Abstract
Several publications considering anatomical, histological, pathological, electrocardiographic, vectorcardiographic, and electrophysiologic studies have shown that the left bundle branch splits into three fascicles or in a “fan‐like interconnected network” in the vast majority of human hearts. The left His system is trifascicular with a left anterior, a left posterior, and a left septal fascicle (LSF). Consequently, the classic term “hemiblock,” to describe the block of one of the fascicles, established several decades ago by the Rosembaum's school, should be updated.
Electrovectorcardiographic changes resulting from conduction abnormalities of the left anterior and left posterior fascicles are commonly diagnosed, mainly by their changes in the frontal plane. However, the existence of conduction defects of the LSF remains controversial. The ECG/VCG hallmark of LSF block is prominent anterior QRS forces (PAF) on the horizontal plane. This ECG/VCG phenomena should be distinguished from other conditions that also produce anterior QRS shift in the HP as: normal variants, right ventricular enlargement, misplaced precordial leads, lateral myocardial infarction, right bundle branch block, Wolff‐Parkinson‐White, obstructive and nonobstructive forms of hypertrophic cardiomyopahty, diastolic left ventricular enlargement, endomiocardial fibrosis, Duchenne muscular dystrophy, and dextroposition.
The two highly frequent etiologies of LSFB are ischemia (coronary artery disease (CAD) with critical proximal obstruction of the left anterior descending coronary artery) and, in Latin America, Chagas’ cardiomyopathy.
The aims of this review are to revise the evidence of the existence of a trifascicular left Hissian system and to help in the ECG/VCG recognition of the LSFB.
Ann Noninvasive Electrocardiol 2011;16(2):196–207
Keywords: heart conduction system, fascicular block, bundle of his, electrocardiography
INTRODUCTION
The three left fascicles of the left bundle branch (LBB) along with the right bundle branch (RBB), constitute the quadrifascicular structure of the intraventricular conduction system of the heart, coined by Dr. Uhley. 1 , 2
Anatomical Considerations of the Left Intraventricular Conduction System
Anatomopathological studies showed that the left septal fascicle (LSF) has diverse morphologies and considerable variability in its structure. Thereby, six basic anatomical variations can be described3, 4, 5, 6, 7:
-
•
Type I: the LSF arises independently from the main LBB (65% of the cases).
-
•
Type II: the LSF originates from the left anterior fascicle (LAF) of the LBB.
-
•
Type III: the LSF originates from the left posterior fascicle (LPF). This type represents about 2.4% of all cases.
-
•
Type IV: the LSF originates concomitantly with the other two fascicles (LAF and LPF).
-
•
Type V: the LSF is represented as a “fan‐like interconnecting network.”
-
•
Type VI: the LSF is absent; consequently, the left Hissian intraventricular system has only two fascicles: LAF and LPF. It occurs in approximately 15% to 40% of the cases. 3
a. Blood Supply (modified from reference 8)
The blood supply of the human His bundle and its proximal branches have a dual origin, with anastomoses within the His bundle. The conduction system is supplied as follows:
-
1
His bundle: it has a dual supply by the AV node artery from the right coronary artery (RCA) and the first septal branch of the left anterior descending artery (LAD) in 90% of the cases, and entirely supplied by the AV node artery in 10% of the cases.
-
2
Proximal right bundle branch: it is supplied by both the AV node artery and the septal branch in 50% of the cases, and only by the septal branch in 40% of the cases. The AV node artery as a single supply occurs in about 10% of the cases.
-
3
Left bundle branch: it is supplied by the AV node artery (ramus septi fibrosi) from the RCA (in 90% of the cases) and ramus septi ventriculorum superior and ramus critae, branches of the LAD.
-
4
Left branch fascicles or divisions branches supply: see Table 1
Table 1.
Blood Supply of the Left Branch Fascicles or Divisions
| Responsible system | LAF (%) | LPF (%) | LSF (%) |
|---|---|---|---|
| LAD branches | 40 | 10 | 100 |
| Double irrigation (LAD & RCA) | 50 | 40 | 0 |
| RCA branches | 10 | 50 | 0 |
LAD = left anterior descending artery; RCA = right coronary artery.
The LSF is supplied exclusively by the septal perforating branches of the LAD. 9 Critical lesions of the LAD before the first septal perforating branch are the main cause of LSFB in developed countries, and it is a major determinant of predominant anterior forces (PAF) from V1 to V3 during acute myocardial ischemia. 10 In Brazil, where Chagas’ disease is very common, coronary artery disease represents only 18% of all LSFB.
LSFB can be also related to exercise‐induced ischemia, 11 sometimes leading to giant R waves in the precordial leads. 12 , 13 , 14 , 15
Sudden development of LSFB in critical LAD lesions indicates a proximal location of the lesion, and therefore, a worse prognosis.
b. Electrophysiology of the Left Intraventricular Conduction System
The electrophysiologic demonstration of the activation of the middle third of the left septal surface 5 ms before the anterosuperior and posteroinferior regions was made in 1970 by Durren et al. 16 They demonstrated in 870 intramural terminals of isolated human hearts, that three endocardial areas were synchronously excited from 0 to 5 ms after the initiation of the left ventricle (LV) activity potential. To demonstrate the time course and instantaneous distribution of the excitatory process of the normal human heart, the authors studied isolated human hearts from seven individuals who died from neurologic disease with no history of cardiac disease. The first LV areas excited were located in the following regions:
-
1
High on the anterior paraseptal wall just below the insertion of the anterolateral papillary muscle (ALPM) where the LAF ends;
-
2
Central on the left surface of the intraventricular septum (IVS), where the LSF ends. Septal activation started in the middle third of the left side of the IVS, in the anterior and lower third at the junction of the IVS and posterior wall.
