Abstract
Background: Ibutilide and amiodarone are used for the pharmacological conversion of atrial fibrillation (AF) or flutter (AFl), but their efficacy is rather moderate.
Methods: To test whether the use of ibutilide as a first‐choice drug and of amiodarone as a second‐line treatment provides a rapid, effective, and safe algorithm for conversion of recent‐onset AF or AFl to sinus rhythm (SR), 85 consecutively recruited patients (59 women; mean age 69.7 ± 0.9 years) with AF or AFl of recent onset received 1 or 2 mg of ibutilide infusion. In the case of ibutilide failure, amiodarone was given (6 mg/kg IV infusion over 60 minutes followed by 1200 mg IV infusion over 24 hours) 4 hours later. Ten patients with AF or AFl of recent onset were used as controls. The maximum rate‐corrected QT interval was calculated in all patients and controls before the start of the study (baseline electrocardiogram (ECG)), 30 minutes later (30‐min ECG), and 4 hours later (4‐h ECG).
Results: Fifty‐eight (68%) patients reversed to SR within the first 4 hours after the end of ibutilide infusion. In those 27 patients in whom ibutilide failed, amiodarone was given. Twenty‐four of them (28%) were converted to SR during amiodarone infusion. Therefore, in total, 82 (96%) patients with recent‐onset AF or AFl were converted to SR. The 10 controls were monitored for the same time period as the study patients and 5 (50%) out of them were spontaneously converted to SR (P < 0.0001). No pro‐arrhythmia or any other side effects were noticed in the study patients or in the controls. QTc was moderately decreased before the start of amiodarone infusion in patients group, while it did not differ among the three ECGs in controls.
Conclusions: The combination of ibutilide as a first‐choice drug and of amiodarone infusion in the case of ibutilide failure provides an effective, rapid, and safe algorithm for restoration of SR in patients with AF or AFl of recent onset.
Keywords: ibutilide, amiodarone, recent onset, atrial fibrillation, atrial flutter
The restoration of sinus rhythm (SR) within the first 48 hours after the start of atrial fibrillation (AF) is associated with minimal risk for thromboembolic phenomena. 1 Therefore, attempts to pharmacologically convert recent‐onset AF should be performed by use of rapid, effective, and safe medications. Ibutilide is a pure class III antiarrhythmic agent that is considered to be a useful agent for the pharmacological cardioversion of recent‐onset AF or atrial flutter (AFl). 2 However, its efficacy to restore SR is rather moderate. 2 On the other hand, intravenous infusion of amiodarone is commonly used for restoring SR in patients with AF. 3 The combination of ibutilide and amiodarone in a therapeutic algorithm to achieve maximal conversion rate of AF or AFl to SR has not been thoroughly investigated in the past. 4 , 5 , 6
The present study was undertaken to test the hypothesis that the use of ibutilide as a first‐choice drug and of amiodarone as a second‐line treatment provides a rapid, effective, and safe algorithm for conversion of recent‐onset AF or AFl to SR.
METHODS
Study Population
The study population consisted of 85 consecutively recruited patients (59 women; mean age 69.7 ± 0.9 years) admitted to the hospital because of a symptomatic episode of AF or AFl of recent onset (<2 days). All patients underwent physical examination, 12‐lead electrocardiogram (ECG), and serial blood tests. No patient had clinically overt heart failure (NYHA classes II–IV) or history of a recent (<1 month) previous myocardial infarction. No patient showed severe (<50 beats/min) bradycardia on admission ECG. Serum potassium levels were >4 mEq/L in all patients. Routine medications were not withheld during patients' evaluation. Excluded from the study were patients with left or right bundle branch block, atrioventricular block, ventricular pre‐excitation, prior pacemaker implantation, or pericarditis. Patients receiving digitalis or any drugs known to influence the QT interval were also excluded. Ten patients (8 women; mean age 67.2 ± 1.4 years) with recent‐onset AF or AFl who fulfilled the above inclusion and exclusion criteria were used as controls.
