Abstract
Purpose: Vasovagal syncope is a common and challenging problem that may result in injury and causes susbstantial anxiety among patients and their relatives. However, treatment of vasovagal syncope with standard pharmacologic approaches is not satisfactory. The aim of this study is to investigate the effect of amitriptyline, a tricyclic antidepressant drug, by using its anticholinergic effects in preventing syncopal episodes in patients with vasovagal syncope.
Methods: In this study, 74 patients (mean age 24 ± 1.9 years, 26 male) with a history of recurrent syncope and baseline positive head‐up tilt table test (syncope or presyncope) were included. Oral amitriptyline treatment was given to all patients, with a starting dose of 10 mg once a day. Head‐up tilt table test was performed in all patients 4 weeks after the treatment started. Patients were followed up clinically for 6 months.
Results: After 4 weeks, during head‐up tilt table test in 69 patients (93%), syncope or presyncope was not seen and test was assumed as negative. At the end of the 6th month, 67 patients (91%) were free of symptoms. Only two patients (0.3%) did not tolerate amitriptyline due to side effects.
Conclusions: Oral amitriptyline can be used in the prevention of recurrent episodes of vasovagal syncope safely. However, randomized controlled studies are essential to assess the real effectiveness of this therapy.
Keywords: vasovagal syncope, amitriptyline, recurrent syncope, head‐up tilt table test
Syncope, defined as the transient loss of consciousness, is a common and challenging condition and emerging as a significant and potentially disabling problem for many patients. Syncope may occur as a result of variety of causes including cardiac, neurologic, metabolic, and psychiatric diseases. 1 The most common cause of syncope is vasovagal syncope. 2 Although the cause is benign, if untreated, recurrent syncope may result in injury and cause anxiety among patients, by decreasing quality of life similar to chronic debilitating diseases such as rheumatoid arthritis and chronic lower‐back pain. 3
Vasovagal syncopes are episodic, which are believed to be hypersensitive autonomic system responses overreacting to normal stimuli such as prolonged upright posture. 4 Although the exact pathophysiological mechanisms causing vasovagal syncope remain unclear, several pharmacological agents, such as beta blockers, alpha‐receptor agonists, fludrohydrocortisone, and serotonin reuptake inhibitors, have been used for the treatment by modifying the afferent or efferent limbs of the abnormal reflex. 5 However, there is no widely accepted treatment for this common clinical problem. Most of the randomized, placebo‐controlled clinical studies with drugs for the management of vasovagal syncope to date show no differences between the placebo and treatment groups. 5 An alternative therapeutic target can be hypervagotonia in this condition. This is mostly due to the inactivation of high‐pressure baroreceptors and paradoxical activation of low‐pressure cardiopulmonary mechanoreceptors leading to parasympathetic stimulation during central volume unloading. 6 Amitriptyline is a tricyclic antidepressant drug with its prominent anticholinergic side effects. By the help of this anticholinergic effects, this drug could be used in the treatment of vasovagal syncope. The purpose of the study was to evaluate the efficacy and safety of amitriptyline in the prevention of recurrent syncope in patients with a history of tilt table positive test results and recurrent syncopes, with a follow up tilt table test.
METHODS
Study Population
A consecutive series of 74 patients with a history of recurrent syncopal episodes and a baseline positive head‐up tilt table test response applying to Cardiology Department were prospectively studied. Each patient served as her or his own control through the baseline study. The study population included 26 males and 48 females with a mean age 24 ± 1.9 years. All patients had a history of recurrent syncopal episodes (at least three episodes in the last 2 years) and inducible syncope or presyncope on the baseline head‐up tilt table study. The diagnosis of vasovagal syncope was given, in addition to a positive tilt table response, with the exclusion of all other possible causes. A systematic diagnostic approach, including careful history taking, physical examination with full neurological evaluation, routine laboratory tests, supine and orthostatic blood pressure measurements, 12‐lead electrocardiography (ECG), bilateral carotid sinus massage, twenty‐four‐hour ambulatory ECG recording, and two‐dimensional echocardiography, was done to all patients. Further diagnostic investigations, such as electrophysiological study, electroencephalogram, and neurological imaging tests, were performed only if clinically indicated. The study protocol was approved by the local ethics committee. All patients were informed about the study and gave their written consent before enrolment.
