Abstract
To address cancer as a multifaceted adaptive system, the increasing momentum for cross-disciplinary connectivity between cancer biologists, physical scientists, mathematicians, chemists, biomedical engineers, computer scientists, clinicians, and advocates is fueling the emergence of new scientific frontiers, principles, and opportunities within physical sciences and oncology. In parallel to highlighting the advances, challenges, and acceptance of advocates as credible contributors, we offer recommendations for addressing real world hurdles in advancing equitable partnerships among advocacy stakeholders.
In 2009, researchers affiliated with the National Cancer Institute (NCI) Physical Sciences-Oncology Centers (PS-OC; https://physics.cancer.gov/), an interdisciplinary hub for work supporting physical sciences and oncology theories and experimental techniques applied to complex cancer problems, predicted that the benefits of the current convergence ‘revolution’ in biomedicine would be enriched and enhanced by vigorous and diverse public and/or advocacy support. Collaborating to spur innovation, researchers felt optimistic that merging the seemingly incompatible qualities of evidentiary data and improvisational techniques with advocacy would help propel them toward accelerating the pace of progress against cancer. As dedicated and passionate knowledge brokers, advocate ‘citizen scientists’ could bring real-time heterogeneous patient experiences and concerns into research practices, facilitate and bridge academia–industry collaborations, promote data transparency and reproducibility, and embrace data sharing as an open exchange of ideas [1].
Informing Science and Policy with an Action-Based Advocacy Framework
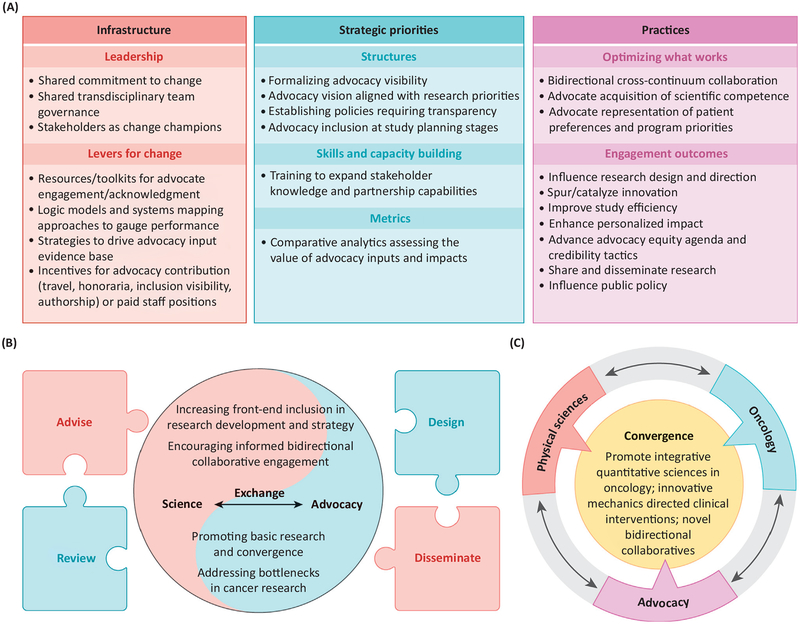
As new frontiers in oncology evolve, advocates have an important role to play as cultural brokers and agents of change. Forwarding the imperatives (think boldly and creatively, question the status quo, and consciously break down the silos that impair collaboration) nullifies along-held paradigm that advocates are passive recipients in convergent science settings. Together, researchers and advocates are cocreating system change interventions for revamping convergent research processes (Figure 1A). By proactively participating in four areas: research and programmatic support, education and outreach, policy and strategy, and representation and advisory, advocates adhere to key NCI Office of Advocacy Relations (OAR; https://www.cancer.gov/about-nci/organization/oar) recommendations for holistic engagement (Figure 1B).
Figure 1. (A) Science Advocacy Engagement.