One milligram of ibutilide fumarate was given in a 10‐minute slow intravenous infusion in all 85 patients. The same dose was repeated 10 minutes later in case the arrhythmia persisted. Ibutilide infusion was stopped in the case of arrhythmia conversion to SR or if significant pro‐arrhythmia ensued. All patients were continuously monitored during ibutilide infusion and for 4 hours afterwards. In the case of arrhythmia persistence, amiodarone infusion was started 4 hours after the end of the second ibutilide infusion. Amiodarone infusion was given as follows: 6 mg/kg IV infusion over 60 minutes followed by 1200 mg IV infusion over 24 hours. Controls received an identical amount of saline solution as the study patients. Enoxaparine 40–60 mg bid was started in all patients or controls in whom arrhythmia persisted 24 hours after admittance to the hospital, while oral anticoagulants were given in those patients who were still on arrhythmia 24 hours later.
Digital 12‐lead resting ECGs were recorded in all patients and controls immediately before the start of the study (baseline ECG), 30 minutes later (30‐min ECG), and 4 hours later (4‐h ECG). The study was approved by our Hospital's Ethics Committee. Informed consent was obtained from all participants.
Twelve‐Lead Surface Electrocardiogram
In all subjects, 12‐lead digital ECGs were recorded in the supine resting position using a computer‐based ECG machine (Schiller AT2 Plus, Schiller AG, Switzerland). All 12 leads of each ECG were recorded simultaneously for 10 seconds and sampled at a rate of 1000 Hz. From each lead, the average complex was automatically calculated (SEMA‐200 1.81 software, Schiller AG, Switzerland). All QT interval measurements were automatically calculated by our analysis system (SEMA‐200 1.81 software, Schiller AG, Switzerland). The QT interval was measured from the QRS onset to the end of the T wave. The point of T wave offset was defined as the return to the baseline. 7 The maximum QT interval in any of the 12 ECG leads was corrected for heart rate using Bazett's formula (QTc maximum = QT maximum/√RR interval).
Statistical Analysis
Continuous variables are expressed as mean ± standard error of the mean. Comparisons between groups were performed with chi‐square test and two‐way analysis of variance where appropriate P values <0.05 were considered statistically significant.
RESULTS
There were no significant differences in the demographic or clinical characteristics between the two study groups (Table 1). From the 85 patients, 32 (38%) received 1 mg of ibutilide and converted to SR, while a 2 mg of the drug was given in the remaining 53 patients. In total, 58 (68%) patients reversed to SR within the first 4 hours after the end of ibutilide infusion. All 10 (100%) patients with AFl reversed to SR after ibutilide infusion, while 48 from the 75 (64%) patients with AF were converted to SR after ibutilide infusion (P = 0.005). The mean time from the start of ibutilide infusion to the restoration of SR was 43 ± 8 minutes. In those 27 patients in whom ibutilide failed to restore SR, amiodarone was given. Twenty‐four (28%) patients were converted to SR during amiodarone infusion. Therefore, in total, 82 (96%) patients with recent‐onset AF or AFl were converted to SR. The remaining 3 patients who failed to convert to SR were discharged on oral anticoagulants and scheduled for DC cardioversion. The 10 controls were monitored for the same time period as the study patients and 5 (50%) out of them were spontaneously converted to SR. Therefore, the combination of ibutilide infusion as a first‐choice drug and of amiodarone infusion in the case of ibutilide failure achieved restoration of SR in patients with AF or AFl of recent onset in a statistically significant way (P < 0.0001). No pro‐arrhythmia or any other side effects were noticed in the study patients or in the controls. Only 1 patient showed a transient episode of asymptomatic bradycardia during amiodarone infusion.
Table 1.
