Abstract
Background: ST depression and T‐wave amplitude abnormalities are known to be independent predictors of cardiovascular (CV) death, but a direct comparison between them has not been described.
Methods: Analyses were performed on the first electrocardiogram (ECG) digitally recorded on 46,950 consecutive patients at the Palo Alto Veterans Affairs Medical Center since 1987. Females and patients with electrocardiograms exhibiting bundle branch block, left ventricular hypertrophy, electronic pacing, diagnostic Q waves, or Wolff–Parkinson–White syndrome were excluded, leaving 31,074 male patients for analysis (mean age 55 ± 14). There were 1878 (6.0%) cardiovascular deaths (mean follow‐up of 6 ± 4 years). Electrocardiograms were classified using Minnesota code according to the degree of ST depression and T‐wave abnormality, and the nine possible combinations of ST segment and T‐wave abnormalities were recoded for analysis.
Results: The combination of major abnormalities in ST segments and T‐waves carried the greatest hazard [3.2 (CI 2.7–3.8)]. Minor ST depression combined with more severe T‐wave abnormalities carried a hazard of 3.1 (CI 2.5–3.7), whereas minor T‐wave abnormalities combined with more severe ST depression carried a hazard of only 1.9 (CI 1.6–2.3).
Conclusion: While both ST segment depression and abnormal T‐wave amplitude are clinically important, T‐wave abnormalities appear to be greater predictors of cardiovascular mortality.
Keywords: electrocardiogram, ST segment, T‐wave, mortality
Clinicians who evaluate resting 12‐lead electrocardiograms (ECGs) are routinely faced with the challenge of characterizing repolarization abnormalities. Whereas Q waves are diagnostic of myocardial infarction and increased QRS duration suggests conduction delay, repolarization abnormalities, especially when minor, are often considered nonspecific. Unfortunately, “nonspecific” can also be interpreted by the reader or the referring clinician as “nonsignficant.” In addition, while many clinicians might recognize ST segment depression as abnormal and perhaps ominous, minor T‐wave amplitude abnormalities may be considered labile and not be considered as significant by comparison.
In fact, repolarization abnormalities have been well described as predictors of cardiovascular (CV) mortality. The repolarization phase is comprised of the ST segment and the T wave; repolarization abnormalities may represent heterogeneities associated with electrical instability and sudden cardiac death. Studies of ST depression, 1 combined ST–T criteria, 2 , 3 , 4 , 5 as well as those of T‐wave abnormalities alone, 6 , 7 have confirmed these changes as significant. However, a direct comparison between them has not been described. The purpose of this study is to compare ST depression and T‐wave abnormalities on the resting ECG as predictors of cardiovascular mortality.
METHODS
All ECGs (n = 46,950) obtained at the Palo Alto VA Medical Center between March 1987 and December 2000 were digitally recorded and stored in the General Electric MUSE ECG management system (http://www.gemedicalsystems.com). When a patient had more than one ECG in the database, only the earliest ECG was considered. Computerized measurements from the ECG as well as several computerized ECG interpretations were extracted. ECGs obtained in an inpatient or outpatient setting, or in the emergency room were coded separately since they could be influenced by acute clinical events. Females (n = 4616) and ECGs exhibiting electronic pacing, Wolff–Parkinson–White syndrome, left ventricular hypertrophy, pathological Q waves, and/or bundle branch block were excluded from all analyses. The remaining 31,074 male patients comprised the study population and were followed for a mean of 6 years.
Standardized computerized ECG criteria as described by the General Electric 12‐lead ECG analysis program were utilized for diagnostic Q waves and bundle branch blocks (see MUSE/12 lead ECG physician program manual at http://www.gemedicalsystems.com). While these interpretations are usually over read by a cardiologist before being released as “confirmed,” we used only the computer interpretation. ST segment and T‐wave patterns were categorized based on the Minnesota code (MC) using computer algorithms (4‐1 and 4‐2 as major ST depression, 4‐3 as minor ST depression, 5‐1 and 5‐2 as major T abnormality, and 5‐3 and 5‐4 as minor T abnormality). Figure 1 details examples of several of these abnormalities.