Together, researchers and advocates are cocreating system change interventions for revamping convergent research processes. Engaging with researchers, advocates codevelop guiding conceptual frameworks, educational strategies, training curriculum, toolkits, and instructional materials to accelerate innovation and advance science; envision a transdisciplinary setting where everyone has access to high quality science and advocacy interface opportunities; and match advocate expertise to research needs, including setting priorities/plans for early stage research and developing best engagement practice and metrics guidelines. (B) Mapping Science: Advocacy Exchange. Aligned from the start as vital catalysts of transdisciplinary innovation, the conceptual puzzle illustrates multimethod science advocacy engagement strategies. Advocates proactively participate in four areas: (i) research and programmatic support, (ii) education and outreach, (iii) policy and strategy, and (iv) representation and advisory. They apply four core principles that forge synergy with the emerging discipline of implementation science and the National Cancer Institute advocacy research working group recommendations (https://deainfo.nci.nih.gov/advisory/ncra/ARWG-recom.pdf): strategic innovation, collaborative execution, evidence based/inspirational decision-making, and ethical codes of conduct. (C) Vision and Convergence. Model depicting the intersections of physical sciences, biomarker discovery, emerging therapeutics, and advocacy that constitute a paradigm shift for biomedical research, one in which resources will be devoted to creating a vision supporting the value, impact, and benefit of advocate engagement, specifically in prediscovery early settings. Model format was adapted from [13].
In an environment of shared transdisciplinary team governance, advocates work closely with investigators in the planning stages of their projects. Often, experienced advocates ‘mentor’ young investigators by providing insight into clinical aspects of cancer research, treatment, and the grant submission process. Reviewing proposals for scientific merit, innovation, and study feasibility, advocates pinpoint areas of research neglect, disparities and inequities in research, as well as problems and alternative strategies to identify a target or modalities of potential therapeutic efficacy. When informing the design, conduct, and interpretation of data while advancing their own preferences and goals within convergent science, advocates focus on six ‘credibility’ tactics: (i) the representation of patient priorities; (ii) the potential benefits of bidirectional collaboration; (iii) the acquisition of scientific competence; (iv) the infusion of nonscientific judgments and language within science advocacy exchange; (v) the impact of communicating and disseminating findings to patient, clinical, and research communities at local, national, and international levels; and (vi) the need to promote advocacy visibility (Box 1).
Box 1. Game Changers: Advocates for Convergent Science.
Mechanobiology in Tune with Advocacy
What happens when you mix the foundations of mechanics with advocacy? In a shared quest for exciting scientific frontiers beyond genomics, Bay Area physical scientists, clinical researchers, and advocates worked in dynamic symbiotic relationships to accelerate innovative and needed paradigm shifts in the mechanobiology of tumor progression in breast cancer research. For example, University of California, San Francisco (UCSF) Breast Oncology Program (http://cancer.ucsf.edu/research/programs/breast/) and NCI advocates shared the convergence goals of researchers and clinicians in determining how tumor microenvironments regulate cancer initiation and progression through interactions between various cell types and tissue architecture (e.g., cancer-initiating cells, activated stromal cells, and acellular components of the extracellular matrix) [1]. Advocates offered insights regarding innovative mechanics-directed clinical interventions that emphasize the importance of the physical organization of cell-to-cell contacts, tissue architecture, tumor microenvironments, mechanical properties in response to therapy, and drug repurposing of a well-tolerated therapy to empower the immune system to eradicate breast tumors and produce a sustained remission that might be construed as a cure [12].
There is emerging evidence that advocacy insights and input may have implications for patient outcomes. For example, alongside researchers, advocates creatively grapple with the challenges of noting progress as they balance uncertainties surrounding the promise of novel targeted and immune-therapeutics benefits. Moreover, in discerning the optimal integration of convergent science and evolving therapeutic data in physical sciences and oncology, advocates embrace issues such as genomics, proteomics, mechanobiology, the microenvironment, breast density, and nanotechnology (Figure 1C).
Yet, although we suggest that advocate intersections with biomedicine have broad implications for our understanding of the cultural authority of science and the boundaries between science and society, there is a distinction to be drawn, namely, that behind the success stories of advocacy’s true prospects and potential, looms uncertainties. Unfortunately, despite the hopes of advocacy in support of convergent science, the nuances of advocacy engagements and influences within preclinical settings often remain elusive. In contrast to drug development and translational settings, where the science of advocacy input and the metrics of engagement is rapidly evolving [2–10], it is unclear how various advocate convergent science involvements impact research processes or lead to improved discoveries. For example, it is difficult to evaluate the effectiveness of practices since there is a paucity of empirical evidence documenting how niche-agnostic volunteer advocates, with unique personal experiences, training, and expertise, serve as critical mentors and representatives of programs in the physical sciences and oncology.
