Abstract
Background: Signal‐averaged electrocardiography of the P wave (P wave SAECG) is a noninvasive method for evaluating the risk of atrial fibrillation (AF). We aimed to study P wave SAECG parameters in a large number of apparently healthy subjects and to compare them with patients with converted AF.
Methods: We examined 591 individuals; P wave SAECG were recorded in 330 normal subjects, 31 patients with converted persistent AF and 57 patients with converted paroxysmal AF immediately after conversion, at 12 and 24 hours after conversion, then after 3 and 6 months. P wave SAECG were recorded using a commercially available machine aiming to obtain a noise level <1 μV.
Results: In the normal population the duration of the filtered P wave (PWD) was higher in men. P wave duration, RMS40 and RMS30 were significantly correlated with age.
By comparing the normal population with patients with persistent AF converted to sinus rhythm we demonstrated significant differences in PWD and P wave integral. Patients with recurrent persistent AF had significantly higher PWD.
The study of patients with paroxysmal AF, compared to the control group, showed significant increase of the same parameters: PWD and integral of the P wave. Patients with recurrent paroxysmal AF had higher PWD and lower RMS40, RMS30, RMS20.
Conclusions: Filtered P wave duration was higher in men; PWD was weakly but significantly correlated with age. Patients with paroxysmal or persistent AF converted to sinus rhythm had significantly higher P wave duration and P wave integral.
Ann Noninvasive Electrocardiol 2011;16(4):351–356
Keywords: noninvasive techniques, signal‐averaged ECG, atrial fibrillation
Atrial fibrillation (AF) remains the most frequent arrhythmia (5% of the population over 69 years), thus any method that could assess the risk for AF may have important implications.
Signal‐averaged electrocardiography of the P wave (P wave SAECG) is a noninvasive method for evaluating the risk of AF onset or of the passing from paroxysmal (PxAF) to persistent AF (PsAF).
Although there have been made some correlation between P wave SAECG parameters and the risk for paroxysmal AF, or for evolution of PxAF to PsAF, normal values of these parameters or their variation with age, sex, or other clinical factors are not well established.
We aimed to study P wave SAECG parameters in a large number of apparently healthy subjects and to compare them with patients with converted AF.
The main objectives of the study were:
-
1
To evaluate P wave SAECG parameters in an apparently normal population, and their variation with age and sex (control group).
-
2
To compare P wave SAECG parameters in a group of patients with electrically converted PsAF with the control group.
-
3
To compare P wave SAECG parameters in a group of patients with PxAF to the control group.
-
4
To compare patients with recurrent PxAF/PsAF to the other patients with PxAF/PsAF.
-
5
To analyze the temporal evolution of P wave SAECG parameters after conversion of AF.
METHODS
For the control group we examined 591 individuals; after exclusion of heart disease (clinical exam, ECG, echocardiography), P wave SAECG were recorded in 330 subjects (208 females, 122 males), using a commercially available machine (General Electric MAC 5000) aiming to obtain a noise level <1 μV.
The following parameters of the P wave SAECG were analyzed:
-
1
Filtered P wave duration (PWD).
-
2
The root mean square in the last 40, 30, and 20 ms (RMS40, RMS30, RMS20).
-
3
The root mean square of the P wave (RMSP).
-
4
Integral of the voltages in the entire P wave (INTP).
We analyzed their variation with age and sex.
The second group included 31 patients with PsAF.
Before electrical conversion patients received amiodarone (800–1000 mg for 7 days, then 200–600 mg for 3 weeks) and acenocumarol (for 3 weeks, target INR between 2 and 3). The cardioversion protocol consisted of administration of Unfractioned Heparin 10000 IU intravenous bolus, Diazepam 10 mg, Pethidine 20 mg, Metoclopramide 10 mg followed by synchronized DC monophasic sinusoidal waveform shock with anterior‐apex paddle placement. The starting energy delivery was 200 J, ranging until 360 J, if necessary.
After cardioversion patients received amiodarone (100–400 mg) and acenocumarol (for minimum 4 weeks).
After electrical conversion to sinus rhythm we recorded P wave SAECG immediately after conversion, at 12 and 24 hours after conversion, then after 3 and 6 months. We compared the parameters to those in control group and studied their variation with time.
