Aberrant ventricular complexes of the type generally recognized as indicating bundle‐branch block were first produced by Eppinger and Rothberger, 3 , 4 by the experimental division of the right branch of the His bundle. Eppinger and Stoerk 5 observed similar curves in five patients, and at autopsy demonstrated division of the right branch of the His bundle in two of these. The work of Cohn and Lewis, 2 and of Carter 1 indicated, however, that gross lesions of the main branches are not invariably found at autopsy in patients who during life present this type of electrocardiogram.
Following these original contributions to the subject, bundle‐branch block curves have been observed as a temporary sign during infections, congestive failure, coronary thrombosis, tachycardias, and various toxic states. In most if not in all of the reported cases the abnormal curves occurred in patients with definite structural heart disease, or with extreme tachycardia. The references already cited 1 , 2 indicate that the type of electrocardiogram under discussion may be obtained in the absence of gross division of a bundle branch.
Experimentally, bundle‐branch block curves may be obtained in normal hearts by causing an impulse to enter one bundle branch later than the other. The same result would be produced should the impulse travel through the bundle branches at different speeds or by an aberrant course. That such a mechanism may occur in human beings with normal hearts seems likely from a study of the cases described in the present paper, the presumption being that vagal stimulation may, in certain individuals, give rise to aberrant ventricular complexes.
We have observed the occurrence of bundle‐branch block curves in healthy young adults and children with apparently normal hearts. The curves may be typically those of complete right or left bundle‐branch block, or of intermediate or lesser grades of aberration. Spontaneously, or following release of vagal tone by exercise or atropinization, there is a transition from aberrant ventricular complexes to perfectly normal ones. Coincident with the change to normal ventricular complexes, the P‐R interval increases from an unusually short one (never greater than 0.1 second) to one of normal length, frequently almost doubling itself. In other words release of vagal tone is accompanied by a lengthening of the P‐R interval; this paradoxical vagal effect is of considerable interest; its mechanism is obscure. Another feature observed in these patients is the occurrence of paroxysmal tachycardia, or paroxysmal fibrillation or perhaps flutter.
The phenomena just mentioned have been present more or less consistently in all of our patients. The combination constitutes a type of rhythm, or mechanism, which has not yet been described as such; it is probably not rare. Considerable importance attaches to the recognition that bundle‐branch block curves do not always indicate organic heart disease. The case with which such cases may be recognized will be apparent from the description of our cases.
CASE REPORTS
Case 1. S.O.S., married, male, aged 35 years when first seen by us April 2, 1928.
Occupation. Physical director.
Chief complaint. Palpitation off and on for the past ten years.
Present history. His general health has always been excellent. Attacks of palpitation, which began ten years ago, are brought on by excitement or exertion, and once followed the drinking of one or two glasses of whiskey. During the attacks, which come on about once a week and last about half an hour, he is conscious of the heart beating rapidly and irregularly, and occasionally during these attacks he has listened to his own heart with a stethoscope, finding a grossly irregular rhythm. This has been confirmed by his physician. During the paroxysm he feels somewhat weak but continues his activity. He does wrestling, boxing, swimming and road work, running ten miles without any undue symptoms. A paroxysm of fibrillation once came on while he was swimming and ended while the swimming was continued. Less frequent attacks of a different type of palpitation occur in which the heart beats much faster and is regular except for occasional intermittence. Blood seems to rush to the head at such times. The attack is stopped by bending forward so that his head is low. Many examinations in the past fifteen years have failed to reveal any evidence of heart disease, though occasionally the heart was said to be irregular.
Active service in the army lasted from May, 1917 to August, 1919. The patient is of a “nervous,” introspective type.
Past history. Negative except for Neisserian infection seventeen years ago, mild influenza in 1918, and psoriasis one year ago.
Marital history. Married five years. Wife living and well, but has never been pregnant.
Physical examination. General condition excellent. Well developed and nourished, muscular, healthy athlete in the pink of condition. The entire examination was negative except that the tonsils were large and the tip of the spleen was just palpable. Heart. The cardiac impulse was felt in the fifth intercostal space 7.5 cm. to the left of the midsternal line. The left border of dulness was 8 cm. and the midclavicular line was 9.5 cm. to the left of the midsternal line. The heart rate was irregular, varying between 50 and 80 per minute, but there was a dominant rhythm. After exercise the heart accelerated moderately, but was normal in rate again in one to two minutes. The sounds were of good quality; the first apical sound was reduplicated; there were no murmurs. The pulse form and artery walls were normal. There was no arcus senilis. Blood pressure was 104 mm. mercury systolic, and 70 diastolic.
Roentgen ray report (“7 foot plate”). The heart shadow was rather round and wide acrosss the auricles, but was not “mitral shaped.” The transverse diameter was within normal limits. The supracardiac shadow was small. The aorta seemed narrowed in both antero‐posterior and oblique views. The measurements were as follows: to the right of the midsternum 5.9 cm., to the left 8.2, total transverse diameter 14.1, length 14.5, base 13.5, width of great vessels 5.2, and internal diameter of thorax 30.5.
The blood Wassermann reaction was negative.
Later notes. (1) April 23, 1928. Is taking quinidine sulphate in daily rations of grs. ix. There have been no more paroxysms of fibrillation.
(2) June 15, 1928. In perfect health. No more paroxysms. Is not taking quinidine.
(3) August 24, 1928. Except for one or two very short paroxysms of auricular fibrillation he has been in excellent health.
(4) October 1929. He has been in excellent health, and has done strenuous athletic work. Several attacks of paroxysmal tachycardia have occurred, but none of auricular fibrillation. Physical examination negative.
