Abstract
Recent studies suggest that the electrocardiographic (ECG) finding of J‐point ST‐elevation, the early repolarization syndrome, is not as benign as earlier believed. Three important articles published in 2008/2009 suggest that this finding in the inferolateral leads of the ECG may be representing a risk for subsequent ventricular fibrillation. Although these retrospective studies do justify a careful evaluation of persons with this electrocardiographic pattern, especially of those with syncope or ventricular arrhythmias and/or family history of sudden cardiac death, it seems to be unjustified to consider it today to be a marker for high risk for sudden cardiac deaths in a general population. Even in athletes, early repolarization was found to increase only minimally their arrhythmic risk. In spite of certain similarities with the Brugada syndrome, their association is far from being proved. Prospective studies and further electrophysiological and genetic information will help to clarify the clinical significance of this syndrome.
Ann Noninvasive Electrocardiol 2011;16(2):192–195
Keywords: electrocardiography, electrophysiology, early repolarization, sudden death
Since the 1930s, several investigators have noted that ST‐segment elevation at the QRS‐ST junction ("the J‐point") is not infrequently a benign ECG feature. Grant et al. 1 seem to be the ones who first used the term “early repolarization” (ER) to describe this electrocardiographic phenomenon and its benign nature, even if accompanied by a terminal QRS notch, has not been questioned for several decades (Fig. 1).
Figure 1.
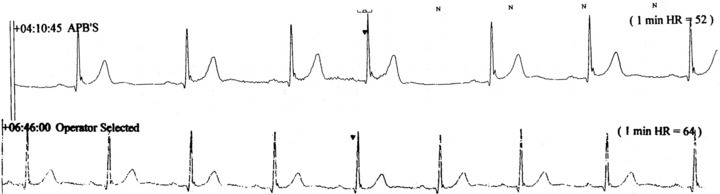
Upper panel, Holter recording: relatively high terminal QRS notch and J‐point ST‐elevation, at heart rate of 52/min. Lower panel: Holter recording on the same day, at heart rate of 64/min: notching and J‐point elevation hardly seen.
An investigation by Haissaguerre and coworkers reported in May 2008, 2 disclosed some surprisingly new data on ER syndrome. This group reviewed data from 2006 on subjects from 22 centers from nine different countries resuscitated after cardiac arrest due to idiopathic ventricular fibrillation (VF). ER was defined as an elevation of the QRS‐ST junction of at least 0.1 mV from baseline in the inferior or lateral lead, manifested as QRS slurring or notching; this pattern was significantly more frequent in the case subjects than in control subjects. Furthermore, during a 5‐year mean follow‐up, defibrillator monitoring showed a higher incidence of recurrent VF in case subjects with repolarization abnormality than in those without.
Later in 2008, Rosso et al. 3 found that J‐point elevation in the inferior leads and in leads I and aVL was more common among the 45 patients with idiopathic VF than among age‐ and gender‐matched control subjects: J‐point elevation V4–6 occurred with equal frequency among patients and matched control subjects. The presence of ST‐elevation or QRS slurring did not add diagnostic value to the presence of J‐point elevation. The authors calculated that an incidental finding of a J wave during screening should not be interpreted as a marker of “increased risk” because the odds for this fatal disease would still be roughly 1:10,000.
From Finland came the third investigation: Tikkanen et al. in 2009 found 4 J‐point elevation ≥0.1 mV in inferior leads in about 6% of the subjects; this finding was associated with a tendency for increased risk (P = 0.03) of cardiac deaths. With a J‐point elevation >0.2 mV, this risk and deaths from arrhythmias became statistically significant.
Editorial comments and Letters to the Editor demonstrated the great interest these three investigations arose. Dr. Wellens 5 seemed to be convinced by the findings of the Haissaguerre group can be important to detect high risk for VF of persons with a history of unexplained syncope or a familial incidence of sudden death at a young age. On the other hand, Dr. Littmann pointed out that inferior J‐point elevation may signify periinfarction block 6 that would indicate latent ischemic heart disease and therefore this ECG sign should prompt clinicians to consider latent ischemic heart disease before attributing the J‐point elevation to a primary electrical abnormality. Dr. Viskin expressed his view 7 that there is too much overlapping between VF patients and control subjects in terms of J‐wave amplitude and that asymptomatic patients with J waves should not undergo further testing.
