Abstract
Objective
To evaluate the response to CPAP in patients with chronic insomnia disorder (CID) with OSAS in an unselected patient population including all OSAS severity groups. As a secondary objective, we also wanted to evaluate the differences between patients that improve insomnia symptoms with CPAP and patients that do not improve, specifically evaluating possible gender differences.
Methods
Retrospective study of patients with a diagnosis of OSAS treated with CPAP and CID at the first clinical visit, selected from a database of an outpatient sleep clinic of University Hospital.
Results
From a database of total of 827 patient, 90 patients were identified with OSAS and CID (53.3% women). Middle / moderate OSAS was diagnosed in 68.9% and severe OSA in 31.1%. Most patients (61.1%) improved insomnia symptoms after CPAP therapy. In the responders group, 58.2% had initial insomnia, 63.6% middle insomnia and 12.7% late insomnia. Responders to CPAP were more frequently women (women 61.8%, men 38.2%, p = 0.035) and there was no other difference between responders and non-responders. On subgroup analysis, this difference was significant only in severe OSAS (women 88.9%, men 31.6%, p = 0.013).
Conclusion
In most patients with CID and OSA, there is a consistent reduction of insomnia symptoms with the CPAP use. This factor emphasizes the importance of performing PSG in CID. Insomnia in men with severe OSAS responds less frequently to CPAP suggesting that in these cases the insomnia phenotype is less dependent on the respiratory symptoms.
Keywords: Sleep Apnea, Obstructive; Continuous Positive Airway Pressure; Sleep Initiation and Maintenance Disorders
INTRODUCTION
Chronic insomnia disorder (CID) and obstructive sleep apnea syndrome (OSAS) are two common sleep disorders which frequently co-occur1. Different studies documented that 40-60% of OSAS patients have insomnia symptoms, far exceeding the percentage present in the general population2,3. Furthermore, 29%-67% of patients with insomnia have an apnoea-hypopnoea index greater than 5, indicating the presence of at least a mild degree of sleep-disordered breathing4. These two diseases influence each other in negative ways leading to greater illness severity5. Some studies reveal that patients with OSAS and comorbid insomnia have more depression, anxiety and stress-related symptoms, comparing with patients with isolated OSAS6. Furthermore, OSAS is an established cardiovascular risk factor7 and there is increasing evidences for similar adverse effects in CID8.
Theoretically, the impact OSA treatment in patients with CID may have contradictory results. On the one hand, the most commonly used treatment for OSA is a continuous positive airway pressure (CPAP)9. Some studies suggest that the co-occurrence of OSAS and insomnia symptoms may complicate OSAS treatment and reduce CPAP adherence, leading to increased sleep difficulties10,11, especially in patient with sleep-onset insomnia2. One the other hand, suppressing abnormal respiratory events may reduce frequent awakenings, which may lead to insomnia improvement.
Despite the aforementioned common co-occurrence of OSAS and CID and its cumulative impact on patient's health, few studies have analyzed the impact of OSAS treatment in insomnia symptoms. Earlier studies using small patient groups have suggested that, in mild OSAS, the combined treatment of insomnia with cognitive-behavioral therapy and OSAS treatment with different but predominantly surgical modalities was superior to isolated insomnia treatment12-14.
More recent case series showed significant improvement in insomnia symptoms in OSAS patients when treated with CPAP2,15-17. However, these studies analyzed mostly patients with severe OSAS diagnosed with ambulatory cardiorespiratory recordings12 or patients without comorbidities like anxiety17. Furthermore there is evidence to support that man and women have different OSAS related symptoms18 and different clinical profiles when OSAS is comorbid with insomnia19. None of the previous studies has specifically analyzed differences in insomnia symptoms response to CPAP treatment in men and women.
We have, therefore, aimed at evaluating the response to CPAP in patients with CID with OSAS in an unselected patient population including all OSAS severity groups. As a secondary objective, we also wanted to evaluate the differences between patients that improve insomnia symptoms with CPAP and patients that do not improve, specifically evaluating possible gender differences.
