Abstract
Holter technology has endured for more than 40 years, and proven to be a valuable adjunctive noninvasive diagnostic technology to record the ambulatory or long‐term electrocardiogram in the study of living creatures. During this span of time, many scientists, physicians, and innovators contributed to the development and evolution of Holter technology. This essay seeks to document a view of the history and evolution of the technology during that time, and concomitantly give recognition to the scientists, physicians, and engineers who contributed so greatly.
Keywords: Holter technology, Jeffrey Holter, Bruce Del Mar
Like many achievements in life, the seminal beginnings of an advance in science or technology are often lost with the passage of time. Nevertheless, it is important for scientists, engineers, physicians, and clinicians to reflect on the development of Holter technology and multiple individuals who contributed to the technology, per se, as we know it. This is not an easy task, and by definition will be limited to the resources available to recall these events. The author recognizes that many “unknown scientists” undoubtedly lived and contributed observations to the development of Holter electrocardiography, both the medical science and the technology … their memory and contribution lost in the fading candle of time. However, we should attempt to see and remember what Longfellow asserted “…great men leave behind them footprints in the sands of time.” In the author's view, more often than not in the field of science, those footprints were unquestionably formed by strong boots of supportive coworkers surrounding them … this was the case for Holter technology.
THE SCIENTISTS AND PHYSICIANS
Whereas the serendipitous discovery of electrical activity from the cardiac muscle occurred in 1856 by Kolliker and Muller 1 working on the frog gastrocnemius muscle, it was Augustus Waller, using a Lippman capillary electrometer, who first reported the electrical deflections of a human heart. 2 The fact that Willem Einthoven, unequivocally regarded as the “Father of Electrocardiography,” was influenced by his good friend, Augustus Waller, is not to be forgotten, as was the work and contributions of his laboratory assistant Van der Woerd and countless trainees who sought this new science (e.g., Sir Thomas Lewis, George E Fahr, and others). This boot of support around the giant foot of Einthoven spawned the evolution of the electrocardiographic technology. Einthoven's introduction of the silver‐coated quartz single strand galvanometer announced as um nouveau galvanometer in 1901 3 was followed by a host of subsequent scientific and technological development.
The similarities between Willem Einthoven and Norman Jefferis Holter are more apparent than their differences. Although Einthoven received his medical degree in 1885, his interest in recording electrical potentials from the heart emanated from his teacher Donders of the University of Utrecht. 4 This interest led to his accepting a position as a physiologist at the University of Leiden in 1886, where his work progressed from the frog gastrocnemius muscle to the string galvanometer. 4 Holter similarly was drawn to work with the frog muscle as an assistant to Dr. Lawrence Detrick at the University of California, Los Angeles. 5 Holter did not receive a medical degree but received a masters degree in physics (University of California, Los Angeles) and chemistry (University of Southern California) and in 1939 began working with Joseph A. Gengerelli, Ph.D., on the idea of stimulating a frog nerve and muscle without touching it directly by mechanical or electrical means. 5 This seminal interest of Jeff Holter to study the electrical activity of humans “without touching” them in their daily activities is what spawned his life pursuit and contributions to Holter technology. This interest arose from the appreciation that electrical fields surrounded nerve conduction. 6 With the evolution of technology over a 20‐year period and the assistance of coworkers …Gengerelli, Holter, and Glasscock established the field of biomagnetics. 6 , 7 , 8 Holter was then delayed by World War II, serving as a physicist in the U.S. Navy Bureau of Ships, but returned to his hometown of Helena, Montana in 1947, and continued his work with Gengerelli. Although their early efforts were directed at the brain waves of rats, it was a visit from the famous cardiologist, Dr. Paul Dudley White, which convinced Holter to focus on recording electrical activity from the heart. As Holter expressed in a conference attended by the author “the voltage was ten times greater (in the heart) which made the electronics easier” and through White's influence, Holter realized that heart disease was the leading public health problem of his day. 9 Subsequently, Holter and Gengerelli recorded the first broadcast of an electrocardiogram with an 85‐pound backpack transmitter during exercise 7 (Fig. 1). This vacumn‐tubed radioelectrocardiograph evolved into smaller components with the invention of the transistor and took the form of a small portable transmitter and antenna connected to body surface electrodes and a portable self‐powered receiver‐recorder that could be carried to record long‐term electrocardiographic records on magnetic tape. 10 Subsequent innovation led to better transistors, and Holter and Glasscock subsequently developed the miniaturized Holter tape recorder with its playback Audio‐Visual Superimposed ECG Presentation methodology to interpret the tape. 11 During this period of early development, Holter interacted with Dr. Eliot Corday of Los Angeles as to the practicality of his observations. 12 Corday in the Cedars of Lebanon Hospital (currently the Cedars‐Sinai Hospital of Los Angeles) had spent several years studying the effects of elusive pathophysiological events, which included transient insufficiency states including myocardial ischemia, and was quick to embrace the technology to record his observations. 12 , 13 Corday collaborated with Holter's team of investigators and was an early physician promoter of the technology to both industry and other physicians. Whereas the first report of a clinical patient's Holter recording was by radioelectrocardiography in 1954, 14 , 15 its introduction to the medical community at large was to occur via the innovation of industry when Holter gave his invention to Bruce Del Mar and the Avionics Research Products Corporation for clinical development.
