Abstract
Background: Brugada syndrome is associated with a risk for sudden death, but the arrhythmic risk in an individual Brugada syndrome patient is difficult to predict. Pathologic changes in the early repolarization phase of the ventricular action potential probably constitute part of the arrhythmogenic substrate in Brugada syndrome. Microvolt T wave alternans (TWA) assesses dynamic beat‐to‐beat changes in repolarization and has been suggested as a marker for repolarization‐related sudden death. We therefore tested whether TWA is an indicator for arrhythmias in Brugada syndrome with a focus on right precordial ECG leads.
Methods: We assessed TWA in nine symptomatic, inducible patients with established Brugada syndrome and in seven healthy controls. TWA was assessed at rest and during exercise using both standard methods and an algorithm that assesses TWA in the early ST segment and the right precordial leads.
Results: None of the Brugada patients developed TWA in this study irrespective of analysis at rest or during exercise, neither using standard methods nor when the early ST segment was included in the analysis. When the early ST segment was included in the analysis, nonsustained TWA was found in three out of seven, and sustained TWA in one control.
Conclusion: T wave alternans is not an appropriate test to detect arrhythmic risk in patients with Brugada syndrome.
Keywords: Brugada syndrome, sudden arrhythmic death, T wave alternans, risk stratification, non‐invasive tests, repolarization
Reversible ST segment elevation in the right precordial leads is the paramount sign of Brugada syndrome. 1 , 2 Patients with Brugada syndrome are at risk for sudden cardiac death, and it has been recommended to implant a defibrillator in these patients. 2 Some data, however, suggest that only a subgroup of patients may benefit from device implantation, 3 and the incidence of arrhythmic events appears low in the first year following defibrillator implantation. 3 , 4 Furthermore, some patients show ECG changes suggestive of Brugada syndrome but may not be at arrhythmic risk. 5 , 6 Given the invasive procedure needed to implant a defibrillator, additional methods are needed to better identify Brugada syndrome patients who would benefit from a defibrillator.
T wave alternans measures microvolt beat‐to‐beat changes in T‐wave amplitude and morphology caused by corresponding alternans of ventricular repolarization. 7 , 8 T wave alternans is a risk marker for arrhythmic death in patients with coronary artery disease and heart failure. 9 , 10 , 11 The Brugada syndrome causes transient alterations in the right ventricular action potential. 12 Microvolt T wave alternans therefore appears to be a promising technique to detect such changes, especially when right ventricular leads and the early ST segment are analyzed.
We therefore studied whether T wave alternans can be detected in patients with Brugada syndrome who are at high risk for sudden death and fine‐tuned the method to detect changes in early repolarization in the right precordial chest ECG leads.
METHODS
Patient Selection
For this study, we prospectively included patients with (1) documented incomplete right bundle branch block and ST‐segment elevation in the right precordial leads during administration of slowly dissociating sodium channel blockers; (2) inducible polymorphic ventricular arrhythmias during electrophysiological testing, and (3) a history of syncope or aborted sudden death. All patients who consented to participate in the study underwent measurement of T wave alternans at rest and during exercise. Follow‐up visits at the Department of Cardiology, University Hospital Münster (n = 7), or at other hospitals (n = 2) included regular interrogation of the implanted defibrillator. The control group consisted of seven persons without a history of ventricular arrhythmias or syncope. One control subject underwent radio frequency ablation in the inferior region of the AV node to cure AV nodal reentrant tachycardia. The other patients had no arrhythmia history. None of the control subjects had a history of syncope or sudden death. All patients gave informed consent.
Measurement of T Wave Alternans
T wave alternans (TWA) was assessed on a computerized bicycle ergometer system (Cambridge Heart 2000). The system for recording of T wave alternans has been described in detail previously. 7 , 9 Data were continuously acquired at rest for a period of 3–7 minutes, during exercise with increasing work load (1W increase/5 sec) until the patients reached a heart rate of >115 beats/min, and after cessation of exercise until heart rate had dropped below 90 beats/min.