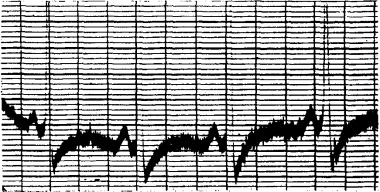
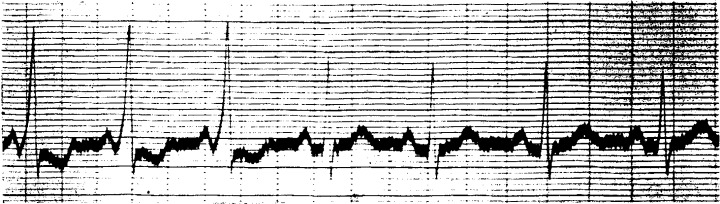
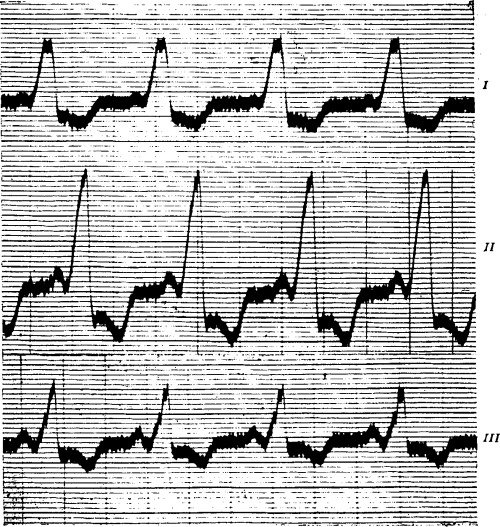
Electrocardiograms. Numerous electrocardiograms were taken. When the patient was at rest the usual finding was normal rhythm at a rate of about seventy, with slight sinus arrhythmia, and intraventricular block of the “right bundle‐branch type.” The QRS complexes were greater than 0.1 second in duration, with the T‐waves directed opposite to the chief deflection. The P‐waves were poorly marked, and the P‐R interval measured 0.10 second (Fig. 1). Exercise (running up and down four flights of stairs) produced a sino‐auricular tachycardia rate 140–120, with perfectly normal ventricular complexes throughout (Fig. 2). The P‐waves were now better marked, and the P‐R interval definitely longer (0.16 second). After a rest of twenty minutes the bundle‐branch block complexes had returned. Following the injection of atropine sulphate (gr. 1/30 subcutaneously) the ventricular complexes again became normal, and the P‐R interval measured 0.15 to 0.16 second (Fig. 3).
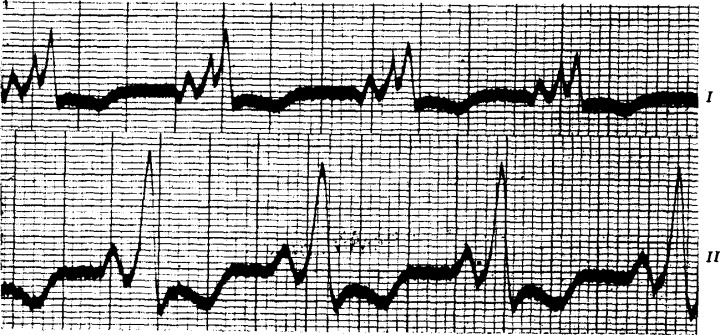
Figure 1.
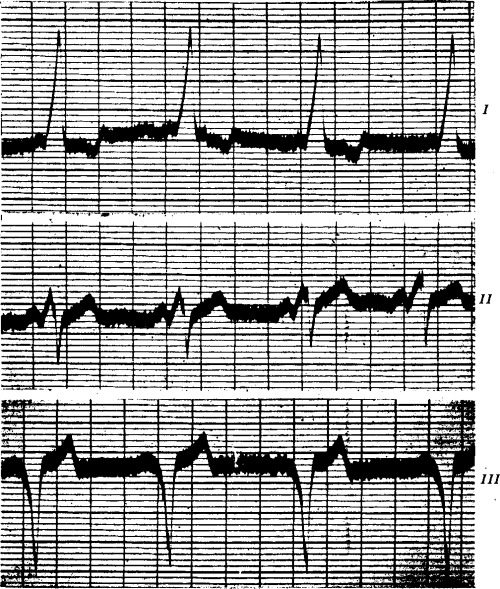
(Case I) Right bundle‐branch block. The P‐R interval is 0.1 second. The rate is 72. Time intervals for this and succeeding figures = 0.2 second. Horizontal lines cut off intervals of 10−4 volt.
Figure 2.
(Case I) Immediately after exercise (running up and down four flights of stairs). Sino‐auricular tachycardia, rate 140 to 120. The ventricular complexes are normal, the P‐waves are better marked, and the P‐R interval is 0.16 second.
Figure 3.
(Case I) One hour after the subcutaneous injection of 1/30 grain of atropine sulphate. The rate is 140, the ventricular complexes are normal, and the P‐R interval is 0.15 to 0.16 second.
The last electrocardiogram, taken in October 1929, showed the normal type of complexes which changed to right bundle‐branch block when pressure was exerted on the right vagus nerve.
(We are indebted to Dr. Hyman Morrison for the privilege of studying this case.)
Case II. D.C., single, male, aged 18 1/2 years when first seen by us March 20, 1928.
Occupation. College freshman.
Present history. His general health had always been excellent. Four years ago he had his first attack of rapid vigorous heart action with sudden onset and offset, lasting fifteen minutes. The heart was regular at a rate of about 160. This had recurred from 3 to 4 times a year since, coming irregularly every few weeks to months. The attacks usually came when he was quiet, except once when he was struck in the chest in a soccer game. He lay down when an attack occurred and it quickly passed off, never lasting more than one‐half hour. The last attack came three months ago while sitting at the edge of the swimming tank. A doctor who happened to be present stopped the attack by vagal pressure.
During the attacks of tachycardia there were slight dyspnea and an aching in the back of the neck. At other times there were no symptoms.
Past history and family history were irrelevant. He was not a blue baby.
Physical Examination, which showed a large and robust athlete, apparently in excellent health, was entirely negative. The maximum apex impulse of the heart was felt behind the fifth rib, 8 cm. to the left of the midsternal line. The left border of dulness was 7.5 cm. from the midsternum and the midclavicular line was 9 cm. to the left of the midsternal line. The sounds were of good quality, the first apical sound double. At the apex a slight systolic murmur was audible when the patient was recumbent. The blood pressure was 115‐120 mm. mercury systolic, and 60 diastolic. The heart rate was 68, and the response to exercise was good.