Figure 1.

(A) Radiotransmitter in the form of an 85‐pound backpack whose signal was carried a distance of one block.
Early physician users of the 1960s included S. Bellet, Eliot Corday, John Gilson, H.K. Hellerstein, Lawrence Hinkle, E. Goldberger, Bernard Tabatznik, Herbert Semler, D.G. Julian, J.M. Martt, Charles Freidberg, Selvyn Bleifer, Shlomo Stern, and many others too numerous to mention. These latter physicians were the boot of support that Jeff Holter worked with to establish the importance of this clinical diagnostic tool. Neither Einthoven nor Holter personally financially profited from the industrial growth and explosion of their technologies and its ensuing wealth, although Einthoven was duly recognized by the scientific community in receiving the Nobel Prize in 1924. It is memorable to have known personally the modest lifestyle that Jeff Holter lived, and the continuing struggle that he endured to pursue his scientific endeavors in Helena, Montana. It is unquestionable that Jefferis Holter is the physician's “Father of Ambulatory or Long‐term Electrocardiography” whether it occurred through radioelectrocardiography, telemetry, or recording and that “footprint in the sand of time” bears remembering.
THE TECHNOLOGY AND INNOVATORS
Unlike most medical discoveries, which receive continuing genesis from further scientific expansion by other scientists or physicians, Holter technology expanded and grew upon the continuous innovation of manufacturers in industry. As shown in Figure 2, technology evolved its hardware from the vacuum tube era, through transistor and microprocessors, to microchip and printed circuit boards; its recording medium from magnetic tape to solid‐state memory; its signal processing from analog to digital; and its interpretive aspects from a local single station, through a local network, to a global capability on the Internet. Bruce Del Mar's singular commitment to Jeff Holter's idea led to the first clinically applicable system of Holter technology which could be marketed by Avionics Research Products to a wide arena of physicians and scientists throughout the globe. This development formulated an entirely new industry. Clearly, Bruce Del Mar was a pivotal part of the boot of support that Jeff Holter received on his scientific path. In a similar analogy, Bruce Del Mar must be regarded as the primary innovator of the technology of Holter recording. This was achieved by Del Mar's continuing efforts with W. Glasscock and the collaborative efforts of Del Mar Avionics engineers W. Thornton, R. Cherry, and C. Sanctuary. The Del Mar Avionics Electrocardioscanner (Model 450) (Del Mar Avionics, Los Angeles, CA, USA) and charter (Model 550) with its accompanying electrocardiocorder (Model 350) and accompanying paraphenalia (1 mV calibrator, rechargeable batteries, magnetic tape eraser, and battery charger) introduced in late 1963 and capable of recording initially 6–8 hours and then 10–12 hours of data became widely dispersed on all continents within the decade of the 1960s, and its clinical value in the diagnosis and assessment of patient symptoms and cardiac arrhythmias was quickly established (Fig. 3). 16 The competitive marketplace attracted other manufacturers to the field beginning in the very late 1960s and throughout the 1970s, reaching its zenith in the 1980s when as many as 26 Holter companies could be counted at the national Scientific Sessions of the American Heart Association and American College of Cardiology.
Figure 2.
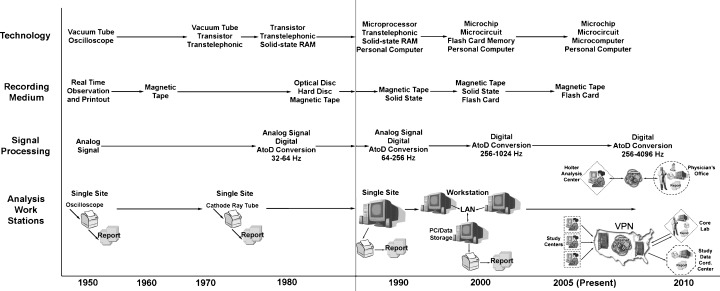
Time trend developments of Holter technology.
Figure 3.
Bruce Del Mar displaying early Holter recording instrumentation.