To better understand and fully address the complexities of intersecting physical sciences and oncology advocacy engagement, we propose broad recommendations that define the conditions needed to transform practices.
First, the next generation of convergent science researchers, practitioners, and advocates must address five noteworthy challenges: (i) the dearth of best practices for engagement and the lack of infrastructure resources and time needed to devote to advocacy programs, (ii) cultural inertia and internal resistance to change, (iii) mismatched expectations and misaligned goals between researchers and advocates, (iv) inconsistencies in advocacy training, and (v) lack of buy-in regarding advocacy credibility as legitimate partners. Stakeholders then and now express serious concerns about the value of advocacy contribution. How can advocates possibly understand the complexities of the science? What expertise do they offer? Why should they be taken seriously?
Second, critical questions and thorny issues need to be considered in order to improve the evidence base for the science of advocacy input. For example, how should we embrace the diversity in advocate expertise and viewpoints? How can advocates acquire and strengthen their knowledge base, skills, and tools? Should we encourage specialized or formal training requirements prior to research engagement? Should the level of training depend upon the type of engagement and the anticipated role of the advocate in a project? Moreover, to what extent does advocacy engagement in specific grants and projects result in improved chances of funding success, impactful publications, and clinical translation?
Third, multilevel approaches are needed to tackle longstanding concerns regarding advocacy recognition, respect, and equity across the physical sciences and oncology research continuum. For example, although advocates appreciate the infrastructure support and incentives of advocacy contribution offered in the form of honoraria and travel sponsorship to attend professional meetings, and although they are honored by the acknowledgment offered by well-intentioned researchers who in oral presentations and publications thank advocates for their advice, they also are keenly aware that too few researchers embrace opportunities for operationalizing advocacy input or promoting advocacy authorship inclusion. In our view, the rules of engagement and the rationale for which advocacy contributions matter most should be agreed upon by the research and advocate community in advance of their commitment to work together. Fortunately, to mitigate advocate concerns regarding their indeterminate partnership role, various governmental agencies and nonprofits are currently developing guidelines and standards to clarify the metrics of advocacy engagement and contribution across research, development, translational, and clinical settings ([11] https://ww5.komen.org/uploadedFiles/_Komen/Content/Get_Involved/Participate/Become_an_Advocate/Guide-Documents-for-Researchers-and-Advocates-0717.pdf).
Fourth, moving forward, to realize advocacy’s potential in catalyzing innovation within physical sciences and oncology, rigorous monitoring and assessment is needed to leverage the scalability, reproducibility, accountability, and significance of engagements. This will require developing practical methods and recommendations for tracking performance; assessing the scientific, institutional, cultural, and improvisational impacts of best practices; studying infrastructures and levers for change; incorporating bidirectional priorities into strategic initiatives; examining funding models; enhancing advocacy visibility and contribution within convergent cancer settings; revealing the differences across advocacy and research cultures that shape decisions; quantifying the impact of engagement in research practices through meeting/advisory participation and presentations; and developing an action plan for next steps needed to plan for successful productive engagements.
Shifting Paradigms to Propel Convergent Innovation
Although the multidisciplinary field of physical sciences and oncology has evolved into one where advocates are poised to propel convergent innovation, formalizing an advocacy presence requires a paradigm shift to the one that is already evolving. In 2009, the NCI included a lead volunteer advocate representative in the administration of the PS-OC. With this stunning gesture of support, the PS-OC sent the unambiguous message that innovation springs from many sources, not least from advocacy circles. Yet, despite vigorous efforts to capture and integrate this potentially transformative resource into decision-making, progress has been uneven. For example, not every center and project has any sort of patient involvement, despite this program existing since 2009. Also, other technology-focused NCI programs have little, if any, advocate involvement. This needs to change. The Physical Sciences-Oncology Network (PS-ON) is setting an example of how advocates can benefit a physical sciences program, which hopefully will be translated to other programs throughout the NCI’s portfolio.