Clinical and Demographic Characteristics of Patients and Controls
| Characteristic | Patients (n = 85) | Controls (n = 10) | P value |
|---|---|---|---|
| Age (years) | 69.7 ± 0.9 | 67.2 ± 1.4 | 0.394 |
| Male n (%) | 26 (30%) | 2 (20%) | 0.157 |
| Duration of the last episode (h) | 19.5 ± 3.3 | 22.3 ± 1 | 0.750 |
| LAD (mm) | 39.3 ± 3.2 | 38.7 ± 0.4 | 0.945 |
| LVEF (%) | 49.5 ± 2 | 50.8 ± 0.7 | 0.836 |
| Disease | |||
| Hypertension | 48 (56%) | 6 (60%) | |
| Coronary artery disease | 19 (22%) | 2 (20%) | |
| COPD | 6 (7%) | 1 (10%) | |
| Lone | 12 (14%) | 1 (10%) | |
COPD = chronic obstructive pulmonary disease; LAD = left atrial maximal diameter; LVEF = left ventricular ejection fraction.
The differences in the heart rate and the maximum rate‐corrected QT interval (QTc) among the baseline, the 30‐minute, and the 4‐hour ECGs are presented in Figures 1 and 2, respectively. The heart rate was significantly decreased after the start of ibutilide infusion in patients group, while it did not differ among the three ECGs in controls (Fig. 1). The maximum QTc interval was moderately decreased before the start of amiodarone infusion in patients group, while it did not differ among the three ECGs in controls (Fig. 2). The QRS duration did not differ among the three ECGs neither in patients, nor in controls.
Figure 1.
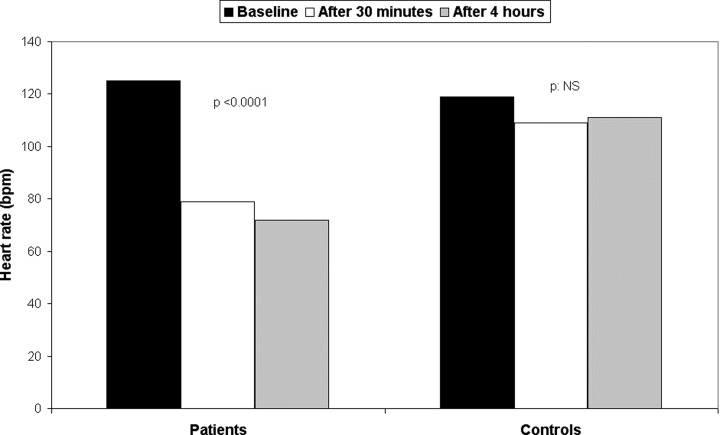
Differences in the heart rate among the baseline, the 30‐minute, and the 4‐hour ECGs.
Figure 2.
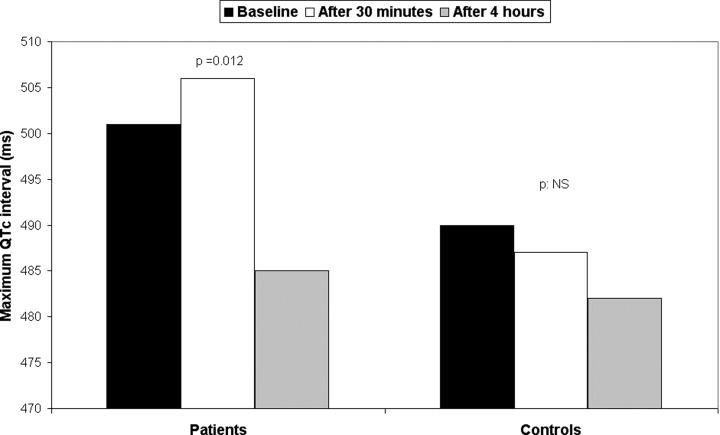
Differences in the maximum rate‐corrected QT interval (QTc) among the baseline, the 30‐minute, and the 4‐hour ECGs.
DISCUSSION
The present study demonstrated that the combination of ibutilide as a first‐choice drug and of amiodarone infusion in the case of ibutilide failure provides an effective, rapid, and safe algorithm for restoration of SR in patients with AF or AFl of recent onset.