METHODS
The study is a retrospective case series. Patients were selected from a database of an outpatient sleep clinic of University Hospital - Hospital de Santa Maria, Centro Hospitalar Lisboa Norte. All patients with a diagnosis of OSAS treated with CPAP and CID at the first clinical visit were included. Patients without clinical follow-up or with insomnia that developed after CPAP use were excluded. OSAS and CID were diagnosed clinically by a sleep disorders specialist.
OSAS was considered when there is five or more predominantly obstructive respiratory events per hour of sleep during PSG plus signs/symptoms (associated sleepiness, fatigue, insomnia, snoring, subjective nocturnal respiratory disturbance, or observed apnea) or associated medial or phychiatric disorder (hypertension, coronary artery disease, atrial fibrillation, congestive heart failure, stroke, diabetes, cognitive dysfunction or mood disorder), according to ICSD-3 criteria.
OSAS severity was classified as mild/ moderate when the RDI was between 5-30/h and severe when the RDI was ≥ 30/h. Hypopneas were classified when there was a > 30% reduction of nasal flow associated with 3% desaturation or microarousal, according to the most recent AASM criteria20. Questions regarding sleep quality were also evaluated through a structured questionnaire that is applied to all patient on the first clinical visit. The main outcome was insomnia improvement after CPAP use, based in clinical impression by a sleep specialist, as recorded in the patient clinical file, from 1 to 12 months after CPAP start. CPAP responder was considered when the patients improved insomnia after initiating CPAP. Given the retrospective nature of the study, the periodicity of the clinical visit was variable. However, as a general rule in our sleep clinic, patients are evaluated 1 month, 3 months and 12 months after starting CPAP.
Other variables analyzed were age, sex, body mass index (BMI), presence of vascular risk factors, presence of anxiety/depressive symptoms, use of sedative/hypnotic treatment before CPAP use, Apnea hypopnea index (AIH), Respiratory distress index (RDI), Epworth sleepiness scale (ESS), CPAP compliance, sedative/hypnotics after the CPAP use, OSAS severity and type of insomnia (initial, maintenance, terminal). CPAP compliance was considered when there was > 75% of use during > 4hours.
Statistical analysis included descriptive statistics and comparisons between responders and non-responders to CPAP made with T test in continuous variables, Qui2 or Fischer exact test in categorical variables (p < 0.05).
RESULTS
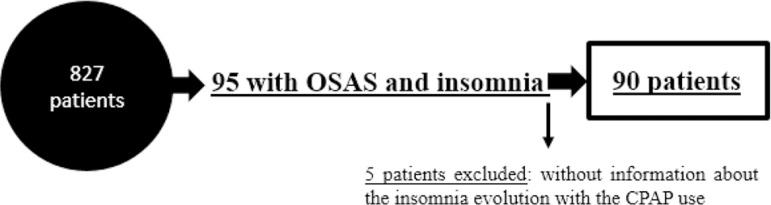
From 827 patients, 95 patients had OSAS and CID in the first clinical evaluation. Five patients were excluded because they did not have follow up information regarding insomnia evolution after CPAP use. Therefore 90 patients were evaluated in this study (Figure 1). Table 1 documents the clinical characteristics of the patients, based on questionnaire responses.
Figure 1.
Flow chart of the participants.
Table 1.
The clinical characteristics of the patients, based on questionnaire responses.
| All (n=90) | |
|---|---|
| Do you have problems in fall asleep? | Yes 59.0% |
| Do you awake up during night? | Yes 98.8% |
| How many times do you wake up during night? | 3.35±1.457 |
| How long do you stay awake? | 3.99±2.471 |
| Have you been sleepy? | Yes 54.2% |
| Have you been tiredness? | Yes 75% |
| Do you have sleep or tired problems in your work? | Yes 48.2% |
| How often do sleep problems arise? | Continuously 52.2 %, Sporadically 6.7%; Often 36.7%; Periodically 4.4% |
The baseline characteristics are presented in Table 2. From the 90 patients with OSAS and insomnia, 53.3% were females. The mean age was 62.1±11.64 years. Most patients were obese (mean BMI 28.68±4.9 kg/m2). Before starting CPAP, 55.6% of patients were on sedative/hypnotic drugs and 36.1% had anxiety/depressive symptoms. Around two thirds (68,9%) had mild/moderate sleep apnea (mean AHI 23.75±18.99; RDI 24.95±13.9). Most patients were not sleepy (mean ESS 8.80±5.26).