A teleroentgenogram (“7 foot plate”) of the heart was normal.
Basal metabolism was normal.
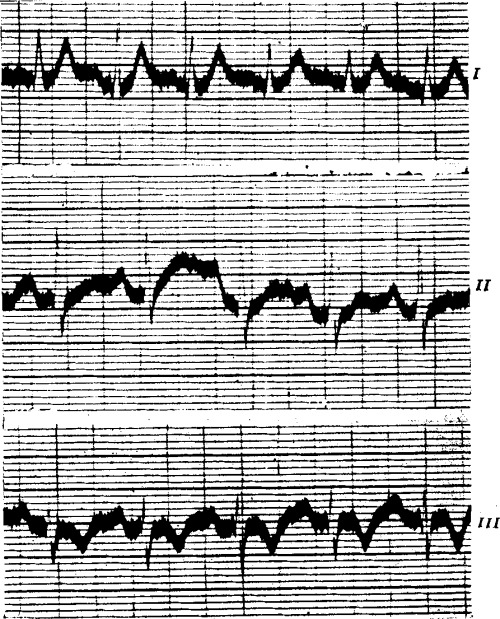
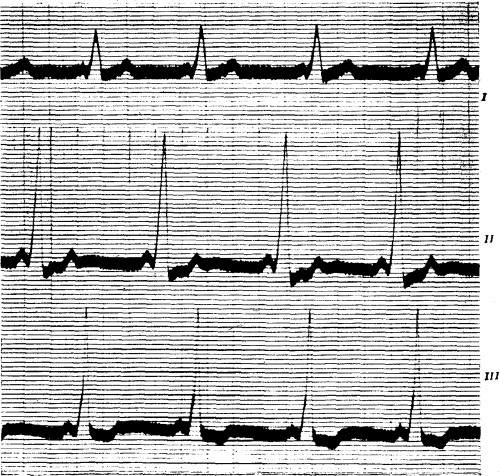
Electrocardiograms showed aberrant ventricular complexes (intraventricular block) and an unusually short P‐R interval (Fig. 4). After exercise the ventricular complexes assumed a normal physiological form and the P‐R interval became distinctly longer (Fig. 5).
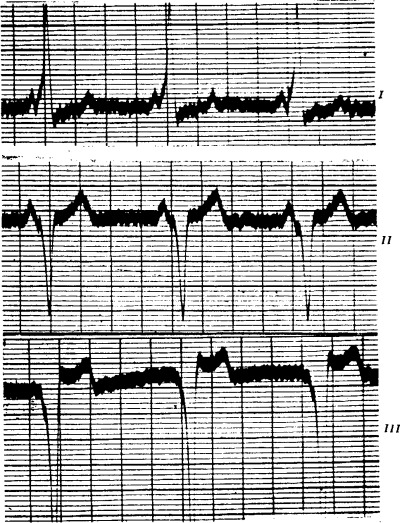
Figure 4.
(Case II) Intraventricular block. The P‐R interval is 0.1 second. Rate 96.
Figure 5.
(Case II) Immediately after exercise. The ventricular complexes are normal except for deformity of the S wave and S‐T interval by artefact (high resistance, resulting in over‐shooting). The T‐wave is upright. The P‐R interval is 0.15 second. Rate 96.
When last heard from in the fall of 1929 this young man was very well and active.
Case III. C.P.R., male, aged 21 years when first seen by us on June 29, 1927.
History. He complained of attacks of palpitation which had recurred ever since school days. The attacks had become more frequent so that he had one or two almost daily. They began suddenly without apparent cause, lasted from a few minutes to three hours, and stopped suddenly. Lying down or bending over usually stopped the attacks. He said that he had always been short‐winded, but that he had been quite well except for the palpitation. There was no rheumatic history.
Examination showed no abnormal signs and he looked plump and well. The blood pressure was 135 mm. mercury systolic and 80 mm. diastolic.
Radioscopy showed no enlargement.
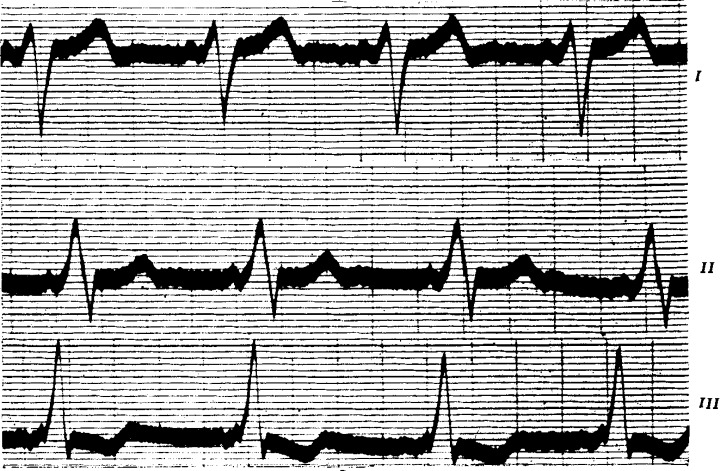
A routine electrocardiogram showed right bundle‐branch block, upright P‐waves in all leads, and a P‐R interval well under 0.1 second (Fig. 6).
Figure 6.
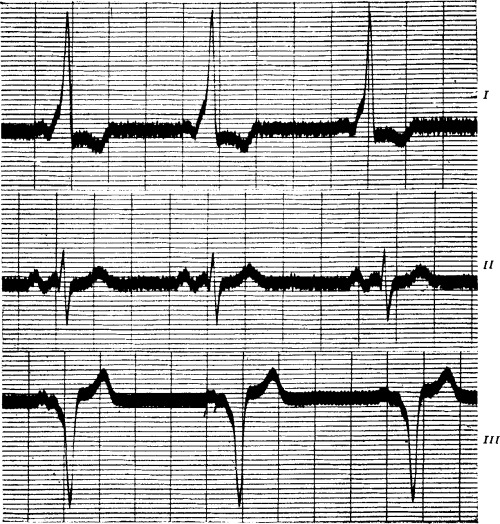
(Case III) Right bundle‐branch block. The P‐R interval is well under 0.1 second. The rate varies between 60 and 70.