Merchant et al. 8 observed that QRS notching is more prevalent in the malignant variants of ER than in the benign cases, findings that could have important implications for risk stratification of patients with ER. In the healed phase of myocardial infarction, patients with implantable cardioverter‐defibrillators (ICDs) had ER pattern in ≥2 leads significantly more frequently than controls, noted more commonly in inferior leads. 9
TREATMENT OF ER
While no investigations were carried out on the treatment of ER as long as it was looked upon as a benign phenomenon without clinical significance, the recent informations raised interest in a possible drug therapy of this condition. Haissaguerre and coworkers, 10 based on their experience on their cohort of 122 patients with idiopathic VF and ER abnormality in the inferolateral leads, concluded that the electrical storms in these patients, all having ICDs implanted, were unresponsive to beta‐blockers, lidocaine/mexiletine, and verapamil, while amiodarone was partially effective (in three of 10). Two specific drugs were efficient to abolish and prevent recurrences of VF in these patients: isoproterenol infusion immediately suppressed electrical storms in all patients used, while quinidine was successful, decreasing recurrent VF to nil in all cases used, and also restored a normal ECG (Table 1).
Table 1.
Treatment of Early Repolarization Syndrome 15
| Effective | |
|---|---|
| Beta‐blockers | No |
| Lidocaine | No |
| Mexiletine | No |
| Verapamil | No |
| Quinidine | Yes |
| Isoproterenol IV for electrical storms | Yes |
| Amiodarone | Partially |
Implantation of ICDs were mentioned by Benito et al. 11 in their recent review article to be justified in individuals at “very high risk” and pacemaking to prevent bradycardia or increase resting heart rate in some “at‐risk” individuals, although no references were provided for the use of these procedures.
ER: A BRUGADA SYNDROME (BS) VARIANT?
In the wake of the new observations about ER creating a hazard for VF, the assumption was raised that we are dealing with a variant of BS. Although a relatively recent consensus report on BS defined the ST‐elevation of these patients strictly to the right precordial leads, 12 it has subsequently been reported 13 that 11% of the classical BS patients exhibit spontaneous ER or coved ≥2 mm ST‐elevation pattern in the inferiorlateral leads, while in three patients, the coved Brugada pattern was only present in the inferior leads; the authors suggested that such patients should also be diagnosed with BS. Similar findings and conclusions were reported by Letsas et al. 14 (Table 2).
Table 2.
Diagnosis of Early Repolarization Syndrome and Differential Diagnosis with Brugada Syndrome
| ER Syndrome | Brugada Syndrome | |
|---|---|---|
| Right BBB | Not requested | Requested |
| ST‐elevation | In L1, aVL, V4–6 | In V1–2 |
| QRS notch or slurring | Frequent | Absent |
| Shape of | Upper | Coved |
| ST‐elevation | Concave |
While a certain overlap obviously exists between ER syndrome and BS, a difference was found between the mode of onset of VF in these two types of patients. Nam et al. 15 found that a transient augmentation was indicative of a highly arrhythmogenic substrate heralding multiple episodes of VF in patients with ER. VT/VF initiation was more commonly associated with a short‐long‐short sequence and premature ventricular contractions displayed a shorter coupling interval in patients with ER compared with those with BS (Table 3).
Table 3.
Mode of Onset of VF in ER Syndrome versus Brugada Syndrome 19
| ER Syndrome | Brugada Syndrome | P Value | |
|---|---|---|---|
| Initiated by PVCs with a short‐long‐short sequence | In 72.4% | In 15.1% | <0.01 |
| Coupling intervals, ms | 328 | 395 | <0.01 |
Antzelevitch and Yan in their recent article 16 proposed to join ER and BS under the name “J‐wave syndromes” (in plural), as they considered them to represent a continuous spectrum of phenotypic expression; they propose three subtypes: type 1, with the ECG pattern predominantly seen in the lateral precordial leads is prevalent among healthy male athletes (see below); type 2, with the ER pattern seen predominantly in the inferior or inferolateral leads and is associated with a higher level of risk; and type 3, in which the ER pattern is displayed globally in the inferior, lateral, and right precordial leads, is associated with the highest level of risk for development of malignant arrhythmias. BS is the fourth type.