Whereas many individual companies contributed to the innovative developments of the technology, this author's attempt to recall all of them with appropriate recognition is appreciated as somewhat futile since many contributions escaped being duly recorded over the past 40 plus years. As one might expect over four decades, many of the early companies have faded with time or merged into new organizations. Nevertheless, their competitive contribution spurred the development of the industry. Such is the case for companies including AdvanceMed, American Optical, Brentwood, Cardiodynamics, Diagnostic Medical Instruments, Hewlett‐Packard, Hittman Medical Systems, Instruments for Cardiac Research, Marquette Electronics, Qmed, Quinton, and Zymed companies. Some have stayed the course, e.g., Applied Cardiac Systems, Biomedical Systems, Del Mar Reynolds (formerly Del Mar Avionics and Reynolds Medical), ELA Medical, Fukuda Denshi Instruments, Instromedix, Mortara Instruments, Rozinn Electronics, Siemens‐Burdick, and Schiller AG. Other companies have emerged from acquisitions as spinoffs, e.g., GE instruments, Phillips Medical Systems, Spacelabs instruments, and Quinton Cardiology. All of these companies contributed to the ongoing innovation experienced in Holter technology. The author's attempt to highlight specific aspects of the technology must not be viewed too critically, but is his best recollection of events.
Following Del Mar's introduction of the initial recording system, the Oxford company (United Kingdom) introduced a Holter tape recorder which utilized a frequency modulated analog system in contrast to the original amplitude modulated signal and used a cassette tape instead of a reel‐to‐reel tape. 16 Whereas there were some distinct advantages during the early development of recorders in frequency modulation recording having a more accurate low‐frequency response, this limitation was subsequently overcome with better reliability to amplitude modulated recordings with improved capacitors and motor speeds from transistors, and improved magnetic tapes. American Optical introduced the concept of a continuous recording of 1 hour data with its “trendscription” drum‐like printout which was revolutionized by the “full‐disclosure” technique introduced by AdvanceMed (optical writer technique) and Del Mar Avionics (mechanical writer technique). During this time, Del Mar Avionics introduced the two‐channel Holter recorder that was extended by Oxford to a four‐channel recorder (three channels of electrocardiographic data with a time track). Instruments from Cardiac Research introduced the 48‐hour cassette recorder. Subsequently, multichannel Holter recording was taken to all 12 channels by Mortara Instruments. During this constant competetive evolution taking place in the marketplace, 16 , 17 the conversion of the analog signal to digital format was a major turning point that opened new medical parameter horizons in the 1980s and began to change the entire business of Holter technology. One of the earliest applications of the digital technology was Del Mar Avionics pacemaker Holter recorder which provided one channel of only the amplified pacemaker stimulus with one or two separate channels of electrocardiographic data to assist in the electrocardiographic interpretation of pacemaker rhythm. 17 This latter innovation suffered the criticism that the atrial stimulus could not be easily differentiated from the ventricular stimulus in some instances of dual‐chamber pacing. This was improved by ELA (France) whose circuitry was designed to detect the differences in pacing stimulus width of its own manufactured pacemakers, allowing accurate differentiation between atrial and ventricular stimuli. 17 This application of Holter recording technology to pacemakers was, however, stymied by the reintroduction of biotelemetry, as increasingly sophisticated pacemakers and subsequently, implantable cardioverter devices emerged in the marketplace during the 1990s which contained internal biotelemetry of endocardial electrograms with added storage capability. The telemetry of stored endocardial electrograms contained within devices is currently utilized to assess the proper function of such devices. 18 , 19 Although Diagnostic Medical Instruments and its Altair‐DISC recorder was an early user of a magnetic hard disk drive to replace tape‐based systems for digital data storage, further innovation led to several varieties of solid‐state digital data storage devices. These storage devices have evolved from 11‐MB storage devices to flash card memory storage with a capability of 512‐MB storage today and 1 GB on the horizon. Sampling rates of the analog signal to digital conversion progressed from 32 and 64 Hz to 1000 Hz, thereby giving Holter genesis to new parameters of heart rate variability and the signal‐averaged ECG. Today's capability of digital sampling on an investigational basis has increased the sampling rate to 4096 Hz to seek measurement data in the electronic functionality of pacemakers and implantable cardioverter devices.
