Abstract
Background: Heart rate turbulence (HRT) has recently been described as a strong, independent risk stratifier in postinfarct patients. To date, however, the incidence of false positive HRT findings in adults is unknown. Therefore, we performed a blinded, retrospective analysis of HRT in a prospectively collected database of 110 apparently healthy persons to determine the prevalence and clinical significance of abnormal HRT findings in healthy controls using previously published cut‐off values.
Methods and Results: The study included 43 out of 110 apparently healthy adults, in whom a sufficient number of ventricular premature beats were available for HRT analysis on 24‐hour Holter recordings. The HRT slope was dichotomized at 2.5 ms per R‐R interval and HRT onset was dichotomized at 0% using previously established criteria to define an abnormal HRT analysis in postinfarct patients. Using these definitions, abnormal HRT results were found in 2 out of 43 controls (5%) for HRT slope and in 8 out of 43 controls (19%) for HRT onset without any cardiac deaths during 32 ± 15 months follow‐up.
Conclusions: The incidence of false positive HRT results in healthy middle‐aged volunteers is low for HRT slope (5%), but not for HRT onset (19%) when previously published cut‐off values are used to define abnormal HRT results. Thus, HRT slope dichotomized at 2.5 ms per R‐R interval, but not HRT onset dichotomized at 0%, may be used as a relatively specific tool for risk stratification in middle‐aged persons.
Keywords: heart rate turbulence analysis, risk stratification, healthy adults
Heart rate turbulence (HRT) describes fluctuations of sinus rhythm cycle length following single premature ventricular beats recorded on Holter electrocardiograms and is characterized by two numerical parameters termed HRT slope and HRT onset. 1 Based on a retrospective analysis of a training sample of 100 postinfarct patients, 1 , 2 HRT slope was dichotomized into abnormal and normal values at 2.5 ms per R‐R interval and HRT onset was dichotomized into abnormal and normal values at 0%, respectively. Using these cut‐off points for dichotomization into abnormal and normal HRT results on Holter recordings, this method has been found to be a quite potent risk stratifier in postinfarct patients. 1 , 3 The prognostic value of HRT analysis for risk stratification in nonischemic dilated cardiomyopathy is currently under investigation. 4 , 5 , 6 To date, however, only few data are available concerning HRT in apparently healthy persons. 7
METHODS
Heart rate turbulence was retrospectively analyzed on 24 hour Holter ECG in a prospectively collected database including 110 healthy volunteers aged 21–71 years who fulfilled the following inclusion criteria: (1) absence of any form of cardiovascular disease by history, physical examination, and noninvasive evaluation including 12‐lead electrocardiogram, bicycle ergometry, and echocardiography; (2) absence of noncardiovascular disorders including diabetes mellitus, arterial hypertension, kidney or liver disease; (3) absence of any medication other than hormonal contraception. The clinical characteristics of the 110 study persons as well as the results of noninvasive arrhythmia risk stratification without HRT analysis have been published previously. 8
Digital 24‐hour Holter recordings (Oxford FD2TM or FD3TM recorders, and Oxford Medilog Excel 2 system, version 7.5, Oxford Instruments, Abington, UK) were obtained from all 110 healthy volunteers at study entry. At least 20 hours of artifact‐free recording time was required for a Holter ECG to be included for analysis. Otherwise, the Holter ECG was discarded, and a new Holter ECG was started. Heart rate turbulence was analyzed by a single experienced observer (R.S.) who was completely blinded with regard to the person to whom the Holter recording belonged. Measures of HRT analysis were used as previously described by Schmidt et al. 1 with the following modifications: ventricular premature beats were accepted if they had (1) a coupling interval of less than 80% of the average of the preceding five sinus intervals; (2) a compensatory pause exceeding 120% of the preceding sinus intervals; and (3) if they were embedded into two preceding and 15 succeeding N‐N intervals. These N‐N intervals had to fulfill the following criteria: (1) cycle length of more than 300 ms but less than 2000 ms; (2) beat‐to‐beat difference of less than 200 ms; and (3) difference to the reference interval of less than 20%. A more detailed description of the filtering algorithm for HRT analysis used in this study is available on the Internet and can be downloaded from http://www.h-r-t.org. In order to exclude any bias during HRT analysis of healthy controls, all Holter R‐R interval files of the 110 healthy controls were copied on optical disks together with R‐R interval files from more than 400 digital Holter recordings from patients with structural heart disease in a random fashion. A total of 67 healthy persons without ventricular premature beats or with ventricular premature beats preceded by noise or artifacts were excluded from HRT analysis (Table 1). Heart rate turbulence was characterized by two parameters termed HRT slope and HRT onset. 1 HRT onset describes the relative shortening of R‐R intervals immediately following the compensatory pause of the index ventricular premature beat. HRT slope reflects the subsequent lengthening of R‐R intervals, which is quantified by the steepest linear regression between the R‐R interval count and the R‐R interval duration as previously described in detail by Schmidt et al. 1 All continuous variables are expressed as mean ± standard deviation. Comparisons between groups were made with standard statistical tests for continuous and categorical variables. A P value of <0.05 was considered statistically significant.