Table 2.
Baseline characteristics.
| All (n=90) | |
|---|---|
| Sex | Female 53.3% |
| Age | Mean 62.06±11.64; Median 64.00 |
| BMI | Mean 28.68±4.88; Median 27.74 |
| Vascular risk factors | Yes 57.8% |
| Anxiety/ depressive symptoms (n=83) | Yes 36.1% |
| Use of the sedative therapeutic before the CPAP use | Yes 55.6% |
| AHI | Mean 23.75±18.99; Median 17.0 |
| RDI | Mean 24.95±13.93; Median 21.0 |
| ESS | Mean 8.80±5.26; Median 8.00 |
| CPAP compliance | Yes 78.9% |
| Sedative therapeutic after CPAP beginning (n=85) | Yes 35.3% |
BMI- body mass index, AHI- apnea hypopnea index; RDI- respiratory disturb index; ESS- Epworth sleepiness scale;
Age, BMI, AHI, RDI, ESS: mean ±SD.
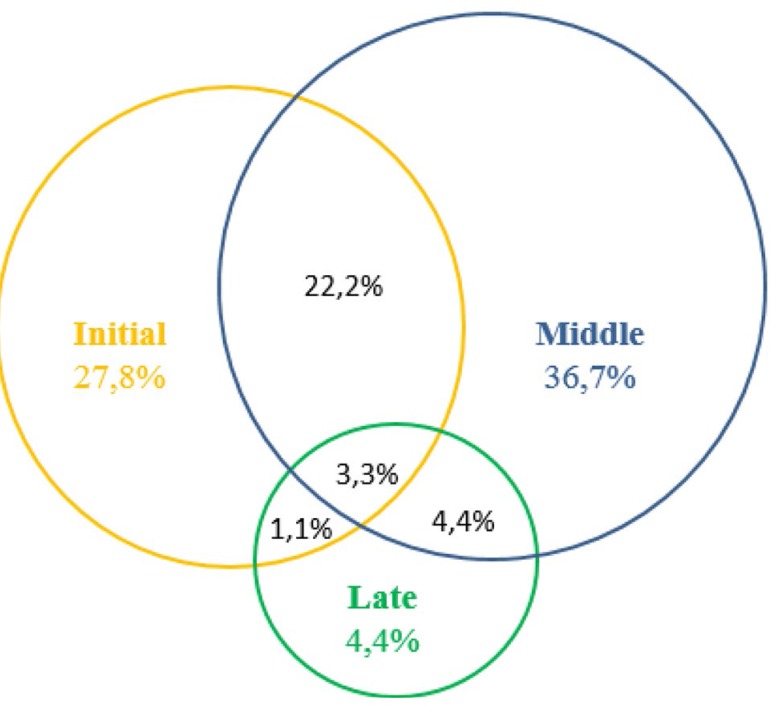
The Figure 2 shows the baseline prevalence of insomnia symptoms among all patients. The most common insomnia subtype was intermediate insomnia, but initial and terminal insomnia were also present. It is important reinforce that there were also patients with concomitant initial and middle insomnia (22.2%), middle and late insomnia (4.4%), initial and late insomnia (1.1%) and also patients that complained of the three insomnia subtypes (3.3%) (Figure 2).
Figure 2.
Baseline prevalence of insomnia symptoms among all patients.