To scale up efforts, in the spring of 2016, leadership from the reconfigured NCI PS-ON and OAR defined new expectations to increase the visibility of advocacy contributions and ease the potential pain points of collaboration. For example, they initiated an advocacy dialogue event: in the spring of 2017, they posted advocacy articles, poster presentations, and toolkits to their online portal (see synapse; https://www.synapse.org/#!Synapse:syn7080714/wiki/) and in the fall of 2017, the leadership invited four advocates to give oral presentations at the Annual PS-ON Investigator’s Meeting. The PS-ON has also included advocate representation on the Steering Committee and the Planning Committee for the 2018 Annual Meeting.
Additionally, within the last year, the PS-ON and OAR jointly convened an ongoing Advocate Working Group to discuss, coordinate, and leverage advocate strategic priorities. Focusing on the approaches utilized across the 18 member NCI centers and regional academic centers, advocates share opportunities and challenges associated with efforts to expand the evolving landscape of advocate engagement; promote cross-sector collaboration; integrate advocate perspectives at earlier stages of research; cultivate professional development opportunities for early stage investigators and advocates; identify common issues that could derail potentially beneficial collaborations; develop and implement new trainings, tools, and resources; communicate and disseminate research priorities at national and regional academic meetings; strengthen community-based education and outreach partnerships with university cancer programs; coauthor articles in lay and scientific publications; and inform research and policy in areas such as mechanobiology, theoretical and spatial modeling, single cell technologies, the role of aging in cancer, novel quantitative methods, imaging and immune cell interactions, in vivo/organoid models, and in vitro and/or genetically-engineered models.
Clearly, incentives created through these exemplary government policy measures are shifting culture toward the evolving inclusion of advocates as credible stakeholders. Nonetheless, the infrastructure needed to take transdisciplinary processes to the next level is limited. For instance, the consistency required to list advocates on a particular group’s NCI website has not been uniformly applied. Given the aim to advance advocate engagement strategies throughout the physical sciences and oncology continuum, we share the hope with members of the Advocate Working Group that prominent visibility should be put in place to acknowledge advocate leadership by name and position on PS-ON websites. The underlying issue is not just giving rhetorical allegiance to advocacy. It is also, more basically, about coming up with processes and practices that reflect equity imperatives and priorities. As it stands, the lead national PS-ON volunteer advocate is an invited member of the Advisory Council and Steering Committee, but is not currently listed by name on the PS-ON website, and there is no mention of advocates as stakeholders on the NCI website (http://cancer.ucsf.edu/research/programs/breast/). Moreover, given our concern that a hidden or attenuated advocacy presence is a call to act, we believe that the benefit of an NCI-led web portal for references to PS-ON advocacy engagement would be improved by their provision as open access sources, rather than the registration-restricted access that currently exists.
Why should we care? We have entered a new phase of physical sciences and oncology research, one in which advocacy has become a critical pillar to help forward scientific advances. Yet, while the PS-ON and OAR are leading an effort to promote advocate visibility within physical sciences and oncology, ultimately, the leadership from American Association for Cancer Research (AACR), American Society of Clinical Oncology, California Breast Cancer Research Program, Patient-Centered Outcomes Research Institute (PCORI), Clinical Trials Transformation Initiative, Drug Information Association, Susan G. Komen, US Department of Defense (DOD), NCI, and the US Food and Drug Administration, those at the vanguard pioneering paradigm shifts within drug development and translational settings, must work together to address systemic foundational challenges in order to ensure that new expectations for unequivocal advocate visibility, equity, and empowered partnership benefits research, clinical, and patient communities.
So how else can we collectively bring meaningful change to the system? Recognizing that time is ticking for the patient and that accountability exists to translate findings into practical applications, we argue for goals that are based on genuine expectations for enactment and a funding model that balances priorities for promoting faster cures with realistic objectives and timetables/milestones for completion. Moreover, we share the sincere hope with others that to facilitate progress, we must continue to make a strong case for the growth of federal support, the reform of peer-review processes evolving from the intersection of disciplines, as well as evaluation efforts identifying progress in transdisciplinary team science and advocacy collaboration.
