrillation 7 , 8 and is associated with LA enlargement 9 and electromechanical dysfunction besides being a potential risk factor for embolism. 10 Despite this, much is yet to be studied about IAB even with regard to its fundamentals. Moreover, IAB investigators have often used different parameters for P‐wave duration to define IAB. For example, Goyal and Spodick used P‐wave durations of ≥120 ms 10 and Montereggi used P‐wave durations ≥130 ms 11 , while others cited P wave ≥ 140 ms 12 as their criteria for definition. This along with overwhelming ignorance of its existence, forces IAB to be underappreciated and greatly overlooked. 13 Heavily contributory is also the common mistake of sole reliance on lead II rather than on all leads. We evaluated the mode duration of P waves in IAB and the specificity and sensitivity of using previously used durations.
METHODS
We prospectively evaluated 225 consecutive 12‐lead ECGs at 25 mm/s with 10 mm/mV standardization in a tertiary care teaching hospital. Patients were aged 15–98 years (52.44% female) and had been admitted to the nontelemetry general medical floors for nonacute presentations. Out of these, 49 ECGs were excluded for severe motion artifact, errors in lead placement, absence of adequate patient identification, junctional rhythms, and atrial flutter or fibrillation. P waves on the remaining 176 ECGs, which were included in this study, were then measured under 10‐fold calibrated magnification for the greatest duration on each lead. The onset of the P wave was defined as the junction between the T–P iso‐electric line and the beginning of the P deflection and the offset as the junction between the end of the P deflection and the PR segment. Mean, standard error of mean (SEM), standard deviation (SD), mode P‐wave duration, specificity, and sensitivity were calculated.
RESULTS
From the sample (N = 176), patients were of ages 15–95 years (mean age ± SD = 69.15 ± 16.53 years) with a slight predominance toward females (50.3%). Measured P‐wave durations ranged from 50 ms to 230 ms (mean ± SD = 113.75 ± 30.56 ms, SEM 2.30 ms) (Fig. 1). Ninety‐six ECGs (54.55%) showed IAB (P wave ≥ 110 ms) with the mode P‐wave duration noted to be 120 ms (Fig. 2, Table 1).
Figure 1.
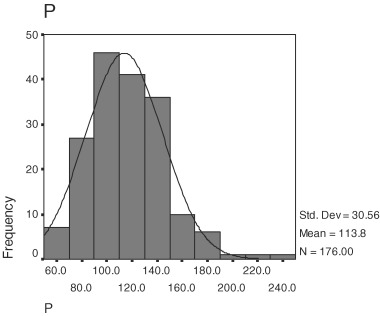
P‐wave durations in all valid ECGs (N = 176).
Figure 2.
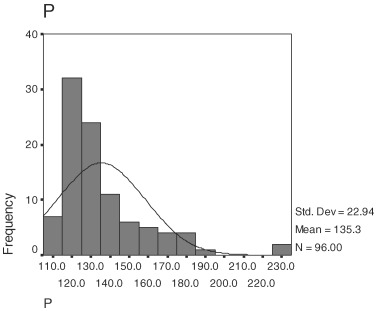
P‐wave durations in patients with IAB (N = 96).
Table 1.
Frequency Table for P‐Wave Durations in Patients with IAB (N = 96)
| P Wave (ms) | Frequency | Percent | Valid Percent | Cumulative Percent |
|---|---|---|---|---|
| 110 | 7 | 7.3 | 7.3 | 7.3 |
| 115 | 3 | 3.1 | 3.1 | 10.4 |
| 120 | 28 | 29.2 | 29.2 | 39.6 |
| 123 | 1 | 1.0 | 1.0 | 40.6 |
| 125 | 2 | 2.1 | 2.1 | 42.7 |
| 130 | 15 | 15.6 | 15.6 | 58.3 |
| 133 | 7 | 7.3 | 7.3 | 65.6 |
| 136 | 1 | 1.0 | 1.0 | 66.7 |
| 140 | 9 | 9.4 | 9.4 | 76.0 |
| 142 | 1 | 1.0 | 1.0 | 77.1 |
| 147 | 3 | 3.1 | 3.1 | 80.2 |
| 150 | 3 | 3.1 | 3.1 | 83.3 |
| 155 | 1 | 1.0 | 1.0 | 84.4 |
| 160 | 4 | 4.2 | 4.2 | 88.5 |
| 165 | 1 | 1.0 | 1.0 | 89.6 |
| 167 | 1 | 1.0 | 1.0 | 90.6 |
| 170 | 2 | 2.1 | 2.1 | 92.7 |
| 180 | 4 | 4.2 | 4.2 | 96.9 |
| 191 | 1 | 1.0 | 1.0 | 97.9 |
| 227 | 1 | 1.0 | 1.0 | 99.0 |
| 230 | 1 | 1.0 | 1.0 | 100.0 |
| Total | 96 | 100.0 | 100.0 |
DISCUSSION
Although IAB, or more appropriately, interatrial delay is highly prevalent 5 , 6 in the general hospital population and is associated with sequelae, 7 , 8 , 9 , 10 it is often underappreciated and often incorrectly deemed insignificant. 13 Lack of emphasis in cardiology textbooks and absence of appropriate management strategies by the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, however, do not justify clinician ignorance. Moreover, lack of standardization in use of P‐wave duration as its diagnostic criterion only causes further confusion and curbs our understanding of IAB. According to the WHO's standardized definition of normal P‐wave duration (<110 ms), 1 our study appraised prolonged P‐wave durations in IAB ranging from 110 ms to 230 ms and shows that the mode P‐wave duration in IAB diagnosed from bedside ECGs is indeed 120 ms (Fig. 2, Table 1).