-
3
The LSF, the left middle septum surface, and the inferior two‐thirds of the septum originate the first vector 17
-
4
Posterior paraseptal, about one third of the distance from the apex to the base, near the insertion of the posteromedial papillary muscle (PMPM), where the LPF ends. The posterobasal area is the last part of the LV to activate.
Rosenbaum et al. 18 , 19 postulated that the activation of the middle‐septal region occurs in most cases, from the anterior “false tendons” that originate from the LPF. His group considered that the LPF in its final portion opens as a fan, and the anterior “pseudo‐tendons” are those responsible for the activation of the middle‐septal region. We think that in fact, only one of the anatomical variations of the LSF (type III), is precisely the one that originates on the LPF (2.4% of cases).
Another consideration should be done to the electrophysiologic explanation of the so called “atypical LBBB.” There are cases of divisional or fascicular LBBB (LAFB + LPFB) that depict a Q wave in the left leads, turning the electrocardiographic pattern of LBBB “atypical.” Alboni et al 17 called them “LBBB with normal septal activation.”
Rosenbaum et al. 19 called the same phenomenon “left intraventricular blocks without changes in the initial portion of the QRS.” His group did not provide an explanation for these cases, and stated in their traditional book, that they were “difficult to explain.”
Medrano et al. 20 proposed that in these atypical LBBB cases, the fibers of the LSF would originate prior to the site or area of the block in the LPF and LAF, so the middle‐septal activation is preserved (vector 1 or anteromedial or septal vector, representing the initial 10 ms of the left surface), originating the Q waves of leads V5‐V6, and turning the LBBB into an atypical one.
Gambeta and Childers 21 also proposed the trifascicular nature of the left Hissian system. The authors observed the development of transient abnormal Q waves during exercise as the heart rate increased. This phenomenon was attributed to transient tachycardia‐dependent ischemic block in the LSF. The initial activation is conducted by the non blocked divisions (LAF and LPF). Since these fascicles have opposite directions and LPF activation predominates over LAF, produces the appearance of initial Q wave in intermediate precordial leads.
The same phenomenon was observed during the acute phase of myocardial infarction with the same electrophysiological explanation. 22 , 23
Another strong argument for the existence of LSFB, was provided by several electrophysiological animal and human models. They showed the development of PAF (anterior shift of QRS loop) as a manifestation of intraventricular block, a consequence of intermittent intraventricular dromotropic disorder in the LSF region, during atrial extrastimuli. 24 , 25 , 26 , 27 , 28 , 29 , 30
A delay in the LSF may explain certain type of ventricular aberration pattern observed by introducing premature atrial beats. This pattern consists of PAF with no or minimal QRS duration prolongation (≤20 ms) and without incomplete RBBB. Such delay is manifested as a narrow QRS with anterior shift in the HP, but no axis shift in the FP. It is important to recognize this aberration, because it may mimic the ECG findings of lateral MI (true posterior MI of the “old nomenclature”) or RVH. 31
In another study, aberrant ventricular conduction was induced in 44 subjects by introduction of atrial premature beats. The distribution of the patterns were RBBB (28); LAFB combined with RBBB (21); LAFB (17); LPFB combined with RBBB (12); LPFB (10); complete LBBB (10) and incomplete LBBB (6).
Other configurations could not be classified into the usual categories of intraventricular blocks. In 7 of them, the alterations only consisted on trivial modifications of the QRS contour. In the other 5, aberrant conduction manifested itself by conspicuous PAF of the QRS loop on the HP. The latter observation is worthy of notice, as it indicates that, in the differential diagnosis of the VCG pattern characterized by PAF, conduction disturbances should be considered a possible etiological factor in addition to RVH, and true posterior MI. 28 , 29 , 30
Related the historical controversy about the bifascicular or trifascicular nature of the human left His system, we conclude that in most cases, the left His system is trifascicular. Consequently, the term “hemiblock,” to refer to the block of the fascicles, should be avoided. 32 , 33 , 34
NOMENCLATURE USED IN LITERATURE
There is a large variety of nomenclatures to name the LSF. This indicates the need of a consensus to unify terminology. This discussion should take place in an International or Worldwide Conference on Electrocardiology. The authors of this review strongly advocate for such a consensus.
In Brazil, a committee of experts in Resting Electrocardiology met in 2003 and developed the “Brazilian Guidelines for Interpretation of Resting Electrocardiogram.” In this consensus, the diagnostic criteria of LSFB were determined and published. 35 However, it is important to remember different terminologies used in the literature: (1) left septal fascicular block (LSFB). 13 , 36 , 37 , 38 , 39 , 40 , 41 , 42 This is the currently accepted terminology and frequently used in more recent publications; (2) septal fascicle of the left bundle branch 43 ; (3) focal septal block 22 ; septal focal block 21 ; (4) left parietal septal block 44 , 45 ; (5) septal fascicular conduction disorders of the left branch 46 ; (6) left septal Purkinje network block 47 , 48 ; (7) left anterior septal block 49 ; (8) anterior fascicular block 50 ; (9) left septal subdivision block of the left bundle branch 31 , 51 , 52 ; (10) left median hemiblock 53 ; 54 ; (11) middle subdivision block of the left bundle branch 55 ; (12) middle fascicle block 17 ; (13) block of the antero‐medial division of the left bundle branch of His 15 ; (14) anteromedial divisional block (AMDB) 12 ; (15) block of the anterior median branch of the bundle of His; (16) blocking of the anterior‐medial Ramulus 56 ; (17) anterior conduction delay 29 , 31 , 52 and (18) intraventricular aberrant conduction. 26 , 57
We conclude that the various denominations only reflect the disparity of opinions on the existence of an anatomic structure defined as LSF. There are still some reasonable doubts on its electrophysiological properties and the effect of its disturbances (delay, block) on the surface ECG.
