Abstract
Background: Increasing QRS duration may be of prognostic significance in patients with right bundle branch block (RBBB) and may assist in predicting overall cardiovascular risk.
Methods: To test this hypothesis, we examined the Computerized Patient Records of patients with complete and persistent RBBB. Primary and secondary end points were all‐cause and cardiac mortality. The effects of QRS duration on death rates were analyzed using the Cox proportional hazards regression model (P < 0.05). We identified 52,852 patients with EKGs and selected all those with diagnosis of RBBB (QRS ≥ 120 ms) between January 2000 and January 2004. Some patients had EKG records confirming RBBB since 1987. The QRS durations were categorized into four groups: 120–129, 130–139, 140–149, and ≥ 150 ms.
Results: A total of 997 (1.9%) patients (mean age 68.9 ± 10 years) with RBBB were followed for 1–226 (median 45) months. All‐cause mortality occurred in 344 (34.5%), cardiac deaths in 59 (5.9%), noncardiac in 191 (19.2%), and unknown causes in 94 (9.4%) patients. Mean left ventricular EF for cardiac patients was 38 ± 15%. In patients with cardiac deaths, QRS duration was associated with increased morality (P < 0.007). For every 10 ms increase in QRS duration, the risk of death rose by 26.6%. The effect of QRS duration on all cause mortality was not statistically significant (P < 0.43).
Conclusion: Increasing QRS duration was an independent predictor of cardiac mortality in patients with RBBB, but had no influence on all‐cause mortality. QRS duration has added prognostic information to the presence of right bundle branch block.
Keywords: right bundle branch block, QRS duration, cardiac risk, mortality
Left bundle branch block (LBBB) has been associated with increased mortality. 1 , 2 Studies on the effects of right bundle branch block (RBBB) on the other hand have yielded conflicting results. 3 , 4 Other studies have shown that both LBBB and RBBB are associated with increased mortality in patients with heart disease especially in those with myocardial infarction. 1 , 5 The population sampled and the study designs might have contributed to differences in outcome. Beside the mere presence of intraventricular conduction delay in RBBB, the duration of the delay may have more prognostic significance as the duration of QRS is important in ventricular synchrony. We postulated that longer QRS durations in patients with RBBB may be associated with increased mortality.
METHODS
Study Design and Patient Population
Using the MUSE CVR Information System (General Electric Medical System, Milwaukee, WI) we identified a total of 52,852 patients who had EKG in our hospital between January 2000 and January 2004. We selected all patients with the diagnosis of complete right bundle branch block (RBBB) (QRS ≥ 120 ms). The computerized system stores all of the patients' EKG from the time they enrolled at the hospital. Some patients had EKG records from 1987. The criteria for complete RBBB were QRS duration ≥120 ms, a secondary R wave (R′) greater than the initial R wave in the right precordial leads and a wide S wave in lead 1 and V6. The electrocardiograms were verified by coinvestigators who are cardiologists. The patients had several EKG tracings during the follow‐up period, which showed persistent RBBB. For each patient, we selected the longest QRS duration and categorized the patients according to this duration.
Inclusion and Exclusion Criteria
All patients aged ≥18 years identified by the MUSE system as having complete and persistent RBBB between January 2000 and January 2004 were included. We excluded electrocardiogram tracings with artifacts or other features that prevent accurate measurements of the QRS duration, such as P wave in atrial flutter aborting the QRS, displacements of ST segment in acute myocardial infarction and paced rhythm.
Data Collection
The Computerized Patient Record System of the Dayton Veterans Affairs (VA) Medical Center was used to obtain medical information of the patients. This record system is comprehensive and it allows tracking of the patients in all of the VA Health System, including the notification of deaths occurring outside of the hospital. Records of care elsewhere were documented by the patients' physicians and were available for review. All the patients could be accounted for throughout the study period.
Clinical Data
Demographic data, clinical diagnoses, comorbid conditions, dates the patients were last seen or died, causes of death, and duration of follow‐up were obtained from their electronic medical records. The primary end point was all‐cause mortality, and cardiac mortality was the secondary end point. Cardiac deaths were defined as death caused by congestive heart failure, myocardial infarction, or fatal cardiac arrhythmia.
Electrocardiographic Data
The EKG tracings were examined for QRS duration and morphology, axis deviation, presence or absence of atrioventricular block, and subsequent use of pacemaker after the diagnosis of RBBB. The patients were categorized into four groups according to the duration of QRS: group 1 = 120–129 ms, group 2 = 130–139 ms, group 3 = 140–149 ms, and group 4 ≥150 ms.