On February 17, 1928 he was seen after a paroxysm of tachycardia lasting seven hours. Electrocardiograms now showed normal complexes (Fig. 7), with recurrent periods of the abnormal curve recorded in 1927. The P‐waves were identical when the QRS waves were normal and when they were of the type designated as indicating bundle‐branch block; the P‐R interval, however, was well under 0.1 second when bundle‐branch block curves were present, and almost 0.2 second when the QRS complexes were normal. (Fig. 7.)
Figure 7.
(Case III) After a paroxysm of tachycardia lasting seven hours. The ventricular complexes are normal, but occasionally there is reversion to the abnormal form. The P‐R interval is almost 0.2 second. The P‐waves are notched, and identical in Figs. 6 and 7.
On September 27, 1928, it was reported that his paroxysms were less frequent.
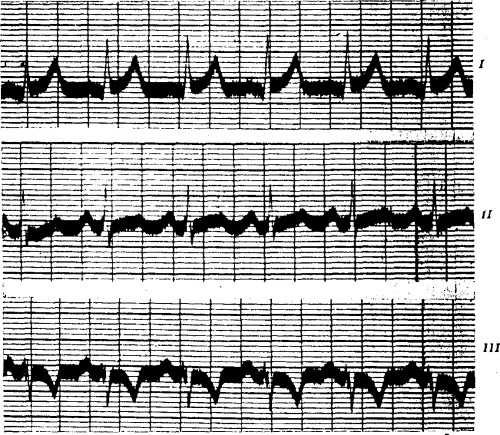
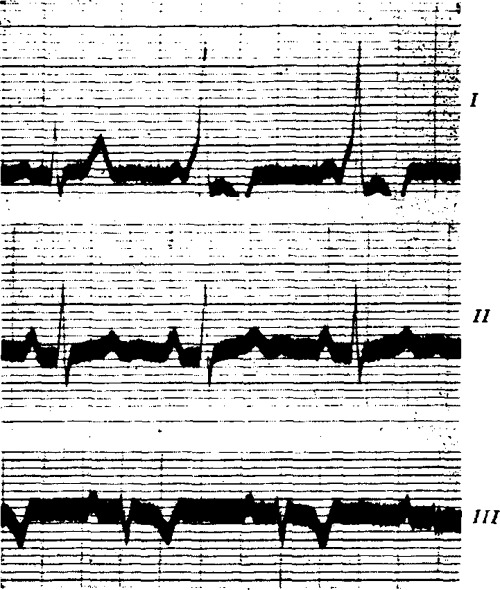
On the 30th of August, 1929, he was re‐examined. There had been only one paroxysm of tachycardia during the previous twelve months. The electrocardiogram was now a normal physiological one (Fig. 8).
Figure 8.
(Case III) Two years after Fig. 6 was taken. Normal physiological curves.
Case IV. C.A., male, aged 16 years when first seen by us on January 7, 1926. There was a history of occasional palpitation. The heart would suddenly become rapid, generally on exertion. The last bad attack was after playing football. There were no other symptoms, and no rheumatic history.
Examination revealed no abnormal signs. The heart rate was slightly rapid, with an irregularity which at first was thought to be a sinus arrhythmia. The blood pressure was 135 mm. mercury systolic, and 75 diastolic.
Radioscopy showed no enlargement.
Electrocardiograms. Two distinct forms of curve were obtained, one replacing the other spontaneously as shown on successive plates (Figs. 9, 10 and 11). Figure 10 shows normal physiological complexes in all leads, P‐R interval 0.15 second. Figure 11 shows a special form of complex with identical normal P‐waves, shortened P‐R interval (less than 0.1 second), and widened QRS complexes. The respective rates are much the same, the normal about 104, the abnormal about 108 a minute.
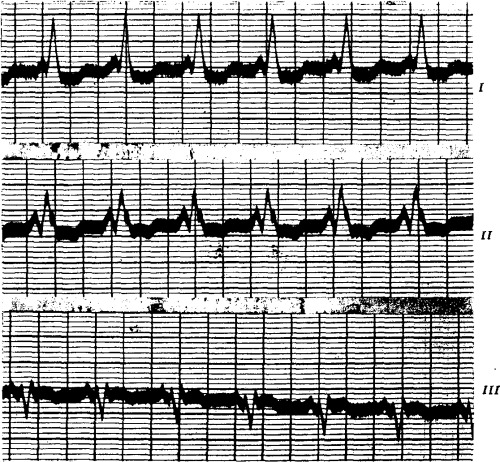
Figure 9.
(Case IV) Spontaneous reversion from bundle‐branch block curves to normal ones. The form of the P‐wave remains unaltered, but the P‐R interval changes from 0.09 second to 0.15 second.
Figure 10.
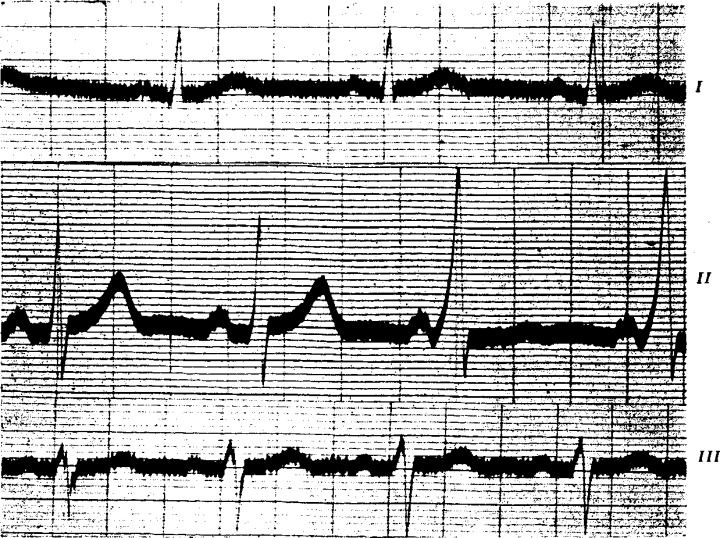
(Case IV) Normal physiological complexes. P‐R interval 0.15 second. In Lead II there is a transition to the abnormal form and short P‐R interval.