This group of authors does not consider themselves the “owners of the truth,” and advocate for an international consensus to find a single terminology, based on a common interpretation of the literature. This will help to recognize this frequently misdiagnosed disorder and will help researchers to organize and focus their opinions on this issue.
LEFT SEPTAL FASCICULAR BLOCK: POSSIBLE ETIOLOGIES
The following list identifies possible causes of LSFB recognized in the literature:
-
1
Ischemia: Coronary Artery Disease (CAD) with critical lesion of proximal LAD and/or its septal branches before the first septal perforating branch. 11
-
2
Chronic Chagas’ Cardiomyopathy: main cause of LSFB in Latin America. 49
-
3
Non‐Obstructive Hypertrophic Cardiomyopathy (NO‐HCM). 58
- 4
-
5
Diabetes Mellitus. 46
-
6
Kearns‐Sayre syndrome. 61
LEFT SEPTAL FASCICULAR BLOCK: ELECTROCARDIOGRAPHIC CRITERIA 36 , 38 , 40 , 41 , 42 , 62 , 63
-
1
Normal QRS duration or minimal widening (up to 110 ms). If LSFB is associated with other fascicular or bundle blocks, the QRS could be wider than 120 ms.
-
2
Frontal plane leads with normal QRS duration and amplitude.
-
3
Increased ventricular activation time or intrinsic deflection in leads V1 and V2≥ 35 ms.
-
4
R wave voltage of lead V1≥ than 5 mm.
-
5
R/S ratio in lead V1 > 2.
-
6
R/S ratio in lead V2 > 2.
-
7
S wave depth in lead V1 < 5 mm.
-
8
Small Q wave in leads V2, V3 or V1 and V2.
-
9
R wave of lead V2 > 15 mm.
-
10
RS or Rs pattern in leads V2 and V3 (frequent rS in V1) with R wave “in crescendo” from V1 through V3 and decreasing from V5 to V6.
-
11
Absence of Q wave in left precordial leads V5, V6 and I (by absence of vector 1 or antero‐medial or septal vector, representing the initial 10 ms of the left surface).
-
12
Intermittent PAF during hyperacute phase of myocardial infarction, 63 exercise stress testing in patients with severe myocardial ischemia 11 , 12 and during early atrial extrastimuli. 29
-
13
Intermittent rate‐dependent Q wave in leads V1 and V2. 21
The authors have provided a classification of the above ECG diagnostic criteria in Major and Minor criteria according to their relevance in:
I) Major Criterion
-
1)
Intermittent PAF: intermittent or transient increment in the R wave voltage in intermediary precordial leads and intermittent or transient anterior displacement of the QRS loop on HP.
II) Minor Criteria
All the other criteria mentioned above.
The diagnosis of LSFB could be done with 1 major criterion or with 2 minor criteria.
The Brazilian Guidelines for Interpretation of Resting Electrocardiogram 35 defined the following ECG criteria for diagnosis of LSFB:
-
1
QRS duration <120 ms, (closer to 100 ms). The development of LSFB does not increase QRS duration by more than 25 ms, due to multiple interconnections between the fascicles of the LBB (“passage way zone” as defined by Rosenbaum). The QRS complex is slightly prolonged (between 100 ms and 115 ms). Thus, LSFB pattern with a prolonged QRS duration indicates the presence of additional conduction disturbances such as other fascicular blocks, RBBB, MI, focal block, or a combination of any of them;
-
2
R wave in leads V1 or V2 and V3 of 15 mm;
-
3
Increased R wave voltage in all intermediary precordial leads and decreased voltage in leads V5 and V6;
-
4
Early transition from lead V1 to V2;
-
5
Absence of QRS axis shift;
-
6
Predominantly negative T waves in the right precordial leads (due to ischemia involving the proximal third of the LAD).
All the above mentioned criteria are valid in the absence of RVH, septal hypertrophy or lateral MI, and other causes of PAF.
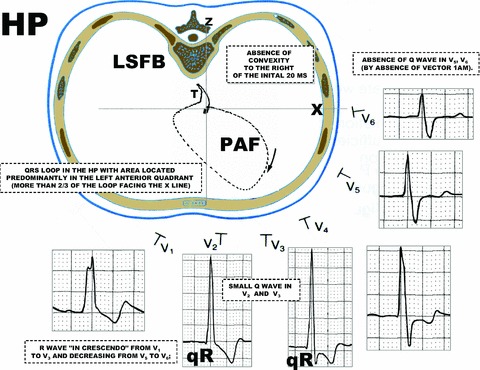
LEFT SEPTAL FASCICULAR BLOCK: VECTORCARDIOGRAPHIC CRITERIA (ALL IN THE HP) 15 , 53 , 54
QRS loop in the HP with an area predominantly located in the left anterior quadrant (>2/3 of the loop facing the orthogonal X lead: 0° to ±180°);
-
1
Absence of normal convexity to the right, of the initial 20 ms of the QRS loop.
-
2
Discrete dextro‐orientation with moderate delay of the vector from 20 to 30 ms.
-
3
Anterior location of the vector from 40 to 50 ms;
-
4
Posterior location with a reduced magnitude of the vector from 60 to 70 ms.
-
5
Maximal vector of the QRS loop located to the right of +30°.
-
6
Intermittent or transient anterior displacement of the QRS loop.