Figure 1.
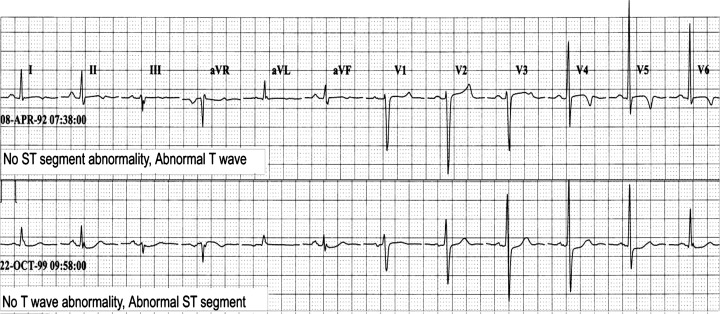
Examples of ST segment and T‐wave abnormalities.
Both the Social Security death index and the California Health Department Service were used to ascertain vital status as of December 30, 2000. The main outcome measure was cardiovascular mortality.
The database was imported into NCSS (Number Cruncher Statistical System®, Kaysville, Utah) for analysis. Differences in characteristics among the groups were compared using chi‐square tests, nonpaired t‐tests, and analysis of variance, as appropriate. Bivariate associations between those who suffered a cardiovascular death and all others were tested by using chi‐square tests for categorical data and t‐tests for continuous variables. P values less than 0.05 were considered significant. Cox Hazard Proportional hazard testing was performed to assess the significance and independence of predictors of CV mortality, and the models were age and heart rate adjusted. ST depression and T‐wave amplitude of all 12 leads, as well as other ECG measurements, were considered. Kaplan–Meier survival curves were performed using ST and T‐wave amplitude categories. Relative risks were calculated for degree of various ST and T‐wave abnormalities to determine criteria for practical clinical utility. Relative risk of each degree of abnormality was calculated to demonstrate incremental risk per each incremental step. The subset analysis was also repeated only in outpatients in order to exclude ECGs associated with acute clinical events.
RESULTS
The demographics of the study population are summarized in Table 1. There were 31,074 patients included in the analysis, and there were 1878 (6.0%) cardiovascular deaths during a mean follow‐up of 6 ± 4 years. The patients had a mean age of 55, and 8560 were inpatients at the time of their ECG; 10354 patients had ECGs without ST or T‐wave abnormalities, and the remaining subjects had repolarization abnormalities involving the ST segment, T wave, or both. Of the 20,025 patients with ST segment depression, only 4618 also had T wave abnormalities, whereas 4618 of the 5313 patients with abnormal T waves also had ST segment depression. While there were 1559 (7.5%) deaths among the patients with ST or T‐wave abnormalities, there were only 319 (3.1%) deaths in the patients without these changes. Deaths also were more likely to occur in older patients and inpatients. The distribution of repolarization abnormalities and the number of cardiovascular deaths are summarized in Tables 2 and 3.
Table 1.
Demographics of the Study Population
| (+) CV Death | (−) CV Death | P Value | |
|---|---|---|---|
| Subjects | 1878 (6.0%) | 29196 (94%) | |
| Age (years) | 66.5 ± 11.8 | 54.0 ± 14.0 | <0.0001 |
| Body mass index (kg/m2) | 26.8 ± 5.2 | 27.3 ± 5.4 | 0.0001 |
| Inpatient | 772 | 7788 | <0.0001 |
| Heart rate (bpm) | 76.8 ± 16.6 | 73.5 ± 15.8 | <0.0001 |
| QRS duration (ms) | 92.5 ± 10.6 | 91.4 ± 9.5 | <0.0001 |
| Minor T (MC 5−3, 5−4) | 687 (36.6%) | 4232 (14.5%) | <0.0001 |
| Major T (MC 5−1, 5−2) | 300 (16%) | 1266 (4.3%) | <0.0001 |
| Minor ST (MC 4−3) | 1368 (72.8%) | 17683 (60.6%) | <0.0001 |
| Major ST (MC 4−1, 4−2) | 447 (23.8%) | 3292 (11.3%) | <0.0001 |
| QT interval (ms) | 386.1 ± 41.2 | 383.8 ± 38.7 | 0.01 |
CV = cardiovascular; MC = Minnesota code.