Some of the patients with converted PsAF presented recurrent episodes in the 6 months of follow‐up, that were converted using pharmacological or electrical methods—this group was compared to patients that stayed in sinus rhytm.
The third group included 57 patients with PxAF, and were compared with the control group. Similarly to group two, patients with recurrent PxAF were compared with the others.
Statistical analyses were performed by using SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA). Student's t‐test was used to analyze differences between mean values. A probability value of 0.05 or less was considered significant. We considered the variables as independent continuous data. For groups with fewer patients we chose t‐repartition that requires a near‐Gaussian distribution of data and similar standard deviations in the compared groups.
To verify the normality of data repartition we used Kolmogorov–Smirnov and Shapiro–Wilk tests; to verify the similarity of dispersions we used Levene test.
RESULTS
Mean age was 51.5 ± 16.9 years in men and 51 ± 15.5 years in women.
P‐Hires Parameters in Control Group
Mean values of P wave SAECG parameters (±standard deviation) in the control group (normal population) are presented in Table 1.
Table 1.
Mean Values of P Wave SAECG Parameters in Control Group
| PWD (ms) | 111.4 ± 14.7 |
| RMS40 (μV) | 6.4 ± 2.6 |
| RMS30 (μV) | 5.7 ± 2.5 |
| RMS20 (μV) | 5.7 ± 2.4 |
| RMSP (μV) | 7.6 ± 2.5 |
| INTP (μV·s) | 669.3 ± 14.3 |
When comparing these parameters in respect with sex (Table 2), we obtained significant differences only for the duration of the filtered P wave, which was higher in men (P = 0.014). The other parameters did not show significant variation with sex.
Table 2.
Variation of P Wave SAECG Parameters with Sex
| Men | Women | Statistical P | |
|---|---|---|---|
| PWD (ms) | 114.11 ± 14.30 | 109.95 ± 14.96 | 0.014 |
| RMS40 (μV) | 6.23 ± 2.61 | 6.56 ± 2.65 | NS |
| RMS30 (μV) | 5.52 ± 2.49 | 5.84 ± 2.46 | NS |
| RMS20 (μV) | 5.53 ± 2.49 | 5.79 ± 2.40 | NS |
| RMSP (μV) | 7.55 ± 2.43 | 7.57 ± 2.51 | NS |
| INTP (μV·s) | 681.29 ± 245.24 | 661.19 ± 248.54 | NS |
We compared SAECG parameters among three age groups (Table 3). P wave duration, RMS40 and RMS30 were significantly correlated with age.
Table 3.
Variation of P Wave SAECG Parameters with Age
| [18–30] Years | [30–50] Years | >50 Years | P for Trend | |
|---|---|---|---|---|
| PWD (ms) | 104.55 ± 11.55 | 109.14 ± 16.16 | 114.45 ± 14.22 | 0.002 |
| RMS40 (μV) | 5.91 ± 2.37 | 6.37 ± 2.37 | 6.64 ± 2.83 | 0.04 |
| RMS30 (μV) | 5.22 ± 2.05 | 5.57 ± 2.27 | 5.94 ± 2.66 | 0.03 |
| RMS20 (μV) | 5.22 ± 2.05 | 5.56 ± 2.28 | 5.90 ± 2.61 | NS |
| RMSP (μV) | 7.53 ± 2.37 | 7.71 ± 2.47 | 7.52 ± 2.51 | NS |
| INTP (μV·s) | 612.00 ± 230.68 | 680.89 ± 252.07 | 678.43 ± 247.37 | NS |
For P wave duration we studied the correlation with age separately by sex (Figs. 1 and 2). In both sex groups PWD was weakly but significantly correlated with age (r = 0.25791, P = 0.004 in men, r = 0.26443, P = 0.007 in women).
Figure 1.
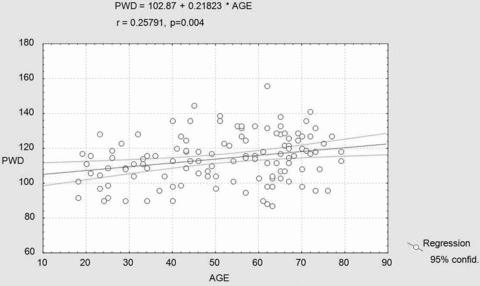
Correlation between PWD (ms) and age (years) in men.
Figure 2.