-
7
T loop with posterior orientation tendency (useful for the differential diagnosis with posterior MI).
-
8
The QRS loop rotation may be:
-
8a
Counterclockwise: incomplete LSFB.
-
8b
Clockwise: advanced or complete LSFB or in association with complete RBBB, LAFB, or LPFB.
Typical examples of LSFB are shown in 1, 1, 1, 2, 2, 2. Figures 3 and 4 show examples of intermittent or transient exercise‐related LSFB.
Figure 1.
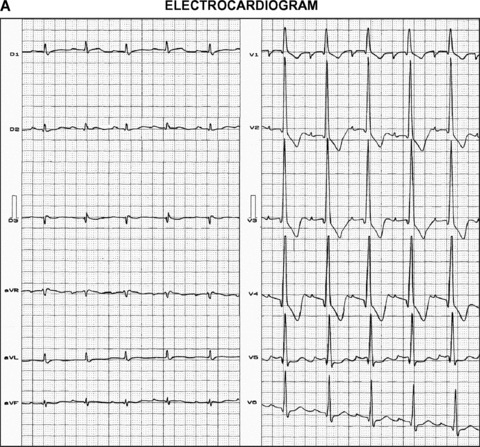
(A) This ECG belongs to a 75‐year‐old male with severe congestive heart failure and severe CAD. LAD: 100%; left circumflex: 100%, RCA: 90% obstructed. It depicts first degree AV block + LSFB + Anterior MI. Low QRS voltage only in the FP leads.
Figure 1.
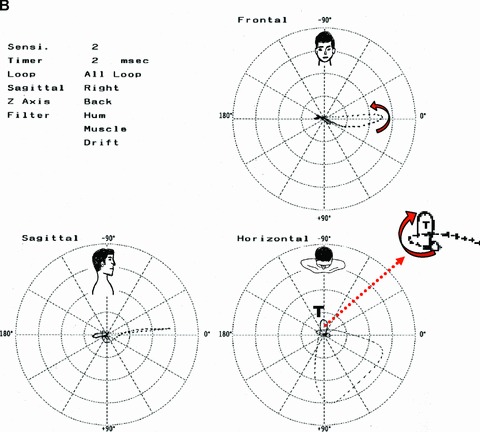
(B) Vectorcardiogram of LSFB. Frontal Plane: QRS loop with counterclockwise (CWW) rotation directed to left. Horizontal Plane: QRS loop with initial forces directed to back, the remained of QRS loop dislocated to the front and leftward (QRS loop predominantly located on left anterior quadrant) and CCW rotation: LSFB. Right Sagittal Plane: QRS loop directed to front: PAF.
Figure 1.
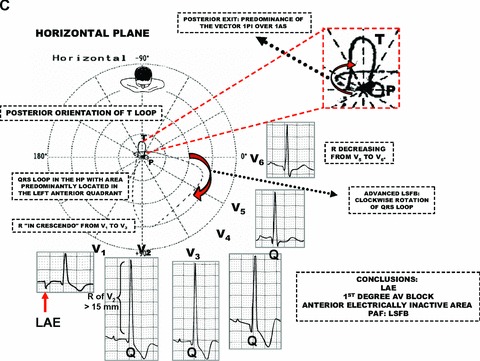
(C) ECG/VCG correlation in the horizontal plane. ECG/VCG diagnosis. Deep negative component of the P wave in lead V1: Left atrial enlargement (LAE). First degree AV block. Initial Q wave in the anterior leads: anterior MI. PAF: V2 R wave voltage >15 mm, R waves “in crescendo” from leads V1 to V3 and decreasing from leads V4 to V6: LSFB. Initial 10 to 20 ms vectors directed posteriorly. CW rotation of the QRS loop. QRS loop dislocated to front and leftward quadrant.
Figure 2.
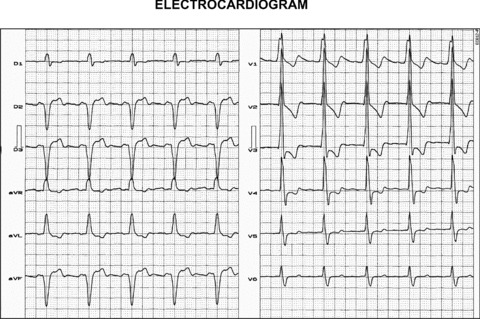
(A) This ECG depicts extreme left QRS axis deviation (‐85°), SIII > SII, final S wave in left leads V5 and V6; all ECG features compatible with LAFB. PAF, R wave voltage “in crescendo” from leads V1 to V3 and decreasing from leads V4 to V6, small initial Q wave in leads V1 toV3, absence of initial Q wave in leads V5 and V6; all ECG features compatible with LSFB. The diagnosis is Left bifascicular block: LAFB + LSFB.
Figure 2.
(B) ECG/VCG correlation in the horizontal plane. ECG/VCG diagnosis: ECG: R wave voltage “in crescendo” from leads V1 to V3 and decreasing from leads V4 to V6, small initial Q wave from leads V1 to V3, absence of initial Q wave in leads V5 and V6; all ECG features compatible with LSFB. VCG: QRS loop with initial QRS 10ms vector directed posteriorly and leftward, CW rotation and localized predominantly on left anterior quadrant: PAF. T loop directed to back.
Figure 2.