Table 1.
Clinical Characteristics of 110 Healthy Volunteers
| All Healthy Volunteers | HRT Analysis Possible | HRT Analysis Impossible a | |
|---|---|---|---|
| Number of healthy volunteers | 110 | 43 | 67 |
| Age (years) | 45 ± 12 | 50 ± 10 | 41 ± 11 b |
| Range | 21–71 | 29–71 | 21–67 |
| Men/women | 76/34 | 27/16 | 49/18 |
| Echocardiographic evaluation | |||
| LV end‐diastolic diameter (mm) | 50 ± 4 | 49 ± 4 | 50 ± 4 |
| LV ejection fraction (%) | 71 ± 5 | 70 ± 4 | 72 ± 4 |
| 24‐Hour Holter electrocardiogram | |||
| Mean R‐R interval (ms) | 817 ± 96 | 822 ± 103 | 814 ± 99 |
| SDNN (ms) | 154 ± 44 | 143 ± 35 | 161 ± 48 b |
| Frequent VPDs (>10/hour) | 7 (6%) | 7 (16%) | 0 (0%)b |
| Couplets of VPDs | 6 (5%) | 6 (14%) | 0 (0%)b |
| Nonsustained VT | 1 (1%) | 1 (2%) | 0 (0%) |
| Follow‐up results | |||
| Follow‐up duration (months) | 32 ± 15 | 28 ± 13 | 34 ± 16 |
| All‐cause mortality | 2 (2%) | 1 (2%) | 1 (2%) |
| Cardiac death | 0 (0%) | 0 (0%) | 0 (0%) |
HRT = heart rate turbulence; LV = left ventricular; SDNN = standard deviation of all normal R‐R intervals; VPD = ventricular premature depolarization; VT = ventricular tachycardia. aHRT analysis impossible due to the lack of premature ventricular beats on Holter; bP < 0.05.
RESULTS
The clinical characteristics of the 110 study persons are summarized in Table 1 stratified for persons with and without sufficient ventricular ectopy for HRT analysis. During 32 ± 15 months follow‐up, no cardiovascular events defined as myocardial infarction, stroke, or symptomatic arrhythmias and no cardiovascular deaths occurred in any study person. The clinical characteristics and follow‐up results of the 43 healthy volunteers with sufficient ventricular ectopy for HRT analysis are summarized in 2, 3, 4. An HRT slope ≤2.5 ms per R‐R interval was found in 2 of the 43 persons (5%), whereas HRT onset ≥0% was present in 8 of the 43 persons (19%) (Tables 2 and 3). The relation between age, gender, and HRT analysis is summarized in Figures 1 and 2. Whereas HRT slope showed a moderate but significant inverse relation with age, no relation was found between age and HRT onset (Fig. 1). In addition, HRT onset and HRT slope did not show significant gender‐related differences (Fig. 2).
Table 2.
Results of Heart Rate Turbulence in 43 Healthy Volunteers
| HRT Slope | HRT Onset | |
|---|---|---|
| Minimum | 1.12 | −0.121 |
| 25th percentile | 8.45 | −0.039 |
| Median | 13.04 | −0.025 |
| 75th percentile | 18.75 | −0.009 |
| Maximum | 48.40 | 0.161 |
| 95% confidence | 11.78–17.69 | −0.033 to −0.009 |
| interval |
Table 3.
Results of HRT Analysis Using Previously Described Cutoff Values
| HRT Slope ≤ 2.5 ms per R‐R Interval | HRT Slope > 2.5 ms per R‐R Interval | Sum of Patients | |
|---|---|---|---|
| HRT onset ≥ 0% | 2 (5%) | 6 (14%) | 8 (19%) |
| HRT onset < 0% | 0 (0%) | 35 (81%) | 35 (81%) |
| Sum of patients | 2 (5%) | 41 (95%) | 43 (100%) |
Table 4.