Statistical Analysis
Descriptive statistics were provided for each variable. The continuous variables were estimated as the mean value ± standard deviation and frequencies were provided for the discrete variables. Age‐adjusted risks for all‐cause and cardiac mortality were calculated for each QRS duration category using logistic regression model. Cox proportional hazards regression model was used to analyze the effect of QRS duration on all‐cause and cardiac mortality.
RESULTS
A total of 52,528 patients had electrocardiograms during the study period. Of these, 997 patients (987 males and 10 females) had complete and persistent RBBB (1.9%). Their mean age was 68 ± 10 years; they were followed up for 1–226 months (median 45 months). There were 420 (42.2%) patients with RBBB without clinically evident structural heart disease. Among the 997 patients, all‐cause mortality occurred in 344 (34.5%) patients. Of these, 59 (5.9%) died of cardiac, 191 (19.2%) of noncardiac, and 94 (9.4%) of unknown causes. Table 1 shows the characteristics of the study patients, categorization of QRS, and mean QRS duration in each category. More than one‐third of the patients had QRS duration ≥150 ms.
Table 1.
Patient Characteristics, Comorbid Conditions, and QRS Categorization
| Characteristic | N* (%) | Condition | N* (%) |
|---|---|---|---|
| Total | 997 (100) | HTN | 798 (80) |
| Male | 987 (98.9) | CAD | 510 (51.2) |
| Female | 10 (1.0) | AMI | 117 (11.7) |
| Race | CHF | 243 (24.4) | |
| White | 808 (81.0) | HLP | 539 (54.1) |
| Black | 118 (11.8) | COPD | 331 (33.2) |
| Other | 71 (7.1) | Cancer | 163 (16.3) |
| Alive | 653 (65.5) | AV block | |
| Died | 344 (34.5) | 1st deg | 215 (21.6) |
| Cardiac | 59 (5.9) | 2nd or 3rd | 6 (0.6) |
| Noncardiac | 191 (19.2) | Fascicular block | |
| Unknown | 94 (9.4) | Anterior | 369 (37.0) |
| Posterior | 19 (1.9) | ||
| QRS Duration(ms) | Mean (± SD in ms) | ||
| 120–129 | 118 (11.8) | 124.8 (±2.9) | |
| 130–139 | 219 (22.0) | 134.8 (±2.6) | |
| 140–149 | 295 (30.0) | 144.5 (±2.9) | |
| ≥150 | 365 (36.6) | 160.8 (±10.8) | |
*Total number, AMI = acute myocardial infarction; AV block = atrioventricular block; CAD = coronary artery disease; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; HLP = hyperlipidemia; HTN = hypertension.
Associated Comorbid Conditions
Comorbid conditions in this patient population consisted of hypertension, coronary artery disease, acute myocardial infarction, congestive heart failure, hyperlipidemia, and chronic obstructive pulmonary disease. The most common conduction abnormality found in association with RBBB was left anterior fascicular block followed by first‐degree atrioventricular (AV) block. Others included second‐ or third‐degree AV block, and left posterior fascicular block. The frequencies and percentages of these are also shown in Table 1.
RBBB and All‐Cause Mortality
The QRS duration as a continuous variable was not significant in its influence on all‐cause survival (P < 0.43) after adjusting for age and comorbid conditions. It also had no effect in the unadjusted analyses (P < 0.58). The age‐adjusted risk of death was similar to the unadjusted death risk because the average age was similar in the four categories of QRS (Table 2). The age‐adjusted categorized QRS duration did not show a statistically significant effect on all‐cause mortality (P < 0.40). Analysis of the unadjusted categorized QRS also did not show a statistically significant effect on all‐cause mortality. Figure 1 shows the survival curves demonstrating the effect of increasing QRS duration on all‐cause mortality.
Figure 1.
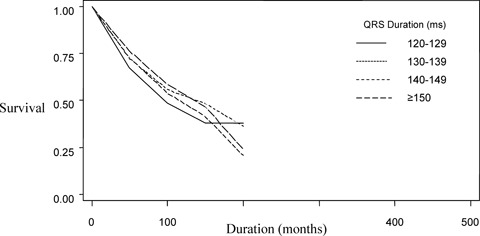
Survival curve showing no statistically significant difference in all‐cause mortality in the four categories of QRS duration (P < 0.40).