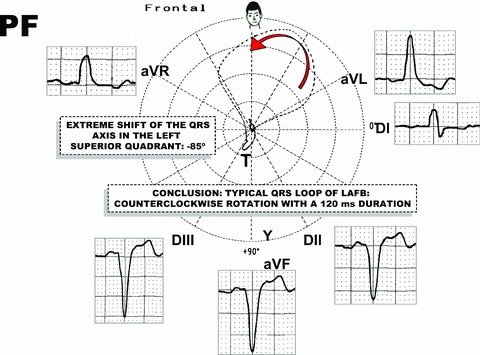
(C) ECG/VCG correlation in the frontal plane. ECG: Extreme QRS left axis deviation (‐85°) SIII > SII; all features compatible with LAFB. VCG: QRS loop with CCW rotation and localized predominantly on left superior quadrant: LAFB.
Figure 3.
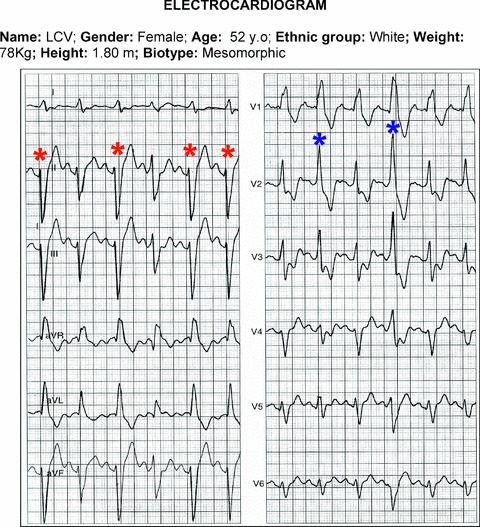
This is a case of a 59‐year‐old female with Chagas’ cardiomyopathy; depressed left ventricular ejection Fraction (35%), LV end diastolic diameter of 74 mm. The 12‐lead ECG shows complete RBBB, LAFB, and LSFB. FP: first, third, fifth and sixth beats (red asterisk) show higher degree of LAFB. HP: second and fourth beats (blue asterisk); LSFB is associated with RBBB. Conclusions: (1) Variable degree LAFB; (2) RBBB; (3) Intermittent LSFB; (4) Intermittent trifascicular block.
Figure 4.
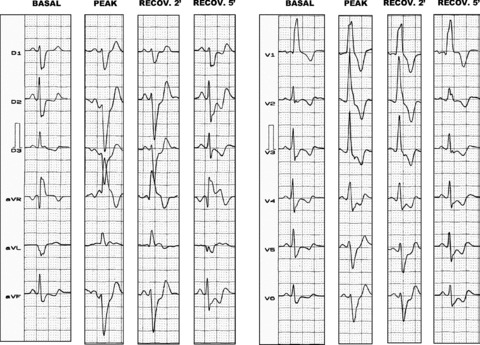
Exercise‐induced LSFB. Transient ischemic bifascicular block. This case (stress test) belongs to a 60‐year‐old man, with prior MI for evaluation of stable chronic angina. Exercise induced transient LAFB, LSFB, and complete RBBB.
DIAGNOSIS OF LSFB
The differential diagnoses of LSFB include all possible etiologies of PAF.
The electrocardiographic diagnosis of PAF can be made when the R wave voltage in any anterior or anteroseptal precordial leads from V1 (+115°) through V4 (+47°) is greater than the normal upper limit for gender and age. Electrovectorcardiographic criteria of PAF should be age and gender‐related. 64
Causes of Prominent Anterior Forces (PAF). Differential Diagnosis of LSFB.
In the presence of PAF in the right and/or middle precordial leads V1 through V3 or V4, the following clinical and/or electrovectorcardiographic differential diagnosis should be accounted:
-
1
Normal variant: PAF are observed in about 1% of normal subjects. 64 Two main types can be distinguished: Normal variant with counterclockwise (CCW) rotation of the heart around the longitudinal axis and athlete's heart, described predominantly in black athletes. 65
-
2
LSFB (see above).
-
3
Misplaced precordial leads. 66
-
4
Strictly posterior, postero‐lateral‐inferior MI (from the “old” nomenclature) 67 or lateral (from the “new“nomenclature). 68
-
5
Right ventricular hypertrophy (RVH). 69
-
6
Diastolic LVH. 70
-
7
Complete RBBB.
-
8
Ventricular preexcitation (Wolff‐Parkinson‐White syndrome), with accessory pathway located in the posterior region (Type A). 71
-
9
Hypertrophic cardiomyopathy: HOCM and NO‐HCM forms. 72
-
10
Duchenne muscular dystrophy. 73
-
11
Endomyocardial fibrosis. 74
-
12
Dextroposition. 75
CONCLUSIONS
There is conclusive evidence of a left human trifascicular His system. The isolated left septal fascicular block has been described by several authors using different terminology inducing confusion in clinicians and researchers. Traditional teaching does not include the concept of a trifascicular left system. The authors provided with the current acceptable terminology and definitions for electrovectorcardiographic diagnosis of left septal fascicular block. Additionally, a call is made to the international societies to generate a position paper or consensus to unify nomenclature and definitions.
The authors have declared no Conflict of Interest.