Most patients (78.9%) were compliant with CPAP. One third of the patients (35.3%) had to start hypnotic/sedative treatment after CPAP. Most of this treatment was introduced to increase CPAP compliance (67.9%) or depressive/anxiety symptoms (21.5%). Only 10.7% of the patients started pharmacological treatment specifically to decrease insomnia symptoms. This treatment was transient in 20% of these patients, having been discontinued at 12 months follow-up.
Insomnia symptoms improved in 61.1% for the patients after CPAP use. This was noted, on average, 5.35±4 months after CPAP use. From these patients, 58.2% had initial insomnia, 63.6% middle insomnia and 12.7% late insomnia.
Table 3 describes the differences between responders and non-responders to CPAP. Responders were more frequently women (p value=0.035). We did not find any other difference between these two groups. Improvement after CPAP was similar in men and women with mild/moderate OSA. However, men with severe OSA were less likely to improve insomnia symptoms (31.6%) that women (88.9%) after CPAP (Table 4).
Table 3.
Baseline characteristics difference between the responders and non-responders to CPAP.
| n=90 | |||
|---|---|---|---|
| Responders (n = 55) | Non- responders (n=35) | p value | |
| Age | 62.78±10.70 | 60.91±13.07 | 0.461 |
| Sex | Fem 61.8%; Male 38.2% | Fem 40%; Male 60% | 0.035 |
| BMI | 28.85±4.68 | 28.45±5.20 | 0.724 |
| Vascular risk factors | Yes 40.0% | Yes 54.3% | 0.593 |
| Anxiety/ depressive symptoms | Yes 38.5% | Yes 32.3% | 0.569 |
| AHI | 22.02±16.78 | 26.48±22.00 | 0.280 |
| RDI | 22.61±12.15 | 26.17±16.51 | 0.349 |
| OSAS type | Mid/Mod 74.6%; Severe 25.4% | Mid/Mod 60.0% Severe 40.0% | 0.167 |
| Initial insomnia | Yes 58.2% | Yes 48.6% | 0.394 |
| Middle insomnia | Yes 63.6% | Yes 71.4% | 0.298 |
| Late insomnia | Yes 12.7% | Yes 20.0% | 0.262 |
| CPAP compliance | Yes 76.4% | Yes 82.9% | 0.611 |
| Sedative therapeutic after CPAP | Yes 34.0% | Yes 31.1% | 0.471 |
Table 4.
Difference by sex in insomnia improvement after the CPAP use, according the OSAS type.
| Middle/moderate OSAS | Insomnia improvement | p = 0.561 | |
| Yes | No | ||
| Sex | Women | n=26, 66.7% | n=13, 33.3% |
| Men | n=15, 65.2% | n=8, 34.8% | |
| Severe OSAS | Insomnia improvement | p = 0.013* | |
| Yes | No | ||
| Sex | Women | n=8, 88.9% | n=1, 11.1% |
| Men | n=6, 31.6% | n=13, 68.4% | |
In Supplementary material, the baseline characteristics of men and women from our sample are described. The only significant difference was a higher percentage of women with anxiety/depression (see in Supplementary material, Table 1).
DISCUSSION
The population of this study was evaluated retrospectively, considering a target population with OSAS and insomnia which started CPAP. We analyzed the occurrence of insomnia improvement in the first 12 months after beginning CPAP. Our results suggest that CPAP has a positive effect in insomnia improvement. From the 90 patients, 61.1% improved insomnia with CPAP use. This percentage of response is similar to other studies2,15-17. Our data shows that even insomniac patients with mild/moderate sleep apnea may respond to CPAP treatment and this response is independent on the presence of previous psychiatric disorders.
In our study, insomnia subtypes were not associated with different treatments responses. Our sample included few patients with isolated terminal insomnia, rendering this patient group less amenable to conclusions. However, we had one third of patients with isolated sleep-onset insomnia. In this group, 58% showed improvement after CPAP, a percentage similar to patients with sleep-maintenance insomnia (68%). The study by Björnsdóttir et al.2 has suggested that only patients with sleep-maintenance insomnia improve after CPAP. In their study, patients with initial insomnia were uncommon (only 3% of the entire insomniac patients) probably due to the way patients were selected, from a cohort of OSAS patients.