Holter Electrocardiographic Parameters
Accompanying these developments of technology, per se, was the evolution of new electrocardiographic parameters. 17 Whereas in the 1960s–1970s, technology focused on ectopic beat detection, early interpretive algorithms and visual interpretive methods; the 1980s aided by the introduction and development of computer technology saw a focus on refinement of ectopic beat detection algorithms, ST segment detection, and quantitative databases. In the 1990s, the development of microchip technology, digital solid‐state storage, and the personal computer technology of printed circuit boards clearly changed all Holter technology from being a hardware‐based business model into a computer software driven industry. With this enhanced capability, digital signal processing allowed the high‐resolution signal‐averaged ECG to be recorded, 20 both time and frequency domain heart rate variability to be extracted, 21 T wave alternans to be detected, 22 identification of heart rate turbulence, 23 and improved detection algorithms of QT measurements/variability 24 and atrial fibrillation 25 were developed. Computer‐generated vectorcardiographic loops, Poncare' plots, histograms, bar graphs, and quantitative/qualitative tables became the normal standard Holter recording expected data in a 24‐hour Holter report. 18 , 26
Other Holter Applications
A variety of diverse applications of Holter technology emerged over its 40‐year history, some of which have not withstood the test of time, on the other hand many improved adaptations have remained. Ambulatory blood pressure pioneered by Del Mar Avionics in the early 1980s did not enjoy widespread clinical application until 20 years later. It is now commonly utilized in hypertension randomized controlled trials. 27 Ambulatory electroencephalography pioneered by the Oxford four‐channel recorder with its innovative page‐mode replay and visual display system never became a widely utilized technology by neurologists, although the page‐mode method of visual interpretation was widely adopted by most Holter manufacturers. 28
Whereas there was early interest in applying Holter technology to sleep disordered breathing (SDB), obstructive sleep apnea, or the sudden infant death syndrome, only in recent years with the National Institute of Health emphasis on the Sleep Heart Study 29 has portable in‐home devices using Holter technology been applied to recording long‐term observations of the electrocardiogram, respiratory patterns, and O2 saturation levels. 30 One recent appearance in the marketplace is a Holter recorder containing a probability algorithm to identify the likely presence of sleep disordered breathing that incorporates changes in respiratory impedance, heart rate variability, and proprietary algorithms to indicate a “probability” score of the presence of a sleep disorder. The validation of such technologies have not been clearly established but currently are the object of ongoing investigation.
Employment of the Frank lead system on three‐channel Holter recorders, particularly utilized in European and Scandinavian countries, has permitted the enduring utility of the vectorcardiogram, and facilitated the derived 12 lead electrocardiogram from 3 channel Holter recordings. Systolic time intervals, muscle activity, body posture, and vibration recording are parameters reported by isolated investigators using Holter technology that have all seemingly faded with the passage of time. On the other hand, the use of Holter technology to record gastrointestinal motility and pH has persisted, albeit not widely utilized. Measurement of penile erection has been obviated by the pharmaceutical development of sildenafil and similar compounds but was a curious application of early Holter technology.
PRESENT DAY AND FUTURE HOLTER TECHNOLOGY
It is always a poignant experience to sometimes hear colleagues opine that the use of the term Holter is outdated. This point of view arose in the 1990s with the introduction of increasingly sophisticated pacemaker and implantable cardioverter devices. The information gained from such cardiac devices by biotelemetry of internal cardiac electrograms from stored or queried data is not widely appreciated as being one of the earliest modalities established by Jeff Holter and his coworkers. Similarly, during the end of the 1990s, the introduction of long‐term loop recorders, 31 both noninvasive and implantable devices (Reveal by Medtronic), 32 was viewed by some clinicians as “obviating the need for Holter.” This perspective reflects a limited view of the adjunctive nature of all Holter technology and clearly lacks the insight of the single mission of Jeff Holter to study humans “without touching” them. These developments within the extending pervasive world of computer technology, and the ubiquitous presence of the Internet, currently bring a focus in the 21st century on new parameters of measurement and new methods of analysis.
Parameters. Among the most notable new parameters being examined at this time is the value of heart rate variability, 21 T‐wave alternans, 33 , 34 heart rate turbulence, 23 , 35 and variations in the QRS complex (i.e., QRS, QT, and JT dynamicity) 24 and brady‐ and tachycardiograms 36 throughout a 24‐hour day. These new parameters are fueled, in part, by the current interest in cost effectively utilizing cardiac device therapies and the expanding knowledge of the importance of autonomic measurements to cardiovascular outcomes. On the other hand, evolving knowledge and a wider appreciation that the autonomic nervous system and its neurohormonal axis are reflected within the 24‐hour electrocardiographic data of a Holter recording are now clearly recognized across a wide spectrum of pathological states.