ER PATTERN IN ATHLETES
J wave, QRS slurring, and/or ST‐segment elevation in athletes with cardiac arrest in the absence of heart disease, was studied recently by Cappato et al. 17 The first two pathologies, without ST‐elevation in the inferior and lateral leads, were significantly more frequently found in these subjects than in control athletes. The authors expressed their opinion that since these changes could reflect an underlying abnormality of repolarization, their myocardium may be more sensitive to various, still not well‐defined arrhythmogenic triggers, the incidental finding of a J wave/QRS slurring in a healthy athlete should be considered as a marker that minimally increases the arrhythmic risk. Sport‐induced rate‐dependent repolarization inhomegeneities also may have been precipitating factors in creating the characteristic ECG patterns, known as ER or “vagotonic heart” in athletes. 18 Bianco and Zeppilli 19 found ER in the ECG of 89% of competitive athletes, none of them has suffered from major ventricular arrhythmias from the time of their study onward; they considered ER to be a complete benign phenomenon, even reversible after a few months of detraining.
ELECTROPHYSIOLOGICAL OBSERVATIONS: ER OR LATE DEPOLARIZATION
As noted, for decades the ST‐elevation starting at or near the J‐point, was unequivocally related to the mechanism of early‐phase repolarization and the transmural voltage gradient during the initial phase of the ventricular repolarization was described as the cellular basis of the J wave. 20
This unequivocal relation of the J wave appearance to ER was questioned by Wilde et al. 20 Although dealing with type 1 BS, the conclusion of Postema et al. 21 that the ECG abnormalities can be attributed to localized depolarization abnormalities, notably terminal conduction delay in the right ventricle, with the repolarization derangements secondary to these, can most probably extrapolated to the ER syndrome as well. Indeed, Drs. Borggrefe and Schimpf 22 devoted their Editorial Comment to “J wave syndromes” (also in plural), stressing that the two divergent use on the fundamental mechanisms underlying the coved‐type diagnostic Brugada ECG, and apparently the ER syndrome as well, are indicative of our limited knowledge of the molecular basis and clinical presentation of a major clinical problem.
As it happens frequently when two mechanisms are supposed to be at work, we may find out that actually both are real. Nishii et al. 23 found in 135 patients abnormal action potential duration restitution properties and conduction delays and concluded that both repolarization and depolarization abnormalities are related to the development of VF; although their conclusion was deducted from endocardial monophasic action potential in BS patients, we may assume that their conclusion is applicable for ER patients as well.
WORDS OF CAUTION
In spite of the new evidences about the association of ER and the risk of idiopathic VF, Myerburg and Castellanos 24 expressed their opinion that the data presented so far do not permit distinction between ER as a single pathophysiological entity with variable expression, or that ER is a nonspecific ECG pattern that might be associated with specific high‐risk or low‐risk entities. Finally, we should not discard the opinion of Dr. Borys Surawicz (personal communication, July 2010) who feels that we are witnessing the “birth of illegitimate nomenclature” and who discourages the use of “J wave Syndromes” as one that cannot be defined and the use of “Early Repolarization Syndromes” that have not been defined by standard ECG terminology.
Acknowledgments
Acknowledgments: The excellent secretarial help of Ms. Estelle Rachamim‐Rayman is greatly acknowledged.
