Abstract
Brugada syndrome is a channelopathy associated with right bundle branch block and ST segment elevation in the right precordial leads. These electrocardiographic signs may not be apparent most of the time but can be unmasked by certain antiarrhythmic agents. Until now, all of the reports on this syndrome have focused on patients with no significant intraventricular conduction delay at baseline electrograms. In this report, we describe a patient with Brugada syndrome with left bundle branch block at baseline ECG. After intravenous ajmaline, the patient developed right bundle branch block and ST segment elevations in the right precordial leads.
Keywords: Brugada syndrome, left bundle branch block, ajmaline, antiarrhythmic agents
Brugada syndrome is an inherited disorder associated with sudden cardiac death. The hallmark of the disease is the specific electrocardiographic findings of right bundle branch block pattern and ST segment elevation in the right precordial leads. 1 , 2 These electrocardiographic findings are dynamic in nature and are not apparent most of the time. Several methods have been described to unmask these changes. Drug challenge with intravenous class Ia or class Ic drugs has been shown to augment or unmask the right bundle branch block pattern and ST segment elevation in patients with Brugada syndrome. 3 , 4 Right precordial electrograms obtained from higher intercostals space leads might also be helpful in making the Brugada sign apparent; however, the validity of this method has not been verified in large‐scale trials. 5 , 6
All of the reports regarding unmasking of these signs with either technique have focused on patients with no significant intraventricular conduction delays on baseline electrocardiograms, and there are no data about the diagnosis of this syndrome in patients with preexisting left bundle branch block pattern. Here, we describe a patient with Brugada syndrome with preexisting left bundle branch block pattern, who showed typical right bundle branch block pattern and ST segment elevation in the right precordial leads after provocative tests.
CASE REPORT
A 26‐year‐old woman was evaluated for Brugada syndrome because of her strong family history. Her mother, who had syncopal spells, recently had been diagnosed as having Brugada syndrome by typical ECG pattern. She had developed a ventricular flutter that degenerated into ventricular fibrillation during an electrophysiological study and was treated with an implantable cardioverter defibrillator (ICD). The woman's grandfather, great grandfather, two maternal uncles, and one cousin had died unexpectedly. Brugada syndrome was diagnosed in her only living maternal uncle, in her elder brother, and in three of her cousins. The detailed family tree is described elsewhere. 7
The patient denied syncope, presyncope, and dizzy spells. Results of her physical examination were normal. Twelve‐lead ECGs, with the precordial electrograms obtained from both standard locations and from one intercostal space higher than normal, did not show any evidence of Brugada syndrome, but a peculiar left bundle branch block pattern without any ST–T segment changes in precordial leads (Fig. 1A and B). A provocation test with ajmaline (10 mg intravenously, at 2‐minute intervals, until the goal of a total of 1 mg/kg body weight had been reached) was performed, and both standard ECGs and ECGs obtained from one intercostal space above, were obtained. After the administration of ajmaline, the left bundle branch block pattern disappeared and a right bundle branch block pattern with ST segment elevation in the right precordial leads appeared in the ECG obtained from one intercostal space above (Fig. 2). These changes reverted to the same as those in the original ECG 2 hours after administration of ajmaline. The next day, the patient was taken to the electrophysiology laboratory for a comprehensive examination. During programmed stimulation, she developed ventricular fibrillation with two extrastimulus given from the right ventricular apex. The patient was treated with an ICD because of her malignant family history and inducible ventricular fibrillation.
Figure 1.
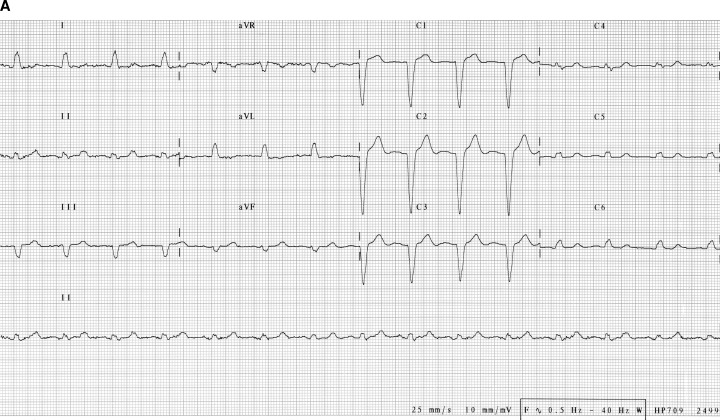
Twelve‐lead ECGs of the patient at the basal state. (A) Precordial electrodes at their standard place. (B) Precordial electrodes at one intercostal space higher than the standard place.