Study Protocol
Patients underwent head‐up tilt table test in the morning, after 12‐hour fasting period. Tilt table testing protocol started with the patient placed in the supine position at baseline. An intravenous access and continuous ECG monitoring was established. Blood pressure and heart rate measurements were recorded at 5‐minute intervals or when patients were symptomatic. Tilt table was performed at 60° angles with foot support up to 45 minutes or until symptomatic. Syncope was defined when a sudden transient loss of consciousness, with inability to maintain postural tone, and with spontaneous recovery developed. When there were preliminary signs and symptoms of imminent syncope, such as nausea, diaphoresis, lightheadedness, blurred vision, and severe weakness with difficulty in maintaining postural tone, presyncope was defined. Tilt table testing was considered positive if the syncope or presyncope were noted, along with an abrupt drop in blood pressure, heart rate, or both. 7 The positive response was defined as cardioinhibitory when a marked bradycardia (<40 beats per minute for >10 seconds) or prolonged asystole (>3 seconds) developed with syncope. 8 Vasodepressor or mixed response was defined when isolated hypotension or hypotension associated with only mild bradycardia (>40 bpm) or brief asystole (<3 seconds) occurred. 8
Amitriptyline (Laroxyl, Roche) was given to all patients for 4 weeks, followed by repetition of the tilt table testing protocol. The drug was started at 10 mg per day and increased up to 20 mg per day, when necessary. Six‐month follow‐up was performed for all patients, using clinical evaluation, in which duration of therapy, recurrence of symptoms, side effects related to amitriptyline, and current dosage were assessed.
Statistical Analysis
All continuous data were expressed as mean ± SD and nominal values were expressed as rates (%). The unpaired 2‐tailed Student's t‐test was used for specific continuous variables and Fisher's exact test was used for categorical variables. A P value less than 0.05 was considered significant.
RESULTS
The baseline characteristics of patients were given in Table 1. Inducible syncope was developed in all patients with clinical symptoms of syncope and presyncope during baseline head‐up tilt table test at 21.18 ± 3.4 minutes. Amitriptyline treatment was effective in preventing reinduction of syncope as evaluated by the repeat (4 weeks later) tilt table testing in 69 of 74 patients (93%, the responders). The other patients (the nonresponders) who developed syncope during repeat tilt table study had inducible syncope at 18.4 ± 2.5 minutes at the baseline tilt study. When compared with initial baseline tilt table study, in nonresponders the onset of inducible syncope was delayed significantly to 43.80 ± 2.1 minutes (P < 0.05). When the effects of pre‐ and postamitriptyline treatment on hemodynamic response to tilt table testing were compared, in responders the minimal heart rate seen during the test increased from 50.2 ± 9.5 beats per minute to 77.1 ± 6.8 beats per minute at repeat tilt table testing (4 weeks later) (Fig. 1). The minimal systolic blood pressure during baseline tilt table testing in responders was recorded to significantly increase from 62.7 ± 9.7 mmHg to 99.2 ± 8.9 mmHg after treatment with amitriptyline (P < 0.05). After treatment with amitriptyline, hemodynamic responses to tilt testing were not changed significantly in nonresponders. Only six patients out of 69 responders exhibited a cardioinhibitory response, while other responder patients exhibited a vasodepressor form or mixed form of syncope. Two patients in nonresponder group exhibited mixed form and vasodepressor response was present in three nonresponder patients.
Table 1.
Baseline Characteristics of the Patients
| The Responders (n = 69) | The Nonresponders (n = 5) | |
|---|---|---|
| Mean age ± SD (years) | 24 ± 1.9 | 23.8 ± 1 |
| Male | 24 (35%) | 2 (40%) |
| No. of syncopes in last 2 years | 3 (3–8) | 4 (3–4) |
| (median; min, max) | ||
| Baseline minimal systolic blood | 62.7 ± 9.7 | 67 ± 2.7 |
| pressure during test (mmHg) | ||
| Baseline minimal heart | 50.2 ± 9.5 | 44.4 ± 9.5 |
| rate during test (bpm) | ||
| Response to baseline tilt test | ||
| Vasodepressor or mixed | 63 | 5 |
| Cardioinhibitory | 6 | 0 |
Figure 1.