REFERENCES
- 1. Uhley HN. Some controversy regarding the peripheral distribution of the conduction system. Am J Cardiol 1972;30:919–920. [DOI] [PubMed] [Google Scholar]
- 2. Uhley HN. The quadrifascicular nature of the peripheral conduction system In Dreifus LS, Likoff W. (eds.): Cardiac Arrhythmias. New York , Grune & Stratton. Inc., 1973. [Google Scholar]
- 3. Kulbertus HE. Significance of segmental blocks of the left branch of the bundle of His. Bull Acad R Med Belg 1973;128:481–493. [PubMed] [Google Scholar]
- 4. Kulbertus HE. Concept of left hemiblocks revisited. A histopathological and experimental study. Adv Cardiol 1975;14:126–135. [DOI] [PubMed] [Google Scholar]
- 5. Kulbertus HE, Demoulin J. Pathological basis of concept of left hemiblock In Wellens HJJ, Lie KI, Janse MJ, Stenfert Krpses HE. (eds.): The Conduction System of the Heart, Leiden , Philadelphia , Lea & Febiger, 1976, p. 287–322. [Google Scholar]
- 6. Demolium JC, Kubertus HE. Histopathological examination of concept of left hemiblock. Br Heart J 1972;34:807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Demoulin JC, Kulbertus HE. Left hemiblocks revisited from the histopathological view point. Am Heart J 1973;86:712–723. [DOI] [PubMed] [Google Scholar]
- 8. Frink RJ, James TN. Normal blood supply to the human his bundle and proximal branches. Circulation 1973;47:8–18. [DOI] [PubMed] [Google Scholar]
- 9. Hosseinpour AR, Anderson RH, Ho SY. The anatomy of the septal perforating arteries in normal and congenitally malformed hearts. J Thorac Cardiovasc Surg 2001;121:1046–1052. [DOI] [PubMed] [Google Scholar]
- 10. Riera AR, Ferreira C, Ferreira Filho C, et al Wellens syndrome associated with prominent anterior QRS forces: An expression of left septal fascicular block? J Electrocardiol 2008;41:671–674. [DOI] [PubMed] [Google Scholar]
- 11. Uchida AH, Moffa PJ, Pérez Riera AR, et al Exercise‐induced left septal fascicular block: An expression of severe myocardial ischemia. Indian Pacing and Electrophysiology Journal 2006;6:135–138. [PMC free article] [PubMed] [Google Scholar]
- 12. Moffa PJ, Ferreira BM, Sanches PC, et al Intermittent ântero‐medial divisional block in patients with coronary disease. Arq Bras Cardiol 1997;68:293–296. [PubMed] [Google Scholar]
- 13. Moffa PJ, Pastore CA, Sanches PCR. The left‐middle (septal) fascicular block and coronary heart disease In: Liebman J. (ed.): Electrocardiology’ 96—From the cell to body surface. Cleveland , Ohio , Word Scientific, 1996, pp. 547–550 [Google Scholar]
- 14. Tranchesi J, Moffa PJ. Electrocardiograma Normal e Patológico. In Moffa PJ, Sanches PCR. (eds.). Sao Paulo , Roca, 2001, Chap 19, pp. 413–461. [Google Scholar]
- 15. Tranchesi J, Moffa PJ, Pastore CA, et al Block of the antero‐medial division of the left bundle branch of His in coronary diseases. Vectrocardiographic characterization. Arq Bras Cardiol 1979;32:355–360. [PubMed] [Google Scholar]
- 16. Durrer D, van Dam RT, Freud GE, et al Total excitation of the isolated human heart. Circulation 1970;44:899–912. [DOI] [PubMed] [Google Scholar]
- 17. Alboni P, Malacarne C, Baggioni G, et al Left bifascicular block with normally conducting middle fascicle. J Electrocardiol 1977;10401–10404. [DOI] [PubMed] [Google Scholar]
- 18. Rosenbaum MB, Elizari MV, Lazzari JO. Los Hemibloqueos, Editorial Paidos. S.A.I.C.F. Buenos Aires , 1967, pp. 72. Spanish. [Google Scholar]
- 19. Rosenbaum MB, Elizari M, Lazzari JO. The Hemiblocks: New Concepts of Intraventricular Conduction Based on Human Anatomical, Physiological and Clinical Studies. Oldsmar , FL , Tampa Tracings; 1971. [Google Scholar]
- 20. Medrano GA, Brenes C, De Michelis A, et al Simultaneous block of the anterior and posterior subdivisions of the left branch of the bundle of His (biphasic block), and its association with the right branch block (triphasic block). Experimental and clinical electrocardiographic study. Arch Inst Cardiol Mex 1970;40:752–770. [PubMed] [Google Scholar]
- 21. Gambeta M, Childers RW. Rate‐dependent right precordial Q waves: “Septal focal block.” Am J Cardiol 1973;32:196–201. [DOI] [PubMed] [Google Scholar]
- 22. Athanassopoulos CB. Transient focal septal block. Chest 1979;75:728–730. [DOI] [PubMed] [Google Scholar]
- 23. Madias JE, Ashtiani R, Agarwal H, et al Diagnosis of ventricular aneurysm and other severe segmental LV dysfunction consequent to a myocardial infarction in the presence of right bundle branch block: ECG correlates of a positive diagnosis made via echocardiography and/or contrast ventriculography. Ann Noninvasive Electrocardiol 2005;10:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cohen SI, Lau SH, Haft JI, et al Experimental production of aberrant ventricular conduction in man. Circulation 1967;36:673–685. [DOI] [PubMed] [Google Scholar]
- 25. Cohen SI, Lau SH, Steiner E, et al Variations of aberrant ventricular conduction in man: Evidence of isolated and combined block within the specialized conduction system. Circulation 1968;38:899–916. [DOI] [PubMed] [Google Scholar]