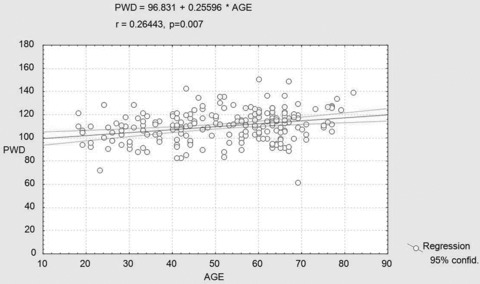
Correlation between PWD (ms) and age (years) in women.
P Wave SAECG in Patients with Converted Persistent Atrial Fibrillation
This group included 31 patients (8 men, 23 women, mean age 60 ± 9.58 years) with PsAF that was electrically converted to sinus rhythm.
There was no uniform trend in the evolution of P wave parameters after 6 months of follow‐up (Table 4).
Table 4.
Variation of P Wave SAECG at 6 Months after Cardioversion
| Initial | 12 Hours | 24 Hours | 3 Months | 6 Months | P Between Groups | |
|---|---|---|---|---|---|---|
| PWD (ms) | 156.90 ± 23.43 | 155.2 ± 25.12 | 157.31 ± 22.41 | 153.57 ± 26.44 | 154.76 ± 25.21 | NS |
| RMS40 (μV) | 6.18 ± 2.75 | 5.96 ± 2.47 | 6.32 ± 3.1 | 6.15 ± 2.49 | 6.07 ± 2.83 | NS |
| RMS30 (μV) | 5.62 ± 3.10 | 5.54 ± 2.84 | 5.63 ± 3.17 | 5.65 ± 3.3 | 5.67 ± 2.98 | NS |
| RMS20 (μV) | 5.21 ± 3.36 | 5.25 ± 3.28 | 5.19 ± 3.14 | 5.23 ± 3.47 | 5.17 ± 3.54 | NS |
| RMSP (μV) | 7.93 ± 2.68 | 8.04 ± 2.94 | 8.24 ± 3.11 | 8.18 ± 2.74 | 8.21 ± 2.82 | NS |
| INTP (μV·s) | 960 ± 341.47 | 964 ± 339.44 | 952 ± 358.14 | 941 ± 374.24 | 943 ± 362.32 | NS |
When comparing P wave SAECG in patients with converted (SAECG obtained immediately after conversion) persistent AF to the control group (Table 5) we obtained highly significant differences regarding P wave duration (156.90 ± 23.43 ms vs 111.52 ± 14.91 ms, P = 0.0001) and the integral of the voltages of the P wave (960 ± 341.47 μV·s vs 669.07 ± 247.09 μV·s, P = 0.0001).
Table 5.
P Wave SAECG in Patients with Converted PsAF versus Control Group
| PsAF – Initial | Control Group | P | |
|---|---|---|---|
| PWD (ms) | 156.90 ± 23.43 | 111.52 ± 14.91 | 0.0001 |
| RMS40 (μV) | 6.18 ± 2.75 | 6.45 ± 2.65 | NS |
| RMS30 (μV) | 5.62 ± 3.10 | 5.72 ± 2.48 | NS |
| RMS20 (μV) | 5.21 ± 3.36 | 5.69 ± 2.45 | NS |
| RMSP (μV) | 7.93 ± 2.68 | 7.57 ± 2.48 | NS |
| INTP (μV·s) | 960 ± 341.47 | 669.07 ± 247.09 | 0.0001 |
Of the 31 patients with converted PsAF, 13 had recurrent episodes that were re‐converted. In these patients PWD was significantly higher than in subjects that maintained sinus rhythm during follow‐up (Table 6).
Table 6.
P Wave SAECG in Patients with Recurrent versus Nonrecurrent PsAF
| Recurrent | Nonrecurrent | P | |
|---|---|---|---|
| PWD (ms) | 168.15 ± 27.01 | 150.44 ± 17.10 | 0.033 |
| RMS40 (μV) | 5.76 ± 1.48 | 6.38 ± 3.44 | Ns |
| RMS30 (μV) | 5.07 ± 1.70 | 5.94 ± 3.88 | Ns |
| RMS20 (μV) | 4.69 ± 1.93 | 5.66 ± 4.18 | NS |
| RMSP (μV) | 7.69 ± 2.86 | 8.05 ± 2.68 | NS |
| INTP (μV·s) | 943.75 ± 343.86 | 965.33 ± 368.02 | NS |
P Wave SAECG in Patients with Converted Paroxysmal Atrial Fibrillation
This group included 57 patients aged 58 ± 11.16 years.
