Abstract
Cardiotoxicity that results from lithium overdose is uncommon and electrocardiographic (ECG) changes are rarely reported. However, some authors have specifically reported the occurrence of ischemic ECG changes due to a lithium overdose. This article describes a case that is demonstrating ECG changes that mimic inferior myocardial infarction during the course of chronic lithium treatment and showing QTc prolongation in this patient. The patients’ ECG changes were partially recovered after hemodialysis.
Ann Noninvasive Electrocardiol 2010;15(3):289–292
Keywords: electrocardiography, lithium, bipolar disorder
CASE
A 70‐year‐old female who suffered from hypertension (HT) and bipolar disorder presented to the emergency department (ED) with dizziness, somnolence, and disorientation of time and place. She reported that she had taken a daily dose of 300 mg of lithium for over 15 years. The patient's antihypertensive therapy also required her to take 16 mg of candesartan cilexetil and 12.5 mg of hydrochlorothiazide each day. She had no relevant cardiac history and did not complain of chest pain or shortness of breath. Seven days prior to the patient's visit to the ED, her psychiatrist had increased her lithium dose to 300 mg twice per day. Upon admission to the ED, the patient's vital signs were abnormal: according to her medical records, “she appeared to be confused and agitated,” and presented cool peripheries, a pulse of 135 bpm, and blood pressure of 90/60 mmHg. She was awake but her speech was incoherent. A cranial CT was conducted to further explore the patient's confused and ataxic state. The test did not reveal any areas of hemorrhagic infarct or mass. Her lithium level was 3.85 mEq/L (therapeutic blood level: 0.8 to 1.5 mEq/L). The patient's laboratory profile revealed a serum sodium level of 134 mmol/l, potassium at 3.5 mmol/l, and creatinine at 1.7 mg/dl. The patient's basic metabolic panel showed a white blood cell count of 8000/mm3. Furthermore, at her arrival, her plasma levels of both troponin I (Trp I) and creatine kinase‐MB (CK‐MB) were within the normal range (0.03 ng/dl and 2.7 ng/dl, respectively). Enzyme prosecutions were normal over 48 hours (CK‐MB: 3.8 ng/dl and Trp I: 0.04 ng/dl).
An electrocardiogram showed ST elevations in leads II, III, and aVF, accompanied by ST depressions in leads I, aVL, V5, and V6. Details from the electrocardiogram revealed V5 with 1 mm of ST‐segment depression, V6 with 2 mm of ST‐segment depression, DI with 1 mm ST‐segment depression, aVL with 1 mm ST‐segment depression, DIII with 2 mm ST‐segment elevation, and aVF with 1 mm ST‐segment elevation. The PR duration was 160 ms; the QT duration was 400 ms; and QTc (corrected QT duration by Bazett formula) was prolonged before and after hemodialysis (QTc: 480 and 481 ms, respectively) (Fig. 1).
Figure 1.
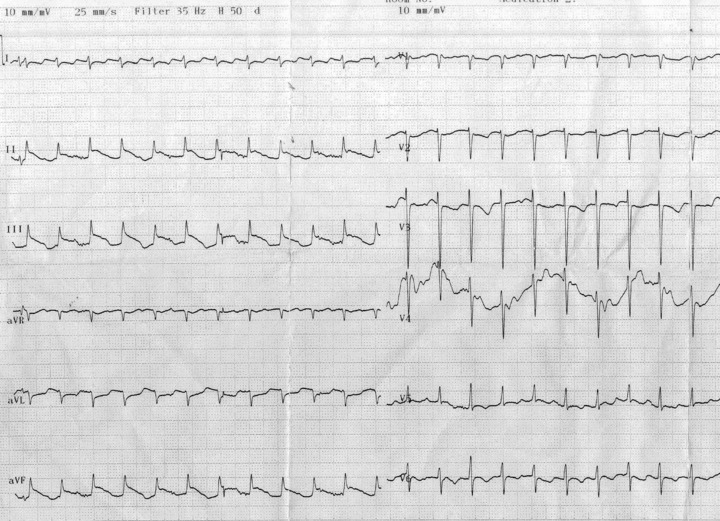
Twelve‐lead electrocardiogram at admission (heart rate: 135 bpm, PR duration: 210 ms, QT duration: 320 ms, QTc: 480 ms, QRS duration: 60 ms).
An echocardiogram showed minimal pericardial effusion, moderate mitral and mild aortic regurgitation, and normal wall motions. The ejection fraction of the left ventricle was calculated at 60% according to a modified Simpson's formula. Pulmonary systolic pressure was measured at approximately 30 mmHg. After two courses of hemodialysis for a total of 7 hours, the lithium level decreased to 0.87 mEq/L. The electrocardiogram showed partial recovery, but deep T inversions persisted in leads V1–V4 (Fig. 2).
Figure 2.