With the expanding indication of device therapies for primary prevention of sudden cardiac death, interest in identifying those at greatest risk to warrant such expensive therapy would seem imperative. Whereas only approximately 10% of sudden cardiac death victims have a high‐risk profile, the number needed to treat (NNT) (to save one life) using the risk stratification tools currently available varies according to the length of follow‐up of the studies that exist. Whereas the NNT may be as low as 3 or 4 for a mean duration of 2.5–5 years within the highly selective risk stratifying criteria of the Multicenter Automatic Defibrillator Implantation Trial I (MADIT‐I) 37 and Multicenter Unsustained Tachycardia Trial (MUSTT) 38 trials, it can be as high as 11–14 for a mean duration of 3–5 years within the stratifying criteria of the MADIT‐II 39 and SCD‐HeFT 40 trials. Thus the search for better risk stratifiers or a combination thereof has come into prominent view and is a concern to clinicians. One interest centered in this regard on T‐wave alternans. The value of T‐wave alternans which classically is observed during exercise, is now being sought through beat‐to‐beat Holter recordings. 34 Whereas risk stratifiers have classically sought to have a high positive predictive accuracy, the value of a high negative predictive value to avoid costly therapeutic interventions is now being realized. 41 T‐wave alternans is one such variable which may be quite valuable in decreasing the NNT with regards to an Implantable Cardioverter‐Defibrillator (ICD). Additional parameters being focused upon in this goal include variations in the QRS complex (dynamicity), which are being added to established markers of the signal‐averaged ECG or heart rate variability in identifying the patient most likely to benefit from costly therapy for which Medicare pays approximately $30,000 per case.
Recently, the importance of sleep disordered breathing, widely characterized as sleep apnea, in creating adverse cardiovascular outcomes has clearly become appreciated. The increasing prevalence of sleep disordered breathing in an aging population and its contributions to the development of hypertension, stroke, myocardial infarction, heart failure, and atrial fibrillation are increasingly recognized. 42 With this appreciation, the need for a more cost‐effective screening tool alternative to the relatively costly classical overnight polysomnography examination has emerged. Whereas for several years the value of electrocardiographic heart rate variability in diagnosing sleep disordered breathing has been realized and is the subject of ongoing investigations, there has now emerged active interest in the brady and tachy changes in heart rate and respiration which occur during the apnea or hyponea episodes. 36 These arousal periods and their characteristic disturbances in heart rate and respiration are now the object of adjunctive Holter screening tests to detect the candidate at risk of SDB during the routine Holter examination. These developments are not surprising in view of the unappreciated nature of SDB in the cardiovascular patient and the need to decrease cardiovascular outcomes in the aging population of the 21st century. 29 , 42
Technology. The greatest impact upon Holter technology in the past decade has been the integration of the Internet into the transmission and analysis of Holter recording data. This latter phenomena, which started without regulation, has now encountered privacy regulations in the health care industry, and subsequently modified its processes to accommodate this changing environment. With the advent of DSL and then broadband technology, the 24‐hour Holter recording which consists of approximately40–80 or 100 MB of data (a three channel recording with sampling rate of 128–256 Hz) can be transmitted within a matter of minutes to distant locations. On the other hand, some analysis applications have avoided this by innovating Holter analysis without the transmission of data (Fig. 4). The latter applications permit a distant operator to enter a satellite station electronically, maintain all raw ECG signal data at the acquisition site, and analyze, edit, and print the final Holter report at the satellite station. Issues of patient privacy and health care regulations are then more easily accounted for by the responsible physician at the satellite station.
Figure 4.
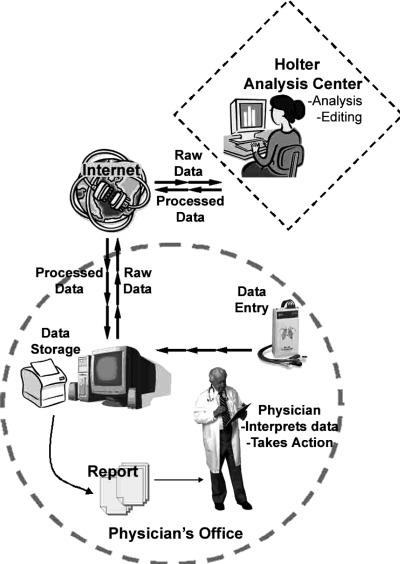
Pictorial of operator interaction of a satellite Holter station from a distant location to analyze, edit, and print a 24‐hour Holter report.
A modification of this analysis service with attention to privacy and blinding for research purposes is through the creation of a multicenter clinical trial virtual private network (VPN) and a core base station (Fig. 5). Coded Holter data from participating satellite stations are transmitted via the Internet to the data servers contained within the VPN. VPNs are currently maintained with assurance of privacy, backup, and regulatory safeguards at both commercial (e.g., Southwestern Bell) and educational (e.g., Duke University) institutions. The Holter raw data analysis, editing, and interpretation are provided by a core base station through the Internet which accesses the VPN. Holter recording results are maintained at the core base station for study purposes and definitive study analysis. If Holter report data are needed at the satellite study center, it can be obtained via the Internet at the VPN. The VPN archived digital raw database then becomes a repository of electrocardiographic data that can be utilized by a myriad of investigators with existing technologies of today, as well as those that might develop in the future. Such developments occurred from previous tape databases of other clinical trials, e.g., European Myocardial Infarction Amiodarone Trial (EMIAT), Autonomic Tone and Reflexes After Myocardial Infarction (ATRAMI) trial, etc., at a far greater cost that required substantial effort and resources to reanalyze the data. 35 Therefore, this archival structure could be expected to cost effectively provide a digital database that is both secure and widely accessible via the Internet.