RBBB and Cardiac Mortality
The effect of QRS prolongation on cardiac mortality was adjusted for age and associated comorbid conditions. The age‐adjusted cardiac death risk is shown in Table 2. There was no significant difference between age‐adjusted and unadjusted cardiac death risks. The QRS duration as a continuous variable had a statistically significant effect on cardiac mortality (P < 0.007). The cardiac death risk increased as QRS duration increased. For every 10 ms increase in QRS duration, the risk of cardiac death increased by 26.6% (hazard ratio = 1.26). However, as a categorical (discretized) variable, QRS duration did not have a statistically significant effect on cardiac survival (P = 0.2217) after adjusting for comorbid conditions. Figure 1 shows the survival curve for all‐cause death in the four categories and Figure 2 demonstrates risk of cardiac death in the QRS categories. The survival rate for the group with the longest QRS duration (category 4) was significantly lower than for all other QRS categories (P < 0.009).
Table 2.
All‐Cause and Cardiac Mortality Within Categories of QRS Duration
| QRS Duration (ms) | Average Age (years) | Risk of Death (%) | Age Adjusted Death Risk (%) |
|---|---|---|---|
| All‐cause mortality | |||
| 120–129 | 68.5 | 30.8 | 29.9 |
| 130–139 | 68.9 | 29.8 | 28.6 |
| 140–149 | 67.5 | 35.7 | 34.6 |
| ≥ 150 | 69.5 | 37.5 | 38.3 |
| Cardiac mortality | |||
| 120–129 | 68.3 | 1.9 | 1.7 |
| 130–139 | 69.3 | 3.1 | 2.9 |
| 140–149 | 68.9 | 5.0 | 4.8 |
| ≥ 150 | 68.0 | 11.2 | 10.8 |
Duration of QRS, average age, percentage risk of death and percentage age‐adjusted risk of death in the four categories of QRS durations.
Figure 2.
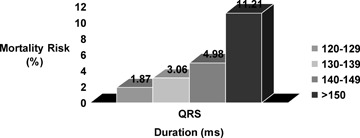
Risk of cardiac mortality in categories of QRS duration.
DISCUSSION
This study examined the impact of wide QRS duration on all‐cause and cardiac mortality in a large cohort of unselected veterans with RBBB enrolled in a VA hospital. The study showed that the wider the QRS duration, the higher the risk of cardiac death. However, there was no effect on all‐cause mortality. Unlike LBBB, RBBB may not be associated with structural heart disease. In the presence of heart disease, however, RBBB may have deleterious effects. In previous studies, patients with RBBB who had coronary artery disease or congestive heart failure have been shown to have increased mortality. 6 , 7 Schenkman et al. found a linear relationship between increased QRS duration and decreased ejection fraction. They also found that a prolonged QRS duration of 120 to 149 ms was associated with increased mortality at 60 months. 7 Excluding patients with heart failure, Hesse et al. found that in a preselected population of patients undergoing stress testing, RBBB strongly predicted mortality. 8
The prevalence of RBBB in our population of patients was 1.9%, which is similar to that previously found in other studies. Fahy et al. showed a prevalence of 1.6% among men older than 64 years of age. 9 The mean age of our patient population was 68 years. The preponderance of male gender and white race reflected the patient population of the VA Health System. Among the comorbid conditions, hypertension was the most prevalent, seen in 80% of patients. Coronary artery disease and hyperlipidemia were present in about half of the patients studied. Left anterior fascicular block was the most common conduction abnormality found with RBBB, occurring in more than one‐third of the patients. It has been shown that RBBB with left anterior fascicular block is an independent predictor of mortality in patients suspected of coronary artery disease. 10 Due to its anatomic course, the right bundle may be subjected to mechanical stretch and trauma, which may adversely affect conduction through it. Thus, conditions that cause structural heart disease may lead to RBBB and the degree of conduction delay may be more deleterious.