Similar to patients with PsAF, this group had significantly higher values of PWD and INTP (Table 7).
Table 7.
P Wave SAECG in Patients with Converted PxAF versus Control Group
| PxAF – initial | Control group | P | |
|---|---|---|---|
| PWD (ms) | 135.89 ± 21.76 | 111.52 ± 14.91 | <0.001 |
| RMS40 (μV) | 6.68 ± 3.32 | 6.45 ± 2.65 | NS |
| RMS30 (μV) | 5.94 ± 3.17 | 5.72 ± 2.48 | NS |
| RMS20 (μV) | 5.08 ± 3.36 | 5.69 ± 2.45 | NS |
| RMSP (μV) | 7.85 ± 2.9 | 7.57 ± 2.48 | NS |
| INTP (μV·s) | 1043.61 ± 384.70 | 669.07 ± 247.09 | <0.001 |
The 17 patients with recurrent PxAF episodes had higher PWD, and lower RMS40, RMS30, RMS20 (Table 8).
Table 8.
P Wave SAECG in Patients with Recurrent versus Nonrecurrent PxAF
| Recurrent – 17 P | Nonrecurrent – 40 P | P | |
|---|---|---|---|
| PWD (ms) | 154.70 ± 17.19 | 127.90 ± 18.42 | <0.001 |
| RMS40 (μV) | 4.64 ± 2.78 | 7.55 ± 3.18 | 0.002 |
| RMS30 (μV) | 4.05 ± 2.38 | 6.75 ± 3.14 | 0.003 |
| RMS20 (μV) | 3.29 ± 2.11 | 5.85 ± 3.52 | 0.008 |
| RMSP (μV) | 6.70 ± 2.99 | 8.35 ± 2.79 | 0.052 |
| INTP (μV·s) | 1526.17 ± 325.01 | 838.52 ± 304.80 | Ns |
DISCUSSIONS
Signal‐averaged electrocardiography of the P wave (P wave SAECG) is a noninvasive method useful in the prediction of AF risk. 1 , 2 The most predictive parameter is the duration of the filtered P wave.
There is a lack of prospective studies evaluating normal values of the P wave signal‐averaged ECG in healthy individuals. Our study of P wave SAECG parameters in a large normal population showed significant correlations of the duration of the filtered P wave with age and sex. Other indices were not influenced by age or sex.
The mean values of P wave SAECG parameters we obtained could help establish the normal values of these indices.
In a study on 123 healthy subjects Ehrlich et al found a mean P wave duration of 114 ± 13 ms. There was a slight but statistically significant increase in filtered P wave duration with age (r = 0.32, P < 0.001). 3
The P wave duration recorded with the SAECG proved to be an accurate, and independent predictor of AF in various conditions.
In a prospective study of 130 patients with acute myocardial infarction SAECG P wave duration >125 ms was independently associated with AF occurence during 14 days of follow‐up. 4
Steinberg et al. 5 showed that PWD predicted AF episodes after cardiac surgery. The P wave duration on the SAECG was significantly longer in the AF patients than in those without AF: 152 ± 18 versus 139 ± 17 ms (P < 0.001). An SAECG P wave duration >140 ms predicted AF with sensitivity of 77%, specificity of 55%, positive predictive accuracy of 37%, and negative predictive accuracy of 87%.
By comparing the normal population with patients with persistent AF converted to sinus rhythm we demonstrated significant differences in P wave duration and P wave integral.
In our study P wave indices did not change significantly on medium term (6 months) after cardioversion. In a study on 60 subjects with persistent AF who underwent successful electrical cardioversion Chalfoun et al observed no significant differences in P wave SAECG duration immediately after cardioversion between those who remained in sinus rhythm and those who recurred in the follow‐up period. A significant reduction in P wave SAECG duration between 30 days and immediately after cardioversion was reported in those who remained in sinus rhythm. The only predictors of AF recurrence were left ventricular hypertrophy and previous AF duration. 6 Other studies have shown an improvement of P wave parameters after conversion of lone AF, that could suggest a reverse electrical remodeling. 7 Our study does not support reverse electrical remodeling on the short term.