Table 2.
Distribution of Repolarization Abnormalities
| No T‐Wave Abnormality | Minor T (MC 5−3, 5−4) | Major T (MC 5−1, 5−2) | |
|---|---|---|---|
| No ST abnormality | 10,354 | 558 | 137 |
| Minor ST (MC 4−3) | 13,365 | 2259 | 662 |
| Major ST (MC 4−1, 4−2) | 2042 | 930 | 767 |
MC = Minnesota code.
Table 3.
Distribution of Cardiovascular Deaths
| No T Wave Abnormality | Minor T (MC 5‐3, 5‐4) | Major T (MC 5‐1, 5‐2) | |
|---|---|---|---|
| No ST abnormality | 319 (17%) | 55 (2.9%) | 12 (0.64%) |
| Minor ST (MC 4‐3) | 661 (35%) | 264 (14%) | 120 (6.4%) |
| Major ST (MC 4‐1, 4‐2) | 149 (7.9%) | 130 (6.9%) | 168 (8.9%) |
MC = Minnesota code.
After adjusting for age and heart rate in the Cox model, ST depression and T‐wave amplitude abnormalities as well as other ECG indicators and measurements were considered univariately. As predicted, both ST segment and T‐wave abnormalities were significantly and strongly associated with CV death. Determinations of these abnormalities were made using both Minnesota code and individual leads, and both yielded similar results. When Minnesota code was used, either abnormality in the absence of the other abnormality failed to reach statistical significance. However, combinations were predictive of cardiovascular mortality. A minor T‐wave abnormality predicted CV mortality in the presence of minor ST depression [1.8 (1.6–2.1)] and major ST depression [2.0 (1.7–2.4)]. However, minor ST depression combined with major T‐wave abnormality had an even greater hazard ratio [3.2 (2.7–3.9)]. The combination of major abnormalities in ST segments and T waves carried the greatest hazard [3.3 (2.8–3.9)]. The three Kaplan–Meier curves in Figure 2 illustrate our findings that T‐wave abnormalities appear to be more predictive of CV mortality than ST depression when both are present. There were similar findings when individual ECG leads were evaluated. T‐wave abnormalities in lead I were most predictive of CV mortality, and ST depression was most predictive in lead V5. For example, Tables 4 and 5 show the hazard ratios for ST depression in lead V5 and T‐wave abnormalities in lead I as well as when Minnesota code was used. They illustrate that T waves are more predictive than ST depression of CV mortality when the two are combined. Similar results were achieved with other leads. Similar results were also obtained in subgroup analyses of outpatients and inpatients. Even when exclusionary criteria such as bundle branch block, left ventricular hypertrophy, diagnostic Q waves, or Wolff–Parkinson–White syndrome were included, our findings were confirmed.
Figure 2.
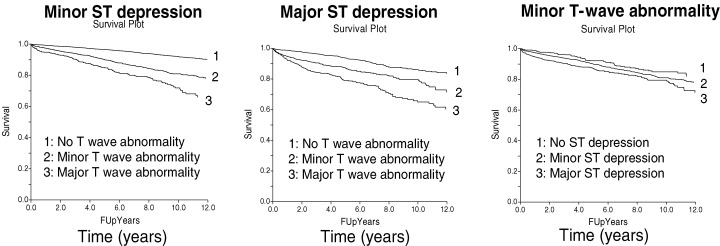
Survival is shown to decrease over time with increasing abnormalities of either T waves or ST segments. However, when these abnormalities are combined, an increase in severity of ST segment depression does not greatly contribute to increased mortality, whereas an increase in severity of T‐wave abnormality clearly corresponds to an increase in mortality.