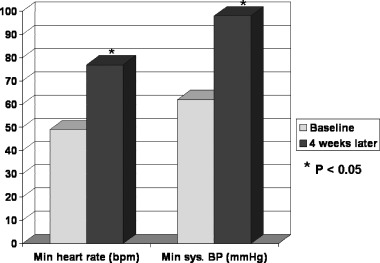
Effect of amitriptyline treatment on minimal heart rate and minimal systolic blood pressure during head‐up tilt table test in responders patients. bpm = beats per minute.
All 74 patients were examined clinically after 6 months. Sixty‐seven patients (91%) were free of symptoms (syncope or presyncope). Three patients from responder group and four from nonresponders had symptoms. One patient stopped using the study medication due to severe dryness of mouth, and one patient due to sleep disorder. Other side effects reported during treatment were dryness of mouth (41 patients), mild headache (five patients), and weakness (five patients).
DISCUSSION
The results of this study have pointed out that treatment with amitriptyline, a tricyclic antidepressant drug, was found to be effective in preventing recurrent syncopal episodes in patients with vasovagal syncope. Moreover, during head‐up tilt table testing, the study drug significantly prolonged the onset of syncope occurrence in nonresponders. All patients but two who participated in the study tolerated the drug. No serious adverse effects, which were related to drug, was noted.
Vasovagal syncope is one of the most common types of the syncope. 9 The pathophysiologic mechanisms of this type of syncope is complex and not fully understood. In normal individuals, reflex activation of sympathetic system and parasympathetic withdrawal cause peripheral vasoconstriction and an increase in heart rate in response to venous pooling due to upright posture. 10 In patients with vasovagal syncope, adaptive neurocardiovascular responses to upright posture are not adequate for a longer time period. 10 Although its overall prognosis is good, sudden loss of consciousness may lead to severe trauma, and may increase the risk of ischemia or bradycardia‐mediated ventricular arrhythmias, may restrict employment, education, and social interactions, and decrease the quality of life especially in patients with frequent episodes. 11
Multiple drugs and strategies have been tried in the management of vasavagal syncope, such as intravascular volume expansion with fluids, salt, and fludrocortisone, beta blockers, serotonin reuptake inhibitors, disopyramide, alpha agonists, and theophylline. 5 Di Girolamo et al. 12 studied the effects of paroxetine, a selective serotonin reuptake inhibitor, on preventing syncopal episodes in patients with refractory vasovagal syncope. Paroxetine was found to be effective in decreasing both the positive response rates to tilt test and spontaneous syncope in this study. Midodrine, a peripheral α‐receptor agonist, was found to improve orthostatic tolerance during tilt table test, and decrease syncope recurrence in relatively small studies, but its use is limited due to serious side effects such as systolic hypertension. 13 , 14 , 15 The studies with beta blockers have mixed results; however, recently Sheldon et al. 16 demonstrated that metoprolol treatment was not effective in preventing syncope recurrence in patients with vasovagal syncope, regardless of age. An alternative therapeutic strategy to this complex clinical condition has been focused on the increased vagal activity seen in these patients. 17 In patients with vasovagal syncope, the cardioinhibitory (vagal) receptors are triggered, resulting in vasodilatation, hypotension, and bradycardia. 18 Baharav et al. 19 studied spectral analysis of heart rate fluctuations to investigate the role of the autonomic nervous system in patients with vasovagal syncope. They demonstrated the role of autonomic system, as reduced sympathetic reserve and increased parasympathetic activity by low and high frequency fluctuations, in patients with recurrent syncopal episodes. Bradycardia, and in some patients asystole, due to hypervagotonia, with subsequent negative chronotropic response results in symptoms. 3 The studies with anticholinergic agents such as atropine and transdernal scopolamine have shown reversal of bradycardias in patients with vasovagal syncope. 20 Disopyramide, a class 1A antiarrhythmic drug, has been shown to prevent tilt table‐induced syncope through combination of decreasing left ventricular contraction (negative inotrophic property) and the exertion of vagolytic effect (anticholinergic effect), preventing bradycardia/asystole. 21 However, this drug has serious side effects, causing proarrhythmia, which leaves clinicians reluctant to use it as a fist line treatment for vasovagal syncope. Yu et al. 17 studied the effects of propantheline bromide, another anticholinergic agent, in patients with neurocardiogenic syncope. They studied 16 patients with positive tilt‐table testing. After propantheline bromide treatment, only three out of 16 patients developed inducible presyncope or syncope on repeat (1 week later) tilt‐table testing, while 81% of patients did not have inducible syncope during the test. In our study, 93% of 74 patients did not have syncope or presyncope during repeat tilt table testing after 4 weeks of amitriptyline therapy. After 6 months of follow up, 67 patients (91%) were free of symptoms.