Figure 11.
(Case IV) Bundle‐branch block. The P‐R interval is less than 0.1 second. The P‐waves are identical in Figs. 10 and 11: note the peculiar notching of the P‐waves.
On January 20, 1926, the abnormal type of curve was constant, and simultaneous electrocardiogram and jugular and radial tracings showed a normal a.c.v.h. sequence (Figure 12).
Figure 12.
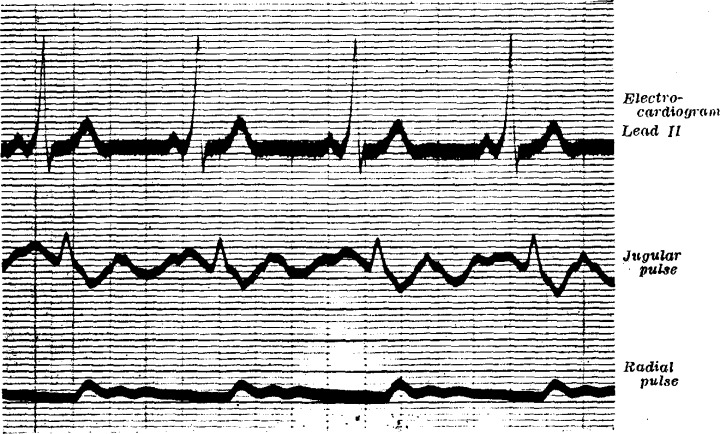
(Case IV) Simultaneous electrocardiogram and jugular and radial tracings. Bundle‐branch block curves are present. The a. c. v. h. sequence is normal.
On February 10, 1928, the normal type of electrocardiogram was constant.
On October 10, 1929, the patient was examined again. He was able to play football and other games, but occasionally the heart would race at a high rate (about 200 per minute) for a few minutes. This would occur generally on exertion but once it took place in church. The electrocardiogram was now of the abnormal type.
On December 12, 1929, records showed the heart alternately in and out of the abnormal rhythm during several minutes, then the normal rhythm ruled. He was still fit and well apart from occasional attacks of palpitation.
Case V. G.H.K., male, aged 23 years when first seen by us on July 2, 1929. He complained of palpitation and slight pain in the left axilla. Once while in bed the heart suddenly beat rapidly for a few minutes; similar attacks of palpitation occasionally occurred during the day. He played tennis and was not breathless on exertion. There was no rheumatic history.
Examination revealed no abnormal signs. The heart rate was 100 per minute. At this rate the blood pressure was 160 mm. mercury systolic, and 90 diastolic; at other times it was lower.
Radioscopy showed no cardiac enlargement.
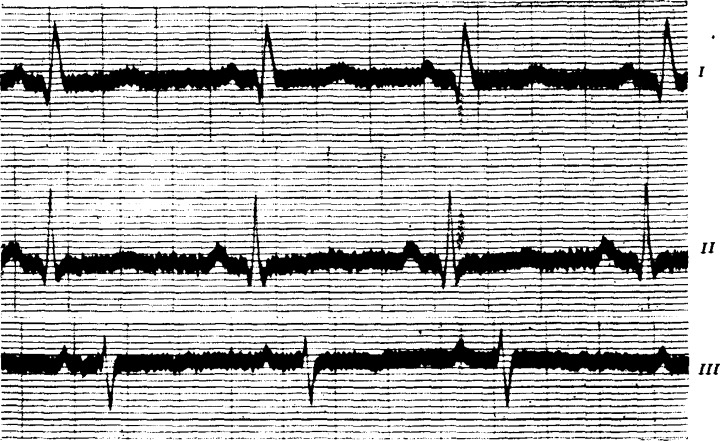
Electrocardiograms were first taken in May, 1929, by Dr. Donald Hall of Brighton, to whom we are indebted for permission to publish the case. Our record of July 2, 1929, is similar (Fig. 13). The P‐waves are normal and upright in all leads. The P‐R interval is well under 0.1 second. The QRS complexes are wide and notched, and the T‐waves are inverted in all leads.
Figure 13.
(Case V) Intraventricular block. The P‐waves are normal and upright in all leads. The P‐R interval is well under 0.1 second.
This man was advised to continue his work as a market gardener.
Case VI. H.R.L., male, aged 23 years when first seen by us on October 8, 1928. He complained of palpitation and of slight breathlessness on exertion. At the age of 6 years he had enteric fever. There was no rheumatic history. At the age of 16 years the heart was found to be beating very rapidly and a doctor said it was enlarged. His games were restricted. Between the ages of 18 and 21 years, he was doing heavy manual work abroad without much distress. He was then rejected on medical examination, though he had only minor symptoms.
Examination revealed no abnormal signs. The heart rate was 80 a minute. The blood pressure was 130 mm. mercury systolic, and 85 diastolic.
The orthodiagram was normal.