Table 4.
Age‐ and Heart Rate‐Adjusted Relative Risk of Cardiovascular Death with 95% Confidence Intervals: Minnesota Code
| No T‐Wave Abnormality | Minor T (MC 5−3, 5−4) | Major T (MC 5−1, 5−2) | |
|---|---|---|---|
| No ST abnormality | Reference | 1.8 (1.4–2.3) | NS |
| Minor ST (MC 4−3) | NS | 1.8 (1.6–2.1) | 3.2 (2.7–3.9) |
| Major ST (MC 4−1, 4−2) | NS | 2.0 (1.7–2.4) | 3.3 (2.8–3.9) |
MC = Minnesota code, ns = nonsignficant.
Table 5.
Age‐ and Heart Rate‐Adjusted Relative Risk of Cardiovascular Death with 95% Confidence Intervals: Individual Leads
| T Wave in Lead | I ST in Lead V5 >1.0 mm | 1.0 to 0.5 | 0.5 to 0 | <0 mm |
|---|---|---|---|---|
| >0 mm | Reference | 1.4 (1.1–1.7) | 1.9 (1.4–2.5) | 3.6 (2.7–4.9) |
| −0.5 to 0 | NS | 1.4 (1.2–1.6) | 2.0 (1.7–2.4) | 2.9 (2.4–3.5) |
| −1.0 to −0.5 | NS | 1.4 (1.0–1.9) | 3.0 (2.3–4.0) | 3.3 (2.7–4.1) |
| <−1.0 mm | NS | 2.2 (1.2–4.2) | 2.8 (1.7–4.6) | 5.2 (3.8–7.2) |
CONCLUSIONS
This study validates the utility of ST segment depression and T‐wave amplitude abnormalities in predicting cardiovascular mortality in a large, general hospital‐based population, using retrospective, computerized spatial ECG measurements of ventricular repolarization abnormalities. Our findings support the value of repolarization measures as a tool for risk stratification. While previous studies have explored repolarization abnormalities as predictive of CV mortality, this study is to our knowledge the first to directly compare the relative contributions of ST depression and T‐wave abnormalities.
It is unclear why T waves should have a more pronounced predictive effect than ST depression. The ST segment is a period of electrocardiographic silence, occurring after depolarization has occurred and before repolarization has begun. The T wave represents the period of ventricular repolarization. Multiple studies have assessed various descriptors of repolarization, including T‐wave residua, 8 T‐wave morphology, 9 and spatial QRS‐T wave angle, 10 and have consistently found a positive association with cardiovascular mortality in general populations. It is notable that our findings were significant in both inpatients and outpatients, suggesting that the ECG abnormalities were not associated with acute ischemia or infarction.
Our population was predominantly male (only 10% of the patients were women). However, other studies have confirmed the predictive value of “nonspecific” ST–T changes in female populations. Greenland et al. 5 examined only minor ST segment and T‐wave abnormalities, and found that isolated minor T‐wave abnormalities were not significant, and isolated minor ST depression carried a hazard of 1.93. Combined abnormalities carried a hazard of 2.5. Interestingly, minor T‐wave abnormalities were significant in the male population studied. It is uncertain why these abnormalities might have different predictive values in men as compared to women.
Our study is also limited by lack of descriptive information about the subject population. Cardiovascular mortality was determined from death certificates, which may potentially have inaccuracies as well as lack specificity. There was a correlation with total mortality as well; however, it was not as strong. The ECGs represent a broad sample from inpatients and outpatients, but the specific reasons why the ECGs were obtained were not available. However, this limitation may actually be a strength in evaluating scores that are applied to a general medical population. In addition, we do not have results of diagnostic testing such as echocardiograms or cardiac catheterization and are therefore unable to evaluate for events such as myocardial infarction, heart failure, and coronary heart disease. However, incorporating other tests or using test results as surrogate endpoints might actually bias our results, since these tests are performed for specific clinical indications.