We included in our sample all patients referred to the sleep clinic, regardless of the reason of referral, as long as on the first clinical interview CID was diagnosed and OSAS was diagnosed on a PSG. They suggest that middle insomnia improves after CPAP because there are less OSAS related awakenings. However, there is another mechanism by which OSAS treatment may lead to insomnia improvement. Reducing symptoms of un-refreshed sleep with CPAP treatment in OSAS reduces the negative impact of bad sleep on daytime functioning and may lead to less sleep-related effort. This mechanism is of foremost importance in all cognitive-behavioral programs for insomnia21.
The most striking finding in our study is related to the gender differences in insomnia response to CPAP treatment. In our cohort, women with insomnia and OSAS were more likely to improve their insomnia symptoms after CPAP, particularly so in the severe OSAS group. There are few studies that have specifically looked from different treatment responses in men and women with OSA. It is noteworthy that the only difference between men and women was higher frequency of depressive symptoms in women. Factors that might be related to this different response, like OSAS severity, CPAP compliance and insomnia subtypes were similar in both groups.
There are very few studies that evaluate sex differences comorbid OSAS and insomnia. One study showed that gender differences in these two pathologies could be partially explained by different sleep architectures between men and women. Men with OSAS-insomnia had decreased sleep efficiency and increased sleep latency comparing to men with OSAS-alone. In contrast, PSG based sleep architecture was not different between women with OSAS-insomnia and OSA alone22.
Insomnia is a much more common manifestation of OSAS in women than in men23. It is possible to hypothesize that for men with OSAS to develop insomnia, the relative importance of other insomnia related-factors, namely genetic, environmental, behavioral or physiological19 has to be bigger than in women. This group of patients may require more specific insomnia related interventions.
It is important to acknowledge that 38.9% of the patients did not improve insomnia with CPAP therapy despite having a good CPAP compliance. Insomnia is a multifactorial disorder and there are other mechanisms related to insomnia which do not depend from respiratory sleep disturbance. Recent reports have shown that insomnia patients may be divided in different phenotypes, related mostly to personality, mood and well-being and psychological reactions to insomnia or life events24.
The response to CPAP therapy may different in this various insomnia phenotypes but further studies specifically designed to evaluate different insomnia subtypes are necessary to confirm this hypothesis. As previously analyzed in small clinical trials and case series4,13 the best treatment approach to patients with comorbid CID and OSAS is combined OSA treatment and cognitive behavioral therapy. These small studies suggest that this combined approach is better than each isolated treatment per se.
Another important clinical finding from our study is the high percentage of compliance to CPAP in patients with OSAS and insomnia. Despite initial studies that suggested that this group of patients might have difficulties with CPAP therapy25 other authors have also shown that CPAP compliance is not influenced by comorbid insomnia, with CPAP use per night ranges from 6.2 to 3.4 hours26,27.
We acknowledge that this study has important limitations. First, it is a retrospective study, carried out on patients followed on usual clinical practice. None of the patients entered a specific cognitive -behavioral therapy program for insomnia (CBTi). However, the clinicians following all patients had expertise in sleep medicine and techniques of CBTi, which were most likely used in each clinical visit. The effect of this cannot be evaluated in our study design28. Secondly, one third of the patients started sedative therapy after the onset of CPAP, which may have contributed to the final result. This variable had not been previously evaluated2,15-17.
Nonetheless, all these patients had chronic insomnia and were previously refractory to these treatments (55.6% did sedative therapeutic before the PAP use) and the percentage of sedative treatment initiation was not different between responders and non-responders. Furthermore, 60.0% of the patients that did not change treatment also showed improvement. It is also noteworthy that CPAP compliance information was evaluated based on clinical impression and no quantitative adherence values were included in our analysis. However, this clinical impression is always based on automated CPAP reports.