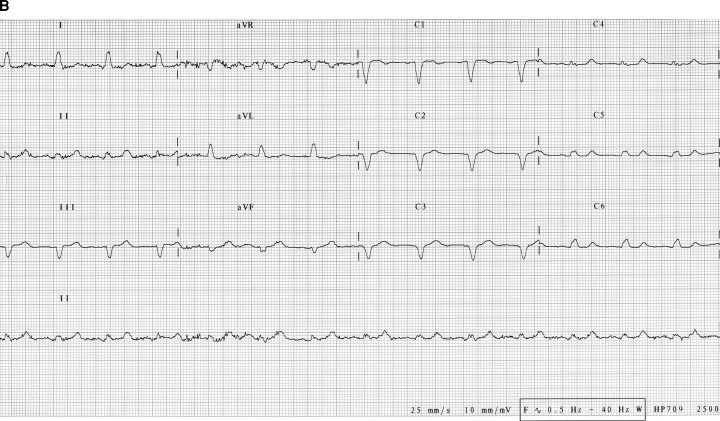
Figure 2.
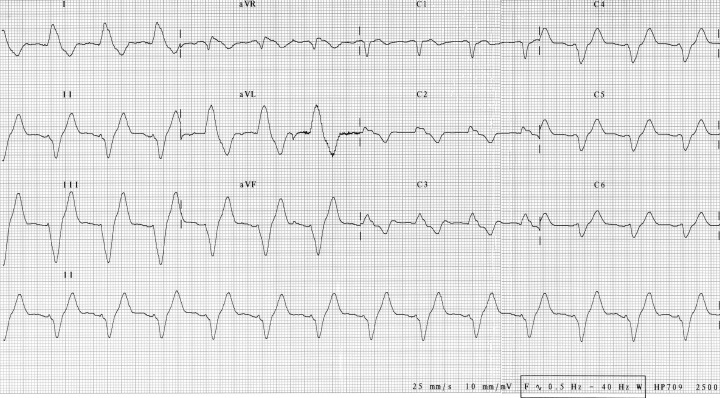
Twelve‐lead ECGs of the patient obtained with the precordial electrodes at one intercostal space higher than the standard place after 45 mg of ajmaline.
DISCUSSION
Left bundle branch block usually results from a conduction block in the left main bundle or in the two fasicles of this bundle. Activation of the left ventricle is delayed, and this causes the typical ECG changes of prolonged QRS duration and loss of septal activation.
Right bundle branch block pattern, with ST segment elevation in right precordial leads unrelated to ischemia, electrolyte abnormalities, or structural heart disease, is the characteristic ECG sign of Brugada syndrome. 1 , 2 However, unlike other causes of right bundle branch block pattern, the right bundle is structurally and functionally intact in this disorder. The loss of the action potential dome in the epicardial, but not endocardial, cells has been shown to cause ST segment elevation in the surface ECG very similar to that observed in Brugada syndrome. 8 Under certain circumstances, the epicardial cells may display a pronounced notch during phase I of the action potential, which results in J point elevation in the surface ECG. 8 It is hypothesized that the accentuation of the notch in the epicardium of the right ventricular outflow tract and the loss of the action potential dome in the epicardium, but not in the endocardium, of the right ventricular outflow tract due to ionic imbalances underlie the typical electrocardiographic features of the Brugada syndrome. 8 , 9 , 10 A delay in right ventricular activation also contributes to these changes. 11 The ionic changes induced by ajmaline in our patient resulted in further prolongation of the QRS and striking changes in the QRS, mimicking right bundle branch block.