Figure 5.
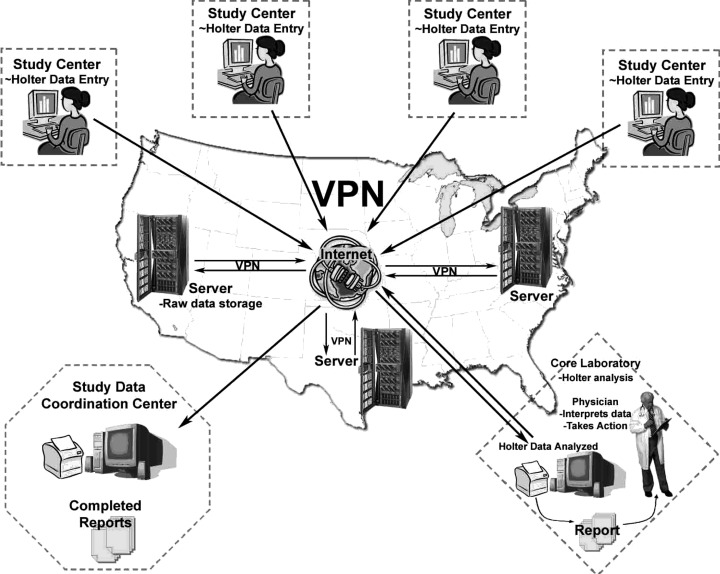
A multicenter Holter VPN network.
THE CIRCLE AND LEGACY OF HOLTER TECHNOLOGY
The often quoted saying “what goes around, comes around” is truly applicable to Holter technology that has seen a circuitous application of the various technologies developed during its lifespan (Fig. 6). Every form of electrocardiographic information of humans who go about their daily activities and is protracted over a long duration of time “without touching” (i.e., without cables) is an evolution of Jeff Holter's earlier paradigm and contributions. Jeffres Norman Holter should be widely regarded and accepted as the “Father of Ambulatory and Long‐Term Electrocardiography,” less we ignore and fail to recognize the clear footstep of a giant that lived within our own time. Whereas Holter received a major boot of support from the physician side which included many, such as Elliott Corday, Lawrence Hinkle, and others. Unquestionably, the other boot of support on the technology side was Bruce Del Mar. Del Mar risked both investment and commitment to formulate an industry that has ultimately extended Holter technology to physicians everywhere on the globe. The Holter technology industry was formulated on Del Mar's innovative efforts and energy, and forever is indebted to that early genesis. On a personal basis Bruce Del Mar was one of the early supporters that urged and financially sponsored the fledgling International Society of Holter Monitoring (now the International Society of Holter and Noninvasive Electrocardiology) with substantial resources pledged from Del Mar Avionics over a number of years, and created the honorary Young Investigator and Senior Investigator Del Mar Awards of the society.
Figure 6.
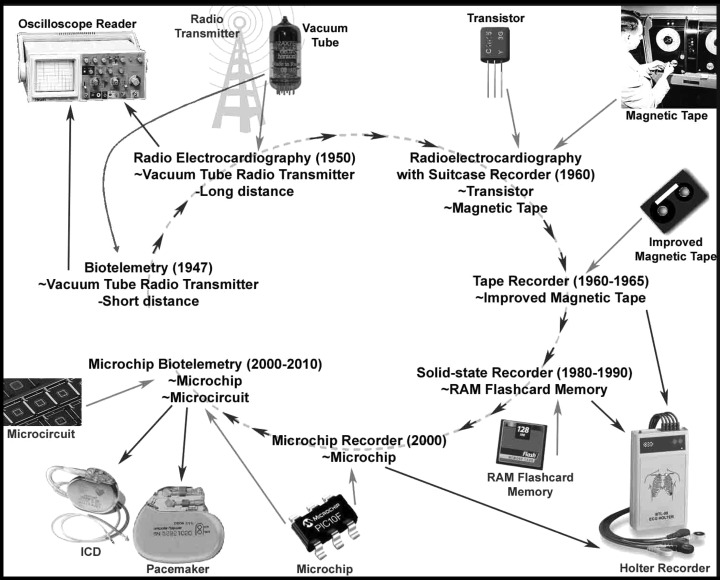
The circuitous applications of Holter technology.