- 26. Iwamura N, Shimizu T, Kodama I, et al In vitro study on the cause of intraventricular aberrant conduction: Comparison of the functional refractory period between the canine right and left bundle branch systems. Jpn Circ J 1976;40:461. [Google Scholar]
- 27. Lazzara R, El‐Sherif N, Befeler B, et al Regional refractoriness within the ventricular conduction system. Circ Res 1976;39:254–262. [DOI] [PubMed] [Google Scholar]
- 28. Kulbertus HE, de‐Leval‐Rutten F, Casters P. Vectorcardiographic study of aberrant conduction. Anterior displacement of QRS: Another form of intraventricular block. Br Heart J 1976;38:549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hoffman I, Mehta J, Hilsenrath J, et al Anterior conduction delay: A possible cause for proeminent anterior QRS forces. J Electrocardiol 1976;9:15–21. [DOI] [PubMed] [Google Scholar]
- 30. Dhala A, Gonzalez Zuelgaray J, Deshapande S, et al Unmasking the trifascicular left intraventricular conduction system by ablation of the right bundle block. Am J Cardiol 1996;77:706–712. [DOI] [PubMed] [Google Scholar]
- 31. Reiffel JA, Bigger T, Jr . Pure anterior conduction delay: A variant “fascicular” defect. J Electrocardiol 1978;11:315–319. [DOI] [PubMed] [Google Scholar]
- 32. Pérez‐Riera AR. Left Septal Fascicular Block. In: Baranchuk A (ed.): Atlas of Advanced ECG Interpretation. REMEDICA, London (UK), 2011, chapter 4, case 23 (in press). [Google Scholar]
- 33. De Pádua F. Bloqueios fasciculares—Os hemibloqueios em questão. Rev Port Clin Terapeutica 1977;3:199. [Google Scholar]
- 34. De Pádua F. Methodology and basic problems of ECG and VCG research. Hemiblocks. Adv Cardiol 1977;19:105–114. [DOI] [PubMed] [Google Scholar]
- 35. Pastore CA, et al Guidelines for Interpreting Rest Electrocardiogram. Arq Bras Cardiol 2003;80:1–17. [Google Scholar]
- 36. Dabrowska B, Ruka M, Walczak E. The electrocardiographic diagnosis of left septal fascicular block. Eur J Cardiol 1978;6:347–357. [PubMed] [Google Scholar]
- 37. Nakaya Y, Hiasa Y, Murayama Y, et al Prominent anterior QRS force as a manifestation of left septal fascicular block. J Electrocardiol 1978;11:39–46. [DOI] [PubMed] [Google Scholar]
- 38. Mori H, Kobayashi S, Mohri S. Electrocardiographic criteria for the diagnosis of the left septal fascicular block and its frequency among primarily elderly hospitalized patients. Nippon Ronen Igakkai Zasshi 1992;29:293–297. [DOI] [PubMed] [Google Scholar]
- 39. Sakai T. Left anterior fascicular block, left posterior fascicular block, left septal fascicular block. Ryoikibetsu Shokogun Shirizu 1996;12:282–284. [PubMed] [Google Scholar]
- 40. Sanches PCR, Moffa PJ, Sosa E, et al Electrical endocardial mapping of five patients with typical ECG of left‐middle (septal) fascicular block In: Pastore CA. (ed.): Proceeeding of the XXVIII International Congress on Electrocardiology Guarujá , SP , Brazil . Heart Institute of the University of São Paulo School of Medicine São Paulo Brazil 2001, Atheneu, pp. 89–95. [Google Scholar]
- 41. MacAlpin RN. Left Septal Fascicular Block: Myth Or Reality? Indian Pacing Electrophysiol J 2003;3:157–177. [PMC free article] [PubMed] [Google Scholar]
- 42. MacAlpin RN. In search of left septal fascicular block. Am Heart J. 2002;144:948–956. [DOI] [PubMed] [Google Scholar]
- 43. Dabrowska B. Role of the septal fascicle of the left bundle branch in the system of intraventricular conduction. Kardiol Pol 1979;22:497–501. [PubMed] [Google Scholar]
- 44. De Micheli A. Diagnosis of fascicular or left partial block. G Ital Cardiol 1976;6:1148–1149. [PubMed] [Google Scholar]
- 45. Alboni P. Left parietal septal block. A physiopathological hypothesis or new diagnostic element? G Ital Cardiol 1980;10:365–371. [PubMed] [Google Scholar]
- 46. Magnacca M, Valesano G, Rizzo G, et al Diagnostic value of electrocardiogram in septal fascicular conduction disorders of the left branch in diabetics Minerva. Cardioangiolica 1988;36:361–363. [PubMed] [Google Scholar]
- 47. Iwamura N, Kodama I, Shimizu T, et al Functional properties of the left septal Purkinje network in premature activation of the ventricular conduction system. Am Heart J 1978;95:60–69. [DOI] [PubMed] [Google Scholar]
- 48. Nakaya Y, Inoue H, Hiasa Y, et al Functional importance of the left septal Purkinje network in the left ventricular conduction system. Jpn Heart J 1981;22:363–376. [DOI] [PubMed] [Google Scholar]
- 49. Moffa PJ, Del Nero E, Tobias NM, et al The left anterior septal block in Chagas’ disease. Jpn Heart J 1982;23:163–165. [Google Scholar]
- 50. Alboni P, Malacarne C, De Lorenzi E, et al Right precordial q waves due to anterior fascicular block. Clinical and vectorcardiographic study. J Electrocardiol 1979; 12:41–48. [DOI] [PubMed] [Google Scholar]
- 51. Nakaya Y, Hiraga T. Reassessment of the subdivision block of the Left Bundle Branch. Jpn Circ J 1981;45:503–516. [DOI] [PubMed] [Google Scholar]