Restoration of Sinus Rhythm by Use of Ibutilide or Amiodarone
Ibutilide is an antiarrhythmic agent with minimal hemodynamic, but major electrophysiologic effects that lead to its characterization as a class III agent. Ibutilide is considered to be a useful agent for the pharmacological cardioversion of AF or AFl. 2 However, its efficacy to restore SR is rather moderate, 2 although efficacy rates around 80% have been reported in patients with AF or AFl episodes of recent‐onset. 8 , 9
Amiodarone is an antiarrhythmic class III agent with unique electrophysiologic properties. Amiodarone is commonly used for conversion of recent‐onset AF. 3 The reported efficacy of intravenous amiodarone infusion for restoration of SR in previous studies was found to be around 80%. 3 , 10 Only in one study, 11 efficacy reached 92% of patients following a total 24‐hour dose of 3.0 g of amiodarone which is significantly higher than ours and those previously reported. 3 , 10
In a previous study, 5 ibutilide and amiodarone were found equally effective in suppressing immediate recurrences of AF, while in another study, ibutilide was able to restore SR in 81.5% of patients with AF or AFl of recent onset in whom low‐dose amiodarone infusion was unsuccessful. 4 Only in one previous publication, 6 amiodarone was administered in patients after cardiac surgery and AF of recent onset in whom ibutilide infusion failed to restore SR. In that study, ibutilide and amiodarone showed a rather similar efficacy (45% and 50%, respectively) for restoration of SR during the first 4 hours of treatment. 6 In our study, ibutilide was able to restore SR in 68% of patients with AF or AFl of recent‐onset. The administration of amiodarone infusion in those patients who failed to respond to ibutilide resulted in restoration of SR in 28% of the patients in the next 24 hours. Therefore, this therapeutic algorithm that combined ibutilide infusion as a first‐choice drug and amiodarone as a second‐line treatment resulted in restoration of SR in 96% of patients who were admitted with recent‐onset AF or AFl. This is statistically significant when compared to the 50% spontaneous restoration rate of SR which was demonstrated in our control group. Spontaneous conversion rates around 50% in patients with AF of 1 week or less have been reported previously. 12 , 13 The use of amiodarone infusion in those patients who failed to respond to ibutilide did not increase the risk of pro‐arrhythmia in our study population. Neither pro‐arrhythmia nor hypotension was noticed after the use of this therapeutic algorithm, as previously reported. 6 , 9 Only 1 patient showed an episode of bradycardia during amiodarone infusion which was transient and asymptomatic.
Ibutilide‐Induced Alterations in the Maximum QTc Interval
In previous studies, ibutilide significantly prolonged the QTc interval in ECG studies in healthy volunteers and patients with AF or AFl. 14 , 15 , 16 , 17 This effect was dose‐related and was directly correlated to plasma ibutilide concentrations. 15 In this study, the mean maximum QTc interval showed a moderate, nonsignificant increase from the baseline to the 30‐minute (post‐ibutilide) ECG and a significant decrease in the 4‐hour (pre‐amiodarone) ECG, 4 hours later (Fig. 2). On the other hand, the maximum QTc interval did not differ among the three ECGs, in controls. QTc interval alterations after ibutilide infusion may be attributed not only to heart rate changes but also to ventricular repolarization alterations during ibutilide infusion, as previously reported. 8 Furthermore, we cannot exclude the impact of the underlying heart disease and of the concomitant medications already administered in our study patients on the observed differences in the maximum QTc interval between the two study groups. Although a prolonged mean QTc interval was recorded during and after ibutilide infusion, none of our patients demonstrated ibutilide‐induced pro‐arrhythmia.
CONCLUSIONS
The present study demonstrated that the combination of ibutilide as a first‐choice drug and of amiodarone infusion in the case of ibutilide failure provides an effective, rapid, and safe algorithm for restoration of SR in patients with AF or AFl of recent onset. Future studies are needed to define the efficacy and the safety of this therapeutic algorithm to restore SR in other groups of patients with AF or AFl.