Data Analysis
The entire recording period was assessed. T wave alternans was measured using two different methods. Primarily, standard criteria for significant T wave alternans (TWA) were used. 7 , 9 In a second analysis, the early ST segment (from 20 ms after the J point) was included in the interval used to compute T wave alternans, and the right precordial leads (V1–V3) were scrutinized for occurrence of TWA (TWA–J20). Presence of TWA was defined by published criteria. 7 , 9 All analyses were performed by a single experienced investigator and confirmed by a second investigator who was unaware of the subject's diagnosis.
RESULTS
All patients showed typical right precordial ST segment elevation, either transiently during a resting ECG or during challenge with ajmaline (1 mg/kg maximal dose). In the Brugada patients, males outnumbered females by 6:3 (66% male). All patients presented with either syncope (n = 6) or aborted sudden arrhythmic death requiring defibrillation (n = 3). One Brugada patient complained of palpitations and was found to have AV nodal reentrant tachycardia during electrophysiological testing. 13 Echocardiography and angiography including right heart catheterization were normal in all patients.
Measurement of T Wave Alternans
The exercise protocol was well tolerated in all patients, and all patients reached a heart rate >115 beats/min. Sustained TWA was not detected in any of the study patients using standard criteria for TWA measurement. Nonsustained TWA was present in one control individual by standard definition, and in none of the Brugada patients (Fig. 1A). When the early ST segment was included in the TWA analysis (TWA–J20), one of the Brugada patients showed nonsustained TWA–J20 (Fig. 1B). In the control group, three individuals were found to have nonsustained TWA–J20. One control subject, a young male with incomplete right bundle branch block but without a history or family history of arrhythmias, syncope, or sudden death, had sustained TWA–J20 (Fig. 1B).
Figure 1.
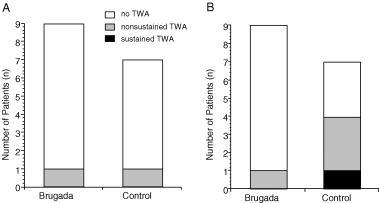
(A). Proportion of individuals with T wave alternans (% TWA, y‐axis) in Brugada patients (Brugada, left column) and control subjects (Control, right column) using standard TWA analysis. (B). Proportion of individuals with TWA when the early ST segment was included in the T wave analysis. White bars indicate no presence of TWA, gray bars indicate presence of nonsustained TWA, and black bars indicate presence of sustained TWA.
Follow‐up
All Brugada syndrome patients received an implantable defibrillator. During a median follow‐up of 34 months, one of the Brugada patients developed a rapid polymorphic ventricular tachycardia that was adequately terminated by the implantable defibrillator (Fig. 2). In this patient, T wave alternans had not been detected, neither at rest nor during exercise.
Figure 2.
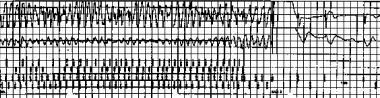
Intracardiac electrograms recorded by the implanted defibrillator in a Brugada patient without detectable T wave alternans who developed a rapid polymorphic ventricular tachycardia during follow‐up. The upper panel shows the intracardiac bipolar electrogram, the middle panel shows the far field electrogram (coil versus can), and the lower panel shows the marker channel. On the right part of the recording, the defibrillator delivers a shock that successfully restores sinus rhythm. Note that the early ST segment is elevated after the ICD shock.
DISCUSSION
In this study of symptomatic Brugada syndrome patients at high risk for arrhythmic death, we found no microvolt T wave alternans at rest or during exercise. Alternans of the early ST segment in the right precordial leads, the portion of the surface ECG showing the characteristic ECG changes associated with Brugada syndrome, was also not detected. T wave alternans does not identify Brugada syndrome patients at high risk for sudden death.