- 52. Hassapoyannes CA, Nelson WP. Myocardial ischemia‐induced transient anterior conduction delay. Am Heart J 1991;67:659–660. [DOI] [PubMed] [Google Scholar]
- 53. De Pádua F, Reis DD, Lopes VM, et al Left median hemiblock – a chimera? In: Rijlant P; Kornreich F. (eds.). 3rd Int. Congr. Electrocardiology. 17th Int. Symp. Vectorcardiography. Brussels , 1976. [Google Scholar]
- 54. De Padua F, dos Reis DD, Lopes VM, et al Left median hemiblock‐ a chimera? Adv Cardiol 1978;21:242–248. [DOI] [PubMed] [Google Scholar]
- 55. Inoue H, Nakaya Y, Niki T, et al Vectorcardiographic and epicardial activation studies on experimentally—induced subdivision block of the left bundle branch. Jpn Circ J 1983;47:1179–1189. [DOI] [PubMed] [Google Scholar]
- 56. Georgiev N. Block of the anterior median branch of the bundle of His. Vutr Boles 1986;25:112–115. [PubMed] [Google Scholar]
- 57. Iwamura N. Experimental study on the cause of ventricular aberrant conduction. Jpn Circ J 1978;42:489–499. [PubMed] [Google Scholar]
- 58. Maron BJ, Wolfson JK, Ciro E, et al Relation of electrocardiographic abnormalities and patterns of left ventricular hypertrophy identified by 2‐dimensional echocardiography in patients with hypertrophic cardiomyopathy. Am J Cardiol 1983;51:189–194. [DOI] [PubMed] [Google Scholar]
- 59. Yamaguchi H, Nishiyama S, Nakanishi S, et al Electrocardiographic, echocardiographic and ventriculographic characterization of hypertrophic non‐obstructive cardiomyopathy. Eur Heart J 1983;4(Suppl F):105–119. [DOI] [PubMed] [Google Scholar]
- 60. Comella A, Magnacca M, Gistri R, et al Right ventricular involvement in hypertrophic cardiomyopathy. A case report and brief review of the literature. Ital Heart J 2004;5:154–159. [PubMed] [Google Scholar]
- 61. Riera AR, Kaiser E, Levine P, et al Kearns‐Sayre syndrome: Electro‐vectorcardiographic evolution for left septal fascicular block of the His bundle. J Electrocardiol 2008;41:675–678. [DOI] [PubMed] [Google Scholar]
- 62. Abrahao HD, Schwartz HJ, Franca FF. Fascicular block. Arq Bras Cardiol. 1979;33:447–451. [PubMed] [Google Scholar]
- 63. Madias JE. The “giant R waves” ECG pattern of hyperacute phase of myocardial infarction. J Electrocardiol 1993;26:77–80. [DOI] [PubMed] [Google Scholar]
- 64. Mattu A, Brady WJ, Perron AD, et al Prominent R wave in lead V1: Electrocardiographic differential diagnosis. Am J Emerg Med 2001;19:504–513. [DOI] [PubMed] [Google Scholar]
- 65. Basavarajaiah S, Boraita A, Whyte G, et al Ethnic differences in left ventricular remodeling in highly‐trained athletes relevance to differentiating physiologic left ventricular hypertrophy from hypertrophic cardiomyopathy. J Am Coll Cardiol 2008;51:2256–2262. [DOI] [PubMed] [Google Scholar]
- 66. MacKenzie R. Tall R wave in lead V1. J Insur Med 2004;36:255–259. [PubMed] [Google Scholar]
- 67. Zema MJ. Electrocardiographic tall R waves in the right precordial leads. Comparison of recently proposed ECG and VCG criteria for distinguishing posterolateral myocardial infarction from prominent anterior forces in normal subjects. J Electrocardiol 1990;23:147–156. [DOI] [PubMed] [Google Scholar]
- 68. Bayés de Luna A, Zareba W. New terminology of the cardiac walls and new classification of Q‐wave M infarction based on cardiac magnetic resonance correlations. Ann Noninvasive Electrocardiol 2007;12:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Suzuki K, Toyama S. Vectorcardiographic criteria of high posterior infarction: Differentiation from normal subjects, right ventricular hypertrophy and primary myocardial disease. J Electrocardiol 1978;11:159–163. [DOI] [PubMed] [Google Scholar]
- 70. Budhwani N, Patel S, Dwyer EM, Jr . Electrocardiographic diagnosis of left ventricular hypertrophy: The effect of left ventricular wall thickness, size, and mass on the specific criteria for left ventricular hypertrophy. Am Heart J 2005;149:709–714. [DOI] [PubMed] [Google Scholar]
- 71. Khan IA, Shaw IS. Pseudo ventricular hypertrophy and pseudo myocardial infarction in Wolff‐Parkinson‐White syndrome. Am J Emerg Med 2000;18:807–809. [DOI] [PubMed] [Google Scholar]
- 72. Kukla P, Petkow‐Dimitrow P, Jastrzebski M, et al Malignant form of familial hypertrophic cardiomyopathy complicated with ventricular fibrillation in siblings. Electrocardiogram in hypertrophic cardiomyopathy—A review. Kardiol Pol 2009;67:774–780. [PubMed] [Google Scholar]
- 73. Thrush PT, Allen HD, Viollet L, et al Re‐examination of the electrocardiogram in boys with Duchenne muscular dystrophy and correlation with its dilated cardiomyopathy. Am J Cardiol 2009;103:262–265. [DOI] [PubMed] [Google Scholar]
- 74. Tobias NM, Moffa PJ, Pastore CA, et al The electrocardiogram in endomyocardial fibrosis. Arq Bras Cardiol 1992;59:249–253. [PubMed] [Google Scholar]
- 75. Cíhalík C. Evaluation of the ECG recording in abnormal positions of the heart in the thorax Vnitr Lek. 2002;48(Suppl 1):90–94. [PubMed] [Google Scholar]