The electronic record system gave notifications of all deaths occurring within or outside the hospital. Specific causes of cardiac and noncardiac deaths, occurring within the hospital were well documented. The deaths occurring outside of the hospital accounted for a large portion of the unknown deaths, which could have included some cardiac deaths. The six patients who had second‐ or third‐degree AV block received permanent pacemaker treatment, thereby potentially preventing cardiac deaths. These factors could account for the relatively small number of cardiac deaths in this study. Other limitations of the study include the lack of female and nonwhite patients. However, there is evidence in a previous study to show that wider QRS complex predicts poor cardiovascular outcome in women with suspected myocardial ischemia. 11
It has been established that LBBB and widened QRS durations predict mortality in patients with heart failure. 12 , 13 , 14 , 15 Studies of patients with RBBB, however, have shown conflicting results. This may be due to different inclusion criteria for the specific QRS durations studied. Our study examined patients with complete and persistent RBBB in an unselected hospital population. It shows that the wider the QRS duration, the higher the risk of cardiac death. The risk of cardiac death rose by 26.6% for every 10 ms increase in QRS duration. Patients with QRS ≥ 150 ms had higher cardiac death rates after adjusting for age and comorbid conditions. This is in agreement with Desai et al., who found that qualitative QRS duration was a significant and independent predictor of cardiovascular mortality in the general population. 16 The cohort of patients in their study demonstrated 18.3% incidence cardiovascular deaths.
The QRS duration in our study had no statistically significant influence on all‐cause mortality. This is in contrast to the findings by Hesse et al. who found that complete RBBB was an independent predictor of risk of all‐cause mortality. 8 Among their 190 patients with RBBB, all‐cause death occurred in 24%. Although in outcome studies, it is more appropriate to use all‐cause mortality rather than cardiovascular mortality, the goal of examining QRS duration in our study was to determine if it can specifically predict cardiovascular deaths rather than noncardiac deaths. Our study is in agreement with the Reykjavik study, which showed a higher mortality from heart disease in men with RBBB, but that total mortality and other causes of death were not associated with RBBB either by univariate or multivariate analysis. 17 As demonstrated by our study, the Reykjavik study found an association between hypertension and RBBB. We also found coronary artery disease and hyperlipidemia in over half of our patients and chronic obstructive pulmonary disease in over one third. However, there was no difference in overall mortality after adjusting for these variables.
A widened QRS is a consequence of delayed ventricular activation resulting in depolarization and repolarization abnormalities. In their study of patients with isolated syncope and negative electrophysiologic studies, Da Costa et al., found that EKG abnormalities including RBBB and LBBB were predictive of significant arrhythmic events. 18 These events included sustained ventricular arrhythmia and sudden cardiac death. On the other hand the Multicenter Unsustained Ventricular Tachycardia Trial (MUSTT) found that only LBBB and not RBBB predicted the risk of arrhythmic death and total mortality in patients with coronary artery disease and left ventricular dysfunction. 19
To prevent sudden cardiac death, patients with left ventricular dysfunction and prolonged QRS durations are now being treated with implantable cardioverter‐defbrillators (ICDs). This practice is based on results of other large trials that show mortality benefit for such patients. For example, the Multicenter Automatic Defbirillator Implant Trial II (MADIT II) showed that patients with QRS duration ≥150 ms derived greatest survival benefit from implantable cardioverter defibrillators. 20 Similarly, the sudden cardiac death‐heart failure (SCD‐HeFT) trial showed lower mortality in patients with either ischemic or nonischemic cardiomyopathy and heart failure who had QRS duration ≥120 ms and were treated with ICDs, regardless of bundle branch morphology. 21 Thus patients with either RBBB or LBBB are expected to benefit from ICD treatment.
It would be important, therefore, to pay close attention to the QRS duration in patients with RBBB who may be at increased risk of cardiac death. For those without an apparent heart disease, a more vigorous search for the underlying heart disease might be sought within reasonable limit of cost‐effectiveness. Our study also shows that an EKG can be used to help predict cardiovascular risk in patients with RBBB. In addition to the current expensive invasive and noninvasive procedures used to assess cardiovascular risk, EKG is an inexpensive method of such risk assessment.