Amitriptyline, a tricyclic antidepressant, has been used for depressive illnesses. It has anticholinergic effects (dry mouth, blurred vision, urinary retention, constipation, palpitations, tachycardia). One of the mechanisms of this drug for the prevention of vasovagal syncope could be due to the exertion of a vagolytic effect (anticholinergic effect), preventing the bradycardic or asystolic component of the syncopal episode. Increased fluid and salt intake leading to volume expansion may prevent syncopal episodes. 2 Plasma volume expansion improves orthostatic tolerance. Lu et al. 22 demonstrated that water drinking had improved orthostatic tolerance in patients with postural tachycardia syndrome. Other side effects such as edema, increased appetite, and weight gain may also work in reducing the number of episodes. Further studies are needed for the clarification of the mechanism of action of this drug for the prevention of vasovagal syncope.
Most of the patients with vasovagal syncope may experience dramatic resolution of symptoms after positive test result. 23 Relatively low number of patients with recurrences could be due to placebo effect of the treatment.
The head‐up tilt table test is an important tool for the diagnosis of vasavagal syncope, of which sensitivity ranges between 67% and 83%, and the specificity between 75% and 100%. 24 Moreover, the reproducibility of the tilt table is low. 25 The response to the baseline test does not predict syncope or presyncope recurrence during repeat test. 26 The reproducibility of the tilt table test is between 85% and 95% for a baseline negative test, but lower for a positive test (30–90%). 2 This variability in the reproducibility raises doubts regarding the utility of tilt table test. Therefore, symptom recurrence becomes far more important outcome measure. In our study, only 7% of patients had positive test results during repeat test. More importantly, most of the patients (91%) did not have any symptoms clinically during 6 months of follow up.
As a conclusion, based on the results of our study, amitriptyline therapy may safely and effectively be used in the treatment of vasovagal syncope. However, more studies are needed to assess the effectiveness of this therapy.
REFERENCES
- 1. Boehm KE, Morris EJ, Kip KT, et al Diagnosis and management of neurally mediated syncope and related conditions in adolescents. J Adolesc Health 2001;28:2–9. [DOI] [PubMed] [Google Scholar]
- 2. Grubb BP. Clinical practice. Neurocardiogenic syncope. N Engl J Med 2005;352:1004–1010. [DOI] [PubMed] [Google Scholar]
- 3. Sealey B, Lui K. Diagnosis and management of vasovagal syncope and dysautonomia. AACN Clin Issues 2004;15:462–477. [DOI] [PubMed] [Google Scholar]
- 4. Grubb BP, Karas B. Diagnosis and management of neurocardiogenic syncope. Curr Opin Cardiol 1998;13:29–35. [DOI] [PubMed] [Google Scholar]
- 5. Chen‐Scarabelli C, Scarabelli TM. Neurocardiogenic syncope. BMJ 2004;329:336–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thomson HL, Wright K, Frenneaux M. Baroreflex sensitivity in patients with vasovagal syncope. Circulation 1997;95:395–400. [DOI] [PubMed] [Google Scholar]
- 7. Brignole M, Alboni P, Benditt D, et al Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001;22:1256–1306. [DOI] [PubMed] [Google Scholar]
- 8. Raviele A, Brignole M, Sutton R, et al Effect of etilefrine in preventing syncopal recurrence in patients with vasovagal syncope: A double‐blind, randomized, placebo‐controlled trial. The Vasovagal Syncope International Study. Circulation 1999;99:1452–1457. [DOI] [PubMed] [Google Scholar]
