Recently, a group of ECG experts, invited by the International Society for Holter and Noninvasive Electrocardiography (ISHNE), prepared a consensus document regarding new terminology of myocardial walls and new classification of Q‐wave myocardial infarction, based on correlation between ECG findings and cardiac magnetic resonance (CMR) imaging. 1 Since this initiative was organized under auspices of ISHNE, this brief editorial provides an overview of key statements regarding new terminology of Q‐wave MI in ECG for the readers of the Annals.
The correlations of electrocardiographic Q‐wave MI and pathologic findings performed by Myers more than 50 years ago 2 , 3 , 4 , 5 led to the establishment of the following classification of Q‐wave myocardial infarction (MI) in ECG: Q in V1‐V2 – septal MI; Q in V3‐V4 – anterior MI; Q in V5‐V6 low lateral MI; Q in I‐VL high lateral MI; Q in II, III, VF – inferior MI. Later, Perloff 6 introduced the concept of “true” or “strict” posterior infarction in order to explain the RS morphology seen in V1‐V2, which occasionally can be seen in post‐MI patients. This author considered that the posterior wall was the basal part of the inferior wall that is bending upwards. In such case, infarction of this wall would produce an infarction vector directed foreword and high R wave would be seen in V1‐V2, as a mirror‐image of the Q wave registered in the posterior leads (Fig 1A). For decades cardiologists were convinced that the RS morphology in V1 in post‐MI patients is due to posterior infarction. This paradigm did not change even though different authors using different techniques (first pathologic correlation, 7 and posteriorly isotopic 8 and even contrast enhanced cardiac magnetic resonance [CE‐CMR]) 9 had already proved that infarction of the lateral wall was responsible for R wave in V1. Nevertheless, these works were not successful in changing the accepted opinion that R wave in V1 was due to posterior MI, probably because they did not point at that: in the majority of the cases the posterior wall does not exist and that infarction of this area (inferobasal segment of the inferior wall) cannot originate R wave in V1. Durrer 10 demonstrated that the myocardial zones which correspond to the posterior wall (now named Segment 4 or inferobasal), depolarizes after 40 ms when the recording of normal QRS complex has been initiated and thus, cannot originate Q wave (or R wave as a mirror‐image in V1‐V2). Although, in such case, a distortion of QRS complex and/or voltage reduction could be recorded.
Figure 1.
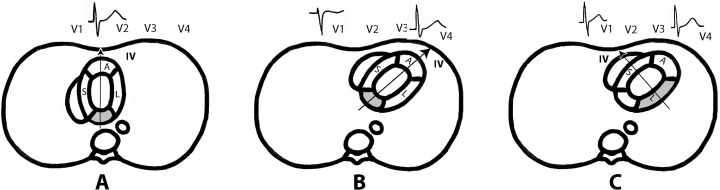
(A) Posterior (inferobasal) wall as it was wrongly considered to be placed. With this location an infarction vector of posterior or inferobasal infarction faces V1‐V2 and explains the RS pattern in these leads. (B) and (C) The real anatomic position of posterior (now named inferobasal segment) and lateral wall infarctions. The infarction vector of inferobasal segment faces V3‐V4 and not V1, and may contribute to the normal RS pattern seen in these leads. On the contrary, the vector of infarction of the lateral wall faces V1 and may explain RS pattern in this lead. However, we have to keep in mind that in the majority of cases, except in very lean individuals (see Fig 2C), the part of inferior wall that is rarely posterior just involves the area of late depolarization (Segment 4 or inferobasal). Therefore, in case of MI, there would not be changes in the first part of QRS because the infarction does not produce the presence of Q wave or equivalent (see text).