Mr. Bruce Del Mar, now more than 90 years of age, can still be seen at the American Heart Association or American College of Cardiology Scientific Sessions prowling the commercial exhibits and scientific presentations to determine the advances that could be potentially applied to the Holter technology industry.
REFERENCES
- 1. Kolliker A, Muller H. Nachweis der negativen Schwankung des Muskelstromes um naturlich sich contrahirenden Muskel. Verh Phys Med Ges 1856;6: 528–533. [Google Scholar]
- 2. Waller AD. A demonstration of electromotive changes accompanying the heart's beat. J Physiol 1887;8: 229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Einthoven W. Un nouveau galvanometre. Arch Neerl Sc Ex Nat 1901;6: 625–633. [Google Scholar]
- 4. Ershler I. Willem Einthoven—The man. Arch Intern Med 1988;148: 453–455. [DOI] [PubMed] [Google Scholar]
- 5. Roberts WC, Silver MA. Norman Jefferis Holter and ambulatory ECG monitoring. Am J Cardiol 1983;52: 903–906. [DOI] [PubMed] [Google Scholar]
- 6. Gengerelli JA, Holter NJ. Experiments on stimulation of nerves by alternating electrical fields. Proc Soc Exp Biol Med 1941;46: 522–534. [Google Scholar]
- 7. Holter NJ, Gengerelli JA. Remote recording of physiological data by radio. Rocky Mt Med J 1949;46: 747–751. [PubMed] [Google Scholar]
- 8. Gengerelli JA, Holter NJ, Glasscock WR. Magnetic fields accompanying transmission of nerve impulses in the frog's sciatic. J Psychol 1961;52: 317–326. [DOI] [PubMed] [Google Scholar]
- 9. Holter NJ. Historical background and development of ambulatory monitoring In Jacobsen NK, Yarnall SR. (eds.): Ambulatory Monitoring. Seattle , Washington , MCSA, 1976, pp. 1–9. [Google Scholar]
- 10. Holter NJ. Radioelectrocardiography: A new technique for cardiovascular studies. Ann N Y Acad Sci 1957;65: 913–923. [DOI] [PubMed] [Google Scholar]
- 11. Holter NJ. New method for heart studies. Continuous electrocardiography of active subjects over long periods is now practical. Science 1961;134: 1214–1220. [DOI] [PubMed] [Google Scholar]
- 12. Corday E, Bazika V, Lang TW. Detection of phantom arrhythmias and evanescent electrocardiographic abnormalities: Use of prolonged direct electrocardiorecording. JAMA 1965;193: 417. [DOI] [PubMed] [Google Scholar]
- 13. Corday E. Historical vignette celebrating the 30th anniversary of diagnostic ambulatory electrocardiographic monitoring and data reduction systems. J Am Coll Cardiol 1991;17: 286–292. [DOI] [PubMed] [Google Scholar]
- 14. MacInnis HF. The clinical application of radioelectrocardiography. Can Med Assoc J 1954;70: 574. [PMC free article] [PubMed] [Google Scholar]
- 15. Kennedy HL. History In: Ambulatory Electrocardiography: Including Holter Technology. Philadelphia , Lea & Febiger, 1981, pp. 3–10. [Google Scholar]
- 16. Kennedy HL. Instrumentation In: Ambulatory Electrocardiography: Including Holter Technology. Philadelphia , Lea & Febiger, 1981, pp. 11–32. [Google Scholar]
- 17. Kennedy HL. Ambulatory (Holter) electrocardiography technology. Cardiol Clin 1992;10: 341–359. [PubMed] [Google Scholar]
- 18. Kennedy HL. Ambulatory (Holter) electrocardiography recordings In Zipes D, Jalife J. (eds.): Cardiac Electrophysiology: From Cell to Bedside, 2nd Edition Philadelphia , WB Saunders, 1995, pp. 1024–1038. [Google Scholar]
- 19. Grubman EM, Pavri BB, Shipman T, et al Cardiac death and stored electrograms in patients with third‐generation implantable cardioverter‐defibrillators. J Am Coll Cardiol 1998;32: 1056–1062. [DOI] [PubMed] [Google Scholar]
- 20. Kennedy HL, Bavishi NS, Buckingham TA. Ambulatory (Holter) electrocardiography signal‐averaging: A current perspective. Am Heart J 1992;124: 1339–1346. [DOI] [PubMed] [Google Scholar]
- 21. Kleiger RE, Stein PK, Bigger JT Jr. Heart rate variability: Measurement and clinical utility. Ann Noninvasive Electrocardiol 2005;10: 88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brockmeier K, Aslan I, Hilbel T, et al T‐wave alternans in LQTS: Repolarization‐rate dynamics from digital 12‐lead Holter data. J Electrocardiol 2001;34(Suppl.):93–96. [DOI] [PubMed] [Google Scholar]