It is, however, acknowledged that even the widest P wave taken from a tracing of a standard bedside‐ECG cannot be accurately established with manual measurement. Neither the true onset nor the offset of the P wave can be so determined even under magnification. Furthermore, P‐wave durations measured in this manner rarely precisely correlate with the actual total atrial activation time recorded during atrial mapping evaluations. However, the purpose of this investigation was to generate a common basis of clinically diagnosing IAB at the bedside. Altering the sweep speed or gain of the ECG in an attempt to achieve optimal results would therefore not be practical as a clinical tool and certainly not facilitate ease of diagnosis in the hands of the clinician, where IAB diagnosis probably is most important.
In this study sample, 10 patients would have had the diagnosis of IAB missed if P wave ≥120 ms was used (Table 1) as a diagnostic criterion. Therefore, IAB would be diagnosed in 86 patients (48.86%) compared with 96 patients (54.54%) if the WHO's definition of P‐wave ≥110 ms is utilized. While it is strictly not our purpose to challenge this guideline nor add to a diagnostic criteria, it is important to note that on most standardized ECG tracings, 10 ms on 25 mm/s recordings equals one‐quarter mm. Therefore, measuring P‐wave durations in 40‐ms multiples (1 mm on the ECG), for example, could be more practical when P wave ≥120 ms (3 mm on the ECG) is used for IAB diagnosis at the bedside. As such, sensitivity and specificity of using P waves ≥110 ms on bedside‐ECGs for IAB diagnosis is 100% and 88.9%, respectively (accuracy 94.31%), while with P waves ≥130 ms, the yield is 64% and 100%, respectively (accuracy 82.38%) (Table 2).
Table 2.
Optimal P‐Wave Duration for Clinical Diagnosis of IAB at the Bedside
| Duration | Sensitivity | Specificity | Accuracy |
|---|---|---|---|
| P wave ≥ 110 ms | 100% | 88.9% | 94.31% |
| P wave ≥ 120 ms | Mode (100%) | ||
| P wave ≥ 130 ms | 64% | 100% | 82.38% |
| P wave ≥ 140 ms | 37.2% | 100% | 69.32% |
CONCLUSIONS
The mode P‐wave duration in IAB is 120 ms (Table 1, Fig. 2). Since this duration represents 3 mm on the ECG recorded at 25 mm/s with 10 mm/mV standardization, for all practical reasons, P wave ≥120 ms can be used for optimal diagnosis of IAB. Given the high prevalence 5 , 6 and significant associations of IAB, 7 , 8 , 9 , 10 standardizing software to include P‐wave durations in computer‐generated ECG readings could perhaps be a useful tool in generating awareness and aiding in clinician diagnosis of IAB.
REFERENCES
- 1. Willems JL, Robles de Medina EO, Bernard R, et al Criteria for intraventricular conduction disturbances and pre‐excitation. World Health Organizational/International Society and Federation of Cardiology Task Force Ad hoc. J Am Coll Cardiol 1985;5:1261–1275. [DOI] [PubMed] [Google Scholar]
- 2. Chung EK. Anatomy, electrophysiology and hemodynamics. Principles of Cardiac Arrhythmias. Baltimore , Williams and Wilkins Co.,1973, pp.14. [Google Scholar]
- 3. Bayes de Luna A. Electrocardiographic alterations due to atrial pathology. Clinical Electrocardiography: A Textbook. New York , Futura Company Inc.,1998, pp.69. [Google Scholar]
- 4. Cohen J, Scherf D. Complete interatrial and intra‐atrial block (atrial dissociation). Am Heart J 1965;70:23–24. [DOI] [PubMed] [Google Scholar]
- 5. Asad N, Spodick DH. Prevalence of interatrial block in a general hospital population. Am J Cardiol 2003;91:609–610. [DOI] [PubMed] [Google Scholar]
- 6. Jairath UC, Spodick DH. Exceptional prevalence of interatrial block in a general hospital population. Clin Cardiol 2001;24:548–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agarwal YK, Aronow WS, Levy JA, et al Association of interatrial block with the development of atrial fibrillation. Am J Cardiol 2003;91:882. [DOI] [PubMed] [Google Scholar]
- 8. Bayes de Luna A, Cladellas M, Cafferas F, et al Interatrial blocks: Their relationship with atrial tachyarrhythmias. In Levy S, (ed.): Cardiac Arrhythmias. New York , Futura, 1984, pp.217–229. [Google Scholar]
- 9. Velury V, Spodick DH. Axial correlates of P‐VI in left atrial enlargement and relation to interatrial block. Am J Cardiol 1994;73:998–999. [DOI] [PubMed] [Google Scholar]
- 10. Goyal SB, Spodick DH. Electromechanical dysfunction of the left atrium associated with interatrial block. Am Heart J 2001;142:823–827. [DOI] [PubMed] [Google Scholar]
- 11. Montereggi A. Marconi P. Olivotto I, et al Signal‐averaged P‐wave duration and risk of paroxysmal atrial fibrillation in hyperthyroidism. Am J Cardiol 1996;77:266–269. [DOI] [PubMed] [Google Scholar]
- 12. Ascione R, Caputo M, Calori G, et al Predictors of atrial fibrillation after conventional and beating heart coronary surgery. Circulation 2000;102:1530–1535. [DOI] [PubMed] [Google Scholar]
- 13. Spodick DH. Unappreciated prevalence of interatrial block and associated consequences: A poorly perceived pandemic. Mayo Clin Proc 2004;79:668–670. [DOI] [PubMed] [Google Scholar]