There were scientific doubts regarding the truthfulness of the established (for more than 50 years) 2 , 3 , 4 , 5 electrocardiographic – anatomic correlation. Fundamentally, there were two main reasons for these doubts: (1) a slight change of the precordial leads placing in the same patient can change the ECG morphology, making present or not the Q wave in one or another lead; and (2) there was not clear convincing anatomical evidence that the basal part of the inferior (or so called diaphragmatic) wall is surely directed upwards and thus, becoming “authentically” posterior.
Having in mind the reliability of CE‐CMR 9 , 10 , 11 in identification and localization of necrosis, we studied the ECG‐CMR correlation in cases of Q‐wave myocardial infarction. It was easily confirmed that in two thirds of the cases, the posterior wall did not exist, and the basal part of the inferior wall was laying on the diaphragm as a simple continuation of the rest of the wall (Fig 2). We evaluated cases in which exclusive or predominant posterior MI was present according to gadolinium enhancement in Segments 4 and 10 of AHA Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. 12 We observed that in these cases in V1, on the contrary of the expected, the morphology was rS instead of RS. The CE‐CMR images in horizontal axial sections may explain these discrepancies because they confirmed that the heart is oriented obliquely in postero‐anterior and right‐to‐left direction (Fig 1B and C), and not located strictly in postero‐anterior direction (Saint Valentine's approach) 13 as presented by the pathologists who study the excised heart. Thus, in the case of inferobasal segment infarction, previously known as posterior wall MI, the necrosis vector is directed towards V3‐V4 and does not originate change in R in V1 (Fig 1B). On the contrary, the lateral wall infarction originates necrosis vector that can produce RS morphology in V1 (Fig 1C). 14 , 15
Figure 2.
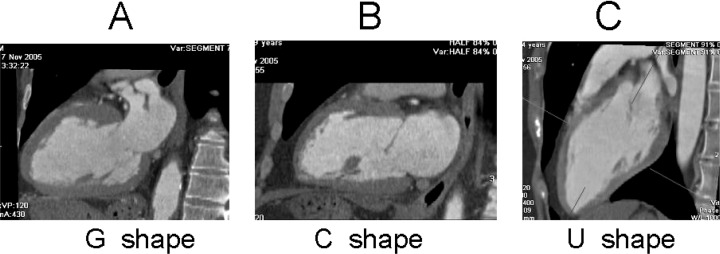
Sagittal‐oblique view in case of normal body built subject (A) (G shape 25%), in a man with horizontal heart (B) (C shape) and in a very lean subject (C) (U shape). We have found that the inferior wall does not bend upward in C shape (70% of the cases) (B) and only in very lean individuals with U shape (5%) the largest part of the wall is posterior (C).
The global correlation ECG‐CE‐CMR helped us to establish a new classification of Q‐wave MI with a very good concordance between ECG and localization of myocardial injury (88%). This classification is presented in Table 1. 14 , 15
Table 1.
New Terminology of the Cardiac Walls and ECG identification of Q‐Wave Myocardial Infarction based on Correlations with Infarction area recognized based on cardiac magnetic resonance (CMR) imaging. (Reproduced from ref. 1 with permission)
| Name | ECG Pattern | Infraction Area (CMR) |
|---|---|---|
| SEPTAL | Q in V1‐V2 |