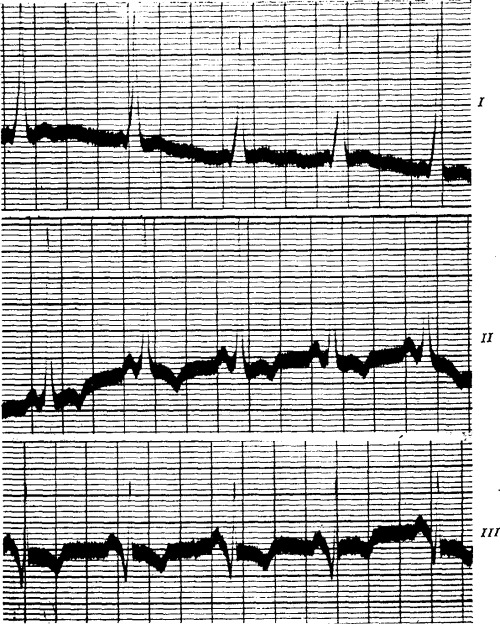
Electrocardiograms showed abnormally widened ventricular complexes, regular at 60 per minute (Fig. 14). The P‐waves were normal and upright in all leads. The P‐R interval was just under 0.1 second. The next day, October 9, 1928, similar electrocardiograms were obtained. He was advised to disregard his occasional palpitation, but to find lighter work in view of the slight dyspnea on exertion. He proceeded abroad again.
Figure 14.
(Case VI) Intraventricular block. The P‐waves are normal and upright in all leads. The P‐R interval is well under 0.1 second.
In August, 1929, he was reported to be quite well and at work.
Case VII. B.H., male, aged 11 years when first seen by us April 13, 1929. There was a history of exhaustion, occasional pallor, and a varying pulse rate, often slow. He was always easily tired, and for a year he had had recurrent attacks in which he was pale and the pulse rate varied between 40 and 65 over a period of a few days. Otherwise he was fairly well and fond of games including football. Dyspnea had not been noticed. There was no rheumatic history.
Examination showed a smallish child, weighing 56 pounds; otherwise he looked well. The pulse rate was from 50 to 60 a minute and sinus arrhythmia was noted. The blood pressure was 110 mm. mercury systolic, and 75 diastolic. The heart sounds were normal and no murmurs were heard.
An orthodiagram showed a heart of normal size and shape.
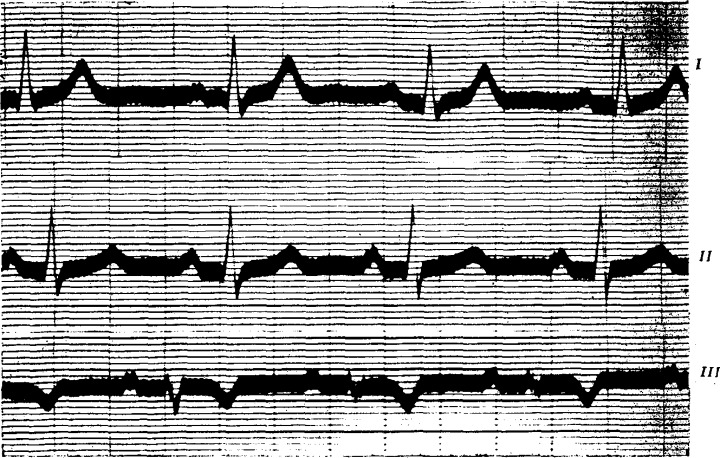
Electrocardiograms on April 13, and again on April 16, 1929, were of the same form (Fig. 15). The P‐waves were small and upright in all leads. The P‐R interval was well under 0.1 second. The ventricular complexes had the form of left bundle‐branch block.
Figure 15.
(Case VII) Left bundle‐branch block. The P‐waves are normal and upright in all leads. The P‐R interval is well under 0.1 second.
Case VIII. C. B., female, aged 16 years when first seen by us on January 15, 1925. There was a history of alleged heart trouble. She had been quite well until two years before when she began to be obviously breathless at dancing and hockey. One night she felt a throbbing in her neck which kept her awake. She had improved since two years ago and scarcely considered herself breathless. There was no rheumatic history.
Examination showed a girl of healthy color and appearance. There were bright red birthmarks on the left leg. There was no clubbing of the fingers. The heart sounds were normal. The blood pressure was 110 mm. mercury systolic, and 75 mm. diastolic.
Radioscopy showed slight to moderate enlargement of the heart to the right, with active systolic pulsation of the right and left borders; the diaphragm moved well.
A brisk walk with the patient showed that she was more breathless than a healthy observer.
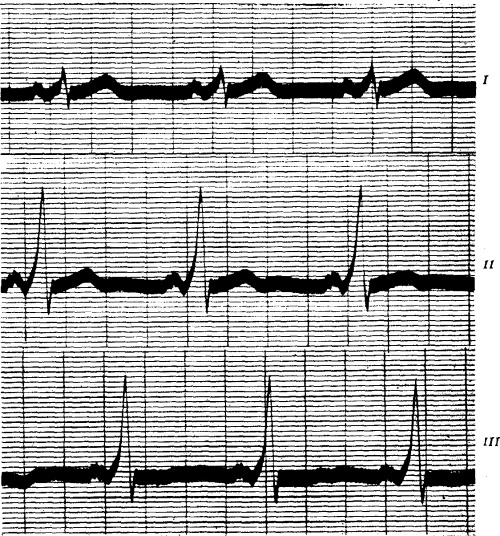
Electrocardiograms showed a regular rhythm at a rate of from 60 to 70 a minute (Fig. 16). The P‐waves were normal and upright in all leads. The P‐R interval was well under 0.1 second. The ventricular complexes had the complete characteristics of right bundle‐branch block. On January 16, 1925, the following day, exactly similar records were obtained.
Figure 16.

(Case VIII) Right bundle‐branch block. The P‐R interval is well under 0.1 second.
Three years later, at the age of 19, she was reported to be in good health and hard at work as a student.
Recently (October 11, 1929) she has been seen again, at the age of 21 years. She is a university student, and is active and well. Her only complaint is that she is easily tired. Physical examination and radioscopy show no abnormalities. The electrocardiogram is now normal (Fig. 17) in contrast with that taken in 1925 (Fig. 16).
Figure 17.
(Case VIII) Three years later. Normal physical curves. The P‐R interval is 0.16 second. The P‐waves are identical in Figs. 16 and 17.
Case IX. H. H., male, a musician, aged 42 years when first seen at the London Hospital on the 28th of May, 1914. He complained then of attacks of palpitation, which began at the age of nine years. They were sudden in onset and offset, and their duration varied from a few minutes to two weeks. Frequently the attacks could be stopped if the patient held his breath or put his head between his knees. Otherwise he was well.