Both ST depression and T‐wave amplitude abnormalities are significant and independent predictors of cardiovascular death. Our study also directly compares T‐wave abnormalities to ST depressions, and our data suggest that T waves are actually a greater predictor of cardiovascular mortality. The standard electrocardiogram is widely available, playing a critical role in evaluation of possible and known cardiac disease. Assessing ST segments and T waves is a basic element of electrocardiographic interpretation. It is our goal to influence clinicians to critically evaluate “nonspecific” interpretations of ST–T wave changes and actually identify these changes as predictors of cardiovascular mortality in a general male population. Our findings confirm previous research regarding the prognostic value of these abnormalities, and in addition provide a direct comparison between them. The physician can apply these results to help make decisions regarding further cardiac testing, the intensity of risk factor management, and/or referral to a cardiologist.
REFERENCES
- 1. Okin PM, Devereux RB, Lee ET, et al Electrocardiographic repolarization complexity and abnormality predict all‐cause and cardiovascular mortality in diabetes: The strong heart study. Diabetes 2004;53(2):434–440. [DOI] [PubMed] [Google Scholar]
- 2. De Bacquer D, De Backer G, Kornitzer M, et al Prognostic value of ischemic electrocardiographic findings for cardiovascular mortality in men and women. J Am Coll Cardiol 1998;32(3):680–685.DOI: 10.1016/S0735-1097(98)00303-9 [DOI] [PubMed] [Google Scholar]
- 3. Daviglus ML, Liao Y, Greenland P, et al Association of nonspecific minor ST–T abnormalities with cardiovascular mortality: The Chicago Western Electric Study. J Am Med Assoc 1999;281(6):530–536.DOI: 10.1001/jama.281.6.530 [DOI] [PubMed] [Google Scholar]
- 4. De Bacquer D, De Backer G, Kornitzer M, et al Prognostic value of ECG findings for total, cardiovascular disease, and coronary heart disease death in men and women. Heart 1998;80(6):570–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Greenland P, Xie X, Liu K, et al Impact of minor electrocardiographic ST‐segment and (or T‐wave abnormalities on cardiovascular mortality during long‐term follow‐up. Am J Cardiol 2003;91(9):1068–1074.DOI: 10.1016/S0002-9149(03)00150-4 [DOI] [PubMed] [Google Scholar]
- 6. Jacobsen MD, Wagner GS, Holmvang L, et al Clinical significance of abnormal T waves in patients with non‐ST‐segment elevation acute coronary syndromes. Am J Cardiol 2001;88(11):1225–1229.DOI: 10.1016/S0002-9149(01)02081-1 [DOI] [PubMed] [Google Scholar]
- 7. Okin PM, Devereux RB, Fabsitz RR, et al Principal component analysis of the T wave and prediction of cardiovascular mortality in American Indians: The Strong Heart Study. Circulation 2002;105(6):714–719. [DOI] [PubMed] [Google Scholar]
- 8. Zabel M, Malik M, Hnatkova K, et al Analysis of T‐wave morphology from the 12‐lead electrocardiogram for prediction of long‐term prognosis in male US veterans. Circulation 2002;105(9):1066–1070. [DOI] [PubMed] [Google Scholar]
- 9. Zabel M, Malik M. Practical use of T wave morphology assessment. Card Electrophysiol Rev 2002;6(3):316–322.DOI: 10.1023/A:1016353714372 [DOI] [PubMed] [Google Scholar]
- 10. Kardys I, Kors JA, Van Der Meer IM, et al Spatial QRS‐T angle predicts cardiac death in a general population. Eur Heart J 2003;24(14):1357–1364.DOI: 10.1016/S0195-668X(03)00203-3 [DOI] [PubMed] [Google Scholar]