Relation Between Heart Rate Turbulence Analysis, Clinical Characteristics, and Follow‐Up Results in 43 Healthy Volunteers
| HRT Onset ≥0% | HRT Slope ≤ 2.5 ms per RRI | |||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Number of healthy volunteers | 8 (19%) | 35 (81%) | 2 (5%) | 41 (95%) |
| Age (years) | 49 ± 12 | 51 ± 10 | 58 ± 3 | 48 ± 5 a |
| Men/women | 6/2 | 21/14 | 1/1 | 26/15 |
| Echocardiographic evaluation | ||||
| LV end‐diastolic diameter (mm) | 48 ± 3 | 49 ± 5 | 50 ± 5 | 49 ± 4 |
| LV ejection fraction (%) | 70 ± 6 | 70 ± 4 | 63 ± 4 | 70 ± 4 |
| 24‐Hour Holter electrocardiogram | ||||
| Mean R‐R interval (ms) | 829 ± 96 | 820 ± 106 | 776 ± 93 | 824 ± 104 |
| SDNN (ms) | 148 ± 30 | 142 ± 36 | 118 ± 26 | 144 ± 35 |
| Frequent VPDs (>10/hour) | 1 (12%) | 6 (17%) | 0 (0%) | 7 (17%) |
| Couplets of VPDs | 1 (12%) | 5 (14%) | 0 (0%) | 6 (15%) |
| Nonsustained VT | 0 (0%) | 1 (3%) | 0 (0%) | 1 (2%) |
| Follow‐up results | ||||
| Follow‐up duration (months) | 34 ± 16 | 27 ± 13 | 48 ± 5 | 27 ± 13 |
| All‐cause mortality | 1 (12%)b | 0 (0%) | 1 (50%)b | 0 (0%) |
| Cardiac death | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
RRI = R‐R interval; other abbreviations as in Table 1. aP < 0.05. bDeath due to cancer, which was first diagnosed several months after study enrollment.
Figure 1.
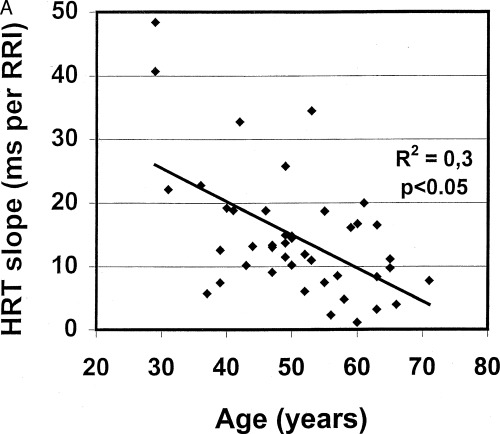
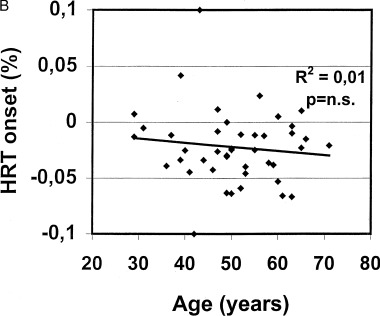
Relation between heart rate turbulence slope and age (A) and heart rate turbulence onset and age (B) in 43 healthy persons without cardiac events during follow‐up.
Figure 2.
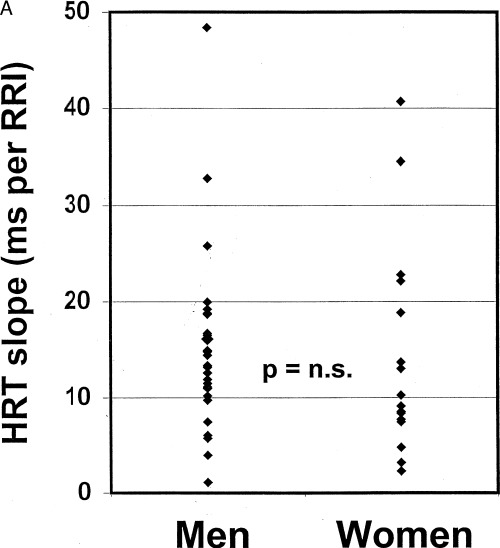
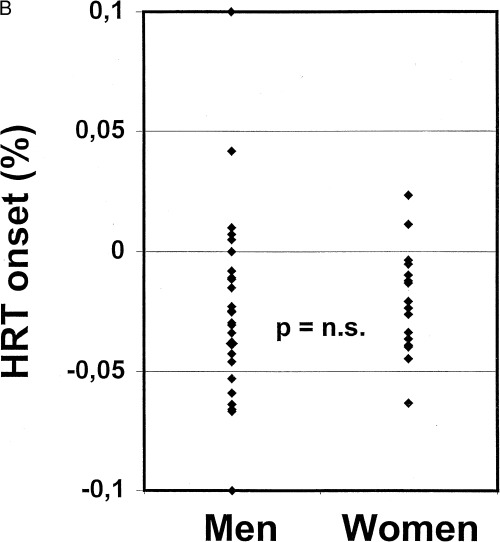
Distribution of heart rate turbulence results between healthy men and women stratified for turbulence slope (A) and turbulence onset (B).