|
| MID‐ANTERIOR | Q (qs or qr) in aVL (l) and sometimes in V2‐V3 without Q in V6 |

|
| APICAL‐ANTERIOR | Q in V1‐V2 to V3‐V6 |

|
| EXTENSIVE ANTERIOR | Q in V1‐V2 to V4‐V6, aVL and sometimes I |

|
| LATERAL | RS in V1‐V2 and/or wave in leads I, aVL, V6 and/or diminished R wave in V6 |

|
| INFERIOR | Q in II, III, aVF |

|
The most important changes are: (1) morphology with Q in VL and without Q in V6 corresponds to mid‐anterior MI (Diagonal branch occlusion) and not to high lateral infarction (left circumflex occlusion); (2) morphology RS in V1 is due to lateral infarction and not to posterior infarction; and (3) the presence of Q wave in intermediate precordial leads is not useful to distinguish between septal, anterior or lateral infarction.
We believe that the above classification should be adopted by clinicians to avoid continuous misinterpretation of localization of myocardial injury. We realize that Q in aVL was always recognized as lateral MI, but we need to accept that from now on it should be called mid‐anterior MI. Even more challenging will be to accept that RS in V1 reflects lateral, not posterior MI. Changing customs and tradition is very difficult and it takes time to get new ideas accepted but with the progress and openness of cardiology in the 21st century supported by rapid and broad dissemination of knowledge we will succeed.
In final words, we would like to stress that this consensus was an example of multi‐specialist teamwork (in this case including electrocardiologists and cardiac imaging experts) which should be encouraged in all areas of medicine, and that the existing paradigms should be reevaluated and challenged since new modalities provide more accurate testing.
REFERENCES
- 1. Bayés de Luna A, Wagner G, Birnbaum Y, et al. A new terminology for the left ventricular walls and for the locations of myocardial infarcts that present Q wave based on the standard of cardiac magnetic resonance imaging. A statement for healthcare professionals from a committee appointed by the International Society for Holter and Non invasive Electrocardiography. Circulation. 2006;114(16):1755–1760. [DOI] [PubMed] [Google Scholar]
- 2. Myers G, Howard AK, Stofer BE. Correlation of electrocardiographic and pathologic findings in posterior infarction. Am Heart J 1948;38:547–582. [DOI] [PubMed] [Google Scholar]
- 3. Myers GB, Howard A, Klein M, et al Correlation of electrocardiographic and pathologic findings in anteroseptal infarction. Am Heart J 1948;36:535–575. [DOI] [PubMed] [Google Scholar]
- 4. Myers GB, Howard A, Klein M, et al Correlation of electrocardiographic and pathologic findings in lateral infarction. Am Heart J 1948;37:374–417. [DOI] [PubMed] [Google Scholar]
- 5. Myers G, Howard AK, Stofer BE. Correlation of electrocardiographic and pathologic findings in anterior infarction. Am Heart J 1948;36:535–550. [DOI] [PubMed] [Google Scholar]
- 6. Perloff JK. The recognition of strictly posterior myocardial infarction by conventional scalar electrocardiography. Circulation 1964;30:706–718. [DOI] [PubMed] [Google Scholar]
- 7. Dunn W, Edwards J, Pruitt R. The electrocardiogram in infarction of the lateral wall of the left ventricle. A clinicopathological study. Circulation. 1956;14:540–555. [DOI] [PubMed] [Google Scholar]
- 8. Bough E, Boden W, Kenneth K, et al Left ventricular asynergy in electrocardiographic “posterior” myocardial infarction. J Am Coll Cardiol 1984;4:209–215. [DOI] [PubMed] [Google Scholar]
- 9. Moon JC, De Arenaza DP, Elkington AG, et al The pathologic basis of Q‐wave and non‐Q‐wave myocardial infarction: A cardiovascular magnetic resonance study. J Am Coll Cardiol 2004;44:554–608. [DOI] [PubMed] [Google Scholar]
- 10. Durrer D, Van Dam R, Freud G, et al Total excitation of the isolated human heart. Circulation 1970;41:899–910. [DOI] [PubMed] [Google Scholar]
- 11. Kim TY, Alturk N, Shaikh N, et al An electrocardiographic algorithm for the prediction of the culprit lesion site in acute anterior myocardial infarction. Clin Cardiol 1999;22:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cerqueira M. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the cardiac imaging committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539–542. [DOI] [PubMed] [Google Scholar]
- 13. Anderson RH, Razavi R, Taylor AM. Cardiac anatomy revisited. Review. J Anat 2004;205:159–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cino J, Pujadas S, Carreras F, et al Utility of contrast‐enhanced cardiovascular magnetic resonance to assess the sensitivity and specificity of different ECG patterns to locate Q‐wave myocardial infarction. J Cardiovasc Magn Res 2006;8:1–10. [DOI] [PubMed] [Google Scholar]
- 15. Bayés de Luna A, Cino JM, Pujadas S, et al Concordance of electrocardiographic patterns and healed myocardial infarction location detected by cardiovascular magnetic resonance. Am J Cardiol 2006;97:443–451. [DOI] [PubMed] [Google Scholar]