REFERENCES
- 1. Grant RP, Estes EH, Doyle JT. Spacial vector electrocardiography. The clinical characteristics of S‐T and T vectors. Circulation 1951;3:182–347. [DOI] [PubMed] [Google Scholar]
- 2. Haissaguerre M, Derval N, Sacher F, et al Sudden cardiac arrest associated with early repolarization. N Eng J Med 2008;358:2016–2023. [DOI] [PubMed] [Google Scholar]
- 3. Rosso R, Kogan E, Belhassen B, et al J‐point elevation in survivors of primary ventricular fibrillation and matched control subjects. J Am Coll Cardiol 2008;52:1231–1238. [DOI] [PubMed] [Google Scholar]
- 4. Tikkanen JT, Anttonen O, Junttila J, et al Long‐term outcome associated with early repolarization on electrocardiography. New Eng J Med 2009;362:2529–2537. [DOI] [PubMed] [Google Scholar]
- 5. Wellens HJ. Early repolarization revisited. New Eng J Med 2008;358:2063–2065. [DOI] [PubMed] [Google Scholar]
- 6. Littmann L. Early repolarization on electrocardiography. N Eng J Med 2010;362:1148. [DOI] [PubMed] [Google Scholar]
- 7. Viskin S. Idiopathic ventricular fibrillation “le syndrome d'Haisaguerre” and the fear of J waves. J Am Coll Cardiol 2009;53:620–622. [DOI] [PubMed] [Google Scholar]
- 8. Merchant FM, Noseworthy PA, Weiner RB, et al Ability of terminal QRS notching to distinguish benign from malignant electrocardiographic forms of early repolarization. Am J Cardiol 2009;104:1402–1406. [DOI] [PubMed] [Google Scholar]
- 9. Patel RB, Ng J, Reddy V, et al Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease. Circ Arrhythm Electrophysiol 2010;3:489–495. [DOI] [PubMed] [Google Scholar]
- 10. Haissaguerre M, Sacher F, Nogami A, et al Characteristics of recurrent ventricular fibrillation associated with inferolateral early repolarization. J Am Coll Cardiol 2009;53:612–619. [DOI] [PubMed] [Google Scholar]
- 11. Benito B, Guasch E, Rivard L, et al Clinical and mechanistic issues in early repolarization: Of normal variants and lethal arrhythmia syndromes. J Am Coll Cardiol 2010;56:1177–1186. [DOI] [PubMed] [Google Scholar]
- 12. Wilde AAM, Antzelevitch C, Borggrefe M, et al For the Study Group on the molecular basis of arrhythmias of the European Society of Cardiology. Proposed diagnostic criteria for the Brugada syndrome. Europ Heart J 2002;23:1648–1654. [DOI] [PubMed] [Google Scholar]
- 13. Sarkozy A, Chierchia G‐B, Paparella G, et al Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol 2009;2:154–161. [DOI] [PubMed] [Google Scholar]
- 14. Letsas KP, Sacher F, Probst V, et al Prevalence of early repolarization pattern in inferolateral leads in patients with Brugada syndrome. Heart Rhythm 2008;5:1685–1689. [DOI] [PubMed] [Google Scholar]
- 15. Nam GB, Ko KH, Kim J, et al Mode of onset of ventricular fibrillation in patients with early repolarization pattern vs. Brugada syndrome. Eur Heart J 2010;31:330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Antzelevitch C, Yan GX. J wave syndromes. Heart Rhythm 2010;7:549–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cappato R, Furlanello F, Giovinazzo V, et al J wave, QRS slurring and ST elevation in athletes with cardiac arrest in the absence of heart disease: Marker of risk or innocent bystander? Circ Arrhythm Electrophysiol 2010;3:305–311. [DOI] [PubMed] [Google Scholar]
- 18. Barbosa EC, Bomfim AS, Benchimol‐Barbosa PR, et al Ionic mechanisms and vectorial model of early repolarization pattern in the surface electrocardiogram of the athlete. Ann Noninvasive Electrocardiol 2008;13:301–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bianco M, Zeppilli P. Early repolarization in the athlete. J Am Coll Cardiol 2009;53:2199–2200. [DOI] [PubMed] [Google Scholar]
- 20. Wilde AAM, Remme CA, Derksen R, et al Brugada syndrome. Europ Heart J 2002;23:675–678. [DOI] [PubMed] [Google Scholar]
- 21. Postema PG, van Dessel PFHM, Kors JA, et al Local depolarization abnormalities are the dominant pathophysiologic echanism for type 1 electrocardiogram in Brugada syndrome. J Am Coll Cardiol 2010;55:789–797. [DOI] [PubMed] [Google Scholar]
- 22. Borggrefe M, Schimpf R. J‐wave syndromes caused by repolarization or depolarization mechanisms: A debated issue among experimental and clinical electrophysiologists. J Am Coll Cardiol 2010;55:798–800. [DOI] [PubMed] [Google Scholar]
- 23. Nishii N, Nagase S, Morita H, et al Abnormal restitution of action potential duration and conduction delay in Brugada syndrome: Both repolarization and depolarization abnormalities. Europace 2010;12:544–552. [DOI] [PubMed] [Google Scholar]
- 24. Myerburg RJ, Castellanos A. Early repolarization and sudden cardiac arrest: Theme or variation on a theme? Nat Rev Cardiol 2008;5:760–761. [DOI] [PubMed] [Google Scholar]