DISCUSSION
In this study, we determined the prevalence and clinical significance of abnormal HRT findings in 43 out of 110 healthy middle‐aged persons using previously published cut‐off values to define abnormal findings. 1 Using these previously in postinfarct patients established criteria for HRT analysis; 1 abnormal results were found in 2 of the 43 healthy volunteers (5%) for HRT slope and in 8 of the 43 volunteers (19%) for HRT onset. Importantly, no cardiovascular deaths occurred in any of the study persons during a mean follow‐up of 32 months indicating that the observed abnormal HRT results in these healthy, middle‐aged persons are likely to represent false positive results of noninvasive risk stratification. A low incidence of false positive results of noninvasive risk stratification, however, should be considered as a prerequisite for risk stratification techniques in patients with heart failure in order to be used in interventional trials to prevent cardiac death or sudden cardiac death. The major finding of the present study is that the incidence of false positive HRT analyses in healthy volunteers is only 5% for HRT slope, whereas the incidence of false positive HRT analyses is as high as 19% when HRT onset ≥0% was used to define an abnormal result. 1 To date, only one previous study by Schwab et al. 7 reported the incidence of “abnormal” HRT results in healthy volunteers. Similar to the study, Schwab et al. 7 found a low incidence of abnormal HRT slope results (4%) compared to abnormal HRT onset results (24%). In contrast to the present study, however, Schwab et al. did not report follow‐up data in order to demonstrate, that “abnormal” HRT results represent false positive results.
STUDY LIMITATIONS
Although there was no evidence for cardiovascular disorders in any of the 110 volunteers by history, physical examination, and noninvasive evaluation including 12‐lead ECG, bicycle ergometry, and echocardiography, the presence of a cardiovascular disease cannot be ruled out with certainty. The presence of ventricular premature beats on Holter might represent a silent pathologic process, which may be undetectable by noninvasive cardiac evaluation. In addition, our study was not powered to evaluate the association between HRT parameters and mortality in these apparently healthy persons.
In conclusion, the incidence of false positive HRT results in apparently healthy middle‐aged volunteers is low for HRT slope (5%) but not for HRT onset (19%) when previously published cut‐off values are used to define abnormal HRT results. Thus, HRT slope dichotomized at 2.5 ms per R‐R interval, but not HRT onset dichotomized at 0%, may be used as a relatively specific tool for risk stratification in middle‐aged persons.
This study was supported by a grant from the German Science Foundation, Bonn, Germany (Grant no. GR 1130/2‐2).
REFERENCES
- 1. Schmidt G, Malik M, Barthel P, et al Heart‐rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction. Lancet 1999;353: 1390–1396. [DOI] [PubMed] [Google Scholar]
- 2. Schmidt G, Morfill GE, Barthel P, et al Variability of ventricular premature complexes and mortality risk. PACE 1996;19: 976–980. [DOI] [PubMed] [Google Scholar]
- 3. Ghuran A, Reid F, La Rovere MT, et al Heart rate turbulence‐based predictors of fatal and nonfatal cardiac arrest (The autonomic tone and reflexes after myocardial infarction substudy). Am J Cardiol 2002;89: 184–190. [DOI] [PubMed] [Google Scholar]
- 4. Davies LC, Francis DP, Ponikowski P, et al Relation of heart rate and blood pressure turbulence following premature ventricular complexes to baroreflex sensitivity in chronic congestive heart failure. Am J Cardiol 2001;87: 737–742. [DOI] [PubMed] [Google Scholar]
- 5. Voss A, Baier V, Schumann A, et al Postextrasystolic regulation patterns of blood pressure and heart rate in patients with idiopathic dilated cardiomyopathy. J Physiol 2002;538: 271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grimm W, Hoffmann J, Menz V, et al Prediction of major arrhythmic events and sudden cardiac death in dilated cardiomyopathy: The Marburg cardiomyopathy study design and description of baseline characteristics. Herz 2000;3: 189–199. [DOI] [PubMed] [Google Scholar]
- 7. Schwab JO, Coch M, Veit G, et al Post‐extrasystolic heart rate turbulence in healthy subjects: Influence of gender and basic heart rate. Circulation 2001;104(Suppl. II):490 (Abstract). [Google Scholar]
- 8. Grimm W, Lietke J, Müller HH. Prevalence of potential noninvasive arrhythmia risk stratification in healthy, middle‐aged persons. Ann. Noninvasive Electrocardiol 2003;8: 37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]