Patient Characteristics
All of the patients studied had an established diagnosis of Brugada syndrome, as demonstrated by typical ECG changes, a history of syncope or aborted sudden cardiac death, and by ventricular arrhythmias during electrophysiologic testing. 1 , 14 One patient received adequate defibrillator shocks terminating polymorphic ventricular tachycardia during the follow‐up period. According to all currently available risk stratification parameters, this patient group therefore represents Brugada syndrome patients at high risk for sudden death. 1 , 2 , 3 , 4
T Wave Alternans in Brugada Syndrome
T wave alternans could be adequately measured in all patients studied. 7 Despite the clinical and electrophysiological indicators for a high risk of sudden cardiac death, there was no sustained T wave alternans in any of the Brugada patients studied. Even when the early ST segment and the right precordial leads were included in the analysis, sustained T wave alternans was not found. Thus, although cardiac repolarization is altered in Brugada syndrome as demonstrated by the reversible ST segment changes, there was no beat‐to‐beat T wave alternans in the early ST segment of symptomatic Brugada syndrome patients. Our data concur with another previously published study on T wave alternans in Brugada syndrome. 15 This study extends that report in two ways: First, this study demonstrates that T wave alternans cannot be detected in Brugada patients at high risk for sudden death. Second, analysis of T wave alternans in the predominant locations of ECG changes in Brugada syndrome, i.e., in the early ST segment and in the right ventricular precordial leads, does also not identify high risk Brugada syndrome patients.
T wave alternans identifies patients with structural heart disease who are at risk for sudden arrhythmic death, including patients with heart failure, 7 patients with inducible ventricular arrhythmias during electrophysiological testing, 16 patients with dilated cardiomyopathy, 11 and patients with hypertrophic obstructive cardiomyopathy. 17 Unlike these diseases, exclusion of structural heart disease is part of the diagnosis of Brugada syndrome. 1 , 3 The syndrome is associated with mutations in the sodium channel SCN5A in some cases, or an altered function of Ito. 2 , 14 , 18 , 19 , 20 Its value in structural heart disease notwithstanding, our data suggest that T wave alternans may not be as valuable in patients with primary electrical disease such as the Brugada syndrome.
CONCLUSIONS
T wave alternans is not an adequate method to identify Brugada syndrome patients who are at high risk for arrhythmic death. T wave alternans might not be an ubiquitous phenomenon in patients at high risk for ventricular arrhythmias and could be related to arrhythmic risk in patients with structural heart disease.
This work was partially supported by grants from the Deutsche Forschungsgemeinschaft (DFG) as part of the Sonderforschungsbereich 556 “heart failure and arrhythmias,” project C4. TW was supported by the interdisciplinary Center for Clinical Research (IZKF, grant # BMBF‐01 KS 9604) of the University of Muenster.
REFERENCES
- 1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 1992;20: 1391–1396. [DOI] [PubMed] [Google Scholar]
- 2. Brugada J, Brugada R, Brugada P. Right bundle‐branch block and ST‐segment elevation in leads V1 through V3: A marker for sudden death in patients without demonstrable structural heart disease. Circulation 1998;97: 457–460. [DOI] [PubMed] [Google Scholar]
- 3. Priori SG, Napolitano C, Gasparini M, et al Clinical and genetic heterogeneity of right bundle branch block and ST‐segment elevation syndrome: A prospective evaluation of 52 families. Circulation 2000;102: 2509–2515. [DOI] [PubMed] [Google Scholar]