No ICD discharges were observed during a 2‐year follow‐up. The ICD indications in asymptomatic patients with Brugada syndrome and the role of EP testing in predicting outcome of patients with this syndrome are controversial. Priori et al. 12 and Eckardt et al. 13 stated that invasive electrophysiology studies do not have any role in risk stratification in patients with Brugada syndrome. Brugada et al. 14 have analyzed the data on 547 patients and concluded that inducible ventricular arrhythmias is an independent predictor of mortality. In a very recent consensus report, 15 ICD implantation in a patient like ours (with this indication) has been considered to be a class IIb indication.
Our case report demonstrates that it is possible to observe typical electrocardiographic features of the Brugada syndrome even in patients with left bundle branch block pattern. However, it should be noted that these electrocardiographic features depend both on the magnitude and the duration of the ionic changes in this particular situation and it may not be possible to observe these features in all patients with left bundle branch block.
None of the authors have associations that might pose a conflict of interest. No financial support from any organization was used.
REFERENCES
- 1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 1992;20: 1391–1396. [DOI] [PubMed] [Google Scholar]
- 2. Brugada J, Brugada R, Brugada P. Right bundle‐branch block and ST‐segment elevation in leads V1 through V3: A marker for sudden death in patients without demonstrable structural heart disease. Circulation 1998;97: 457–460. [DOI] [PubMed] [Google Scholar]
- 3. Brugada R, Brugada J, Antzelevitch C, et al Sodium channel blockers identify risk for sudden death in patients with ST‐segment elevation and right bundle branch block but structurally normal hearts. Circulation 2000;101: 510–515. [DOI] [PubMed] [Google Scholar]
- 4. Miyazaki T, Mitamura H, Miyoshi S, et al Autonomic and antiarrhythmic drug modulation of ST segment elevation in patients with Brugada syndrome. J Am Coll Cardiol 1996;27: 1061–1070. [DOI] [PubMed] [Google Scholar]
- 5. Takagi M, Toda I, Takeuchi K, et al Utility of right precordial leads at higher intercostal space positions to diagnose Brugada syndrome. Pacing Clin Electrophysiol 2002;25: 241–242. [DOI] [PubMed] [Google Scholar]
- 6. Hisamatsu K, Morita H, Fukushima Kusano K, et al Evaluation of the usefulness of recording the ECG in the 3rd intercostal space and prevalence of Brugada‐type ECG in accordance with recently established electrocardiographic criteria. Circ J 2004;68: 135–138. [DOI] [PubMed] [Google Scholar]
- 7. Altunkeser B, Atar İ, Özdemir K, et al Brugada syndrome: Two cases and description of their family. Turk J Arrhythmia Pacing Electrophysiol 2004;2: 119–125. [Google Scholar]
- 8. Yan GX, Antzelevitch C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST‐segment elevation. Circulation 1999;100: 1660–1666. [DOI] [PubMed] [Google Scholar]
- 9. Gussak I, Antzelevitch C, Bjerregaard P, et al The Brugada syndrome: Clinical, electrophysiologic and genetic aspects. J Am Coll Cardiol 1999;33: 5–15. [DOI] [PubMed] [Google Scholar]
- 10. Kurita T, Shimizu W, Inagaki M, et al The electrophysiologic mechanism of ST‐segment elevation in Brugada syndrome. J Am Coll Cardiol 2002;40: 330–334. [DOI] [PubMed] [Google Scholar]
- 11. Tukkie R, Sogaard P, Vleugels J, et al Delay in right ventricular activation contributes to Brugada syndrome. Circulation 2004;109: 1272–1277. [DOI] [PubMed] [Google Scholar]
- 12. Priori SG, Napolitano C, Gasparini M, et al Natural history of Brugada syndrome: Insights for risk stratification and management. Circulation 2002;105: 1342–1347. [DOI] [PubMed] [Google Scholar]
- 13. Eckardt L, Probst V, Smits JP, et al Long‐term prognosis of individuals with right precordial ST‐segment‐elevation Brugada syndrome. Circulation 2005;111: 257–263. [DOI] [PubMed] [Google Scholar]
- 14. Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation 2003;108: 3092–3096. [DOI] [PubMed] [Google Scholar]
- 15. Antzelevitch C, Brugada P, Borggrefe M, et al Brugada syndrome: Report of the second consensus conference: Endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 2005;111: 659–670. [DOI] [PubMed] [Google Scholar]