REFERENCES
- 1. Lip GH, Hart RG, Conway DSG. Antithrombotic therapy for atrial fibrillation. Br Med J 2002;325: 1022–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Foster RH, Wilde MI, Markham A. Ibutilide. A review of its pharmacological properties and clinical potential in the acute management of atrial flutter and fibrillation. Drugs 1997;54: 312–330. [DOI] [PubMed] [Google Scholar]
- 3. Vardas PE, Kochiadakis GE, Igoumenidis NE, et al Amiodarone as a first‐choice drug for restoring sinus rhythm in patients with atrial fibrillation. Chest 2000;117: 1538–1545. [DOI] [PubMed] [Google Scholar]
- 4. Hennersdorf MG, Perings SM, Zuhlke C, et al Conversion of recent‐onset atrial fibrillation or flutter with ibutilide after amiodarone has failed. Intensive Care Med 2002;28: 925–929. [DOI] [PubMed] [Google Scholar]
- 5. Oral H, Ozaydin M, Tada H, et al Comparison of amiodarone versus ibutilide for the prevention of immediate recurrences of atrial fibrillation during pulmonary vein isolation. Am J Cardiol 2002;90: 492–495. [DOI] [PubMed] [Google Scholar]
- 6. Bernard EO, Schmid ER, Schmidlin D, et al Ibutilide versus amiodarone in atrial fibrilation: A double‐blinded, randomized study. Crit Care Med 2003;31: 1031–1034. [DOI] [PubMed] [Google Scholar]
- 7. Zabel M, Acar B, Klingenheben T, et al Analysis of 12‐lead T‐wave morphology for risk stratification after myocardial infarction. Circulation 2000;102: 1252–1257. [DOI] [PubMed] [Google Scholar]
- 8. Dilaveris P, Theoharis A, Giaouris P, et al Ibutilide‐induced alterations in electrocardiographic and spatial vectorcardiographic descriptors of ventricular repolarization. Clin Cardiol 2004;27: 359–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Varriale P, Sedighi A. Acute management of atrial fibrillation or flutter in the critical care unit: Should it be ibutilide? Clin Cardiol 2000;23: 265–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cybulski J, Kulakowski P, Budaj A, et al Intravenous amiodarone for cardioversion of recent‐onset atrial fibrillation. Clin Cardiol 2003;26: 329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cotter G, Blatt A, Kaluski E, et al Conversion of recent onset paroxysmal atrial fibrillation to normal sinus rhythm: The effect of no treatment and high‐dose amiodarone. A randomized, placebo‐controlled study. Eur Heart J 1999 December;20(24):1833–1842. [DOI] [PubMed] [Google Scholar]
- 12. Falk RH, Knowlton AA, Bernard SA, et al Digoxin for converting recent‐onset atrial fibrillation to sinus rhythm. A randomized, double‐blinded trial. Ann Intern Med 1987;106: 503–506. [DOI] [PubMed] [Google Scholar]
- 13. Tejan‐Sie SA, Murray RD, Black IW, et al Spontaneous conversion of patients with atrial fibrillation scheduled for electrical cardioversion. An ACUTE trial ancillary study. J Am Coll Cardiol 2003;42: 1638–1643. [DOI] [PubMed] [Google Scholar]
- 14. Jungbluth GL, VanderLugt JT, Welshman IR. Relationship between subject age and QTc interval prolongation induced by the class III antiarrhythmic drug ibutilide. (abstract) Clin Pharmacol Ther 1996;59: 164. [Google Scholar]
- 15. VanderLugt JT, Gaylor SK, Wakefield LK. Effects of ibutilide fumarate, a new class III antiarrhythmic agent in man. (abstract) Clin Pharmacol Ther 1991;49: 188. [Google Scholar]
- 16. Ellenbogen KA, Stambler BS, Wood MA, et al Efficacy of intravenous ibutilide for rapid termination of atrial fibrillation and atrial flutter: A dose response study. J Am Coll Cardiol 1996;28: 130–136. [DOI] [PubMed] [Google Scholar]
- 17. Stambler BS, Wood MA, Ellenbogen KA, et al Efficacy and safety of repeated intravenous doses of ibutilide for rapid conversion of atrial flutter or fibrillation. Circulation 1996;94: 1613–1621. [DOI] [PubMed] [Google Scholar]