Patients with recurrent persistent AF had significantly higher P wave duration than patients without reoccurrence after cardioversion. Other parameters were not significantly correlated.
The study of patients with paroxysmal AF, compared to the control group, showed significant increase of the same parameters: P wave duration and integral of the P wave.
Moreira et al. following 181 patients (117 with confirmed PxAF and 64 without PxAF) showed that the best parameters to distinguish patients with or without paroxysmal AF were the filtered P wave duration and the P wave late potential durations below 3 μV. 8
Similarly to our results, Dhala et al. in a study comparing 199 normal controls and 81 patients with paroxysmal AF found that the filtered P wave duration and P wave integral were significantly different between the two groups (filtered P wave duration 120 ± 9 ms vs 145 ± 21 ms and P wave integral 666 ± 208 μV·s vs 868 ± 352 μV·s), whereas RMS20, RMS30, RMS40 showed no significant differences. 9
Patients with recurrent paroxysmal AF had higher PWD and lower RMS40, RMS30, RMS20 than patients without reoccurrence of AF.
Maintaining sinus rhythm after conversion of AF is an important objective. Identifying patients with high risk for AF reoccurence could help establish an adequate antiarrhythmic treatment, and P wave SAECG parameters (especially filtered P wave duration), may be useful in the risk stratification in these patients.
CONCLUSION
We measured P wave SAECG parameters in a large normal population. Filtered P wave duration measured was higher in men, and PWD was weakly but significantly correlated with age, both in men and women. Comparing the normal population with patients with paroxysmal or persistent AF converted to sinus rhythm demonstrated significant differences in P wave duration and P wave integral. There was no significant change in SAECG parameters in the first 6 months after cardioversion. Patients with recurrent AF had significantly higher P wave duration than patients without reoccurrence after cardioversion.
REFERENCES
- 1. Hutchinson LA, Steinberg JS. A prospective study of AF after cardiac surgery: Multivariate risk analysis using P wave signal‐averaged ECG and clinical variables. Ann Noninvas Electrophysiol 1996;1:133–140. [Google Scholar]
- 2. Ehberth FM, Zaman N, Steinberg JS. Immediate and short‐term reproducibility of the P‐wave signal‐averaged electrocardiogram. Pacing Clin Electrophysiol 1997;20:1636–1645. [DOI] [PubMed] [Google Scholar]
- 3. Ehrlich JR, Zhang GQ, Israel CW, et al P‐wave signal averaging‐ECG: Normal values and reproducibility. Z Kardiol 2001;90(3):170–176. [DOI] [PubMed] [Google Scholar]
- 4. Rosiak M, Bolinska H, Ruta J. P wave dispersion and P wave duration on SAECG in predicting atrial fibrillation in patients with acute myocardial infarction. Ann Noninvasive Electrocardiol 2002;7(4):363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Steinberg JS, Zelenkofske S, Wong SC, et al Value of the P‐wave signal‐averaged ECG for predicting atrial fibrillation after cardiac surgery. Circulation 1993;88(6):2618–2622. [DOI] [PubMed] [Google Scholar]
- 6. Chalfoun N, Harnick D, Pe E, et al Reverse electrical remodeling of the atria post cardioversion in patients who remain in sinus rhythm assessed by signal averaging of the P‐wave. Pacing Clin Electrophysiol 2007;30(4):502–509. [DOI] [PubMed] [Google Scholar]
- 7. Barbosa EC, Benchimol‐Barbosa PR, Bomfim Ade S, et al Reversal atrial electrical remodeling following cardioversion of long‐standing lone atrial fibrillation. Arq Bras Cardiol 2009;93(3):213–220. [DOI] [PubMed] [Google Scholar]
- 8. Moreira JO, Moffa PJ, Uchida AH, et al The signal‐averaged electrocardiogram of atrial activation in patients with or without paroxys mal atrial fibrillation. Arq Bras Cardiol 2006;87(5):564–569. [DOI] [PubMed] [Google Scholar]
- 9. Dhala A, Underwood D, Leman R, et al Multicenter PHi‐Res Study. Signal‐averaged P‐wave analysis of normal controls and patients with paroxysmal atrial fibrillation: A study in gender differences, age dependence, and reproducibility. Clin Cardiol 2002;25(11):525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]