- 4. Eckardt L, Kirchhof P, Schulze‐Bahr E, et al Electrophysiologic investigation in Brugada syndrome. Yield of programmed ventricular stimulation at two ventricular sites with up to three premature beats. Eur Heart J 2002;23: 1394. [DOI] [PubMed] [Google Scholar]
- 5. Fujiki A, Usui M, Nagasawa H, et al ST segment elevation in the right precordial leads induced with class IC antiarrhythmic drugs: Insight into the mechanism of Brugada syndrome. J Cardiovasc Electrophysiol 1999;10: 214–218. [DOI] [PubMed] [Google Scholar]
- 6. Viskin S, Fish R, Eldar M, et al Prevalence of the Brugada sign in idiopathic ventricular fibrillation and healthy controls. Heart 2000;84: 31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosenbaum DS, Jackson LE, Smith JM, et al Electrical alternans and vulnerability to ventricular arrhythmias. N Engl J Med 1994;330: 235–241. [DOI] [PubMed] [Google Scholar]
- 8. Pastore JM, Girouard SD, Laurita KR, et al Mechanism Linking T‐Wave Alternans to the Genesis of Cardiac Fibrillation. Circulation 1999;99: 1385–1394. [DOI] [PubMed] [Google Scholar]
- 9. Ikeda T, Sakata T, Takami M, et al Combined assessment of T‐wave alternans and late potentials used to predict arrhythmic events after myocardial infarction. A prospective study. J Am Coll Cardiol 2000;35: 722–730. [DOI] [PubMed] [Google Scholar]
- 10. Hohnloser SH, Klingenheben T, Li YG, et al T wave alternans as a predictor of recurrent ventricular tachyarrhythmias in ICD recipients: Prospective comparison with conventional risk markers. J Cardiovasc Electrophysiol 1998;9: 1258–1268. [DOI] [PubMed] [Google Scholar]
- 11. Adachi K, Ohnishi Y, Shima T, et al Determinant of microvolt‐level T‐wave alternans in patients with dilated cardiomyopathy. J Am Coll Cardiol 1999;34: 374–380. [DOI] [PubMed] [Google Scholar]
- 12. Eckardt L, Kirchhof P, Johna R, et al Transient local changes in right ventricular monophasic action potentials due to ajmaline in a patient with Brugada Syndrome. J Cardiovasc Electrophysiol 1999;10: 1010–1015. [DOI] [PubMed] [Google Scholar]
- 13. Eckardt L, Kirchhof P, Loh P, et al Brugada syndrome and supraventricular tachyarrhythmias: A novel association? J Cardiovasc Electrophysiol 2001;12: 680–685. [DOI] [PubMed] [Google Scholar]
- 14. Brugada R, Brugada J, Antzelevitch C, et al Sodium channel blockers identify risk for sudden death in patients with ST‐segment elevation and right bundle branch block but structurally normal hearts. Circulation 2000;101: 510–515. [DOI] [PubMed] [Google Scholar]
- 15. Ikeda T, Sakurada H, Sakabe K, et al Assessment of noninvasive markers in identifying patients at risk in the Brugada syndrome: Insight into risk stratification. J Am Coll Cardiol 2001;37: 1628–1634. [DOI] [PubMed] [Google Scholar]
- 16. Estes NAr, Michaud G, Zipes DP, et al Electrical alternans during rest and exercise as predictors of vulnerability to ventricular arrhythmias. Am J Cardiol 1997;80: 1314–1318. [DOI] [PubMed] [Google Scholar]
- 17. Momiyama Y, Hartikainen J, Nagayoshi H, et al Exercise‐induced T‐wave alternans as a marker of high risk in patients with hypertrophic cardiomyopathy. Jpn Circ J 1997;61: 650–656. [DOI] [PubMed] [Google Scholar]
- 18. Bezzina C, Veldkamp MW, Van Den Berg MP, et al A single Na(+) channel mutation causing both long‐QT and Brugada syndromes. Circ Res 1999;85: 1206–1213. [DOI] [PubMed] [Google Scholar]
- 19. Rook MB, Alshinawi CB, Groenewegen WA, et al Human SCN5A gene mutations alter cardiac sodium channel kinetics and are associated with the Brugada syndrome. Cardiovasc Res 1999;44: 507–517. [DOI] [PubMed] [Google Scholar]
- 20. Chen Q, Kirsch GE, Zhang D, et al Genetic basis and molecular mechanism for idiopathic ventricular fibrillation. Nature 1998;392: 293–296. [DOI] [PubMed] [Google Scholar]