Disclosures: None
REFERENCES
- 1. Hod H, Goldbourt U, Behar S. Bundle branch block in acute Q wave inferior wall myocardial infarction. A high risk sub group of inferior myocardial infarction patients. The SPRINT Study Group. Secondary Prevention Reinfarction Israeli Nifedipine Trial. Eur Heart J 1995;16:471–477. [DOI] [PubMed] [Google Scholar]
- 2. Fahy GJ, Pinski SL, Miller DP, et al Natural history of isolated bundle branch block. Am J Cardiol. 1996;77:1185–1196. [DOI] [PubMed] [Google Scholar]
- 3. Ericksson P, Hansson PO, Eriksson H, et al Bundle branch block in a general male population: The study of men born in 1913. Circulation 1998;98:2492–2500. [DOI] [PubMed] [Google Scholar]
- 4. Rotman M, Triebwassser JH. A clinical and follow‐up study of right and left bundle branch block. Circulation 1975;51:477–484. [DOI] [PubMed] [Google Scholar]
- 5. Ricou F, Nicod P, Giplin E, et al Influence of right bundle branch block on short and long‐term survival after acute anterior myocardial infarction. Am J Cardiol 1991;17:858–863. [DOI] [PubMed] [Google Scholar]
- 6. Freedman RA, Alderman EL, Sheffield LT, et al Bundle branch block in patients with chronic coronary artery disease: Angiographic correlates and prognostic significance. J Am Coll Cardiol 1987;10:73–80. [DOI] [PubMed] [Google Scholar]
- 7. Shenkman HJ, Pampati V, Khandelwal AK, et al Congestive heart failure and QRS duration. Chest 2002;122:528–534. [DOI] [PubMed] [Google Scholar]
- 8. Hesse B, Diaz LA, Snader CE, et al Complete bundle branch block as an independent predictor of all‐cause mortality: Report of 7,073 patients referred for nuclear exercise testing. Am J Med 2001;110:253–259. [DOI] [PubMed] [Google Scholar]
- 9. Fahy J, Pinski L, Miller P, et al Natural history of isolated bundle branch block. Am J Cardiol 1996;77:1185–1190. [DOI] [PubMed] [Google Scholar]
- 10. Cortigiani L, Bigi R, Gigli G, et al Prognostic implications of intraventricular conduction defects in patients undergoing stress echocardiography for suspected coronary artery disease. Am J Med 2003;115:12–18. [DOI] [PubMed] [Google Scholar]
- 11. Triola B, Olson M, Reis S, et al Electrocardiographic predictors of cardiovascular outcomes in women: the National Heart, Lung and Blood Institute Sponsored Women's Ischemic Syndrome Evaluation (WISE) Study. J Am Coll Cardiol 2005;46:51–56. [DOI] [PubMed] [Google Scholar]
- 12. Padeletti L, Giaccardi M, Turrni F, et al Influence of QRS prolongation on the natural history of CHF. E Heart J Suppl 2004;6:D79–D82. [Google Scholar]
- 13. Baldasseroni S, Opasich C, Gorini M, et al Left bundle branch block is associated with increased 1‐year sudden and total mortality rate in 5,517 outpatients with congestive heart failure report from Italian network on congestive heart failure. Am Heart J 2002;143:398–405. [DOI] [PubMed] [Google Scholar]
- 14. Iuliano S, Fisher S, Karasik P, et al QRS duration and mortality in patients with congestive heart failure. Am Heart J 2002;143:1085–1091. [DOI] [PubMed] [Google Scholar]
- 15. Gottipaty VK, Krelis SP, Lu F, et al The resting electrocardiogram provides a sensitive and inexpensive marker of prognosis in chronic congestive heart failure. J Am Coll Cardiol 1999;33(Suppl A):145A. [Google Scholar]
- 16. Desai AD, Yaw TS, Yamazaki T, et al Prognostic significance of quantitative QRS duration. Am J Med 2006;119:600–606. [DOI] [PubMed] [Google Scholar]
- 17. Thrainsdottir IS, Hardarson T, Thorgeirsson G, et al The epidemiology of right bundle branch block and its association with cardiovascular morbidity—The Reykjavik Study. Eur Heart J 1993;14:1590–1596. [DOI] [PubMed] [Google Scholar]
- 18. Da Costa A, Gulian L, Romeyer‐Bouchard, et al Clinical predictor of cardiac events in patients with isolated syncope and negative electrophysiologic study. International J Cardiol 2006;109:28–33. [DOI] [PubMed] [Google Scholar]
- 19. Zimetbaum PJ, Buxton AE, Bastsford W, et al Electrocardiographic predictors of arrhythmic deaths and total mortality in the Multicenter Unsustained Tachycardia Trial. Circulation 2004;110:766–769. [DOI] [PubMed] [Google Scholar]
- 20. Moss AJ, Zareba W, Hall WJ, et al Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877–883. [DOI] [PubMed] [Google Scholar]
- 21. Bardy GH, Lee KL, Mark DB, et al Amiodarone or an implantable cardioverter‐defibrillator for congestive heart failure. N Engl J Med 2005;352:225–237. [DOI] [PubMed] [Google Scholar]