There was no rheumatic history. He had diphtheria and scarlet fever some years after the onset of the attacks of paroxysmal tachycardia.
Examination when first seen, which was on the tenth day of an attack of paroxysmal tachycardia showed dyspnea, a large heart, dulness and crepitations at the lung bases, and a large pulsating liver. The blood Wassermann reaction was negative.
Electrocardiograms taken after the paroxysm ended showed a regular rhythm with upright P‐waves in all leads, a short P‐R interval, abnormally widened QRS complexes and inverted T‐waves in all leads (Fig. 18). An electrocardiogram was obtained during a paroxysm of tachycardia at a rate of 150, the form of the curve being unlike that between attacks.
Figure 18.
(Case IX) Intraventricular block. The P‐R interval is 0.1 second. Time intervals = 0.2 and 0.04 seconds.
He was examined again on the 15th of September, 1914. The last paroxysm had occurred six weeks before and lasted three weeks. There was cardiac enlargement both on physical examination and by radioscopy. There were no murmurs. The lungs were normal.
Between the ages of 47 and 57 years he had no attacks. In 1928 the paroxysms returned. The heart was enlarged (radioscopy). An electrocardiogram between attacks was in general like that taken in 1914, as was another obtained during a paroxysm.*
Case X. Mrs. A. C. M., a widow, aged 44 years when first seen in the Out‐Patient Department of the Massachusetts General Hospital on November 26, 1927. She complained of attacks of palpitation. The attacks, which began at the age of 7, were always sudden in onset and offset. For the three years from 1924 to 1927 they had occurred more frequently, often daily. They lasted from a few minutes to several hours (intermittently) and were easily terminated by taking a deep breath and holding it, or by lying down.
She had measles and diphtheria at the age of 5 years. In 1923 she had had her tonsils revmoved because of recurring tonsillitis and peritonsillar abscess. There was no rheumatic history.
Physical examination was entirely negative. The blood pressure was 140 mm. mercury systolic, and 85 diastolic.
Electrocardiograms showed a regular rhythm at the rate of 65 a minute (Fig. 19). The P‐waves were normal and upright, and the P‐R interval was 0.1 second. The ventricular complexes were of the type designated as indicating right bundle‐branch block.
Figure 19.
(Case X) Intraventricular block. The P‐R interval is 0.1 second.
She was again seen on December 29, 1927, in an attack of paroxysmal tachycardia. The heart rate was over 200 and regular. An electrocardiogram was taken which showed auricular paroxysmal tachycardia at a rate of 230, without A‐V block.
The ventricular complexes were normal in form. After the electrocardiogram was taken she ended the attack by a forced inspiration. She then had frequent premature beats. She stated that since taking quinidine the attacks had become less frequent.
Case XI. Mrs. R. E., aged 55 years, entered the West Medical Service of the Massachusetts General Hospital on February 26, 1918, complaining of palpitation. The attacks of palpitation had begun ten years previously, but for the past four years the attacks had been somewhat more severe, occurring with change of weather to wet and cold, as well as after any indiscretion in diet. For two months prior to entrance into the hospital attacks of palpitation had been occurring at night, waking her out of sleep. As a rule the attacks lasted ten minutes.
There was no rheumatic history. She had had tonsillitis every year during youth. For a year there had been slight localized edema of the legs. She considered herself nervous.
Physical examination showed a poorly nourished, cyanotic, uncomfortable woman. The heart was moderately enlarged, the systolic blood pressure varied between 175 and 205 mm. mercury, the diastolic between 95 and 105. There was a loud apical systolic murmur transmitted to the axilla. There were signs of pulmonary tuberculosis.
The blood Wassermann reaction was negative.
Roentgen ray examination showed cardiac enlargement and pulmonary tuberculosis.
The electrocardiogram revealed normal P‐waves which were upright in all leads. The P‐R interval was less than 0.1 second. The ventricular complexes were of the type designated as indicating bundle‐branch block (Fig. 20). The rhythm was regular and the rate 114.
Figure 20.
(Case XI) Intraventricular block. The P‐R interval is less than 0.1 second.
DISCUSSION
The combination of bundle‐branch block, abnormally short P‐R interval, and paroxysms of tachycardia (also paroxysmal auricular fibrillation and perhaps flutter) in young, healthy patients with normal hearts is distinctive, and worthy of recognition as a mechanism heretofore undescribed as such. The reversion to normal ventricular complexes and longer (normal) P‐R interval, spontaneously or by vagal release following exercise or atropinization is characteristic. The paradoxical effect of vagal stimulation on the P‐R interval is noteworthy.
We have been unable to demonstrate structural heart disease in our patients, except in the two oldest ones. One of these (Case IX) was first seen at the age of 42 years; he then had had paroxysms of tachycardia for 33 years. An electrocardiogram showed bundle‐branch block with abnormally short P‐R interval. Fourteen years later his electrocardiogram was essentially unaltered. The abnormal cardiovascular signs on physical examination in this patient may have been the result of coincidental development of organic heart disease. The other patient (Case XI) was 55 years old when first seen, and on account of her age and the presence of hypertension, we believe that the abnormal cardiovascular sings were probably coincidental and not associated with the peculiar mechanism, already described, present in this case.
None of our patients presented evidence or gave a history of rheumatic infections. Other infections, toxic states, and rapid heart rates were not responsible for the abnormal electrocardiograms. The subjects were in good health, and as a rule the only complaint was palpitation. The age of our patients suggests that a congenital anomaly may be responsible for the phenomena observed in this group. We have no proof for or against this suggestion. All the available evidence points to vagal influence as the controlling factor in this mechanism. Incidentally, it may be pointed out that here is a group of patients in whom paroxysmal tachycardia and auricular fibrillation (and perhaps flutter) is obviously associated with this unusual mechanism, quite possibly of vagal origin.