Lastly, insomnia improvement after the CPAP use was evaluated through clinical impression. Validated insomnia questionnaires are not used routinely in our sleep clinic, so this data was not available. It was not possible also to establish which insomnia symptoms, in patients with concomitant initial, middle or terminal insomnia improved mostly. Nonetheless, we consider that the information derived from the clinician opinion is a good reflection of the usual clinical practice.
To summarize, our results show that in most patients with CID and OSA, there is a consistent reduction of insomnia symptoms with the CPAP use. This factor emphasizes the importance of performing PSG in CID, as recently suggested in European guidelines for insomnia management29. Insomnia in men with severe OSAS responds less frequently to CPAP suggesting that in these cases the insomnia phenotype is less dependent on the respiratory symptoms. Further studies are needed to understand and confirm this finding and define the best treatment approach to this subgroup of patients.
REFERENCES
- 1.Zhang Y, Ren R, Lei F, Zhou J, Zhang J, Wing YK, et al. Worldwide and regional prevalence rates of co-occurrence of insomnia and insomnia symptoms with obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev. 2019;45:1–17. doi: 10.1016/j.smrv.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Björnsdóttir E, Janson C, Gíslason T, Sigurdsson JF, Pack AI, Gehrman P, et al. Insomnia in untreated sleep apnea patients compared to controls. J Sleep Res. 2012;21(2):131–138. doi: 10.1111/j.1365-2869.2011.00972.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krell SB, Kapur VK. Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath. 2005;9(3):104–110. doi: 10.1007/s11325-005-0026-x. [DOI] [PubMed] [Google Scholar]
- 4.Luyster FS, Buysse DJ, Strollo PJ., Jr Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196–204. [PMC free article] [PubMed] [Google Scholar]
- 5.Krakow B, Melendrez D, Ferreira E, Clark J, Warner TD, Sisley B, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923–1929. doi: 10.1378/chest.120.6.1923. [DOI] [PubMed] [Google Scholar]
- 6.Smith S, Sullivan K, Hopkins W, Douglas J. Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS) Sleep Med. 2004;5(5):449–456. doi: 10.1016/j.sleep.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Archontogeorgis K, Voulgaris A, Nena E, Strempela M, Karailidou P, Tzouvelekis A, et al. Cardiovascular Risk Assessment in a Cohort of Newly Diagnosed Patients with Obstructive Sleep Apnea Syndrome. Cardiol Res Pract. 2018;2018:6572785–6572785. doi: 10.1155/2018/6572785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2014;21(1):57–64. doi: 10.1177/2047487312460020. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1(8225):862–865. doi: 10.1016/s0140-6736(81)92140-1. [DOI] [PubMed] [Google Scholar]
- 10.Pieh C, Bach M, Popp R, Jara C, Crönlein T, Hajak G, et al. Insomnia symptoms influence CPAP compliance. Sleep Breath. 2013;17(1):99–104. doi: 10.1007/s11325-012-0655-9. [DOI] [PubMed] [Google Scholar]
- 11.Wickwire EM, Smith MT, Birnbaum S, Collop NA. Sleep maintenance insomnia complaints predict poor CPAP adherence: A clinical case series. Sleep Med. 2010;11(8):772–776. doi: 10.1016/j.sleep.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 12.Guilleminault C, Palombini L, Poyares D, Chowdhuri S. Chronic insomnia, premenopausal women and sleep disordered breathing: part 2. Comparison of nondrug treatment trials in normal breathing and UARS post-menopausal women complaining of chronic insomnia. J Psychosom Res. 2002;53(1):617–623. doi: 10.1016/s0022-3999(02)00463-4. [DOI] [PubMed] [Google Scholar]
- 13.Krakow B, Melendrez D, Lee SA, Warner TD, Clark JO, Sklar D. Refractory insomnia and sleep-disordered breathing: a pilot study. Sleep Breath. 2004;8(1):15–29. doi: 10.1007/s11325-004-0015-5. [DOI] [PubMed] [Google Scholar]