- 9. Nair N, Padder FA, Kantharia BK. Pathophysiology and management of neurocardiogenic syncope. Am J Manag Care 2003;9:327–334; quiz 335–336. [PubMed] [Google Scholar]
- 10. Hainsworth R. Pathophysiology of syncope. Clin Auton Res 2004;14(Suppl 1):18–24. [DOI] [PubMed] [Google Scholar]
- 11. Folino AF, Buja GF, Martini B, et al Prolonged cardiac arrest and complete AV block during upright tilt test in young patients with syncope of unknown origin—Prognostic and therapeutic implications. Eur Heart J 1992;13:1416–1421. [DOI] [PubMed] [Google Scholar]
- 12. Di Girolamo E, Di Iorio C, Sabatini P, et al Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: A randomized, double‐blind, placebo‐controlled study. J Am Coll Cardiol 1999;33:1227–1230. [DOI] [PubMed] [Google Scholar]
- 13. Mitro P, Trejbal D, Rybar AR. Midodrine hydrochloride in the treatment of vasovagal syncope. Pacing Clin Electrophysiol 1999;22:1620–1624. [DOI] [PubMed] [Google Scholar]
- 14. Perez‐Lugones A, Schweikert R, Pavia S, et al Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: A randomized control study. J Cardiovasc Electrophysiol 2001;12:935–938. [DOI] [PubMed] [Google Scholar]
- 15. Kaufmann H, Saadia D, Voustianiouk A. Midodrine in neurally mediated syncope: A double‐blind, randomized, crossover study. Ann Neurol 2002;52:342–345. [DOI] [PubMed] [Google Scholar]
- 16. Sheldon R, Connolly S, Rose S, et al Prevention of Syncope Trial (POST): A randomized, placebo‐controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006;113:1164–1170. [DOI] [PubMed] [Google Scholar]
- 17. Yu JC, Sung RJ. Clinical efficacy of propantheline bromide in neurocardiogenic syncope: Pharmacodynamic implications. Cardiovasc Drugs Ther 1997;10:687–692. [DOI] [PubMed] [Google Scholar]
- 18. Kosinski D, Grubb BP, Temesy‐Armos P. Pathophysiological aspects of neurocardiogenic syncope: Current concepts and new perspectives. Pacing Clin Electrophysiol 1995;18:716–724. [DOI] [PubMed] [Google Scholar]
- 19. Baharav A, Mimouni M, Lehrman‐Sagie T, et al Spectral analysis of heart rate in vasovagal syncope: The autonomic nervous system in vasovagal syncope. Clin Auton Res 1993;3:261–269. [DOI] [PubMed] [Google Scholar]
- 20. White CM, Tsikouris JP. A review of pathophysiology and therapy of patients with vasovagal syncope. Pharmacotherapy 2000;20:158–165. [DOI] [PubMed] [Google Scholar]
- 21. Milstein S, Buetikofer J, Dunnigan A, et al Usefulness of disopyramide for prevention of upright tilt‐induced hypotension‐bradycardia. Am J Cardiol 1990;65:1339–1344. [DOI] [PubMed] [Google Scholar]
- 22. Lu CC, Diedrich A, Tung CS, et al Water ingestion as prophylaxis against syncope. Circulation 2003;108:2660–2665. [DOI] [PubMed] [Google Scholar]
- 23. Parry SW, Kenny RA. The management of vasovagal syncope. QJM 1999;92:697–705. [DOI] [PubMed] [Google Scholar]
- 24. Kapoor WN, Smith MA, Miller NL. Upright tilt testing in evaluating syncope: A comprehensive literature review. Am J Med 1994;97:78–88. [DOI] [PubMed] [Google Scholar]
- 25. Benditt DG, Van Dijk JG, Sutton R, et al Syncope. Curr Probl Cardiol 2004;29:152–229. [DOI] [PubMed] [Google Scholar]
- 26. Moya A, Permanyer‐Miralda G, Sagrista‐Sauleda J, et al Limitations of head‐up tilt test for evaluating the efficacy of therapeutic interventions in patients with vasovagal syncope: Results of a controlled study of etilefrine versus placebo. J Am Coll Cardiol 1995;25:65–69. [DOI] [PubMed] [Google Scholar]