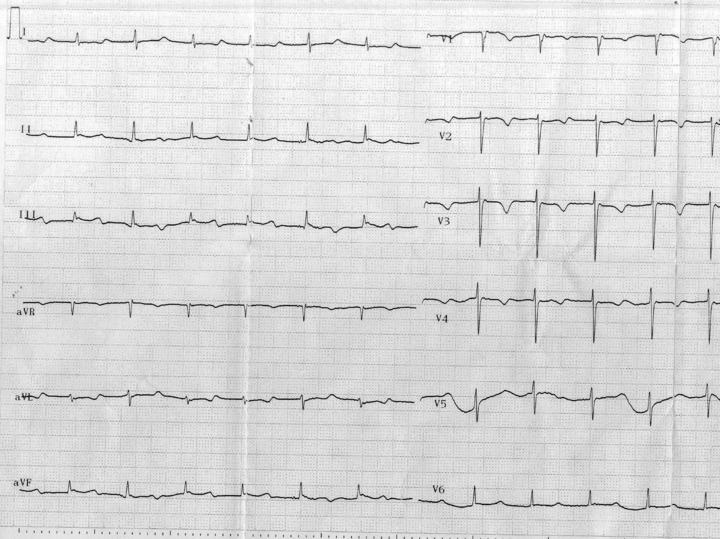
Twelve‐lead electrocardiogram after hemodialysis (heart rate: 79 bpm, PR duration: 260 ms, QT duration: 420 ms, QTc: 482 ms, QRS duration: 60 ms).
DISCUSSION
Lithium toxicity may be associated with variable electrocardiographic (ECG) changes including QT prolongation, sinus node dysfunction, ST‐segment changes, and T‐wave changes. 1 , 2 , 3 , 4 , 5 Darbar et al. showed lithium‐induced transient ST‐segment elevation (Brugada type 1 pattern) in the right precordial leads in therapeutic concentrations in 2 patients with bipolar disorder. 6 In these 2 patients, ST elevation was seen in leads V1 and V2. Lithium causes toxicity through several mechanisms including competition with sodium, potassium, calcium, and magnesium ions, each of these ions playing an important role in cellular membrane physiology.
We present a case of lithium toxicity that shows an unusual ECG pattern mimicking inferior ST‐segment elevation myocardial infarction (MI). ST‐segment changes suggesting ischemia due to lithium toxicity were first described by Puhr et al. 7 and Canan et al. 8 Puhr et al. reported that ST segments were elevated in the anterior leads with downward concavity, and T waves were biphasic. More specifically, V1 showed 1 mm of ST‐segment elevation, V2, 2 mm of ST‐segment elevation, and V3, 1.5 mm of ST‐segment elevation. 6 Canan et al. showed ST‐wave depressions in leads V2 and V3 and a common T‐wave inversion. But, our case was focused on ST elevations in leads II, III, and aVF accompanied by ST depressions and deep T inversions in leads V1–V4.
With an electrocardiogram suggesting an acute MI, cardiac enzymes and an emergency echocardiogram were used to rule out MI. Resolution of the ECG ST‐segment changes with hemodialysis suggested that ECG changes associated with lithium toxicity can be misinterpreted as cardiac ischemia.
The electrocardiogram also revealed QTc prolongation in this patient. Among the many psychotropic drugs, antipsychotics and antidepressants have proved to be determinants of QT prolongation. 9 Mamiya et al. reported that lithium concentration correlates with QTc intervals in patients with psychosis. 10
Our case involved an elderly female who experienced comorbid conditions including HT, hypovolemia, renal dysfunction, and candesartan and hydrochlorothiazide use. Our observations indicate that advanced age and the other comorbid conditions may have contributed to the development of intoxication symptoms. Age and HT were also important factors contributing to decreased creatinine clearence. In addition, reversible increases in serum lithium concentrations and toxicity have been reported during concomitant administration of lithium with angiotensin converting enzyme inhibitors, and with some angiotensin II receptor antagonists. Also, lithium generally should not be given with diuretics. Diuretic agents (such as hydrochlorothiazide) reduce the renal clearance of lithium and add a high risk of lithium toxicity.
In conclusion, emergency physicians, internal medicines, cardiologists, and also nurses should be reminded that patients may occasionally present with ECG changes that mimic MI because of lithium toxicity.
REFERENCES
- 1. Hsu CH, Liu PY, Chen JH, et al Electrocardiographic abnormalities as predictors for over‐range lithium levels. Cardiology 2005;103:101–106. [DOI] [PubMed] [Google Scholar]
- 2. Jacob AI, Hope RR. Prolongation of the Q‐T interval in lithium toxicity. J Electrocardiol 1979;12:117–119. [DOI] [PubMed] [Google Scholar]
- 3. Tilkian AS, Schroeder JS, Kao JJ. Cardiovascular effects of lithium in man: A review of the literature. Am J Med 1976;61:665–670. [DOI] [PubMed] [Google Scholar]
- 4. Farag S, Watson RD, Honeybourne D. Symptomatic junctional bradycardia due to lithium intoxication in patient with previously normal electrocardiogram. Lancet 1994;343:1371. [DOI] [PubMed] [Google Scholar]
- 5. Rosenqvist M, Bergfeldt L, Aili H, et al Sinus node dysfunction during long‐term lithium treatment. Br Heart J 1993;70:371–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Darbar D, Yang T, Churchwell K, et al Unmasking of Brugada syndrome by lithium. Circulation 2005;112:1527–1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Puhr J, Hack BJ, Early AJ, et al Lithium overdose with electrocardiogram changes suggesting ischemia. J Med Toxicol 2008;4:170–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Canan F, Kaya A, Bulur S, et al Lithium intoxication related multiple temporary ECG changes: A case report. Cases Journal 2008;1:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goodnich PJ, Jerry J, Parra F. Psychotropic drugs and the ECG: Focus on the QTc interval. Expert Opin Pharmacother 2002;3:479–498. [DOI] [PubMed] [Google Scholar]
- 10. Mamiya K, Sadanaga T, Sekita A, et al Lithium concentration correlates with QTc in patients with psychosis. J Electrocardiol 2005;38:148–151. [DOI] [PubMed] [Google Scholar]