- 14.Guilleminault C, Davis K, Huynh NT. Prospective randomized study of patients with insomnia and mild sleep disordered breathing. Sleep. 2008;31(11):1527–1533. doi: 10.1093/sleep/31.11.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyên XL, Rakotonanahary D, Chaskalovic J, Fleury B. Insomnia related to sleep apnoea: effect of long-term auto-adjusting positive airway pressure treatment. Eur Respir J. 2013;41(3):593–600. doi: 10.1183/09031936.00080011. [DOI] [PubMed] [Google Scholar]
- 16.Glidewell RN, Renn BN, Roby E, Orr WC. Predictors and patterns of insomnia symptoms in OSA before and after PAP therapy. Sleep Med. 2014;15(8):899–905. doi: 10.1016/j.sleep.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Mendes MS, dos Santos JM. Insomnia as an expression of obstructive sleep apnea syndrome--the effect of treatment with nocturnal ventilatory support. Rev Port Pneumol (2006) 2015;21(4):203–208. doi: 10.1016/j.rppnen.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Won C, Guilleminault C. Gender differences in sleep disordered breathing: implications for therapy. Expert Rev Respir Med. 2015;9(2):221–231. doi: 10.1586/17476348.2015.1019478. [DOI] [PubMed] [Google Scholar]
- 19.Lee MH, Lee SA, Lee GH, Ryu HS, Chung S, Chung YS, et al. Gender differences in the effect of comorbid insomnia symptom on depression, anxiety, fatigue, and daytime sleepiness in patients with obstructive sleep apnea. Sleep Breath. 2014;18(1):111–117. doi: 10.1007/s11325-013-0856-x. [DOI] [PubMed] [Google Scholar]
- 20.The AASM Manual for the Scoring of Sleep and Associated Events. Darien: AASM; 2018. [Google Scholar]
- 21.Katofsky I, Backhaus J, Junghanns K, Rumpf HJ, Hüppe M, von Eitzen U, et al. Effectiveness of a cognitive behavioral self-help program for patients with primary insomnia in general practice - a pilot study. Sleep Med. 2012;13(5):463–468. doi: 10.1016/j.sleep.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 22.Buysse DJ. Insomnia. JAMA. 2013;309(7):706–716. doi: 10.1001/jama.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suh S, Cho N, Zhang J. Sex Differences in Insomnia: from Epidemiology and Etiology to Intervention. Curr Psychiatry Rep. 2018;20(9):69–69. doi: 10.1007/s11920-018-0940-9. [DOI] [PubMed] [Google Scholar]
- 24.Blanken TF, Benjamins JS, Borsboom D, Vermunt JK, Paquola C, Ramautar J, et al. Insomnia disorder subtypes derived from life history and traits of affect and personality. Lancet Psychiatry. 2019;6(2):151–163. doi: 10.1016/S2215-0366(18)30464-4. [DOI] [PubMed] [Google Scholar]
- 25.Ghosh D, Allgar V, Elliott MW. Identifying poor compliance with CPAP in obstructive sleep apnoea: a simple prediction equation using data after a two week trial. Resp Med. 2013;107(6):936–942. doi: 10.1016/j.rmed.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 26.Björnsdóttir E, Janson C, Sigurdsson JF, Gehrman P, Perlis M, Juliusson S, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013;36(12):1901–1909. doi: 10.5665/sleep.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nguyên XL, Chaskalovic J, Rakotonanahary D, Fleury B. Insomnia symptoms and CPAP compliance in OSAS patients: A descriptive study using Data Mining methods. Sleep Med. 2010;11(8):777–784. doi: 10.1016/j.sleep.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 28.Dyas JV, Apekey TA, Tilling M, Ørner R, Middleton H, Siriwardena AN. Patients' and clinicians' experiences of consultations in primary care for sleep problems and insomnia: a focus group study. Br J Gen Pract. 2010;60(574):e180–e200. doi: 10.3399/bjgp10X484183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. doi: 10.1111/jsr.12594. [DOI] [PubMed] [Google Scholar]