While the time seems right to forward new opportunities for revolutionizing convergence in biomedical science, at the end of the day we are left with a snapshot of the many challenges faced in the effort to create more effective transparent partnerships: tensions between credentialed and lay expertise, complexities of science, competition between differing disciplines, contradictions between the rhetoric and reality of advocacy engagements, and the culture and programmatic changes needed to promote successful advocacy engagements in physical sciences and oncology.
Charting the future of advocacy as a hypothetical game changer in physical sciences and oncology research, we remain hopeful that the next generation of strategic initiatives will benefit from our commentary on areas of harmony and divergence amongst stakeholders, the mutual respect needed for understanding each sector’s unique challenges, the metrics and funding needed for assessing and improving science advocacy effectiveness, the fresh approaches required to reverse the liminality of advocacy roles, as well as the novel tactics taken by committed, albeit tentative partners, who recognize that there is always room for improvement.
Acknowledgements
We thank the leadership of the UCSF Breast Oncology Program and Breast Science Advocacy Core and others for their stewardship of this process. Special thanks to Lamorna Brown-Swigart, Diane Heditsian, Susie Brain, Joan Venticinque, Marjorie Neuwirth, and Samson Walsey for their editorial comments and valuable insights regarding the frameworks, toolkits, and training programs needed to meaningfully engage advocates. We also acknowledge funding from an AACR-Janssen Fellowship in Cancer Interception Research (17-40-48-NORT) to J.J.N., a DOD Breast Cancer Research Program grant (DOD BCRP BC122990,) and a National Institute of Health/National Cancer Institute PS-ON grant (NIH/NCI 1U01CA202241-01) to V.M.W. and S.S., a DOD Era of Hope (BC141351) to M.L. and S.S., a CDMRP Breast Cancer Research Program Grant (W81XWH-16-1-0603) to A.G., S.S., and C.B., a California Breast Cancer Research Program (23IB-0018) IDEA Award to V.P., and a NIH/NCI UCSF Cancer Center Support Grant (P30 CA82103, Ashworth), and a Breast Cancer Research Foundation (BCRF 2014) to L.V., which also supported this work.
References
- 1.Samson SA et al. (2013) Advocacy spurs innovation: promoting synergy between physical and biomedical sciences. EPJ Nonlin. Biomed. Phys 1, 1–13 [Google Scholar]
- 2.Baas C (2010) Helping unravel the complexity of cancer: the role of the advocate. Natl. Cancer Inst. Phys. Sci. Oncol. Perspect 1, 17–18 [Google Scholar]
- 3.Perlmutter J (2011) Advocate Involvement in I-SPY 2. Breast Dis. Yearb. Q 22, 21–23 [Google Scholar]
- 4.Samson S (2012) Bay area physical-sciences in oncology center (PS-OC) advocacy forward: move it! Natl. Cancer Inst. Sci. Oncol. Perspect 1, 16–17 [Google Scholar]
- 5.Silk KJN et al. (2010) The Breast Cancer and the Environment Research Centers: A Transdisciplinary Model, Springer [Google Scholar]
- 6.Collyar D (2005) How have patient advocates in the United States benefited cancer research? Nat. Rev. Cancer 5, 73–78 [DOI] [PubMed] [Google Scholar]
- 7.Mayer M (2009) A seat at the table: a research advocate’s journey. J. Particip. Med 1, e14 [Google Scholar]
- 8.Mayer M (2011) Patient advocacy in research: merely an afterthought? Patient 4, 69–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson M and McCleary KK (2015) From passengers to co-pilots: patient roles expand. Sci. Transl. Med 7, 291fs25. [DOI] [PubMed] [Google Scholar]
- 10.Perlmutter J et al. (2013) Cancer research advocacy: past, present, and future. Cancer Res. 73, 4611–4615 [DOI] [PubMed] [Google Scholar]
- 11.Sheridan S et al. (2017) The PCORI engagement rubric: promising practices for partnering in research. Ann. Fam. Med 15, 165–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Acerbi I et al. (2015) Human breast cancer invasion and aggression correlates with ECM stiffening and immune cell infiltration. Integr. Biol. (Camb.) 7, 1120–1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chambers DA et al. (2016) Convergence of implementation science, precision medicine, and the learning health care system: a new model for biomedical research. JAMA 315, 1941–1942 [DOI] [PMC free article] [PubMed] [Google Scholar]