- 23. Schmidt G, Malik M, Barthel P, et al Heart‐rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction. Lancet 1999;353: 1390–1396. [DOI] [PubMed] [Google Scholar]
- 24. Clinical relevance of assessing QT dynamicity in Holter recordings. J Electrocardiol 1994;27(Suppl.):62–66. [DOI] [PubMed] [Google Scholar]
- 25. Hickey B, Heneghan C, De Chazal P. Non‐episode‐dependent assessment of paroxysmal atrial fibrillation through measurement of RR interval dynamics and atrial premature contractions. Ann Biomed Eng 2004;32: 677–687. [DOI] [PubMed] [Google Scholar]
- 26. Heilbron EL. Advances in modern electrocardiographic equipment for long‐term ambulatory monitoring. Card Electrophysiol Rev 2002;6: 185–189. [DOI] [PubMed] [Google Scholar]
- 27. American College of Physicians . Automated ambulatory blood pressure and self‐measured blood pressure monitoring devices: Their role in the diagnosis and management of hypertension. Ann Intern Med 1993;118: 889–892. [DOI] [PubMed] [Google Scholar]
- 28. Kennedy HL. Instrumentation In: Ambulatory Electrocardiography: Including Holter Technology. Philadelphia , Lea & Febiger, 1981, pp. 281–306. [Google Scholar]
- 29. Newman AB, Nieto FJ, Guidry U, et al Sleep Heart Health Study Research Group. Relation of sleep‐disordered breathing to cardiovascular disease risk factors: The sleep heart health study. Am J Epidemiol 2001;154: 50–59. [DOI] [PubMed] [Google Scholar]
- 30. De Chazal P, Penzel T, Heneghan C. Automated detection of obstructive sleep apnea at different time scales using the electrocardiogram. Physiol Meas 2004;25: 967–983. [DOI] [PubMed] [Google Scholar]
- 31. Fogel RI, Evans JJ, Prystowsky EN. Utility and cost of event recorders in the diagnosis of palpitation, presyncope and syncope. Am J Cardiol 1997;79: 207–208. [DOI] [PubMed] [Google Scholar]
- 32. Krahn AD, Klein GJ, Yee R, et al, for the Reveal Investigators . Use of an extended monitoring strategy in patients with problematic syncope. Circulation 1999;99: 406–410. [DOI] [PubMed] [Google Scholar]
- 33. Verrier RL, Nearing BD. Ambulatory ECG monitoring of T‐wave alternans for arrhythmia risk assessment. J Electrocardiol 2003;36(Suppl.):193–197. [DOI] [PubMed] [Google Scholar]
- 34. Verrier RL, Nearing BD, Kwaku KF. Noninvasive sudden death risk stratification by ambulatory ECG based T‐wave alternans analysis: Evidence and methodological guidelines. Ann Noninvasive Electrocardiol 2005;10: 110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Francis J, Wanatabe MA, Schmidt G. Heart rate turbulence: A new predictor for risk of sudden cardiac death. Ann Noninvasive Electrocardiol 2005;10: 102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stein PK, Duntley SP, Domitrovich PP, et al A simple method to identify sleep apnea using Holter recordings. J Cardiovasc Electrophysiol 2003;14: 1–7. [DOI] [PubMed] [Google Scholar]
- 37. Moss AJ, Hall WJ, Cannon DS, et al Improved survival with an implanted defibrillator in patients with coronary artery disease at high risk for ventricular arrhythmias. N Engl J Med 1996;335: 1933–1940. [DOI] [PubMed] [Google Scholar]
- 38. Buxton AE, Lee KL, Fisher JD, et al A randomized study of the prevention of sudden death in patients with coronary artery disease. N Engl J Med 1999;341: 1882–1890. [DOI] [PubMed] [Google Scholar]
- 39. Moss AJ, Zareba W, Hil WJ, et al Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346: 877–883. [DOI] [PubMed] [Google Scholar]
- 40. Bardy GH, Lee KL, Mark DB, et al, for the SCD‐HeFT Investigators . Amiodarone or an implantable cardioverter‐defibrillator for congestive heart failure. N Engl J Med 2005;352: 225–237. [DOI] [PubMed] [Google Scholar]
- 41. Hohnloser SH, Ikeda T, Bloomfield DM, et al T‐wave alternans negative coronary patients with low ejection fraction and benefit from defibrillator implantation. Lancet 2003;362: 125–126. [DOI] [PubMed] [Google Scholar]
- 42. Peppard PE, Young T, Palta M, et al Prospective study of the association between sleep‐disordered breathing and hypertension. N Engl J Med 2000;342: 1378–1384. [DOI] [PubMed] [Google Scholar]