A case undoubtedly exhibiting the same mechanism was described in 1921 by A. M. Wedd. 6 A student, 19 years old, had had paroxysms of tachycardia since the age of 5 years. He was well otherwise and the heart and blood pressure were normal. Electrocardiograms showed intraventricular block and a P‐R interval of 0.08 second. The P‐waves were upright in all leads. At other times the ventricular complexes were normal, and the P‐R interval doubled. The author assumes the presence of A‐V nodal rhythm.
A somewhat similar case was reported by F. N. Wilson in 1915. 7 This patient had mitral stenosis, and the author suggests that it is “improbable that the bundle‐branch block was due to vagus influence alone,” but that “conduction through the right branch of the A‐V bundle was already impaired and that this rendered it especially susceptible to vagus influence.” The short P‐R interval was explained by assuming that A‐V nodal rhythm was present; the P‐wave was inverted in Leads II and III.*
A study of the electrocardiograms of our patients has enabled us to exclude the presence of A‐V nodal rhythm because frequent ventricular premature beats were followed consistently by compensatory pauses, and the form of the P‐waves occurring with both long and short P‐R intervals was identical. In several patients the P‐waves were distinctly notched, making identification easy and certain. Finally, the P‐waves were always upright in all three leads.
The group includes eight males and three females. The youngest patient was eleven years old when first seen. Two patients were 16, one 18, one 21, two 23, one 35, and the three oldest patients were 43, 44 and 55 years respectively. One patient had attacks of paroxysmal tachycardia for 48 years, another for 37 years, one for 14 years, and two patients for 10 years respectively.
SUMMARY AND CONCLUSIONS
-
1
Eleven cases are here reported of an unusual cardiac mechanism, heretofore undescribed as such, consisting of functional bundle‐branch block and abnormally short P‐R interval, occurring mostly in otherwise healthy young people with paroxysms of tachycardia or of auricular fibrillation.
-
2
Spontaneously, or following release of vagal tone by exercise or atropinization, the ventricular complexes revert to the normal physiological form, and the P‐R interval lengthens to become normal.
-
3
Vagal influences seem to be largely responsible for the mechanism described. A paradoxical effect of vagal stimulation on the P‐R interval has been observed.
-
4
Infection, rheumatic and otherwise, toxic states, and rapid heart rates are not responsible for the abnormal electrocardiogram. Auriculo‐ventricular nodal rhythm is apparently not responsible for the short P‐R interval.
-
5
From a study of the cases here presented we conclude that:
-
a)
Aberrant ventricular complexes of the type generally recognized as indicating bundle‐branch block may occur in healthy people with normal hearts.
-
b)
Vagal stimulation is capable of altering markedly the form of the ventricular complex, and may be responsible for the occurrence of complete bundle‐branch block curves in apparently normal hearts at normal rates of beating.
-
c)
Vagal stimulation may shorten markedly the P‐R interval without the production of A‐V nodal rhythm, and without dislocating the auricular pacemaker.
-
d)
In the group of cases reported paroxysmal tachycardia and auricular fibrillation are associated with the nervous control of the heart.
-
e)
The recognition of functional bundle‐branch block is of considerable practical importance. The combination of intraventricular block with abnormally short P‐R interval, interchangeable with normal ventricular complexes with longer P‐R interval (reversion spontaneous or following exercise or atropinization) in healthy young people with paroxysmal tachycardia (or auricular fibrillation) is distinctive.
-
f)
This mechanism is apparently not indicative of disease of the heart.
-
a)
NOTE: In this paper bundle‐branch block when mentioned is referred to according to the old nomenclature of right bundle‐branch block for upright widened Q‐R‐S waves in Lead I and inverted widened Q‐R‐S waves in Lead III, and left bundle‐branch block for inverted widened Q‐R‐S waves in Lead I, and upright widened Q‐R‐S waves in Lead III according to the newly revised nomenclature, which is probably correct, these designations would be changed, so that one should read “left bundle‐branch block” for “right” and “right bundle‐branch block” for “left” in this paper.
Footnotes
The patient's present condition has been described recently in a paper by Dr. Francis Bach entitled, “Paroxysmal Tachycardia of 48 Years' Duration, and Right Bundle‐Branch Block.” Proc. Roy. Soc. Med. London, 22: 412, 1929.
Recently W. W. Hamburger in the Medical Clinics of North America (13: 343, 1929) reported the occurrence of bundle‐branch block with a short P‐R interval in a child aged four and one‐half years, who had had paroxysmal tachycardia for one year. The author assumed that acute severe right bundle‐branch block occurred as the result of an acute respiratory infection.
REFERENCES
- 1. Carter, E. P .: Clinical Observations on Defective Conduction in the Branches of the Auriculo‐Ventricular Bundle. Arch. Int. Med., 13, 803, 1914. [Google Scholar]
- 2. Cohn, A. E. , and Lewis, T .: The Pathology of Bundle‐Branch Lesions of the Heart. Proc. N. Y. Path. Soc., 14, 207, 1914. [Google Scholar]
- 3. Eppinger, H. , Und Rothberger, J .: Zur Analyse des Elektrokardiogramms. Wien Klin. Wchnschr., 22, 1091,1909. [Google Scholar]
- 4. Eppinger, H. , Und Rothberger, J .: Ueber die Folgen der Durchschneidung der Tawaraschen Schenkel des Reizleitungssystems. Ztschr. f. klin. Med., 70, 1, 1910. [Google Scholar]
- 5. Eppinger, H. , Und Stoerk, O. : Zur Klinik des Elektrokardiogramms. Ztschr. f. klin. Med., 71, 157, 1910. [Google Scholar]
- 6. Wedd, A. M. : Paroxysmal Tachyeardia. Arch. Int. Med., 27, 571, 1921. [Google Scholar]
- 7. Wilson, F. N .: A Case in Which the Vagus Influenced the Form of the Ventricular Complex of the Electrocardiogram. Arch. Int. Med., 16, 1008, 1915. [DOI] [PMC free article] [PubMed] [Google Scholar]


